Summary
We conducted a systematic review of studies employing telehealth interventions which focused on family caregivers’ outcomes. The Embase, CINHAL, Cochrane and PubMed databases were searched using combinations of keywords including “telehealth,” “telemedicine,” “telecare,” “telemonitoring,” “caregiver” and “family.” The initial search produced 4205 articles, of which 65 articles met the inclusion criteria. The articles included 52 experimental studies, 11 evaluation studies, one case study and one secondary analysis. Thirty-three articles focused on family caregivers of adult and older patients, while 32 articles focused on parental caregivers of paediatric patients. The technologies included video, web-based, telephone-based and telemetry/remote monitoring. Six main categories of interventions were delivered via technology: education, consultation (including decision support), psychosocial/cognitive behavioural therapy (including problem solving training), social support, data collection and monitoring, and clinical care delivery. More than 95% of the studies reported significant improvements in the caregivers’ outcomes and that caregivers were satisfied and comfortable with telehealth. The review showed that telehealth can positively affect chronic disease care, home and hospice care.
Introduction
In the past decade, the leading causes of death in the world have shifted from acute and infectious disease to chronic and degenerative diseases. The demand for both formal and informal caregivers (family caregivers) is increasing as a result of the increase in ageing population and patients with chronic illness. Family caregivers are the informal or unpaid caregivers who take care of a loved one. They play a key role in the delivery of care and support services to relatives who suffer from a chronic illness or a disabling condition that necessitates ongoing assistance with everyday tasks.1 In 2009, approximately 66 million adults, or 29% of the US adult population, were family caregivers and provided care to a relative who was ill, disabled or aged.2 The economic value for family caregivers’ unpaid services was $450 billion per year.3 Family caregivers will become the largest source of long-term care services in the US.4
While the caregiving role may be a fulfilling one, studies have shown that it can also adversely affect to the caregivers themselves, including affecting their physical and psychological health, or introducing financial, and social challenges.5–7 Approximately 17% of caregivers reported that they had increased health problems as a result of their caregiving responsibilities which in turn affected their ability to provide care.1
Technology can support caregivers and facilitate better coping. Caregivers believe that technology can help them to make caregiving more efficient, effective, safer and less stressful when delivering care to the patients.8 Although telehealth has been widely utilized for patients with chronic diseases in the past 15 years, most studies have focused on patients’ health outcomes as a result of a telehealth intervention. Little attention has been paid to the effect of telehealth interventions on family caregivers or the use of telehealth specifically to support family caregivers and address their needs. The present study aimed to systematically review evidence on the effect of telehealth applications on family caregivers.
Methods
We reviewed studies that described a telehealth-based intervention or application in any stage (design, implementation or evaluation) with a focus on family caregivers’ outcomes in all potential settings and life stages, and for any type of clinical condition. Studies were included if they used any telehealth interventions and focused on family caregivers’ outcomes. Studies were excluded if they were not published in English, did not involve human subjects or did not employ a telehealth intervention (commentary, expert opinions, study protocol, instrument, technology, framework development articles, review, exploratory, descriptive paper, and secondary analysis of an original study that did not utilize telehealth).
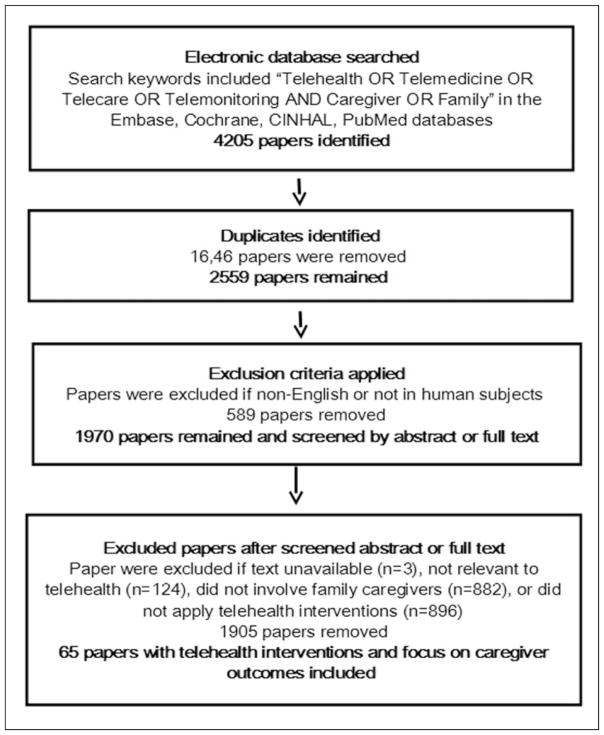
The review was conducted in May 2014 using the Embase, CINHAL, Cochrane and PubMed databases with combinations of keywords including “telehealth”, “telemedicine”, “telecare”, “telemonitoring”, “caregiver” and “family.” The initial search found 4205 articles matching the keywords. After eliminating 1646 duplicate articles, 589 studies were excluded either because of non-English publication or lack of human subjects. The articles were screened by a researcher who read either the abstracts or full text, which eliminated another 1905 articles. Articles that were not relevant to telehealth (n =124), text unavailable (n =3), did not involve family caregivers (n =882) or did not apply any telehealth interventions (n =896) were also excluded. A second researcher reviewed a randomly selected sample of 10% of all the articles by reading their abstracts in order to determine the inter-rater reliability in inclusion/exclusion of studies. There was agreement on all cases.
Information from the included articles was extracted using a standardized form. The extraction process identified from each article: the authors, published year, journal, study country, area and setting, sample and size, study design, objective, type of technology and intervention, and caregiver outcomes.
Each article was also scored for the level of evidence using the Oxford Centre for Evidence-based Medicine framework to evaluate the strength of the findings.9 This framework scores the quality of evidence on a 10-point scale, with lower scores indicating higher strength of evidence (1a: Meta-analyses; 1b: Individual randomized controlled trials, RCTs; 1c: Non-randomized controlled trials; 2a: Systematic reviews of cohort studies; 2b: Individual cohort studies; 2c: Outcomes Research; 3a: Systematic reviews of case-control studies; 3b: Individual case-control studies; 4: Case-series; 5: Expert opinions without explicit critical appraisal).
Results
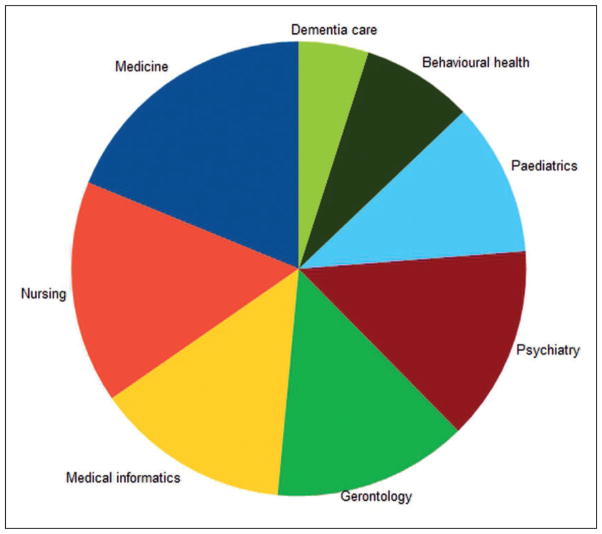
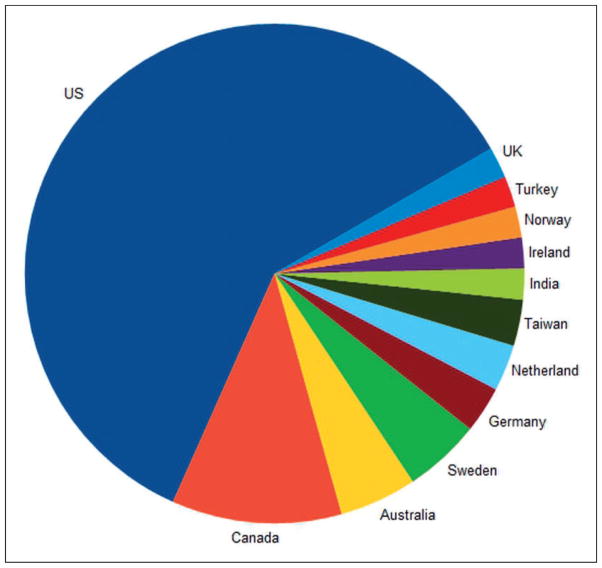
A total of 65 articles were included in the review, see Figure 1. The articles were published in 37 different journals from eight different fields. The most common field was medicine, Figure 2. The articles were from 12 different countries. The most common country was the US, Figure 3.
Figure 1.
Flow chart of study inclusions.
Figure 2.
Journal fields (n =37).
Figure 3.
Countries (n =12).
Study settings
The most common setting for studies was the home (55 or 85%). Eight studies were conducted in hospitals or clinical settings (12%), and two were at senior-living communities (3%).
Fifteen articles (23%) examined the use of telehealth specifically for rural caregivers. These studies were from the US (Ohio, Illinois, Missouri, California, Washington, Alaska, Montana, Idaho, Texas, and Oklahoma),10–16 Canada (Ontario, and British Columbia),17–20 Australia (Queensland),21–22 Sweden,23–24 and Ireland.25 They found that telehealth significantly improved the outcomes for caregivers who lived in rural areas.
Study design
The study designs were 19 RCTs (1b) (29%), 33 non-RCTs (pilot, feasibility, comparison, quasi-experimental, and pre- and post-test design) (1c) (51%), one secondary analysis (2b) (2%), 11 evaluation studies (2c) (17%) and one case study (3b) (2%). The level of evidence from these studies ranged from high (1b) to medium (3b).
Sample and sample size
Forty-one articles (63%) recruited only caregivers to test the effect of telehealth technologies, and 24 articles (37%) included both patients/providers and caregivers to measure the effect of telehealth on them.
Thirty-three articles (51%) focused on family caregivers of adult and older patients, while 32 articles (49%) focused on parental caregivers of paediatric patients. The types of patients varied, including patients with chronic disease or disability (Alzheimer’s disease, AD),26–28 dementia,11,29–33 cancer,34–36 stroke,20,37,38 heart disease,39–41 spinal cord injury,42 brain injury,17,43 chronic disease16,44–46) (38%), mental illness (schizophrenia) (3%),25,47 end-of-life care (5%),48–50 and home or community-dwelling older adults (5%).51–53
Parental caregivers were mostly of paediatric cases including new parents after childbirth (5%),23,24,54 parents of premature or low birth-weight infants (3%),55,56 of children with chronic disease18,57,58 or disability (asthma,13,59–62 renal disease,63 heart disease,64 diabetes,65,66 obesity,14 brain injury,10 hearing loss22 and autism12,67) (26%), of children with mental or behavioural disease (psychiatric disorders,15,19,68 attention-deficit hyperactivity disorder (ADHD),69,70 and oppositional or disruptive behaviour21,71,72) (12%), of children in end-of-life care (2%),73 and of preschool children (2%).74
Twenty articles included more than 100 participants (31%), 13 included 50–100 participants (20%), 25 included 10–50 participants (38%) and seven articles included less than 10 participants (11%).
Technology utilization and interventions
The telehealth technologies used in the studies included: video (videoconferencing or videophone) (40%) (Table 1, see online archive),10,13–16,18–20,22–25,30,35,42,43,48–50,54,55,57,58,62,64,69 telephone-based (phone call or text message) (31%) (Table 2, see online archive),11,17,21,26,27,32–34,37,39,44–47,60,65,66,68,72,74 web-based information (18%) (Table 3, see online archive),12,36,38,51,56,59,61,63,67,70,71,73 and telemetry/remote monitoring (electronic data collection) (11%) (Table 4, see online archive).28,29,31,40,41,52,53 Video was the most commonly-used technology.
There were six main categories of interventions delivered via technologies: education (37%), consultation (including decision support aid) (37%), psychosocial/cognitive behavioural therapy (including problem solving training) (35%), social support (23%), data collection and monitoring (20%) and clinical care delivery (11%).
Education. One of the most common uses of tele-health was to deliver education to caregivers. The most common forms of technology to deliver educational interventions to caregivers included educational telephoned-based, web-based and video technologies. For example, Smith et al.38 designed an educational website for caregivers caring for stroke patients. The components included a Professional Guide, Educational Videos, Online Chat Sessions, Email and Message Board, and a Resource Room to provide the caregivers with knowledge, resources, communication channels and social support to relieve their distress.38
Consultation. Twenty-one articles used telehealth to provide consultation services for the patients and their caregivers from home, and 14 of them (66%) were applied in paediatric case. For example, Myers et al.15 designed an interactive video-conferencing tool for children with psychiatric disorders and their parents who lived in rural areas to provide consultation and management services. Overall, the parents were satisfied with their children’s care.15
Psychosocial/cognitive behavioural therapy. Taking care of patients with dementia or children with behavioural problems requires specific care-giving skills or parenting training. Psychosocial therapy can help caregivers examine their thoughts and improve their caregiving skills. Telephone is a feasible technology to deliver distance coaching. Wilz et al. delivered therapeutic sessions via telephone for three months and the caregivers achieved complete or partial goal attainment.33 Problem-solving training is one kind of the psychosocial therapy. Caregivers face many different challenges and decision-making on difficult choices when taking care of patients. Caregivers can learn how to cope with problems and make better decisions through problem-solving training. Videoconferencing and telephone are the main technologies used to to deliver problem-solving training. In the study of Demiris et al.,49 the researchers and hospice caregivers identified the caregivers’ concerns and problems; the researchers and caregivers then practised problem-solving skills via videoconferencing to solve the problems. The caregivers reported that they were satisfied with the interventions, as well as experiencing lower level of anxiety and slightly higher quality of life (QOL).49
Social support. Long-term caregiving and parenting are physically and mentally demanding. Telehealth can serve as a platform for caregivers to obtain support from providers or exchange experiences with other caregivers. In two studies,23,24 the researchers organized regular group meetings via videoconferencing for new parents to share their caregiving experience. As a result, participants reported that they experienced more social support.23,24
Data collection and monitoring systems. Monitoring was commonly used, especially for older adults with dementia or living alone. In the study of Chou et al.,29 the units of a home monitoring system designed for dementia patients included a 24-hour response centre, personal wireless pendants, fall detectors, bed and chair occupancy sensors, and property exit sensors. The system provided round-the-clock care management and safety checks for dementia patients and their caregivers, which decreased the caregivers’ uncertainty and sense of isolation effectively.29 In addition, as older adults frequently require emergency care, telemetry can be used to support emergency care and home care for older adults. In the study of Shah et al.,53 certified telemedicine assistants used an electronic stethoscope, electrocardiograms, a high-resolution camera and a web camera to collect older adults’ data in home visits. All information collected was captured in an electronic medical record for review by the provider to facilitate efficient and effective cares.53
Clinical care delivery. Constantinescu22 conducted the Auditory-Verbal Therapy programme for children with hearing loss via weekly PC-based video-conferencing between the therapist and the parents and their children. The participating therapists and parents were satisfied with the care delivery programme.22
Outcomes
Sixty-two articles (95%) reported that caregivers had significant improvements in outcomes. The outcomes included enhanced psychological health (less anxiety, depression, stress, burden, irritation and isolation) (44%), higher satisfaction/confidence/preference/comfort/use with telehealth (38%), improved caregiving knowledge/skills/patient management (20%), higher QOL (12%), more social support/social function/need met (14%), improved coping/problem solving skills/goal attainment/decision-making (8%), better communication with providers (5%), more cost saving (5%), enhanced physical health (2%) and productivity (2%).
Three articles (5%) reported that the caregivers did not have significant improvement nor differences in satisfaction post-telehealth intervention compared to the control group.14,61,73 The main limitations were small sample size or data collection problems. Gustafson et al.61 conducted a large scale RCT with 301 parent-child dyads and reported that monthly nurse case management via telephone calls did not significantly improve the children’s asthma control and parents’ self-efficacy and information competence. Limitations noted by the authors included: the participants were not blinded and self-reported questionnaires were not reliable.61 Mulgrew et al.14 compared the effects of delivering patient-centred counselling for childhood obesity face-to-face with delivery via videoconferencing. The parents’ satisfaction was not significantly different between the groups. The authors acknowledged that the sample size (n =25) was too small to detect satisfaction between groups.14 Bradford et al.73 did not find differences in parent’s QOL between a paediatric palliative telehealth group and a control group, due to a small sample size (n =14) and the high mortality rate among children with terminal illness.73
Discussion
More than 95% of the studies in our review reported significant improvements in the caregivers’ outcomes and that caregivers were satisfied and comfortable with telehealth. Although three controlled or comparative studies did not show significant differences in outcomes or satisfaction, they indicated that the effect of telehealth was similar to conventional face-to-face care. The review showed that telehealth tools can enhance care not only to patients but also to family caregivers. As caregivers take care of a loved one, they may benefit from increased and more efficient communication with health care providers or other caregivers, as well as from access to tailored information. Approximately 60% of the papers in the review included only caregivers as participants, which suggests that more attention has been paid to caregivers’ health, QOL and satisfaction than before. The review showed that the role of telehealth in supporting family caregivers has been examined to some extent. However, further research needs to be done to examine cost-effectiveness and identify the most effective telehealth technology for caregivers.
The studies in the review came from 37 different journals, a range of disciplines and from 12 countries. The results are likely therefore to be generalizable. Of the 65 identified intervention studies, only 19 were RCTs. The others were comparative studies, quasi-experimental studies, pre- and post-test, feasibility studies, pilot studies, a case study, a secondary analysis and evaluation studies. Although many of the studies had a low level of evidence strength, their findings provide valuable considerations for the design of future experimental studies.
More than 80% of the studies delivered interventions for family caregivers at home and 23% of the studies were conducted for caregivers living in remote or rural areas and brought significant improvements in the caregivers’ psychological health and QOL. This suggests that telehealth can provide efficient care and save travel costs for caregivers of patients who need long-term care and monitoring.
The articles identified in the review covered a wide range of caregivers (ranging from paediatric to geriatric patient populations, with a broad range of diagnoses and symptom management needs). In paediatric cases, most studies focused on caregivers with children who had chronic or behavioural diseases such as asthma, renal disease, heart disease, type 1 diabetes, obesity, ADHD, oppositional and disruptive behavioural problems. Hence, education, consultation and cognitive behavioural therapy were the most common interventions for parental caregivers. They learned health education and received professional consultations and coping training remotely. In adult and geriatric cases, most of the studies were conducted with the caregivers of patients with dementia, AD, cancer, stroke, heart disease and hospice patients. Psychosocial therapy was the most common intervention to encourage caregivers to change their mentality and behaviour in caring for the patients. Also, some studies focused on older adults living in a community or alone, and telemetry and remote monitoring shared caregivers’ workloads and relieved caregivers’ stress. This demonstrates that various technologies can be tailored to support monitoring and communication in different settings involving various stakeholders.
The most common technology used was videoconferencing which allowed patients and caregivers better access to healthcare providers. Such real time interactions can support the delivery of various cognitive behavioural or educational interventions to patients and families.
The use of technology can enhance the caregiving experience and facilitate shared decision making, where patients and their families are actively involved in the care process and participate in the decision making process. In various settings such as in paediatrics or in hospices, family caregivers are called upon to make decisions or act as proxy for the patient. In such cases, the availability of tools that facilitate access to information and/or support services is important. The present review demonstrates that it can positively affect chronic disease care, home and hospice care.
Acknowledgments
This study was supported in part by the NIH National Institute for Nursing Research Grant R01NR012213.
References
- 1.Family Caregiver Alliance. Caregiver Assessment: principles, guidelines and strategies for change. See https://caregiver.org/sites/caregiver.org/files/pdfs/v1_consensus.pdf(last checked 17 September 2014)
- 2.National Alliance for Caregiving. Caregiving in the US. See http://www.caregiving.org/data/Caregiving_in_the_US_2009_full_report.pdf (last checked 17 September 2014)
- 3.Family Caregiver Alliance. Selected caregiver statistics. See http://www.caregiver.org/caregiver/jsp/content_node.jsp?nodeid=439 (last checked 4 September 2014)
- 4.Coughlin J. Estimating the impact of caregiving and employment on well-being. See http://www.nasuad.org/sites/nasuad/files/hcbs/files/196/9797/Estimating_the_Impact_of_Caregiving_and_Employment_on_Well-Being.pdf (last checked 17 September 2014)
- 5.Kuster PA, Merkle CJ. Caregiving stress, immune function, and health: implications for research with parents of medically fragile children. Issues Compr Pediatr Nurs. 2004;27:257–76. doi: 10.1080/01460860490884165. [DOI] [PubMed] [Google Scholar]
- 6.Pakenham KI, Chiu J, Bursnall S, Cannon T. Relations between social support, appraisal and coping and both positive and negative outcomes in young carers. J Health Psychol. 2007;12:89–102. doi: 10.1177/1359105307071743. [DOI] [PubMed] [Google Scholar]
- 7.Winter KH, Bouldin ED, Andresen EM. Lack of choice in caregiving decision and caregiver risk of stress, North Carolina, 2005. Prev Chronic Dis. 2010;7:A41. [PMC free article] [PubMed] [Google Scholar]
- 8.National Alliance for Caregiving. E-connected Family Caregiver: bringing caregiving into the 21st century. See http://www.caregiving.org/data/FINAL_eConnected_Family_Caregiver_Study_Jan%202011.pdf (last checked 4 September 2014)
- 9.Centre for Evidence-based Medicine. See http://www.cebm.net/?o=1025 (last checked 4 September 2014)
- 10.Antonini TN, Raj SP, Oberjohn KS, Wade SL. An online positive parenting skills programme for paediatric traumatic brain injury: feasibility and parental satisfaction. J Telemed Telecare. 2012;18:333–8. doi: 10.1258/jtt.2012.120404. [DOI] [PubMed] [Google Scholar]
- 11.Dang S, Remon N, Harris J, et al. Care coordination assisted by technology for multiethnic caregivers of persons with dementia: a pilot clinical demonstration project on caregiver burden and depression. J Telemed Telecare. 2008;14:443–7. doi: 10.1258/jtt.2008.080608. [DOI] [PubMed] [Google Scholar]
- 12.Heitzman-Powell LS, Buzhardt J, Rusinko LC, Miller TM. Formative evaluation of an ABA outreach training program for parents of children with autism in remote areas. Focus Autism Other Dev Disabl. 2014;29:23–38. [Google Scholar]
- 13.Romano MJ, Hernandez J, Gaylor A, Howard S, Knox R. Improvement in asthma symptoms and quality of life in pediatric patients through specialty care delivered via telemedicine. Telemed J E Health. 2001;7:281–6. doi: 10.1089/15305620152814683. [DOI] [PubMed] [Google Scholar]
- 14.Mulgrew KW, Shaikh U, Nettiksimmons J. Comparison of parent satisfaction with care for childhood obesity delivered face-to-face and by telemedicine. Telemed J E Health. 2011;17:383–7. doi: 10.1089/tmj.2010.0153. [DOI] [PubMed] [Google Scholar]
- 15.Myers KM, Valentine JM, Melzer SM. Child and adolescent telepsychiatry: utilization and satisfaction. Telemed J E Health. 2008;14:131–7. doi: 10.1089/tmj.2007.0035. [DOI] [PubMed] [Google Scholar]
- 16.Sorocco KH, Bratkovich KL, Wingo R, Qureshi SM, Mason PJ. Integrating care coordination home telehealth and home based primary care in rural Oklahoma: a pilot study. Psychol Serv. 2013;10:350–2. doi: 10.1037/a0032785. [DOI] [PubMed] [Google Scholar]
- 17.Brown R, Pain K, Berwald C, Hirschi P, Delehanty R, Miller H. Distance education and caregiver support groups: comparison of traditional and telephone groups. J Head Trauma Rehabil. 1999;14:257–68. doi: 10.1097/00001199-199906000-00006. [DOI] [PubMed] [Google Scholar]
- 18.Dick PT, Filler R, Pavan A. Participant satisfaction and comfort with multidisciplinary pediatric telemedicine consultations. J Pediatr Surg. 1999;34:137–41. doi: 10.1016/s0022-3468(99)90244-0. [DOI] [PubMed] [Google Scholar]
- 19.Greenberg N, Boydell KM, Volpe T. Pediatric telepsychiatry in ontario: caregiver and service provider perspectives. J Behav Health Serv Res. 2006;33:105–11. doi: 10.1007/s11414-005-9001-3. [DOI] [PubMed] [Google Scholar]
- 20.Taylor DM, Cameron JI, Walsh L, et al. Exploring the feasibility of videoconference delivery of a self-management program to rural participants with stroke. Telemed J E Health. 2009;15:646–54. doi: 10.1089/tmj.2008.0165. [DOI] [PubMed] [Google Scholar]
- 21.Connell S, Sanders MR, Markie-Dadds C. Self-directed behavioral family intervention for parents of oppositional children in rural and remote areas. Behav Modif. 1997;21:379–408. doi: 10.1177/01454455970214001. [DOI] [PubMed] [Google Scholar]
- 22.Constantinescu G. Satisfaction with telemedicine for teaching listening and spoken language to children with hearing loss. J Telemed Telecare. 2012;18:267–72. doi: 10.1258/jtt.2012.111208. [DOI] [PubMed] [Google Scholar]
- 23.Nyström K, Ohrling K. Parental support: mothers’ experience of electronic encounters. J Telemed Telecare. 2006;12:194–7. doi: 10.1258/135763306777488726. [DOI] [PubMed] [Google Scholar]
- 24.Nyström K, Ohrling K. Electronic encounters: fathers’ experiences of parental support. J Telemed Telecare. 2008;14:71–4. doi: 10.1258/jtt.2007.070605. [DOI] [PubMed] [Google Scholar]
- 25.Haley C, O’Callaghan E, Hill S, et al. Telepsychiatry and carer education for schizophrenia. Eur Psychiatry. 2011;26:302–4. doi: 10.1016/j.eurpsy.2009.12.021. [DOI] [PubMed] [Google Scholar]
- 26.Eisdorfer C, Czaja SJ, Loewenstein DA, et al. The effect of a family therapy and technology-based intervention on caregiver depression. Gerontologist. 2003;43:521–31. doi: 10.1093/geront/43.4.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mahoney DF, Tarlow BJ, Jones RN. Effects of an automated telephone support system on caregiver burden and anxiety: findings from the REACH for TLC intervention study. Gerontologist. 2003;43:556–67. doi: 10.1093/geront/43.4.556. [DOI] [PubMed] [Google Scholar]
- 28.Williams K, Arthur A, Niedens M, Moushey L, Hutfles L. In-home monitoring support for dementia caregivers: a feasibility study. Clin Nurs Res. 2013;22:139–50. doi: 10.1177/1054773812460545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chou HK, Yan SH, Lin IC, Tsai MT, Chen CC, Woung LC. A pilot study of the telecare medical support system as an intervention in dementia care: the views and experiences of primary caregivers. J Nurs Res. 2012;20:169–80. doi: 10.1097/jnr.0b013e318263d916. [DOI] [PubMed] [Google Scholar]
- 30.Czaja SJ, Loewenstein D, Schulz R, Nair SN, Perdomo D. A videophone psychosocial intervention for dementia caregivers. Am J Geriatr Psychiatry. 2013;21:1071–81. doi: 10.1016/j.jagp.2013.02.019. [DOI] [PubMed] [Google Scholar]
- 31.Engström M, Lindqvist R, Ljunggren B, Carlsson M. Relatives’ opinions of IT support, perceptions of irritations and life satisfaction in dementia care. J Telemed Telecare. 2006;12:246–50. doi: 10.1258/135763306777889127. [DOI] [PubMed] [Google Scholar]
- 32.Tremont G, Davis JD, Bishop DS, Fortinsky RH. Telephone-delivered psychosocial intervention reduces burden in dementia caregivers. Dementia (London) 2008;7:503–520. doi: 10.1177/1471301208096632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wilz G, Schinköthe D, Soellner R. Goal attainment and treatment compliance in a cognitive-behavioral telephone intervention for family caregivers of persons with dementia. GeroPsych (Bern) 2011;24:115–25. [Google Scholar]
- 34.Badger TA, Segrin C, Hepworth JT, Pasvogel A, Weihs K, Lopez AM. Telephone-delivered health education and interpersonal counseling improve quality of life for Latinas with breast cancer and their supportive partners. Psychooncology. 2013;22:1035–42. doi: 10.1002/pon.3101. [DOI] [PubMed] [Google Scholar]
- 35.Badger T, Segrin C, Pasvogel A, Lopez AM. The effect of psychosocial interventions delivered by telephone and video-phone on quality of life in early-stage breast cancer survivors and their supportive partners. J Telemed Telecare. 2013;19:260–5. doi: 10.1177/1357633X13492289. [DOI] [PubMed] [Google Scholar]
- 36.Chih MY, DuBenske LL, Hawkins RP, et al. Communicating advanced cancer patients’ symptoms via the Internet: a pooled analysis of two randomized trials examining caregiver preparedness, physical burden, and negative mood. Palliat Med. 2013;27:533–43. doi: 10.1177/0269216312457213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Grant JS, Elliott TR, Weaver M, Bartolucci AA, Giger JN. Telephone intervention with family caregivers of stroke survivors after rehabilitation. Stroke. 2002;33:2060–5. doi: 10.1161/01.str.0000020711.38824.e3. [DOI] [PubMed] [Google Scholar]
- 38.Smith GC, Egbert N, Dellman-Jenkins M, Nanna K, Palmieri PA. Reducing depression in stroke survivors and their informal caregivers: a randomized clinical trial of a Web-based intervention. Rehabil Psychol. 2012;57:196–206. doi: 10.1037/a0029587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chiang LC, Chen WC, Dai YT, Ho YL. The effectiveness of telehealth care on caregiver burden, mastery of stress, and family function among family caregivers of heart failure patients: a quasi-experimental study. Int J Nurs Stud. 2012;49:1230–42. doi: 10.1016/j.ijnurstu.2012.04.013. [DOI] [PubMed] [Google Scholar]
- 40.Keeping-Burke L, Purden M, Frasure-Smith N, Cossette S, McCarthy F, Amsel R. Bridging the transition from hospital to home: effects of the VITAL telehealth program on recovery for CABG surgery patients and their caregivers. Res Nurs Health. 2013;36:540–53. doi: 10.1002/nur.21571. [DOI] [PubMed] [Google Scholar]
- 41.Schwarz KA, Mion LC, Hudock D, Litman G. Telemonitoring of heart failure patients and their caregivers: a pilot randomized controlled trial. Prog Cardiovasc Nurs. 2008;23:18–26. doi: 10.1111/j.1751-7117.2008.06611.x. [DOI] [PubMed] [Google Scholar]
- 42.Elliott TR, Brossart D, Berry JW, Fine PR. Problem-solving training via videoconferencing for family caregivers of persons with spinal cord injuries: a randomized controlled trial. Behav Res Ther. 2008;46:1220–9. doi: 10.1016/j.brat.2008.08.004. [DOI] [PubMed] [Google Scholar]
- 43.Hauber RP, Jones ML. Telerehabilitation support for families at home caring for individuals in prolonged states of reduced consciousness. J Head Trauma Rehabil. 2002;17:535–41. doi: 10.1097/00001199-200212000-00005. [DOI] [PubMed] [Google Scholar]
- 44.Dollinger SC, Chwalisz K, Zerth EO. Tele-Help Line for Caregivers (TLC): a comprehensive telehealth intervention for rural family caregivers. Clin Gerontol. 2007;30:51–64. [Google Scholar]
- 45.Vincent C, Reinharz D, Deaudelin I, Garceau M, Talbot LR. Public telesurveillance service for frail elderly living at home, outcomes and cost evolution: a quasi experimental design with two follow-ups. Health Qual Life Outcomes. 2006;4:41. doi: 10.1186/1477-7525-4-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Griffiths PC, Davis N, Lin J, et al. Using telehealth technology to support family caregivers: description of a pilot intervention and preliminary results. Phys Occup Ther Geriatr. 2010;28:307–20. [Google Scholar]
- 47.Ozkan B, Erdem E, Demirel Ozsoy S, Zararsiz G. Effect of psychoeducation and telepsychiatric follow up given to the caregiver of the schizophrenic patient on family burden, depression and expression of emotion. Pak J Med Sci. 2013;29:1122–7. doi: 10.12669/pjms.295.2613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Demiris G, Parker Oliver D, Courtney KL, Day M. Telehospice tools for caregivers: a pilot study. Clin Gerontol. 2007;31:43–57. [Google Scholar]
- 49.Demiris G, Oliver DP, Wittenberg-Lyles E, Washington K. Use of videophones to deliver a cognitive-behavioural therapy to hospice caregivers. J Telemed Telecare. 2011;17:142–5. doi: 10.1258/jtt.2010.100503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Oliver DP, Demiris G. Comparing face-to-face and tele-health-mediated delivery of a psychoeducational intervention: a case comparison study in hospice. Telemed J E Health. 2010;16:751–3. doi: 10.1089/tmj.2010.0013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mahoney DM, Mutschler PH, Tarlow B, Liss E. Real world implementation lessons and outcomes from the Worker Interactive Networking (WIN) project: workplace-based online caregiver support and remote monitoring of elders at home. Telemed J E Health. 2008;14:224–34. doi: 10.1089/tmj.2007.0046. [DOI] [PubMed] [Google Scholar]
- 52.Lexis M, Everink I, van der Heide L, Spreeuwenberg M, Willems CG, de Witte L. Activity monitoring technology to support homecare delivery to frail and psychogeriatric elderly persons living at home alone. Technol Disabil. 2013;25:189–97. [Google Scholar]
- 53.Shah MN, Morris D, Jones CM, et al. A qualitative evaluation of a telemedicine-enhanced emergency care program for older adults. J Am Geriatr Soc. 2013;61:571–6. doi: 10.1111/jgs.12157. [DOI] [PubMed] [Google Scholar]
- 54.Lindberg I, Christensson K, Ohrling K. Parents’ experiences of using videoconferencing as a support in early discharge after childbirth. Midwifery. 2009;25:357–65. doi: 10.1016/j.midw.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 55.Gund A, Sjöqvist BA, Wigert H, Hentz E, Lindecrantz K, Bry K. A randomized controlled study about the use of eHealth in the home health care of premature infants. BMC Med Inform Decis Mak. 2013;13:22. doi: 10.1186/1472-6947-13-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gray JE, Safran C, Davis RB, et al. Baby CareLink: using the internet and telemedicine to improve care for high-risk infants. Pediatrics. 2000;106:1318–24. doi: 10.1542/peds.106.6.1318. [DOI] [PubMed] [Google Scholar]
- 57.Dick PT, Bennie J, Barden W, et al. Preference for pediatric telehome care support following hospitalization: a report on preference and satisfaction. Telemed J E Health. 2004;10(Suppl 2):45–53. [PubMed] [Google Scholar]
- 58.Young NL, Bennie J, Barden W, et al. An examination of quality of life of children and parents during their Tele-Homecare experience. Telemed J E Health. 2006;12:663–71. doi: 10.1089/tmj.2006.12.663. [DOI] [PubMed] [Google Scholar]
- 59.Chan DS, Callahan CW, Hatch-Pigott VB, et al. Internet-based home monitoring and education of children with asthma is comparable to ideal office-based care: results of a 1-year asthma in-home monitoring trial. Pediatrics. 2007;119:569–78. doi: 10.1542/peds.2006-1884. [DOI] [PubMed] [Google Scholar]
- 60.Garbutt JM, Banister C, Highstein G, et al. Telephone coaching for parents of children with asthma: impact and lessons learned. Arch Pediatr Adolesc Med. 2010;164:625–30. doi: 10.1001/archpediatrics.2010.91. [DOI] [PubMed] [Google Scholar]
- 61.Gustafson D, Wise M, Bhattacharya A, et al. The effects of combining Web-based eHealth with telephone nurse case management for pediatric asthma control: a randomized controlled trial. J Med Internet Res. 2012;14:e101. doi: 10.2196/jmir.1964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Reznik M, Ozuah PO. Asthma educational videoconferencing for parents: a case-control study. J Telemed Telecare. 2004;10(Suppl 1):83–5. doi: 10.1258/1357633042614447. [DOI] [PubMed] [Google Scholar]
- 63.Braverman J, Samsonov DV. A study of online consultations for paediatric renal patients in Russia. J Telemed Telecare. 2011;17:99–104. doi: 10.1258/jtt.2010.100410. [DOI] [PubMed] [Google Scholar]
- 64.Weatherburn G, Dowie R, Mistry H, Young T. An assessment of parental satisfaction with mode of delivery of specialist advice for paediatric cardiology: face-to-face versus videoconference. J Telemed Telecare. 2006;12(Suppl 1):57–9. doi: 10.1258/135763306777978560. [DOI] [PubMed] [Google Scholar]
- 65.Monaghan M, Hilliard ME, Cogen FR, Streisand R. Supporting parents of very young children with type 1 diabetes: results from a pilot study. Patient Educ Couns. 2011;82:271–4. doi: 10.1016/j.pec.2010.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wangberg SC, Arsand E, Andersson N. Diabetes education via mobile text messaging. J Telemed Telecare. 2006;12(Suppl 1):55–6. doi: 10.1258/135763306777978515. [DOI] [PubMed] [Google Scholar]
- 67.Kobak KA, Stone WL, Wallace E, Warren Z, Swanson A, Robson K. A web-based tutorial for parents of young children with autism: results from a pilot study. Telemed J E Health. 2011;17:804–8. doi: 10.1089/tmj.2011.0060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Scharer K, Colon E, Moneyham L, Hussey J, Tavakoli A, Shugart M. A comparison of two types of social support for mothers of mentally ill children. J Child Adolesc Psychiatr Nurs. 2009;22:86–98. doi: 10.1111/j.1744-6171.2009.00177.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Reese RJ, Slone NC, Soares N, Sprang R. Telehealth for underserved families: an evidence-based parenting program. Psychol Serv. 2012;9:320–2. doi: 10.1037/a0026193. [DOI] [PubMed] [Google Scholar]
- 70.Ossebaard HC, van Gemert-Pijnen JE, Sorbi MJ, Seydel ER. A study of a Dutch online decision aid for parents of children with ADHD. J Telemed Telecare. 2010;16:15–9. doi: 10.1258/jtt.2009.001006. [DOI] [PubMed] [Google Scholar]
- 71.Sanders MR, Baker S, Turner KM. A randomized controlled trial evaluating the efficacy of Triple P Online with parents of children with early-onset conduct problems. Behav Res Ther. 2012;50:675–84. doi: 10.1016/j.brat.2012.07.004. [DOI] [PubMed] [Google Scholar]
- 72.Kierfeld F, Ise E, Hanisch C, Görtz-Dorten A, Döpfner M. Effectiveness of telephone-assisted parent-administered behavioural family intervention for preschool children with externalizing problem behaviour: a randomized controlled trial. Eur Child Adolesc Psychiatry. 2013;22:553–65. doi: 10.1007/s00787-013-0397-7. [DOI] [PubMed] [Google Scholar]
- 73.Bradford N, Young J, Armfield NR, et al. A pilot study of the effectiveness of home teleconsultations in paediatric palliative care. J Telemed Telecare. 2012;18:438–42. doi: 10.1258/jtt.2012.gth103. [DOI] [PubMed] [Google Scholar]
- 74.Sharma R, Hebbal M, Ankola AV, Murugabupathy V. Mobile-phone text messaging (SMS) for providing oral health education to mothers of preschool children in Belgaum City. J Telemed Telecare. 2011;17:432–6. doi: 10.1258/jtt.2011.110416. [DOI] [PubMed] [Google Scholar]