Abstract
Objective
The objective of this study was to determine whether patients' families' violence-prevention behaviors would be affected by their primary care practitioner's use of a violence-prevention clinical intervention during the routine well-child examination.
Methods
In this cluster-randomized, controlled trial (2002–2006), 137 Pediatric Research in Office Settings practices were randomly assigned and initiated patient recruitment for either an office-based violence-prevention intervention or a control group (educational handout on literacy promotion provided). Primary caregivers of children who were aged 2 to 11 years and presented for a well-child visit were surveyed at baseline and 1 and 6 months. Practitioners were trained to (1) review a parent previsit summary regarding patient-family behavior and parental concern about media use, discipline strategies, and children's exposure to firearms, (2) counsel using brief principles of motivational interviewing, (3) identify and provide local agency resources for anger and behavior management when indicated, and (4) instruct patient-families on use of tangible tools (minute timers to monitor media time/timeouts and firearm cable locks to store firearms more safely where children live or play). Main outcomes were change over time in self-reported media use < 120 minutes per day, use of timeouts, and use of firearm cable locks.
Results
Generalized estimating equation analysis revealed a significant effect at 6 months for decreased media use and safer firearm storage. The intervention group compared with the control group showed an increase in limiting media use to < 120 minutes per day. There was no significant effect for timeout use. There was a substantial increase in storing firearms with cable locks for the intervention group versus a decrease for the control group.
Conclusions
This randomized, controlled trial demonstrated decreased media exposure and increased safe firearm storage as a result of a brief office-based violence-prevention approach.
Keywords: randomized, controlled trial, violence prevention, primary care, effect
Violence and Violence-Related behaviors in children and adolescents remain problematic in the United States.1 Homicide is the second leading cause of death for youth.2 Research suggests that normative expectations for using violence to resolve conflicts, achieve goals, and acquire status are established by early adolescence.3,4 This socialization process is multifactorial and affected by witnessing violence in the media,5–7 experiencing corporal punishment as a primary means of discipline,8–10 and adolescent gun access and ownership.11–13
Health care practitioners grapple with their role in addressing violence prevention. The majority of primary care practitioners agree that they should address this issue but doing so is not always feasible because of issues such as lack of time, inadequate training, and uncertainty of the effect.14–21 To understand better how pediatric primary care providers can facilitate a reduction in behaviors that are associated with child violence, we conducted a cluster-randomized, controlled trial in pediatric practices to test the effectiveness of a violence-prevention intervention focused on decreasing media use, increasing the use of timeouts (noncorporal forms of discipline), and storing firearms more safely for families who were not interested in removing firearms where children live and play.
This study addressed the research question, “Will patients' families' violence-prevention behaviors (media use, discipline approaches, and children's access to firearms) be affected by their primary care practitioner's use of a violence-prevention clinical intervention during the routine well-child examination?” We hypothesized that patients' families who are exposed to the intervention would improve their behaviors related to violence prevention more than those who were exposed to an attention placebo control intervention (educational handout on literacy promotion).
Methods
Practice Participants
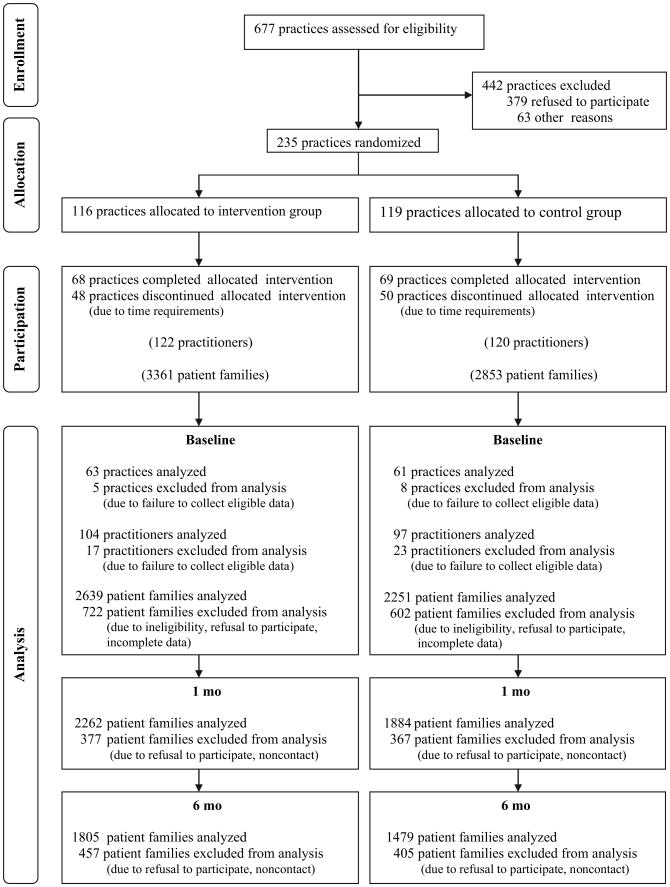
All 677 practices that belong to Pediatric Research in Office Settings (PROS), the practice-based research network of the American Academy of Pediatrics (AAP), were invited to participate. The 235 PROS practices that expressed interest were block-randomized to either the intervention (violence prevention) or the control group (usual care enhanced by a literacy promotion handout) on 2 strata: rural versus urban and service to ≥50% minority patients. These strata were chosen to ensure a diverse balanced sample. A total of 137 practices initiated the study (began enrolling patients), and 124 practices completed the study (Fig 1). Institutional review board (IRB) approval for the study was obtained from Wake Forest University School of Medicine and the AAP. Also, 30 additional local IRBs connected with the practices gave their approval (this was necessary because some sites required IRB oversight beyond that provided by Wake Forest and the AAP). The majority of participating practices were in group practice.
Figure 1.
Flow of participants through the trial.
Practitioner Participants
All PROS practitioners in participating study practices were invited to participate. Before patient enrollment, participating practitioners completed written informed consent and a survey to identify current well-child counseling practices for children aged 2 to 11 years. Practices were trained via videotape instruction in enrolling eligible patients and obtaining informed consent. Practitioners received audiotaped training to learn how to deliver either the violence-prevention intervention (see “Safety Check Violence-Prevention Intervention”) or the control educational handout on literacy promotion. Participating practitioners were mostly pediatricians (91%) with some nurse practitioners (9%).
Family Participants
Parents/primary caregivers of children who were aged 2 to 11 years and presenting for a well-child visit were eligible for the study unless they (1) were unable to complete the surveys in English or Spanish, (2) did not have a telephone number where they could be reached 1 and 6 months later, or (3) had already participated in the study with another child. On the basis of these criteria, 363 parents/primary caregivers were excluded from the study.
Study Design
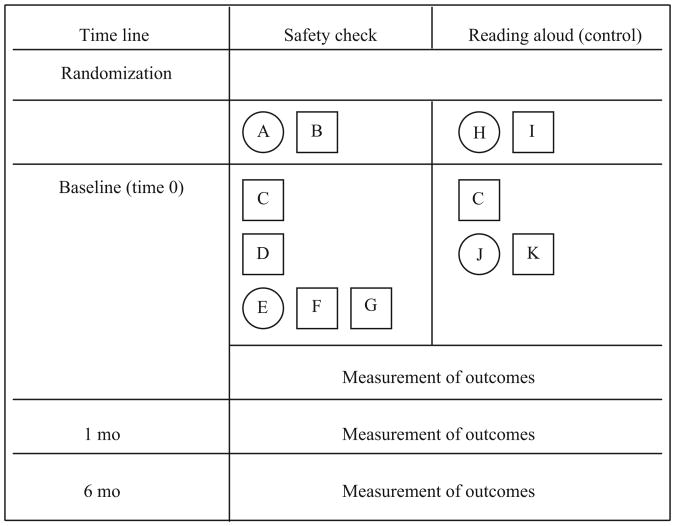
We chose a cluster-randomization design in which the unit of randomization was the pediatric practice. This design helped keep the intervention and control groups separate, thereby minimizing contamination. The components of the study process, intervention, timing, and the differences between study arms are depicted in Fig 2, in a format that follows the recently proposed graphic method for depicting randomized trials of complex interventions.22 The intervention and study materials were pilot-tested in 10 PROS practices to minimize time constraints and maximize ease of use. Providers from these practices reported that the average time of the intervention was 3 to 4 minutes. Although we did not collect data on the total time of the visit, other studies have noted that the mean well-child visit time is ∼20 minutes.23,24
Figure 2.
The SC trial compared the office-based violence-prevention approach (intervention group) with a reading-aloud passive educational program (control group). The time scale of the trial runs from top to bottom Components of the intervention delivered consecutively are shown 1 beneath the other. Components delivered concurrently are depicted side by side. Components are categorized as either objects or activities. Objects are represented by squares, reflecting their fixed nature. Activities are represented by circles, reflecting their flexibility. A, Intervention practitioners were trained to (1) complete (or have 1 of their staff complete) a worksheet that identified local agency resources for childhood aggression or anger/behavior management, (2) review the parent previsit survey regarding patient-family behavior and parental concern about child's media use, discipline strategies, and children's exposure to firearms, (3) counsel using brief principles of MI, (4) instruct patient-families to use tangible tools (minute timers to monitor media time and timeouts and firearm cable locks to store firearms more safely where children live or play), and (5) provide local agency referral (resources identified in SC component 1) when either parent or practitioner concerned at the time of the visit. B, Practitioners received SC materials: (1) local agency violence-prevention worksheets, (2) patient-family previsit surveys to assess patient-family behavior and parental concern about child's media use, firearm accessibility/storage, and discipline/childhood aggression, (3) practitioner brief MI pocket cards, (4) recommendation guides (for patient education) on media use, discipline, and firearm safety, (5) tangible tools (minute timers to monitor media time and timeouts and firearm cable locks to store firearms more safely), and (6) training videotapes for the practice (enrolling eligible patients, conducting informed consent, gathering data) and audiotapes for the practitioner (brief MI training included). Training for the practice (10-minute videotape) and training for the provider (20-minute audiotape) were considered to be a study-specific requirement. C, As part of the routine well-child visit, 8-page previsit surveys were completed by the patient-family to determine whether media use was >2 hours per day, which discipline techniques were used, and whether firearms were present where the child lives or plays and to elicit whether patient-family had any concerns about media use, discipline/childhood aggression, and firearm accessibility/storage (study-related requirement; 10–20 minutes for families to complete). D, The practitioner reviewed the previsit survey summary page and identified patient-family behaviors and concerns during the visit (intervention-related requirement;<1 minute for providers). E, During the visit, the practitioner used brief principles of MI to counsel patient-family on violence-prevention behaviors specific to media use, discipline concerns, and firearm accessibility/storage (intervention-related requirement; 2–4 minutes of provider discussion). F, The patient-family received tangible tool(s) (minute timer and/or cable gun lock) and/or referral to local agency during visit when indicated by either parental concern of excessive childhood aggression or practitioner concern. Note: In this study, practitioners offered free cable locks to parents who lived in homes with children where guns were stored. Cable locks have several advantages over other locks, such as trigger locks. First, they are easily installed on a wide variety of guns, and explaining to a parent how to use the lock properly is quick and simple and can be done with written instructions with illustrations. Second, although guns should be stored unloaded, if parents choose to have a loaded firearm in the home, then a cable lock will prevent the firing pin from making contact with a bullet or shell, thereby preventing the accidental firing of the gun (intervention-related requirement; time included with that noted in E). G, The patient-family received the Recommendation Guide, a trifold educational handout that reviews AAP recommendations on media use, discipline techniques, and firearm accessibility/storage (intervention-related requirement; time included in E). H, The control practitioners were trained (via audiotape) to provide literacy promotion recommendations and to distribute a literacy handout explaining the value of reading aloud to children. I, The practitioner received literacy promotion handouts. J, The practitioner delivered usual care regarding injury/violence prevention and used the reading handout to discuss family reading habits during the visit (control group–required component; <1 minute). K, The patient-family received a literacy promotion handout.
Safety Check Violence-Prevention Intervention
Figure 2 provides all of the details of the study and the intervention. The intervention was guided by social cognitive theory25 and emphasized changing violence-prevention behaviors through skills building for both the provider (counseling behaviors) and the patient-family (behaviors at home).
The Safety Check (SC) intervention had 5 components: (1) provider or staff in participating practices identified community-specific resources for child aggression or anger/behavior management; (2) parent completed a previsit summary page to assess behaviors and concerns about media use, discipline strategies, and children's exposure to firearms (the provider reviewed this summary page before the visit); (3) provider was trained to apply brief motivational interviewing (MI) techniques26–30 (this is an assessment of family interest and confidence in changing behavior that generates patient-centered solutions) to discuss media use, discipline strategies, and children's access to firearms when parents expressed concern or when the provider was concerned after reviewing family behaviors; (4) provider offered tangible tools (minute timers for timeouts and limiting media; cable locks [as many as were requested] to store firearms more safely) when indicated as per the previsit summary; and (5) provider offered a local agency referral (resources identified in SC component 1) when parents or practitioners were concerned about childhood aggression.
Data Collection
The data collection process was identical for both groups. Practitioners enrolled 30 consecutive patients (15 between 2 and 5 years and 15 between 6 and 11 years) who presented for well-child visits. A trained office staff member obtained written informed consent from participating families. In the waiting room, parents completed an 8-page previsit survey that ended in a summary page noting patient-family behaviors and parental concerns in the areas of media use, discipline techniques, and children's access to firearms. The self-administered questionnaire included information on (1) demographics (child age, race/ethnicity, maternal education, and family income) and (2) behaviors including media use, discipline techniques, and firearm accessibility and storage in the home. Media-related behavior questions included the following: “When this child is at home, how many hours per day does he or she watch TV/videos? Play computer games/Gameboy?” This was broken down by hours on an average weekday and average weekend day. Questions about current discipline strategies included the following: In the past month, “How often did you use timeouts or cool-down periods?” “How often have you yelled at this child?” “How often did you take away privileges (something this child enjoys)?” “How often did you spank this child?” Response categories varied on a 4-point scale from “never” to “always.” Firearm storage–related behavior questions included the following: “Are any guns stored or hidden in a place other than a locked cabinet or gun safe?” “Are all guns stored with a gunlock on them?” “Are bullets stored separate from all guns?” These responses were rated as “yes,” “no,” or “don't know.”
Immediately after the visit but before leaving the office, parents and practitioners completed a postvisit survey to record the anticipatory guidance topics (based on Bright Future recommendations31) discussed. Practitioner reports of topics discussed served as the gold standard for what occurred during the visit.
Baseline data were collected between August 2002 and December 2005 for 5286 consecutive patients, 4890 of whom met eligibility requirements. More than 80% of eligible patients across all sites participated. Patients who were eligible but not enrolled closely resembled enrolled patients with respect to age and gender.
Telephone Interviews
One and 6 months after the office visit, computer-assisted telephone interviews of families were completed by the University of South Carolina's Institute for Policy and Survey Research. One-month interviews were conducted between October 2002 and February 2006; 6-month interviews were conducted between March 2003 and July 2006. The same questions that were used to identify previsit behaviors were asked, with an additional adherence survey that assessed (1) recall of practitioner recommendations, (2) receipt of tangible tools, and (3) when received, how the tools were used.
On average, 4.9 calls were made to complete the 1-month interview and 5.5 calls were made to complete the 6-month interview. Spanish interviews composed 5.7% of the 1-month interviews and 5.0% of the 6-month interviews. Eighty-six percent of 1-month and 76% of 6-month telephone interviews were completed.
Statistical Analysis
Sample Size and Randomization
We calculated the sample size incorporating intraclass correlation coefficients (ICCs) for potential clustering effects at the level of the practitioner within the practice (ICC assumed as <0.05) and the patient within the practitioner (ICC assumed at <0.10). Randomization was performed at the practice level with computerized random numbers by the study biostatistician, who was blinded to the identity of the practices. Approximately 3% of practices were not randomized to a group but automatically assigned as a result of being covered by the same IRB or working for the same practice network. After allocation, practices were alerted to their group assignment via a letter included with the training materials. Practices were blinded to the study hypotheses.
Main Outcome Variables and Associated Analysis
In previous reports, we described the identification of aggressive children and connection to community resources identified via the community resource worksheet (SC components 1 and 5).32 Likewise, we reported on findings that were associated with baseline media, discipline, and firearm storage behaviors.33–35 In this report, we focus on the intervention effect (SC components 2, 3, and 4) for the specified behaviors over time.
For each of the 3 domains measured (media use, timeout use, and firearm storage), the primary outcome variable was dichotomized and pertained to the individual patient level. For the purposes of our analysis, we collapsed data to reflect average media use (inclusive of television, video games, computer games, and electronic handheld devices) time per day. Media use was dichotomized by applying a cutoff point of 120 minutes for average daily media use because this reflects current clinical recommendations.36 Use of timeouts was defined as reporting by using timeout either “often” or “always” (on a response scale anchored at never, rarely, sometimes, often, and always). Because some categories were used only sparingly by respondents (eg, “never”), “timeout” was dichotomized to provide more stable estimates. Firearm storage with cable lock was defined as reportedly storing all guns with a gun lock on them.
The analysis for use of timeouts was restricted only to a sample of families with children aged 2 to 5, a tool used most commonly in this age range, and the analysis of firearm storage was restricted to self-reported gun owners. Statistical analyses were performed for all participants under an intent-to-treat principle.
Unadjusted summary statistics including proportion and percentage change between groups were compared by using t tests. An adjusted analysis was used to analyze the mean response of the participants.37 To take into account the clustered structure of the data from the group randomized clinical trial design and to adjust for covariates, we adopted a generalized estimating equation (GEE) approach.38 Applying the CONSORT statement recommendations,39,40 the study was adjusted for the stratifying variables of rural versus urban practice status and practice service to ≥50% minority patients. Analysis focused on group × time interaction. The group × time interaction term evaluates whether the slopes of the 2 trend lines (examining change over time comparing the intervention group with the control group) are different beyond chance. All statistical analyses were conducted using SAS 9.0.41 All significance tests were 2-sided, and P < .05 was considered statistically significant.
Results
The final sample was derived from 124 practices (90% practice retention) in 41 states, Canada, and Puerto Rico. A total of 201 practitioners completed study participation. Participating practices did not differ from nonparticipating ones in terms of location (eg, ∼40% of each group practiced in urban areas) or type (eg, ∼50% of each group in pediatric or multispecialty group). Practitioners who declined to participate or who did not respond to recruitment efforts were statistically similar to the participating practitioners in age (median age: 50 vs 48) and gender (male: 48% vs 43%).
Table 1 indicates the baseline demographic characteristics of the practice-based patient sample. Most respondents were mothers (almost 90%), and approximately 1 quarter of all respondents represented single-parent families. Eighteen percent of our participants were Latino, and 12% were black. At baseline, patients in the intervention group were more likely to be aged 6 to 11, live in a dual-parent household, have a higher income, and have a mother with a college degree than patients in the control group.
Table 1. Demographic Characteristics of Study Participants (N = 4890).
| Domain | Intervention (N = 2639), n (%) | Control (N = 2251), n (%) |
|---|---|---|
| Age, y | ||
| 2–5 | 1373 (53.4) | 1269 (58.3) |
| 6–11 | 1200 (46.6) | 907 (41.7) |
| Male gender | 1262 (41.9) | 1110 (49.3) |
| Adults in the home | ||
| 2 parents | 1921 (74.6) | 1592 (72.2) |
| 1 parent | 648 (25.2) | 598 (27.1) |
| Other | 5 (0.2) | 14 (0.6) |
| Income | ||
| <$40 000/y | 896 (37.7) | 883 (43.8) |
| $41 000–$80 000/y | 753 (31.7) | 678 (33.6) |
| >$80000/y | 725 (30.5) | 457 (22.7) |
| Race/ethnicity | ||
| Black | 329 (13.7) | 244 (11.8) |
| Latino | 376 (15.7) | 462 (22.3) |
| White | 1497 (62.6) | 1220 (58.9) |
| Other | 189 (8.0) | 146 (7.0) |
| Maternal education | ||
| Less than high school | 229 (8.9) | 232 (10.6) |
| More than high school and less than college graduate | 1388 (54.1) | 1271 (58.0) |
| College graduate or more | 945 (36.9) | 687 (31.4) |
| Respondent | ||
| Mother | 2346 (89.2) | 2005 (89.5) |
| Father | 211 (8.0) | 163 (7.3) |
| Other | 73 (2.8) | 72 (3.2) |
Practitioners in the intervention group discussed the topics of media use (92% vs 61%), discipline (89% vs 42%), and firearm access/storage (76% vs 51%) significantly more often (all at the P < .001 level) than control group practitioners. In addition, patients in the intervention group received tangible tools often, with 86% (n = 2284) receiving minute timers and 72.1% of reported gun owners (n = 470) receiving firearm cable locks. Overall, 1 quarter (23.5%) of respondents indicated that they owned firearms.
As noted in Table 2, at baseline the intervention and control groups did not differ by media use < 120 minutes per day and frequency of timeouts for younger children aged 2 to 5 years; however, they did differ on locks reported on firearms, with the control group reporting more use than the intervention group. At baseline, the mean media use time was 2.90 hours per day (SD: 1.87 hours); approximately 1 third of families with children aged 2 to 5 years reported frequent timeout use, and approximately half of self-reported gun owners indicated use of locks on all firearms.
Table 2. Unadjusted and Adjusted Proportions and Risk Differences for the Effects of the Intervention Group Relative to the Control Group.
| Outcome | Intervention | Control | Risk Difference | OR | P | |
|---|---|---|---|---|---|---|
|
|
||||||
| % | P | |||||
| Media use <120 min/d | ||||||
| Baseline, n/N | 891/2288 | 755/1931 | ||||
| Unadjusted, % | 38.9 | 39.1 | ||||
| Adjusted, % | 34.4 | 34.1 | ||||
| 1 mo, n/N | 935/2258 | 722/1878 | ||||
| Unadjusted, % | 41.4 | 38.5 | 3.1 | .150 | 1.1 | .050 |
| Adjusted, % | 36.4 | 33.1 | 3.0 | .150 | 1.1 | .120 |
| 6 mo, n/N | 850/1907 | 642/1579 | ||||
| Unadjusted, % | 44.6 | 40.7 | 4.1 | .080 | 1.2 | .020 |
| Adjusted, % | 39.7 | 36.2 | 3.2 | .150 | 1.2 | .030 |
| Use of timeouts (children 2–5 y) | ||||||
| Baseline, n/N | 526/1338 | 501/1241 | ||||
| Unadjusted, % | 39.3 | 40.4 | ||||
| Adjusted, % | 37.7 | 38.1 | ||||
| 1 mo, n/N | 484/1165 | 438/1068 | ||||
| Unadjusted, % | 41.6 | 41.0 | 1.7 | .550 | 1.0 | .800 |
| Adjusted, % | 40.2 | 39.6 | 1.0 | .730 | 1.0 | .660 |
| 6 mo, n/N | 400/974 | 351/888 | ||||
| Unadjusted, % | 41.01 | 39.5 | 2.6 | .370 | 1.1 | .500 |
| Adjusted, % | 39.4 | 37.3 | 2.5 | .400 | 1.1 | .290 |
| Use of firearm cable lock | ||||||
| Baseline, n/N | 346/590 | 294/461 | ||||
| Unadjusted, % | 58.6 | 63.8 | ||||
| Adjusted, % | 57.8 | 65.8 | ||||
| 1 mo, n/N | 342/537 | 217/374 | ||||
| Unadjusted, % | 63.7 | 58.0 | 10.9 | .010 | 1.3 | .080 |
| Adjusted, % | 63.5 | 59.2 | 12.3 | .006 | 1.7 | .003 |
| 6 mo, n/N | 310/454 | 171/328 | ||||
| Unadjusted, % | 68.3 | 52.1 | 21.4 | <.001 | 2.0 | <.001 |
| Adjusted, % | 68.1 | 54.1 | 22.0 | <.001 | 2.0 | <.001 |
This table presents both unadjusted and adjusted differences. The adjusted model includes group, time × group interaction, practice urbanicity, and practice service to ≥50% minority populations versus the unadjusted table that examines only the group differences. Risk difference refers to difference in effect (follow-up minus baseline) between intervention and control groups. The values for ICCs at the practice level varied from 0.02 to 0.07. At the provider level, the CCs varied from 0.0004 to 0.0450. OR indicates odds ratio.
Table 2 summarizes and compares the results of the primary outcome variables of interest unadjusted and adjusted. Unadjusted analyses revealed that households in the intervention group showed an increase in limiting media use to <120 minutes per day during a 6-month period (5.7% for intervention and 1.6% for control; P = .02). Likewise, examining media as a continuous variable yields the same trend; the intervention group decreased media time by 30 minutes per day compared with the control group from baseline to 6 months later (P = .01). During the same period, there was a small but statistically insignificant positive effect (1.7%) for using timeout for the intervention group and a small negative effect (−0.90%; P = .50) for the control group. Conversely, there was a substantial increase in storing firearms with cable locks for the intervention group (9.7%) and a decrease for the control group (−11.70%; P < .001). When the model was adjusted for the stratification variables (rural versus urban status and >50% minority population served), media use reduction during 6 months had an associated odds ratio of 1.2 (P = .03), and storing firearms more safely had an odds ratio of 2.0 (P < .001). Using the information from Table 2, we derived the number needed to treat to result in the desired outcome.42 For every 26 patients for whom the SC approach is used, 1 patient will decrease his or her media use. For every 2.5 patients for whom parents report gun ownership, 1 patient-family will report use of cable locks for safer firearm storage.
We computed the multilevel ICCs43 at both the practice and the provider levels. The values for ICCs at the practice level varied from 0.02 to 0.07. At the provider level, the ICCs varied from 0.0004 to 0.0450. The differences in the magnitudes of the ICC suggest that patients of providers within the same practice tend to behave similarly. According to the GEE analysis, which takes ICCs into account and allows us to examine change at the level of the patient, for media use, the group × time interaction was not significant at 1 month (P = .12) but was significant at 6 months (P = .04). For the use of timeout, neither group (P = .67) nor group × time interaction was significant (P = .51 and P = .27 for 1 and 6 months, respectively). Storing firearms with cable locks in the intervention group revealed that the group × time interaction both was highly significant at both 1 and 6 months (P = .009 and P < .0001, respectively), showing that there was a strong and consistent effect of the intervention over time.
Discussion
In too many families and too many communities, violence is a part of daily life. Reducing violence is a pediatric and public health imperative. Factors that contribute to violence include media exposure,44–46 parenting behavior,8–10 and firearm accessibility.47–49 For example, 90% of children are now exposed to >2 hours of media per day,44–46 and 60% of media content depicts violent acts.50,51 Exposure to unsafely stored firearms is likewise a significant risk factor for childhood and adolescent injury.47,48 Among homes with children and firearms, >40% have at least 1 unlocked firearm.49 Data also indicate that substantial numbers of pediatric patients are exposed to excessive media and either live in or visit a home where a gun is present,49,52–55 which allows the setting of a provider's office to serve as an opportunity to address these issues that affect children's health.
We conducted a national, randomized, controlled trial to test the effectiveness in the real-world setting of the community pediatric practice of a violence-prevention intervention focused on decreasing media use, increasing the use of timeouts (noncorporal forms of discipline), and storing firearms more safely for families who choose to keep a firearm in their home. After 6 months, children in the intervention group were more likely to have media use restricted to <2 hours per day, as recommended by the AAP.36 Likewise, after 6 months, families in the intervention group who reported owning a firearm (1 quarter of our sample) increased their use of cable locks. Both of these effects could have a significant public health impact.
These findings combined with results from several previous studies illustrate the potential effect of wide-scale incorporation of an SC type of intervention into routine well-child care for children 2 to 11 years. The 15-year longitudinal study by Huesmann et al6 demonstrated that men who were exposed to violent television in early childhood were 3 times more likely to have been convicted of crimes than men who were not exposed, and women were 4 times more likely to have punched, beaten, or choked another adult when they were exposed to violent television in early childhood compared with unexposed women. These findings were consistent regardless of the child's initial aggression level, intellectual capabilities, and parental education level or occupation. When we consider that there are 34.8 million children aged 2 to 11 in the United States,56,57 that at least 90% of them are exposed to >2 hours of media per day,44–46 and that most media content contains violence, then >31 million children are exposed to violent media each day. Although the intervention effect of 4% seems relatively small, the large number of children who are exposed to media violence makes this finding important. If 20 million children aged 2 to 12 years are seen by primary care providers,58 then the incorporation of the SC approach could translate into 807 870 children per year who would be exposed to fewer than 2 hours of media per day and thus many fewer violent images. As the study by Robinson et al59 indicated, children who decrease media exposure are rated as being less aggressive by their peers. Extrapolating, this intervention could translate into >800 000 children per year being less aggressive and thus less likely to use violence to resolve conflict or to be charged with a crime.6
The potential public health impact of the study also is illustrated by the fact that 1.7 million children who are younger than 18 years are living with loaded and unlocked household firearms.60 In 1 study,61 storing a firearm locked was likely to result in a 73% reduction in a firearm-related injury. The study reported here led to a 21.4% increase in storing a firearm locked. Implementation of the SC approach could thus result in 361 660 families who would lock their firearms and an estimated 264 012 children who would have a reduction in firearm-related injury each year.
Our findings that a brief intervention affects firearm storage behavior differs from some previous research.62 We believe that part of the difference stems from a large sample size, allowing for adequate power. In addition, part of the effect could be attributable to the combination of components used to promote behavior change. Screening for exposure (to excess media use or firearm access) was linked to the practitioner's delivering a brief health promotion message, assessing parents' interest and confidence in changing their child's exposure, then providing a tool to facilitate concretely that behavior change. Isolated individual components (eg, brochures), given without accounting for the parent's readiness to change, may not be as effective.63 Paradoxic, giving too much information, as from an unselected list of important topics, can decrease parental recall of what was discussed during the visit.64
The study intervention did not affect parents' use of timeouts as a discipline technique. Sege et al65 demonstrated the short-term effectiveness of an office-based intervention in the initiation of timeout use among parents who had never used the technique. By contrast, in our study, ∼40% of parents already used timeout frequently. This could explain some of the difference in the study findings. Furthermore, as this study team recently reported,34 one third of study families reported feeling ineffective in their discipline techniques, timeouts included. Parents also reported using the same techniques that their parents used for them, and timeouts were not common a generation ago. Thus, the lack of effect of the intervention in the area of encouraging timeouts indicates that parents do not find this a useful technique, that it is difficult to do, and/or that our intervention did not adequately motivate or teach parents to use this behavioral technique.
Despite the success of the intervention, it is reasonable to question the extent to which practitioners would persist in using components of this intervention over time. We queried study participants regarding their continued use of intervention components immediately after study completion and 6 months later. By 6 months, tangible tool use had dropped nearly to 0 (as their supply dwindled). Approximately one third of practitioners had maintained use of the screening questionnaire, and nearly all reported incorporating brief principles of motivational interviewing into patient encounters.66 This finding is consistent with Rogers's67 work on the diffusion of innovations, whereby continuation of an innovation such as SC involves integration into ongoing routines. Motivational interviewing skills, once acquired, are readily integrated into well-child care counseling, whereas provision of tangible tools would involve a more complex series of steps to obtain and maintain an adequate supply; this would be less easily incorporated into practice.
This study has some limitations. The PROS Network has conducted office-based research for 20 years. Network practices and practitioners may not be typical of the universe of office-based pediatricians, because PROS participants may represent early adopters67 who are more likely to introduce innovation into their work. Even so, PROS practices and practitioners provide a good test of how successful initial responders to practice innovation might be, given that the patients who are seen in these practices do not differ significantly from national samples of patients.68
There are distinct components of PROS practice participation: (1) study-related requirements (completing informed consent, collecting an 8-page parent household survey for each enrolled patient) and (2) SC intervention requirements (review of 1-page patient-family behaviors/parental concerns, application of brief principles of MI, distribution of tangible tools when appropriate). Although some practitioners (10%–20%) were excluded from the analysis because of lack of ability to complete study-related requirements, we anticipated this dropout rate and included this assumption in our power calculations. These barriers would not exist if practices were not participating in an intervention trial but instead merely applying the lessons learned from the study.
We were surprised that firearm owners in the control group reported storing firearms less safely (decreased gun-lock use) over time and believe that this could indicate an initial socially desirable response that decayed with time. We recognize that data were collected via self-report, and we must contend with socially desirable reporting. Even so, in this large study, we demonstrated statistically and clinically meaningful change over time.
For noncorporal discipline strategies, we examined the change in use of timeouts as a major outcome variable. Although reduction in use of physical punishment is an important clinical outcome, few respondents indicated use of this technique frequently. Nonetheless, we did note a trend toward reduced use of “spanking” in the intervention group (2.76% at baseline, 1.43% at 6-month follow-up), with little change in the control group (2.44% baseline, 2.14% at 6 months).
Because of randomly allocating the practices and not the patients, it was not surprising to note differences in our intervention and control group patient demographics. The intervention group had a greater proportion of higher income families and fewer Latino families; however, by conducting GEE analysis, these covariates are taken into account.
We cannot examine the fidelity of intervention implementation and conducted our analysis with an intention-to-treat principle. Even with the possible practice variation, this violence-prevention office-based intervention was robust enough to demonstrate significant findings with a potential public health impact.
Conclusions
To our knowledge, this is the first national randomized, controlled trial to demonstrate the effectiveness of an office-based approach that included reviewing parent report of behaviors and concerns before the visit, use of brief principles of motivational interviewing, and provision of tangible tools to decrease media use and increase safer firearm storage in the context well-child care. The findings suggest that the current schedule of pediatric well-child visits provides a platform for effective preventive innovations. Finding the best means for translating this evidence-based approach into practice on a large scale is a logical next step.
What's Known on This Subject
Violence, a public health issue for children, is associated with factors that include excessive media use, corporal punishment, and firearm access. Medical organizations recommend that providers address this problem during the office visit; however, few studies have demonstrated an effective approach.
What This Study Adds
To our knowledge, this is the first national randomized, controlled trial to demonstrate the effectiveness of a brief office-based violence-prevention approach.
Acknowledgments
This study was supported by National Institute of Child Health and Human Development grant R01 HD 42260, the Agency for Healthcare Research and Quality, the Health Resources and Services Administration Maternal and Child Health Bureau, the Robert Wood Johnson Generalist Faculty Scholars Program, and the AAP's Friends of Children Fund. The funders had no role in the design or conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript.
We especially appreciate the efforts of the PROS practices and practitioners. The pediatric practices or individual practitioners who enrolled participants in this study are listed here according to AAP chapter: Alabama: Pediatric Care Group (Montgomery); Alaska: Anchorage Pediatric Group, LLC (Anchorage), Practice of Joy Neyhart, MD (Juneau); Arizona: Orange Grove Pediatrics (Tucson), Tanque Verde Pediatrics (Tucson); California-1: Practice of Arthur S. Dover, MD (Freedom), Sierra Park Pediatrics (Mammoth Lakes), Palo Alto Medical Foundation (Palo Alto), Pediatric and Adolescent Medical Associates of the Pacific Coast, Inc (Salinas); California-3: East County Community Clinic–Lakeside (Lakeside), Pediatric Medical Associates of Tri-City, Inc (Vista), La Jolla Pediatrics (La Jolla); California-4: Edinger Medical Group and Research Center, Inc (Fountain Valley); Colorado: Community Health Services (Commerce City), Lamar Pediatrics (Lamar), Rocky Mountain Health Centers, North (Denver); Connecticut: Mauks Koepke Medical, LLC (Danbury), Jeff Cersonsky, MD (Southbury), Pediatric Associates of Connecticut, PC (Waterbury); Florida: Atlantic Coast Pediatrics (Merritt Island), Family Health Center East and Oviedo Children's Health Center (Orlando), Heartland Pediatrics of Lake Placid (Lake Placid); Georgia: The Pediatric Center (Stone Mountain), Practice of Victor Lui, MD (Chamblee), Practice of Nandlal Chainani, MD (Ocilla), Snapfinger Woods Pediatric Associates, PC (Decatur), Gwinnett Pediatrics and Adolescent Medicine (Lawrenceville); Hawaii: Island Youth Heart and Health Center (Hilo), Children's Medical Association Inc (Aiea), Medicine Pediatrics Associates (Honolulu); Iowa: Children's Hospital Physicians (Des Moines); Illinois: Yacktman Children's Pavilion (Park Ridge), S.W. Pediatrics (Orland Park), Stroger Hospital of Cook County (Chicago), Macomb Pediatrics, SC (Macomb); Indiana: Georgetown Pediatrics (Indianapolis), Jeffersonville Pediatrics (Jeffersonville); Kansas: Ashley Clinic (Chanute); Louisiana: Carousel Pediatrics (Metairie), Shalom Clinic for Children (Natchitoches), The Baton Rouge Clinic, AMC (Baton Rouge); Massachusetts: Burlington Pediatrics (Burlington), Holyoke Pediatric Associates (Holyoke), Pediatric Associates of Norwood (Franklin), Mary Lane Pediatric Associates (Ware); Maryland: Practice of Steven E. Caplan, MD, PA (Baltimore), Dundalk Pediatric Associates (Baltimore), Practice of Ralph Brown, MD (Baltimore); Maine: Maine Coast Memorial Hospital (Ellsworth); Michigan: Pediatric and Adolescent Medicine (Bay City), Pediatric Health Care (Sterling Heights); Minnesota: Brainerd Medical Center, PA (Brainerd), Lakeview Clinic– Watertown Pediatrics (Watertown); Missouri: Children's Mercy Hospital Pediatric Care Center (Kansas City), Tenney Pediatric and Adolescent LLC (Kansas City); North Carolina: Guilford Child Health, Inc–Greensboro (Greensboro), Goldsboro Pediatrics, PA (Goldsboro), Aegis Family Health Center–Winston East Pediatrics (Winston-Salem), Guilford Child Health, Inc–High Point (High Point); North Dakota: Altru Clinic (Grand Forks); New Hampshire: Foundation Pediatrics (Nashna); New Jersey: Lourdes Pediatric Associates (Camden), Chestnut Ridge Pediatric Associates (Woodcliff Lake); New York-1: Elmwood Pediatric Group (Rochester), Lewis Pediatrics (Rochester), United Medical Associates Pediatrics (Binghamton), Wayne Medical Group (Williamson); New York-3: Pediatric Primary Care–Montefiore Medical Center (Bronx), Cardinal Mc Closkey Services (Bronx), Pediatric Practice Bronx–Lebanon Hospital (Bronx), Westchester Avenue Medical and Dental Center (Bronx), Bronx Lebanon Pediatric Clinic– Third Avenue (Bronx); New Mexico: Presbyterian Family Healthcare–Rio Bravo (Albuquerque), Santa Fe Pediatric Associate, PC (Santa Fe); Ohio: Oxford Pediatrics and Adolescents (Oxford), Pediatric Associates of Lancaster (Lancaster); Oklahoma: Pediatric and Adolescent Care, LLP (Tulsa), Oklahoma State University (OSU)–Center for Health Sciences (Tulsa); Oregon: NBMC (Coos Bay); Ontario: Richard J. MacDonald, MD (Oakville, Ontario); Pennsylvania: Pennridge Pediatric Associates (Sellersville), Buckingham Pediatrics (Buckingham), Pediatric Practices of Northeastern Pennsylvania (Honesdale), Laurel Health Center–Blossburg (Blossburg); Quebec: Clinique Enfant-Medic (Dollard des Ormeaux); Puerto Rico: Practice of Dra Ethel Lamela, MD (Isabela); Rhode Island: Northstar Pediatrics (Providence); South Carolina: Edisto Pediatrics (Walterboro), Oakbrook Pediatrics (Summerville), Palmetto Pediatrics and Adolescent Clinic, PA (Columbia), Barnwell Pediatrics, PA (Barnwell); Tennessee: ETSU Physicians and Associates (Johnson City), Pediatric Consultant, PC (Memphis), Memphis and Shelby County Pediatric Group (Memphis); Texas: The Pediatric Clinic (Greenville), Winnsboro Pediatrics (Winnsboro), Su Clinica Familiar (Harlingen), Parkland Health and Hospital System (Dallas), Child Wellness Center (Horizon City), Danette Elliott-Mullens, DO, PA (New Braunfels); Utah: University of Utah Hospitals and Clinics (Park City), Utah Valley Pediatrics, LC (American Fork), University of Utah Health Sciences Center (Salt Lake City), Willow Creek Pediatrics–Draper (Draper), IHC Health Center–Memorial (Salt Lake City); Virginia: Tidewater Pediatric Consultants, PC (Virginia Beach), Hampton Roads Pediatrics/CMG (Hampton), Alexandria Lake Ridge Pediatrics (Alexandria), Pediatrics of Arlington, PLC (Arlington), Fishing Bay Family Practice (Deltaville); Vermont: University Pediatrics, UHC Campus (Burlington), Pediatric Medicine (South Burlington), Brattleboro Primary Care (Brattleboro), University Pediatrics (Williston), Practice of Rebecca Collman, MD (Colchester), Springfield Pediatric Network (Springfield); Washington: Harbor Pediatrics (Gig Harbor), Central Washington Family Medicine (Yakima); Wisconsin: 16th Street Community Health Center (Milwaukee), Beloit Clinic SC (Beloit), Gundersen Clinic–Whitehall (Whitehall), Ministry Medical Group–Woodruff (Woodruff); West Virginia: Grant Memorial Pediatrics (Petersburg); Wyoming: Jackson Pediatrics, PC (Jackson).
Sabina B. Gesell, PhD, affiliated with Vanderbilt University Medical Center, reviewed and revised the manuscript and provided administrative assistance in her role as research coordinator. We express our appreciation for Robert H. DuRant, PhD, who contributed to the study design and implementation.
All authors met the International Committee of Medical Journal Editors requirements for authorship. All authors had full access to all of the data in the study. Dr Barkin takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors endorse the data and conclusions, have seen and approved of the final manuscript, and have taken care to ensure the integrity of the research. Dr Barkin was responsible for the whole content; conception and design; acquisition of data; analysis and interpretation of data; drafting of the manuscript; critical revision of the manuscript for important intellectual content; statistical analysis; obtaining funding; and administrative, technical, and material support. Ms Finch was responsible for the whole content; conception and design; acquisition of data; analysis and interpretation of data; drafting of the manuscript; statistical analysis; obtaining funding; and administrative, technical, and material support. Dr Ip was responsible for part of the content, analysis and interpretation of data, critical revision of the manuscript for important intellectual content, and statistical analysis. Dr Scheindlin was responsible for part of the content; conception and design; acquisition of data; drafting of the manuscript; critical revision of the manuscript for important intellectual content; obtaining funding; and administrative, technical, and material support. Dr Craig was responsible for part of the content; conception and design; acquisition of data; drafting of the manuscript; and administrative, technical, and material support. Ms Steffes was responsible for part of the content; acquisition of data; drafting of the manuscript; and administrative, technical, and material support. Ms Weiley was responsible for part of the content; acquisition of data; drafting of the manuscript; and administrative, technical, and material support. Dr Slora was responsible for the part of the content; conception and design; acquisition of data; analysis and interpretation of data; drafting of the manuscript; obtaining funding; administrative, technical, and material support; and supervision. Dr Altman was responsible for part of the content, conception and design, analysis and interpretation of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content, and supervision. Dr Wasserman was responsible for the whole content; conception and design; acquisition of data; analysis and interpretation of data; critical revision of the manuscript for important intellectual content; obtaining funding; administrative, technical, and material support; and supervision.
Abbreviations
- PROS
Pediatric Research in Office Setting
- AAP
American Academy of Pediatrics
- IRB
institutional review board
- SC
Safety Check
- MI
motivational interviewing
- ICC
intraclass correlation coefficient
- GEE
generalized estimating equation
Footnotes
The authors have indicated they have no financial relationships relevant to this article to disclose.
References
- 1.Cook P, Ludwig J. Aiming for evidence-based gun policy. J Policy Anal Manage. 2006;25(3):691–735. [Google Scholar]
- 2.Centers for Disease Control and Prevention. Deaths: Preliminary Data for 2004. [Accessed January 25, 2007];Natl Vital Stat Rep. 2006 45(19) Available at: www.cdc.gov/nchs/data/nvsr/nvsr54/nvsr54_19.pdf. [PubMed] [Google Scholar]
- 3.DuRant RH, Treiber F, Goodman E, Woods ER. Intentions to use violence among young adolescents. Pediatrics. 1996;98(6 pt 1):1104–1108. [PubMed] [Google Scholar]
- 4.Cotten NU, Resnick J, Browne DC, Martin SL, McCarraher DR, Woods J. Aggression and fighting behavior among African-American adolescents: individual and family factors. Am J Public Health. 1994;84(4):618–622. doi: 10.2105/ajph.84.4.618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.DuRant RH, Champion H, Wolfson M. The relationship between watching professional wrestling on television and engaging in date fighting among high school students. Pediatrics. 2006;118(2) doi: 10.1542/peds.2005-2098. Available at: www.pediatrics.org/cgi/content/full/118/2/e265. [DOI] [PubMed] [Google Scholar]
- 6.Huesmann LR, Moise-Titus J, Podolski CL, Eron LD. Longitudinal relations between children's exposure to TV violence and their aggressive and violent behavior in young adulthood: 1977-1992. Dev Psychol. 2003;39(2):201–221. doi: 10.1037//0012-1649.39.2.201. [DOI] [PubMed] [Google Scholar]
- 7.Christakis DA, Zimmerman FJ. Violent television viewing during preschool is associated with antisocial behavior during school age. Pediatrics. 2007;120(5):993–999. doi: 10.1542/peds.2006-3244. [DOI] [PubMed] [Google Scholar]
- 8.Holmes SJ, Robins LN. The role of parental disciplinary practices in the development of depression and alcoholism. Psychiatry. 1988;51(1):24–36. doi: 10.1080/00332747.1988.11024377. [DOI] [PubMed] [Google Scholar]
- 9.Michels S, Pianta R, Reeve R. Parent self-reports of discipline practices and child acting-out behaviors in kindergarten. Early Educ Dev. 1993;4:139–144. [Google Scholar]
- 10.Straus MA, Kantor GK. Corporal punishment of adolescents by parents: a risk factor in the epidemiology of depression, suicide, alcohol abuse, child abuse, and wife beating. Adolescence. 1994;29(115):543–561. [PubMed] [Google Scholar]
- 11.Callahan C, Rivara F. Urban high school youth and handguns: school based survey. JAMA. 1992;267(22):3038–3042. [PubMed] [Google Scholar]
- 12.Grossman DC, Reay DT, Baker SA. Self-inflicted and unintentional firearm injuries among children and adolescents: the source of the firearm. Arch Pediatr Adolesc Med. 1999;153(8):875–878. doi: 10.1001/archpedi.153.8.875. [DOI] [PubMed] [Google Scholar]
- 13.Miller M, Hemenway D. Unsupervised firearm handling by California adolescents. Inj Prev. 2004;10(3):163–168. doi: 10.1136/ip.2004.005447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.American Academy of Pediatrics, Committee on Injury and Poison Prevention. Firearm injuries affecting the pediatric population. Pediatrics. 1992;89(4 pt 2):788–790. [PubMed] [Google Scholar]
- 15.American Medical Association. Policy 145 990. Chicago, IL: American Medical Association; 1996. [Google Scholar]
- 16.Borowsky IW, Resnick MD. Adolescents and firearms: position paper of the Society for Adolescent Medicine. J Adolesc Health. 1998;23(2):117–118. doi: 10.1016/s1054-139x(98)00072-x. [DOI] [PubMed] [Google Scholar]
- 17.Olson LM, Christoffel KK, O'Connor KG. Pediatricians' experience with and attitudes toward firearms: results of a national survey. Arch Pediatr Adolesc Med. 1997;151(4):352–359. doi: 10.1001/archpedi.1997.02170410026003. [DOI] [PubMed] [Google Scholar]
- 18.Barkin S, Duan N, Fink A, Brook RH, Gelberg L. The smoking gun: do clinicians follow guidelines on firearm safety counseling? Arch Pediatr Adolesc Med. 1998;152(8):749–756. doi: 10.1001/archpedi.152.8.749. [DOI] [PubMed] [Google Scholar]
- 19.Notarianni MA, Clements PT, Tillman HJ. Caring for the future: strategies for promoting violence prevention in pediatric primary care. J Am Acad Nurse Pract. 2007;19(6):306–314. doi: 10.1111/j.1745-7599.2007.00230.x. [DOI] [PubMed] [Google Scholar]
- 20.Borowsky IW, Ireland M. National survey of pediatricians' violence prevention counseling. Arch Pediatr Adolesc Med. 1999;153(11):1170–1176. doi: 10.1001/archpedi.153.11.1170. [DOI] [PubMed] [Google Scholar]
- 21.Cheng TL, DeWitt TG, Savageau JA, O'Connor KG. Determinants of counseling in primary care pediatric practice: physician attitudes about time, money, and health issues. Arch Pediatr Adolesc Med. 1999;153(6):629–635. doi: 10.1001/archpedi.153.6.629. [DOI] [PubMed] [Google Scholar]
- 22.Perera R, Heneghan C, Yudkin P. Graphical method for depicting randomised trials of complex interventions. BMJ. 2007;334(7585):127–129. doi: 10.1136/bmj.39045.396817.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Magar NA, Dabova-Missova S, Gjerdingen DK. Effectiveness of targeted anticipatory guidance during well-child visits: a pilot trial. J Am Board Fam Med. 2006;19(5):450–458. doi: 10.3122/jabfm.19.5.450. [DOI] [PubMed] [Google Scholar]
- 24.LeBaron CW, Rodewald L, Humiston S. How much time is spent on well-child care and vaccinations? Arch Pediatr Adolesc Med. 1999;153(11):1154–1159. doi: 10.1001/archpedi.153.11.1154. [DOI] [PubMed] [Google Scholar]
- 25.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall; 1986. [Google Scholar]
- 26.Miller W, Rollnick S. Motivational Interviewing: Preparing People for Change. 2nd. New York, NY: Guilford Press; 2002. [Google Scholar]
- 27.Resnicow K, DiIorio C, Soet JE, Ernst D, Borrelli B, Hecht J. Motivational interviewing in health promotion: it sounds like something is changing. Health Psychol. 2002;21:444–451. [PubMed] [Google Scholar]
- 28.Colby SM, Monti PM, O'Leary Tevyaw T, et al. Brief motivational intervention for adolescent smokers in medical settings. Addict Behav. 2005;30(5):865–874. doi: 10.1016/j.addbeh.2004.10.001. [DOI] [PubMed] [Google Scholar]
- 29.Gance-Cleveland B. Motivational interviewing: improving patient education. J Pediatr Health Care. 2007;21(2):81–88. doi: 10.1016/j.pedhc.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 30.Poirier MK, Clark MM, Cerhan JH, Pruthi S, Geda YE, Dale LC. Teaching motivational interviewing to first-year medical students to improve counseling skills in health behavior change. Mayo Clin Proc. 2004;79(3):327–331. doi: 10.4065/79.3.327. [DOI] [PubMed] [Google Scholar]
- 31.Green M, Palfrey J, editors. Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents. 2nd., rev. Arlington, VA: National Center for Education in Maternal and Child Health; 2002. [Google Scholar]
- 32.Barkin S, Ip E, Finch S, Martin K, Steffes J, Wasserman RM. Clinician practice patterns: linking to community resources for childhood aggression. Clin Pediatr (Phila) 2006;45(8):750–756. doi: 10.1177/0009922806292812. [DOI] [PubMed] [Google Scholar]
- 33.Barkin S, Ip E, Richardson I, Klinepeter S, Finch S, Krcmar M. Parental media mediation styles for children aged 2 to 11 years. Arch Pediatr Adolesc Med. 2006;160(4):395–401. doi: 10.1001/archpedi.160.4.395. [DOI] [PubMed] [Google Scholar]
- 34.Barkin S, Scheindlin B, Ip EH, Richardson I, Finch S. Determinants of parental discipline practices: a national sample from primary care practices. Clin Pediatr (Phila) 2007;46(1):64–69. doi: 10.1177/0009922806292644. [DOI] [PubMed] [Google Scholar]
- 35.DuRant RH, Barkin S, Craig JA, Weiley VS, Ip EH, Wasserman RC. Firearm ownership and storage patterns among families with children receiving well-child care in pediatric offices. Pediatrics. 2007;119(6) doi: 10.1542/peds.2006-1485. Available at: www.pediatrics.org/cgi/content/full/119/6/e1271. [DOI] [PubMed] [Google Scholar]
- 36.American Academy of Pediatrics Committee on Public Education. Children, adolescents, and television. Pediatrics. 2001;107:423–426. doi: 10.1542/peds.107.2.423. [DOI] [PubMed] [Google Scholar]
- 37.Fitzmaurice GM, Laird NM, Ware JH. Applied Longitudinal Analysis. Hoboken, NJ: Wiley; 2004. [Google Scholar]
- 38.Diggle P, Heagerty P, Liang K, Zeger S. Analysis of Longitudinal Data. 2nd. Oxford, England: Oxford University Press; 2002. [Google Scholar]
- 39.Campbell MK, Elbourne DR, Altman DG. CONSORT statement: extension to cluster randomised trials. BMJ. 2004;328(7441):702–708. doi: 10.1136/bmj.328.7441.702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Moher D, Schulz KF, Altman D. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomized trials. JAMA. 2001;285(15):1987–1991. doi: 10.1001/jama.285.15.1987. [DOI] [PubMed] [Google Scholar]
- 41.SAS Software. Release 9.0. Cary, NC: SAS Institute, Inc; 2002. computer program. [Google Scholar]
- 42.Laupacis A, Sackett DL, Roberts RS. An assessment of clinically useful measures of the consequences of treatment. N Engl J Med. 1988;318(26):1728–1733. doi: 10.1056/NEJM198806303182605. [DOI] [PubMed] [Google Scholar]
- 43.Gulliford MC, Ukoumunne OC, Chinn S. Components of variance and intraclass correlations for the design of community-based surveys and intervention studies. Am J Epidemiol. 1999;149(9):876–883. doi: 10.1093/oxfordjournals.aje.a009904. [DOI] [PubMed] [Google Scholar]
- 44.von Feilitzen C, Carlsson U. Image, Education, Participation, Children and Media Violence. Göteborg, Sweden: UNESCO Clearinghouse; 1999. Children and Media. [Google Scholar]
- 45.Groebel J. Media violence and children. Educ Media Int. 1998;35:216–227. [Google Scholar]
- 46.Christakis DA, Zimmerman FJ, DiGiuseppe DL, McCarty CA. Early television exposure and subsequent attentional problems in children. Pediatrics. 2004;113(4):708–713. doi: 10.1542/peds.113.4.708. [DOI] [PubMed] [Google Scholar]
- 47.Johnson RM, Miller M, Vriniotis M, Azrael D, Hemenway D. Are household firearms stored less safely in homes with adolescents? Analysis of a national random sample of parents. Arch Pediatr Adolesc Med. 2006;160(8):788–792. doi: 10.1001/archpedi.160.8.788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Miller M, Azrael D, Hemenway D, Vriniotis M. Firearm storage practices and rates of unintentional firearm deaths in the United States. Accid Anal Prev. 2005;37(4):661–667. doi: 10.1016/j.aap.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 49.Schuster MA, Franke TM, Bastian AM, Sor S, Halfon N. Firearm storage patterns in US homes with children. Am J Public Health. 2000;90(4):588–594. doi: 10.2105/ajph.90.4.588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Thompson KM, Haninger K. Violence in E-rated video games. JAMA. 2001;286(5):591–598. doi: 10.1001/jama.286.5.591. [DOI] [PubMed] [Google Scholar]
- 51.Seawell M, editor. National Television Violence Study. Santa Barbara, CA: University of California; 1998. [Google Scholar]
- 52.Stennies G. Firearm storage practices and children in the home, United States, 1994. Arch Pediatr Adolesc Med. 1999;153:586–590. doi: 10.1001/archpedi.153.6.586. [DOI] [PubMed] [Google Scholar]
- 53.Cook P, Ludwig J. Guns in America: National Survey on Private Ownership and Use of Firearms: Research in Brief. Washington, DC: National Institute of Justice; 1997. [Google Scholar]
- 54.Senturia YD, Christoffel KK, Donovan M. Children's household exposure to guns: a pediatric practice-based survey. Pediatrics. 1994;93(3):469–475. [PubMed] [Google Scholar]
- 55.Senturia YD, Christoffel KK, Donovan M. Gun storage patterns in US homes with children: a pediatric practice-based survey. Pediatric Practice Research Group. Arch Pediatr Adolesc Med. 1996;150(3):265–269. doi: 10.1001/archpedi.1996.02170280035006. [DOI] [PubMed] [Google Scholar]
- 56.Hosmer D, Lemeshow S. Applied Logistic Regression. 2nd. New York, NY: Wiley; 2000. [Google Scholar]
- 57.US Census Bureau. [Accessed March 21, 2001];Overview of race and Latino origin: Census 2000 brief. Available at: www.census.gov/prod/2001pubs/cenbr01-1.pdf.
- 58.Hing E, Cherry DK, Woodwell DA. National Ambulatory Medical Care Survey: 2005 Summary. Hyattsville, MD: National Center for Health Statistics; 2006. [PubMed] [Google Scholar]
- 59.Robinson TN, Wilde ML, Navracruz LC, Haydel KF, Varady A. Effects of reducing children's television and video game use on aggressive behavior: a randomized controlled trial. Arch Pediatr Adolesc Med. 2001;155(1):17–23. doi: 10.1001/archpedi.155.1.17. [DOI] [PubMed] [Google Scholar]
- 60.Okoro CA, Nelson DE, Mercy JA, Balluz LS, Crosby AE, Mokdad AH. Prevalence of household firearms and firearm-storage practices in the 50 states and the District of Columbia: findings from the Behavioral Risk Factor Surveillance System, 2002. Pediatrics. 2005;116(3) doi: 10.1542/peds.2005-0300. Available at: www.pediatrics.org/cgi/content/full/116/3/e370. [DOI] [PubMed] [Google Scholar]
- 61.Grossman DC, Mueller BA, Riedy C, et al. Gun storage practices and risk of youth suicide and unintentional firearm injuries. JAMA. 2005;293(6):707–714. doi: 10.1001/jama.293.6.707. [DOI] [PubMed] [Google Scholar]
- 62.Sidman E, Grossman D, Koepsell T, et al. Evaluation of a community-based handgun safe-storage campaign. Pediatrics. 2005;115(6) doi: 10.1542/peds.2004-1625. Available at: www.pediatrics.org/cgi/content/full/115/6/e654. [DOI] [PubMed] [Google Scholar]
- 63.Bero LA, Grilli R, Grimshaw JM, Harvey E, Oxman AD, Thomson MA. Closing the gap between research and practice: an overview of systematic reviews of interventions to promote the implementation of research findings. The Cochrane Effective Practice and Organization of Care Review Group. BMJ. 1998;317(7156):465–468. doi: 10.1136/bmj.317.7156.465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Barkin SL, Scheindlin B, Brown C, Ip E, Finch S, Wasserman RC. Anticipatory guidance topics: are more better? Ambul Pediatr. 2005;5(6):372–376. doi: 10.1367/A04-2131R1.1. [DOI] [PubMed] [Google Scholar]
- 65.Sege RD, Perry C, Stigol L, et al. Short-term effectiveness of anticipatory guidance to reduce early childhood risks for subsequent violence. Arch Pediatr Adolesc Med. 1997;151(4):392–397. doi: 10.1001/archpedi.1997.02170410066009. [DOI] [PubMed] [Google Scholar]
- 66.Finch D, Steffes J, Weiley V, Barkin S. But will you love me tomorrow? Will clinicians sustain use of intervention components after study completion?. Presented at: Pediatric Academic Societies meetings; Toronto, Ontario, Canada. May 5–8, 2007. [Google Scholar]
- 67.Rogers EM. Diffusions of Innovations. New York, NY: Free Press; 1995. [Google Scholar]
- 68.Slora EJ, Thoma KA, Wasserman RC, Pedlow SE, Bocian AB. Patient visits to a national practice-based research network: comparing Pediatric Research in Office Settings with the National Ambulatory Medical Care Survey. Pediatrics. 2006;118(2) doi: 10.1542/peds.2005-0701. Available at: www.pediatrics.org/cgi/content/full/118/2/e228. [DOI] [PubMed] [Google Scholar]