Abstract
Background and study aims: Type III achalasia is characterized by rapidly propagating pressurization attributable to spastic contractions. Although laparoscopic Heller myotomy (LHM) is the current gold standard management for type III achalasia, peroral endoscopic myotomy (POEM) is conceivably superior because it allows for a longer myotomy. Our aims were to compare the efficacy and safety of POEM with LHM for type III achalasia patients.
Patients and methods: A retrospective study of 49 patients who underwent POEM for type III achalasia across eight centers were compared to 26 patients who underwent LHM at a single institution. Procedural data were abstracted and pre- and post-procedural symptoms were recorded. Clinical response was defined by improvement of symptoms and decrease in Eckardt stage to ≤ 1. Secondary outcomes included length of myotomy, procedure duration, length of hospital stay, and rate of adverse events.
Results: Clinical response was significantly more frequent in the POEM cohort (98.0 % vs 80.8 %; P = 0.01). POEM patients had significantly shorter mean procedure time than LHM patients (102 min vs 264 min; P < 0.01) despite longer length of myotomy (16 cm vs 8 cm; P < 0.01). There was no significant difference between POEM and LHM in the length of hospital stay (3.3 days vs 3.2 days; P = 0.68), respectively. Rate of adverse events was significantly less in the POEM group (6 % vs 27 %; P < 0.01).
Conclusions: POEM allows for a longer myotomy than LHM, which may result in improved clinical outcomes. POEM appears to be an effective and safe alternative to LHM in patients with type III achalasia.
Abbreviations
- LHM
laparoscopic Heller myotomy
- EGJ
esophagogastric junction
- LES
lower esophageal sphincter
- POEM
peroral endoscopic myotomy
Introduction
The Chicago classification of esophageal motility disorders divides achalasia into three subtypes based on high-resolution esophageal manometry 1. Type I achalasia is characterized by minimal contractility of the esophageal body. Type II achalasia is the most common type occurring in 65 % of patients and is defined by absence of peristalsis and intermittent periods of compartmentalized esophageal pressurization. Type III achalasia is the least common occurring in 10 % of patients and is distinguished by spastic contractions that can involve the entire length of esophagus 2.
There are a variety of therapies available to palliate the symptoms of achalasia with varying rates of success 3. Type III achalasia is classified as a spastic esophageal disorder and is the least well studied achalasia subtype because of its low incidence. Management of spastic esophageal disorders is a particular challenge and standard pharmacologic and endoscopic therapy fail in as many as 74 % of patients 4. The outcomes of transabdominal laparoscopic Heller myotomy (LHM) for type III achalasia has been reported in subgroup analysis of achalasia studies with clinical response rates of 69.3 % to 86 % 5 6. These outcomes are inferior to LHM for other achalasia subtypes as evidenced by response rates for type II of 95 % 5 6. The lower response rates observed in type III achalasia are presumably because of the limitation of the proximal extent of esophageal myotomy that can be reliably achieved with the surgical approach.
Peroral endoscopic myotomy (POEM) was first described in a porcine model in 2007, and now, seven years later, more than 5 000 clinical procedures have been performed in several centers across the world 7 8. Initial clinical data from Europe, Asia, and United States has demonstrated the effectiveness and safety of this procedure when performed by experienced endoscopists 8. POEM is potentially an ideal endoscopic therapy for type III achalasia because it not only allows myotomy of the lower esophageal sphincter (LES) but also of the esophageal body, where the hypertensive contractions often occur 9. There are currently no reports comparing the outcomes of POEM with LHM for the management of type III achalasia.
Our hypothesis was that the suboptimal clinical response observed with LHM in the treatment of type III achalasia is due to an inadequate myotomy length. Therefore, because POEM allows for a longer myotomy, it may be more successful in achieving clinical response. Our aims were to compare the effectiveness and safety of POEM and LHM for the treatment of patients with type III achalasia.
Patients and methods
This retrospective study was approved by the Institutional Review Board for Human Research and complied with Health Insurance Portability and Accountability Act regulations at each institution. All patients who underwent POEM for treatment of type III achalasia at eight centers (4 US, 3 Asian, and 1 European) between January 2011 and November 2013 were included. Results from these patients were compared to those of a retrospective cohort of patients who had undergone transabdominal LHM for type III achalasia between August 2000 and December 2013 at a single tertiary United States institution (Johns Hopkins Hospital). In all patients, the diagnosis was based on a combination of clinical presentation, barium esophagram, and manometric findings. Because the Chicago classification was published in 2008, all patients with a diagnosis of spastic or vigorous achalasia (diagnosis made prior to 2008) were defined as having type III achalasia in this study 10. Patients with other spastic esophageal disorders (Jackhammer esophagus, diffuse esophageal spasm) and altered surgical anatomy were excluded. Patients in the POEM cohort were identified from a multicenter database of spastic esophageal disorders. Patients in the LHM cohort were identified by review of the single institution’s billing database and those who had the indication of vigorous, spastic, or type III achalasia were included. Relevant clinical (prior therapy, Eckardt stage), manometric findings, length of myotomy, and procedure time were abstracted (Fig. 1) 11. Pre-procedural and post-procedural symptoms (eg, Eckardt stage, requirement for ongoing PPI therapy, and need for subsequent therapy) were also recorded. Adverse events were graded according to the American Society for Gastrointestinal Endoscopy (ASGE) lexicon’s severity grading system 12.
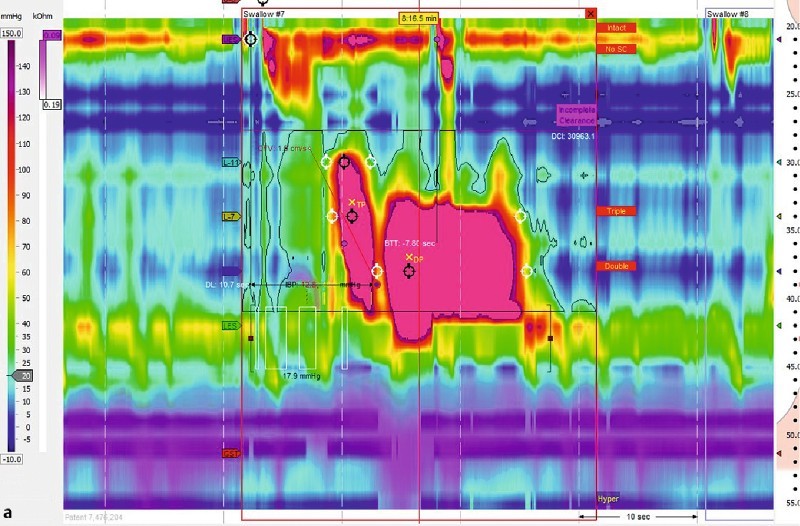
Fig. 1 Manometric and endoscopic findings in a patient with type III achalasia. a High intensity spastic contraction (DCI of 30,000) with elevated lower esophageal sphincter baseline pressure typical of type III achalasia. b Endoscopic view during an episode of spastic contraction in the midesophagus.
Clinical response was defined by improvement of symptoms and decrease in Eckardt stage to ≤ 1 (Table 1) 13 14 15. The length of follow-up for patients was defined as the time from the procedure to the date of last clinical follow-up.
Table 1. Eckardt symptom scoring and staging.
| Score | Dysphagia | Retrosternal pain | Regurgitation | Weight loss |
| 0 | None | None | None | None |
| 1 | Occasional | Occasional | Occasional | < 5 Kg |
| 2 | Daily | Daily | Daily | 5 – 10 Kg |
| 3 | Every meal | Every meal | Every meal | > 10 Kg |
| Stage 0 | Stage 1 | Stage 2 | Stage 3 | |
| Score total | 0 – 1 (Remission) | 2 – 3 (Remission) | 4 – 6 (Failure) | > 6 (Failure) |
POEM procedures
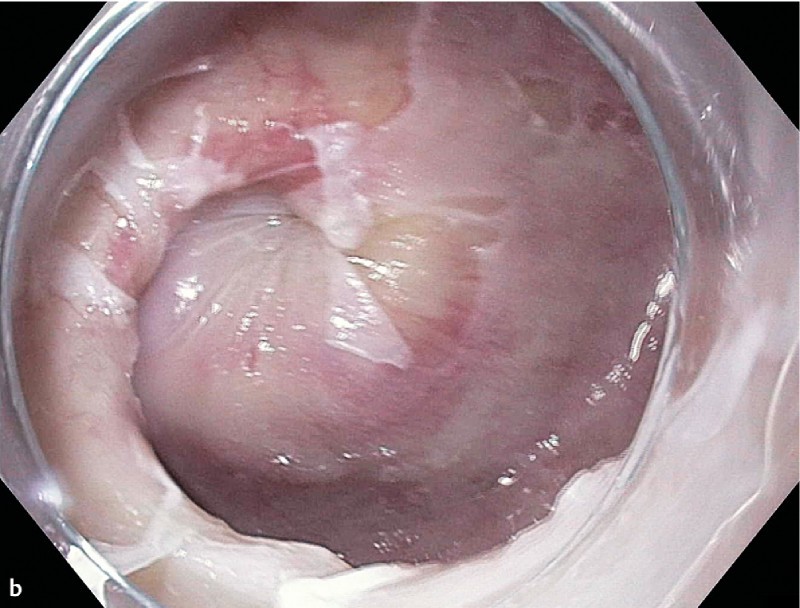
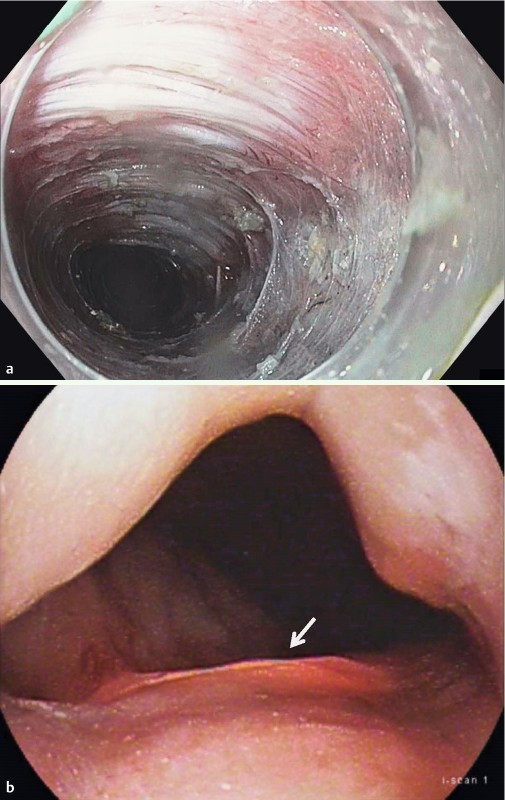
POEM procedures were performed as previously described by Inoue et al. using high-definition gastroscopes fitted with transparent caps under general anesthesia and insufflation using carbon dioxide 16. Either a triangular tip knife (KD 640 L, Olympus, Japan) or HybridKnife (ERBE, Tubingen, Germany) was used. In brief, after a submucosal bleb was created, a longitudinal mucosal incision was made and the endoscope then entered the submucosal space. The submucosal fibers were dissected and a submucosal tunnel was extended 2 cm – 3 cm into the proximal stomach (Fig. 2). Subsequently, either selective myotomy of the inner circular muscle bundles or full-thickness myotomy was performed (Fig. 3). The length of myotomy was determined based on the findings at high-resolution esophageal manometry and/or the proximal level of visible spastic contractions observed endoscopically. Mucosal entry was closed using endoscopic clips (Video 1).
Fig. 2.
Treatment of a patient with spastic esophageal disorder. a Long submucosal tunnel performed during peroral endoscopic myotomy. b Translumination observed 3 cm below the esophagogastric junction indicating extension of myotomy into the proximal stomach.
Fig. 3.
Myotomy during peroral endoscopic myotomy. a Selective inner circular myotomy. b Full thickness myotomy.
Video
Characteristic endoscopic findings and steps involved during peroral endoscopic myotomy in a patient with type III achalasia.
Laparoscopic Heller myotomy procedures
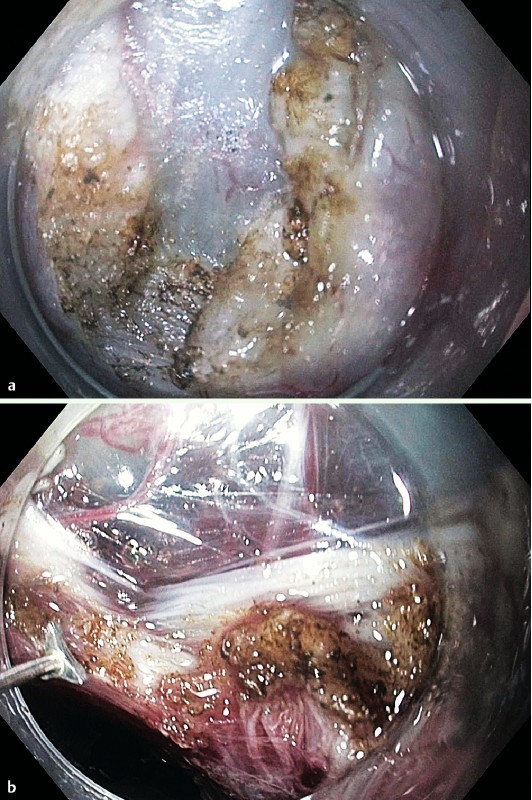
LHM procedures were performed using the daVinci robotic system (Intuitive Surgical, Inc., Palo Alto, California, United States) via a transabdominal approach. The diaphragmatic hiatus was dissected open to allow for mobilization of the medial esophagus to at least 6 cm proximal to the esophagogastric junction (EGJ). A myotomy of both the circular and longitudinal muscle layers was performed from at least 6 cm proximal to the EGJ to 2 cm – 3 cm into the proximal stomach using hook electrocautery (Fig. 4). The open jaws of a laparoscopic grasper (2.5 cm) were used to measure myotomy length. The crura was then loosely approximated to allow for the passage of a 5 mm diameter instrument through the hiatus. Patients then underwent a 270° posterior (Toupet) fundoplication or anterior 180° (Dor) fundoplication for postoperative reflux control. A posterior Toupet fundoplication was performed preferentially unless excessive angulation of the EGJ resulted or mucosal perforation occurred in which patient an anterior Dor fundoplication was utilized.
Fig. 4.
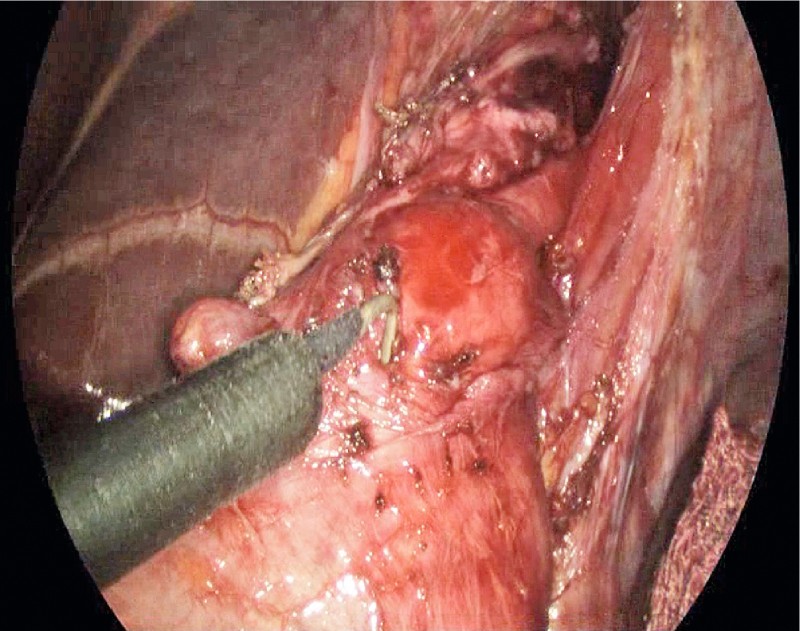
Intraoperative image of the myotomy during transabdominal laparoscopic Heller myotomy.
All patients were subsequently admitted for inpatient hospital observation. Esophagram was obtained the following day and soft diet was commenced after esophageal leak was excluded.
Study outcomes
Our primary outcome was clinical response, which was defined as improvement in symptoms reflected by an Eckardt stage ≤ 1 at time of last clinical follow-up. Our secondary outcomes were length of myotomy, procedure duration, requirement for ongoing PPI therapy, length of hospital stay, and rate of adverse events.
Results are reported as mean ± standard deviation (SD) and/or range for quantitative variables, and absolute and relative frequencies for categorical variables. Outcomes between pre- and post-procedure parameters were compared using the Student’s t-test (paired t-test/Wilcoxon, where applicable) for continuous variables and the Chi-squared test for categorical variables. Chi-squared test/Fisher’s exact test and t-test/Mann – Whitney U test were used to compare patient and procedural characteristics for the two groups. A univariate and multivariate analysis taking into consideration the factors of age, gender, pre-procedure Eckardt stage, prior therapy, residual pressure, and the procedure type were performed. Statistical significance was based on two-sided design-based tests evaluated at α = 0.05. Statistical analysis was performed using STATA v13.
Results
There were 63 patients that underwent POEM for spastic esophageal disorders with 14 being excluded (Jackhammer, 8; diffuse esophageal spasm, 6) leaving 49 suitable for analysis. There were 187 patients that underwent LHM for achalasia with 161 being excluded (149 had achalasia subtype I or II and 12 had achalasia subtype not specified). Therefore, there were 26 patients in this cohort suitable for analysis (Fig. 5). The baseline demographics were similar between the POEM and LHM group with respect to age (58.3 years vs 51.6 years; P = 0.15) and sex (women: 40.8 % vs 50.0 %, P = 0.45) (Table 2).
Fig. 5.
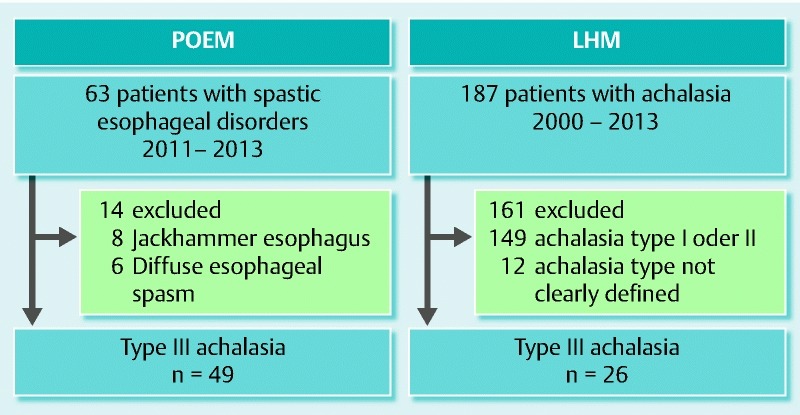
Flow diagram depicting the criteria used to include patients suitable for analysis.
Table 2. Baseline characteristics of patients who underwent peroral endoscopic myotomy and laparoscopic Heller myotomy.
| POEMn = 49 | LHMn = 26 | P value | |
| Age, mean (SD) | 58.3 (18.8) | 51.6 (17.9) | 0.15 |
| Female, n (%) | 20 (40.8) | 13 (50.0) | 0.45 |
| Prior therapy, n (%) None Endoscopic therapies LHM | 30 (61.2)15 (30.6)4 (8.2) | 7 (26.9)19 (73.1)0 | < 0.01 < 0.010.29 |
| Eckardt stage, n (%) 0 I II III | 1 (2.0)2 (4.1)24 (49.0)22 (44.9) | 004 (15.4)22.0 (84.6) | 10.54 < 0.01 < 0.01 |
| Mean residual pressure, mmHg (SD) | 34.4 (15.5) | 36.2 (13.9) | 0.79 |
There were statistically significant differences between the two groups with regard to prior therapies with 38.8 % of patients in the POEM cohort undergoing prior therapy as opposed to 72 % of patients in the LHM cohort (P < 0.01). There were 4 patients (8.2 %) in the POEM cohort that had been treated previously with LHM (Table 2).
There was no statistically significant difference in the LES mean residual pressure at baseline between POEM and LHM (34.4 mmHg vs 36.3 mmHg; P = 0.79). However, statistically significant differences in the pre-procedure Eckardt symptom stage were noted between the two groups with patients in LHM having a higher mean baseline Eckardt stage than those in POEM (2.85 vs 2.37; P < 0.01) (Table 2).
The primary outcome of clinical response was statistically significant more frequently with POEM than with LHM (98.0 % vs 80.8 %; P = 0.01) at a mean follow-up of 8.6 months vs 21.5 months, respectively (P < 0.01). One patient in the POEM cohort was deemed a clinical failure because they had an Eckardt symptom of stage II on follow-up despite resolution of their pre-procedure manometry abnormality. There were five patients (19.2 %) in the LHM cohort who did not meet the primary outcome. Two patients (7.7 %) were subsequently treated successfully with a second LHM and the other went onto have an esophagectomy after failing Botox and pneumatic dilation. The other three patients, despite having an Eckardt stage II on follow-up, have received no further intervention (Table 3).
Table 3. Procedural characteristics and outcomes.
| POEMn = 49 | LHMn = 26 | P value | |
| Median length of myotomy (cm) | 16 (7 – 26) | 8 (6 – 10) | < 0.01 |
| Median procedure time (min) | 102 (43 – 345) | 264 (189 – 331) | < 0.01 |
| Adverse events, n (%) Mild Moderate Total | 2 (4) 1 (2) 3 (6) | 1 (4) 6 (23) 7 (27) | 1 < 0.01 < 0.01 |
| Mean length of stay, days (SD) | 3.3 (1.9) | 3.2 (2.3) | 0.68 |
| PPI therapy, n (%) | 19 (38.8) | 12 (46.1) | 0.7 |
| Eckardt stage II or III, n (%) | 1 (2.0) | 5 (19.2) | 0.01 |
| Need for subsequent therapy, n (%) | 0 | 2 (7.7) | 0.11 |
| Clinical response, n (%) | 48 (98) | 21 (80.8) | 0.01 |
| Duration of follow-up, months (SD) | 8.6 (1.7) | 21.5 (3.9) | < 0.01 |
Regarding secondary outcomes, the median length of myotomy was twice as long with POEM as compared to LHM (16 cm vs 8 cm; P < 0.01). Despite the statistically significant longer myotomy, the median procedure time was significantly shorter in the POEM cohort (102 min vs 264 min; P < 0.01) (Table 3). There was no statistically significant difference in the mean length of stay between the POEM and LHM cohorts (3.3 days vs 3.2 days; P = 0.68).
The overall rate of adverse events was statistically significantly higher in the LHM cohort (27.0 % vs 6 %; P = 0.01). Additionally, 6/7 adverse events in the LHM cohort were moderate grade as compared to 1/3 in the POEM cohort. The moderate adverse events in the LHM were: ileus (3/6), wound infection (1/6), arrhythmia (1 /6), and urinary tract infection (1/6). The one moderate adverse event in the POEM group was a pulmonary embolus. There were no severe adverse events noted in either group (Table 3). There was no significant difference between POEM and LHM in terms of ongoing requirement for PPI (38.8 % vs 46.1 %; P = 0.7), respectively.
On univariate analysis, LHM patients had statistically significant more odds of being a clinical failure compared to POEM patients (OR, 11.43; 95 %CI, 1.26 – 103.91; P = 0.031). However, on multivariate analysis, there was no statistical difference found, although a trend to significance was noted (OR, 11.32; 95 %CI, 0.86 – 151.39; P = 0.06).
Discussion
There is sufficient evidence to suggest that the subtype of achalasia is an independent predictor of successful outcome after therapy 2 6 10. Type III achalasia is characterized by well-defined, lumen-obliterating spastic contractions in the mid and distal esophagus. In this subtype of achalasia patients, reducing the LES pressure may not suffice to control symptoms, because the segment affected by the spastic motility extends well above the EGJ 2. There is no consensus to guide the clinician as to the optimal treatment modality for patients with type III achalasia. Oral pharmacological therapies have dismal response rates with a paucity of data for their use specifically in type III achalasia. Furthermore, these agents are short acting and associated with side effects, including headache and hypotension often limiting their use 17. Hence, these agents are commonly reserved for patients who are not suitable to undergo more definitive therapies or have failed botulinum toxin injections 18. Botox injections are also associated with poor outcomes with Pandolfino et al. reporting therapeutic success of 9 % in treatment naïve patients 10. Pneumatic dilation has also been shown to be essentially ineffective in type III achalasia patients with response rates between 33 % to 40 % 6 19.
LHM is an established treatment of type III achalasia with success rates far superior to that of the aforementioned less invasive therapies. Salvador et al. reported in their series of 23 patients a clinical response rate of 69.3 % at a mean follow-up of 31 months 5. Rohof et al. reported an 86 % response rate in their series of 18 patients at a mean follow-up of 43 months 6. A long surgical myotomy extending from the LES proximally onto the esophageal body has been used to treat patients with spastic esophageal disorders. Leconte et al. reported in a series of 20 patients who underwent an extended modified transabdominal LHM for DES (14 cm on the esophagus and 2 cm below the EGJ) that dysphagia and chest pain were significantly improved after a median follow-up of 50 months 20.
In 2010, the novel technique of POEM was introduced for esophageal achalasia 16. Existing data suggest that this minimally invasive endoscopic approach achieves similar response to LHM in the management of achalasia 21 22 23 24. Recent reports have also documented its success in patients with spastic esophageal disorders 25 26 27. However, the specific role of POEM in the management of patients with type III achalasia is largely unknown.
Given the data suggesting the relative effectiveness of LHM in treating patients with type III achalasia, we propose POEM as a minimally invasive alternative. The primary advantage of POEM over LHM in this setting is that it allows access to the entire length of the esophagus with ease and thus, an extensive myotomy can be performed. In comparison, access to the proximal esophageal body may not always be possible through a laparoscopic transabdominal approach, which may explain the poorer response of type III achalasia patients to LHM compared to other subtypes 6 10.
In this report, we compared the efficacy and safety of POEM to LHM specifically for the management of type III achalasia. There were 49 POEM patients included from an international multicenter database and 26 LHM patients included from a single expert center. POEM was carried out in standard fashion, however, an extensive myotomy was performed. Clinical response was significantly more frequent in the POEM cohort (98.0 % vs 80.8 %; P = 0.01). Additionally, POEM patients had significantly shorter procedure times despite a substantially longer length of myotomy. There was no difference in length of stay. Adverse events were significantly less common with POEM.
The high clinical response rate observed in the POEM cohort was consistent with that reported in the POEM literature for all achalasia subtypes varying from 82 % to 100 % 8 14 16 28 29 30.
The median procedure times in the POEM cohort of 102 min is comparable to that reported in the International Per Oral Endoscopic Myotomy (IPOEMS) survey with a mean procedure time of 98 min 29. This result is surprising in view of the lengthy myotomy procedure reported in this type III achalasia study. The median procedure times in the LHM cohort were substantially longer than that of the POEM cohort at 264 min. However, LHM procedure times were longer than those reported in the literature, which range from a median 125 min to 160 min 22 23. A potential reason for such lengthy procedure times was likely because robotic daVinci surgery was performed as opposed to the standard transabdominal laparoscopic approach 31.
In this retrospective study, the use of ongoing PPI therapy was a surrogate for symptomatic gastroesophageal reflux disease. Regarding the presence of PPI at follow-up, there was no significant difference between POEM and LHM cohorts (38.8 % vs 46.1 %; P = 0.7). This is in keeping with studies reporting rates of reflux with LHM plus partial fundoplication of 21 % to 42 % and rates of reflux with POEM reported at 20 % to 46 % 8 32 33.
POEM had a favorable adverse event profile as compared to LHM (6 % vs 27 %; P < 0.01). There were significantly more moderate complications reported in the LHM cohort. These complications were likely the result of the transabdominal approach with ileus occurring in 3/6 and wound infection in 1/6. The longer procedure times for LHM may have also contributed to these adverse events.
There are several limitations of this study. In this retrospective study, there were many differences that existed between the groups pre-procedurally, including a greater proportion of LHM patients who had a higher Eckardt symptom stage and had undergone prior endoscopic interventions, which may have contributed to the poorer clinical response and lengthier procedure time in the LHM group, respectively. Additionally, the LHM cohort was a single-center as opposed to the multicenter POEM cohort. The diagnostic criteria used for patients (pre-2008) in the LHM group were different from the POEM cohort because of the absence of high-resolution esophageal manometry (gold standard for diagnosing type III achalasia) at that time. Furthermore, Eckardt stage as opposed to Eckardt score was used in this study as the determination of clinical symptoms was based review of the hospital medical records. However, the Eckardt stage is a validated scoring system and has been reported as the primary outcome measure in several studies 11 14 15. Last, the mean length of follow-up in the LHM cohort was substantially longer at 21.5 months compared to 8.6 months in the POEM cohort, which may have biased the clinical response in favor of POEM.
In conclusion, POEM is a logical therapeutic modality for patients with type III achalasia because it allows for a longer myotomy due to the endoscopist’s access to the esophageal body. This may have contributed to the superior clinical response compared to LHM in this study. POEM appears to be an effective and safe alternative to LHM in patients with type III achalasia. The advantages of POEM over LHM shown in this study must be verified in prospective randomized controlled trials.
Footnotes
Competing interests: M. Khashab is a consultant for Boston Scientific, Xlumena and Olympus America and has received research support from Cook Medical. H. Inoue is a founding member, equity holder, and consultant for Apollo Endosurgery. No other financial relationships relevant to this article were disclosed.
References
- 1.Bredenoord A J, Fox M, Kahrilas P J. et al. Chicago classification criteria of esophageal motility disorders defined in high resolution esophageal pressure topography. Neurogastroenterol Motil. 2012;24 01:57–65. doi: 10.1111/j.1365-2982.2011.01834.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boeckxstaens G, Zaninotto G. Achalasia and esophago-gastric junction outflow obstruction: focus on the subtypes. Neurogastroenterol Motil. 2012;24 01:27–31. doi: 10.1111/j.1365-2982.2011.01833.x. [DOI] [PubMed] [Google Scholar]
- 3.Moonen A, Boeckxstaens G. Current diagnosis and management of achalasia. J Clin Gastroenterol. 2014;48:484–490. doi: 10.1097/MCG.0000000000000137. [DOI] [PubMed] [Google Scholar]
- 4.Patti M G Pellegrini C A Arcerito M et al. Comparison of medical and minimally invasive surgical therapy for primary esophageal motility disorders Arch Surg 1995130609–615.; discussion 615–616 [DOI] [PubMed] [Google Scholar]
- 5.Salvador R, Costantini M, Zaninotto G. et al. The preoperative manometric pattern predicts the outcome of surgical treatment for esophageal achalasia. Journal of gastrointestinal surgery. J Gastrointest Surg. 2010;14:1635–1645. doi: 10.1007/s11605-010-1318-4. [DOI] [PubMed] [Google Scholar]
- 6.Rohof W O Salvador R Annese V et al. Outcomes of treatment for achalasia depend on manometric subtype Gastroenterology 2013144718–725.; quiz e713–714 [DOI] [PubMed] [Google Scholar]
- 7.Pasricha P J, Hawari R, Ahmed I. et al. Submucosal endoscopic esophageal myotomy: a novel experimental approach for the treatment of achalasia. Endoscopy. 2007;39:761–764. doi: 10.1055/s-2007-966764. [DOI] [PubMed] [Google Scholar]
- 8.Stavropoulos S N, Desilets D J, Fuchs K H. et al. Per-oral endoscopic myotomy white paper summary. Surg Endosc. 2014;28:2005–2019. doi: 10.1007/s00464-014-3630-7. [DOI] [PubMed] [Google Scholar]
- 9.Roman S, Kahrilas P J. Management of spastic disorders of the esophagus. Gastroenterol Clin North Am. 2013;42:27–43. doi: 10.1016/j.gtc.2012.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pandolfino J E, Kwiatek M A, Nealis T. et al. Achalasia: a new clinically relevant classification by high-resolution manometry. Gastroenterology. 2008;135:1526–1533. doi: 10.1053/j.gastro.2008.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gockel I, Junginger T. The value of scoring achalasia: a comparison of current systems and the impact on treatment--the surgeon's viewpoint. Am Surg. 2007;73:327–331. [PubMed] [Google Scholar]
- 12.Cotton P B, Eisen G M, Aabakken L. et al. A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc. 2010;71:446–454. doi: 10.1016/j.gie.2009.10.027. [DOI] [PubMed] [Google Scholar]
- 13.Eckardt A J, Eckardt V F. Treatment and surveillance strategies in achalasia: an update. Nat Rev Gastroenterol Hepatol. 2011;8:311–319. doi: 10.1038/nrgastro.2011.68. [DOI] [PubMed] [Google Scholar]
- 14.Swanstrom L L, Kurian A, Dunst C M. et al. Long-term outcomes of an endoscopic myotomy for achalasia: the POEM procedure. Ann Surg. 2012;256:659–667. doi: 10.1097/SLA.0b013e31826b5212. [DOI] [PubMed] [Google Scholar]
- 15.Ujiki M B Yetasook A K Zapf M et al. Peroral endoscopic myotomy: a short-term comparison with the standard laparoscopic approach Surgery 2013154893–897.; discussion 897-900 [DOI] [PubMed] [Google Scholar]
- 16.Inoue H, Minami H, Kobayashi Y. et al. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. 2010;42:265–271. doi: 10.1055/s-0029-1244080. [DOI] [PubMed] [Google Scholar]
- 17.Bortolotti M, Mari C, Lopilato C. et al. Effects of sildenafil on esophageal motility of patients with idiopathic achalasia. Gastroenterology. 2000;118:253–257. doi: 10.1016/s0016-5085(00)70206-x. [DOI] [PubMed] [Google Scholar]
- 18.Vaezi M F Pandolfino J E Vela M F ACG clinical guideline: diagnosis and management of achalasia Am J Gastroenterol 20131081238–1249.; quiz 1250 [DOI] [PubMed] [Google Scholar]
- 19.Pratap N, Kalapala R, Darisetty S. et al. Achalasia cardia subtyping by high-resolution manometry predicts the therapeutic outcome of pneumatic balloon dilatation. J Neurogastroenterol Motil. 2011;17:48–53. doi: 10.5056/jnm.2011.17.1.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Leconte M, Douard R, Gaudric M. et al. Functional results after extended myotomy for diffuse oesophageal spasm. Br J Surg. 2007;94:1113–1118. doi: 10.1002/bjs.5761. [DOI] [PubMed] [Google Scholar]
- 21.Teitelbaum E N Rajeswaran S Zhang R et al. Peroral esophageal myotomy (POEM) and laparoscopic Heller myotomy produce a similar short-term anatomic and functional effect Surgery 2013154885–891.; discussion 891–892 [DOI] [PubMed] [Google Scholar]
- 22.Hungness E S, Teitelbaum E N, Santos B F. et al. Comparison of perioperative outcomes between peroral esophageal myotomy (POEM) and laparoscopic Heller myotomy. J Gastrointest Surg. 2013;17:228–235. doi: 10.1007/s11605-012-2030-3. [DOI] [PubMed] [Google Scholar]
- 23.Bhayani N H, Kurian A A, Dunst C M. et al. A comparative study on comprehensive, objective outcomes of laparoscopic Heller myotomy with per-oral endoscopic myotomy (POEM) for achalasia. Ann Surg. 2014;259:1098–1103. doi: 10.1097/SLA.0000000000000268. [DOI] [PubMed] [Google Scholar]
- 24.Teitelbaum E N, Boris L, Arafat F O. et al. Comparison of esophagogastric junction distensibility changes during POEM and Heller myotomy using intraoperative FLIP. Surg Endosc. 2013;27:4547–4555. doi: 10.1007/s00464-013-3121-2. [DOI] [PubMed] [Google Scholar]
- 25.Shiwaku H, Inoue H, Beppu R. et al. Successful treatment of diffuse esophageal spasm by peroral endoscopic myotomy. Gastrointest Endosc. 2013;77:149–150. doi: 10.1016/j.gie.2012.02.008. [DOI] [PubMed] [Google Scholar]
- 26.Khashab M A, Saxena P, Kumbhari V. et al. Peroral endoscopic myotomy as a platform for the treatment of spastic esophageal disorders refractory to medical therapy (with video) Gastrointest Endosc. 2014;79:136–139. doi: 10.1016/j.gie.2013.08.021. [DOI] [PubMed] [Google Scholar]
- 27.Minami H, Isomoto H, Yamaguchi N. et al. Peroral endoscopic myotomy (POEM) for diffuse esophageal spasm. Endoscopy. 2014;46:E79–81. doi: 10.1055/s-0032-1309922. [DOI] [PubMed] [Google Scholar]
- 28.Ren Z, Zhong Y, Zhou P. et al. Perioperative management and treatment for complications during and after peroral endoscopic myotomy (POEM) for esophageal achalasia (EA) (data from 119 patients) Surg Endosc. 2012;26:3267–3272. doi: 10.1007/s00464-012-2336-y. [DOI] [PubMed] [Google Scholar]
- 29.Stavropoulos S N, Modayil R J, Friedel D. et al. The International Per Oral Endoscopic Myotomy Survey (IPOEMS): a snapshot of the global POEM experience. Surg Endosc. 2013;27:3322–3338. doi: 10.1007/s00464-013-2913-8. [DOI] [PubMed] [Google Scholar]
- 30.Von Renteln D Fuchs K H Fockens P et al. Peroral endoscopic myotomy for the treatment of achalasia: an international prospective multicenter study Gastroenterology 2013145309–311..e1-3 [DOI] [PubMed] [Google Scholar]
- 31.Huffmanm L C Pandalai P K Boulton B J et al. Robotic Heller myotomy: a safe operation with higher postoperative quality-of-life indices Surgery 2007142613–618.; discussion 618–620 [DOI] [PubMed] [Google Scholar]
- 32.Khajanchee Y S Kanneganti S Leatherwood A E et al. Laparoscopic Heller myotomy with Toupet fundoplication: outcomes predictors in 121 consecutive patients Arch Surg 2005140827–833.; discussion 833–824 [DOI] [PubMed] [Google Scholar]
- 33.Rawlings A, Soper N J, Oelschlager B. et al. Laparoscopic Dor vs Toupet fundoplication following Heller myotomy for achalasia: results of a multicenter, prospective, randomized-controlled trial. Surg Endosc. 2012;26:18–26. doi: 10.1007/s00464-011-1822-y. [DOI] [PubMed] [Google Scholar]


