Abstract
Family systems play a crucial, albeit complex, role in pediatric chronic illness. Unfortunately, very few psychosocial interventions are available to help these stressed families navigate the developmental steps of chronic illness. A new intervention (MEND) addresses the needs of these families and applies to a broad range of chronic illnesses. This article presents this family systems intervention as well as includes preliminary program evaluation data on 22 families that graduated from the program. Results show consistently strong effects across an array of psychosocial measures. Conclusions from this preliminary study suggest that families entering MEND present with high levels of stress due to the child's chronic illness, but after MEND, the level of stress and other functioning measures are comparable to those seen in healthy families, suggesting that the program offers a significant benefit to families with pediatric chronic illness.
Keywords: Chronic illness, Pediatric, Diabetes, Kidney Disease, Rheumatology, Psychosocial Intervention
Introduction
It is estimated that 13–27% of children in the United States have an existing chronic illness (Modi et al., 2012). Furthermore, the prevalence of pediatric chronic illness has increased in the last decades with 1.8% of children being diagnosed with a chronic illness in the 1960s and more than 25% in 2007 (Halfon & Newacheck, 2010). While this increased prevalence may be in part due to improved screening and early identification of chronic illness, the Center for Disease Control points out that a significant portion of children have a chronic illness and more should be done to help these children thrive in spite of their disease (Ward & Schiller, 2013).
For children with chronic illnesses, managing the necessary treatment regimen is often overwhelming and, as a result, is often mismanaged and therefore treatment adherence becomes one of the largest factors predicting an individual's health later on in their adulthood (Dashiff, Bartolucci, Wallander, & Abdullatif, 2005; Possemato, Geller, & Ouimette, 2009). It is well known that treatment adherence during these formative adolescent years is highly dependent on the parental and familial environment (Armstrong, Mackey, & Streisand, 2011; Lewandowski & Drotar, 2007). In addition, as the ill child grows older and more independent, the responsibility of the care increasingly shifts from parental control to self-management (Armstrong et al., 2011; Lewandowski & Drotar, 2007). To reduce preventable negative health outcomes later in life and instill personal treatment efficacy in the children as they mature, it is critical to achieve treatment adherence during the child's adolescent years (La Greca et al., 1995).
Achieving the developmental milestone of self-management is often tied directly to the parent–child relationship (Armstrong et al., 2011; Lewandowski & Drotar, 2007). While this parent–child relationship is critical to the chronically ill adolescent's health, few psychosocial interventions are available to help adolescents develop healthy self-management skills (Eccleston, Palermo, Fisher, & Law, 2012). Of these existing interventions, few involve the family system in the treatment, and only two apply a theoretical or conceptual lens, which are truly family systems based. These are adapted versions of Multisystemic Therapy (MST) (Ellis et al., 2005) and Brief Strategic Family Therapy (BSFT-D) (Wysocki et al., 2007). While these interventions are promising, the empirical evidence for both is limited to diabetes. Therefore, it is not clear if these interventions work as well with other chronic illnesses.
To address this need, a 21-session/7 week comprehensive intensive outpatient family therapy-based treatment model, called Mastering Each New Direction (MEND), was created. This program acknowledges the family as an interdependent system and therefore intervenes on individual, family, social, and health care system levels. MEND facilitates disease self-management through techniques based on cognitive, emotional, and social processes. MEND is grounded in family system and ecological theoretical frameworks and assumes a complex, interdependent relationship between disease activity, stress, parent– child relationships, and family system processes.
The purpose of this paper was to briefly present the MEND program inclusive of some of its underlying theories and assumptions as well as a brief overview of the program structure. We also present a case study and pilot data from this program.
Background
Treatment of Pediatric Chronic Illness
Overall, psychosocial interventions are beneficial for improving the quality of life of a chronically ill child. Three meta-analysis studies reviewing a wide range of psychosocial approaches support this conclusion (Barlow & Ellard, 2004; Beale, 2005; Eccleston et al., 2012). These reviews note that typical targeted outcomes within existing psychosocial interventions include chronic pain, cancer, diabetes, asthma, traumatic brain injuries, or eczema. Evidence-based treatment approaches to address these outcomes include cognitive behavioral therapies (CBT), family therapy, and problem solving therapy (PST), which range in their level of intervention from psycho-educational to more traditional therapy modalities. Evaluative comparisons conducted in these meta-analyses indicate that outcomes vary by interventions. For example, CBT has shown strong effects for improving a child's medical symptoms, whereas PST has been shown to reduce parental distress and improve a parent's ability to solve problems.
However, Eccleston et al. (2012), the authors of one meta-analysis, note that while it is common to include parent(s), there is little evidence to support the hypothesis that including parents within the interventions results in improved adherence in the child. In addition, across all approaches beneficial effects are seen immediately posttreatment, but are not sustained over time. In contrast to this meta-analysis, a number of research studies are beginning to show that family involvement in treatment can have immediate and sustained benefits. For example, McBroom and Enriquez (2009) examined family-centered treatments for type I diabetes. They concluded that these family-centered approaches produced effects similar to the individual-based approaches such as CBT. They also found some preliminary evidence to suggest that a family systems approach might provide a better degree of sustainability, which is also supported by empirical studies of the effects of the family system on the long-term health-related quality of life of children with chronic illnesses (Santos, Crespo, Silva, & Canavarro, 2012; Woods & McWey, 2012). In addition, a version of CBT which includes the parents more intentionally provided a more sustainable effect in comparison to CBT alone (Scholten et al., 2013). Furthermore, other family systems-based approaches for diabetes have begun to test the issue of sustainability and are showing promise in this regard (Ellis et al., 2012).
Given that the vast majority of psychosocial interventions are individual in focus and either use CBT, PST, or motivation interviewing techniques (Eccleston et al., 2012), the lack of sustainability found in the meta-analysis may be an indication of the limitation of individual-based approaches. Therefore, the key to sustainability may be tied to the inclusion of the family system.
MEND
General Overview
MEND is a biopsychosocial intensive outpatient program that provides mental health treatment for children and families with chronic illness. Its target population is children (ages 8–18) diagnosed with a chronic illness and their family members. Most often patients are referred to MEND through their specialty care physician (or team) to address treatment regimen adherence problems. MEND uses individual and family therapy as well as peer group and multifamily group processes over the course of 21 sessions (three sessions a week for 7 weeks). The desired outcome of MEND is to increase treatment adherence as well as improve disease-specific outcomes.
Targeted Outcomes of Therapy
MEND targets first and second order outcomes for patients and their families. The first order outcomes are specific to a child's disease and center around treatment adherence such as: taking prescribed medications, following testing protocols, and adhering to dietary requirements. In addition, MEND therapists collaborate with the medical team to identify relevant disease-specific biomarkers for each child's illness.
As seen in the previous meta-analysis studies, observed outcomes (treatment adherence and overall health quality) are difficult to retain over time and a systems perspective would suggest that other second order factors mediate these outcomes. MEND assumes that these factors exist in several ecological levels of influence. Because chronic illness places stress on the family and the child, MEND places significant focus on understanding and addressing patterns of coping and stress. Often families referred to MEND have developed maladaptive stress and coping patterns that prevent the family and the child from adapting to the developmental life span of the illness. We will discuss these concepts in detail below, but for now we would note that a significant outcome for MEND families is the presence of adaptive illness-related stress response patterns. As we will demonstrate below, stress response patterns are not simply experienced by the individual (child), but are interdependent with the parent–child relationship, larger family system, and peer networks. Because of this, MEND works to produce sustainable improvement in stress responses in the micro- and mesosystem levels while also targeting treatment adherence and disease activity.
Principles of MEND
In an effort to shift maladaptive systemic patterns of coping and responding to stress within the family and ultimately provide improved treatment adherence and health outcomes, MEND employs three principles: the ecological evaluation of influences on a child's stress response pattern, introception, and shifting patterns through shifting meaning. Similar to other biopsychosocial approaches to chronic illness (for example, the Biobehavoiral Family Model; Wood, 1993; Wood, Klebba, & Miller, 2000), MEND is also grounded in both family systems assumptions such as earlier works utilizing structural family therapy (Minuchin et al., 1975; Minuchin & Fishman, 1981) as well as an ecological framework.
Ecological
MEND intervenes at multiple ecological levels. Specifically the program utilizes individual and family therapy sessions as well as peer and multifamily groups to directly intervene in the micro- and mesosystem levels. For example, in addition to working with the entire family system, MEND therapists maintain constant contact with the child's medical team throughout all stages of the program. Also, the therapist interacts with the child's school system toward the end of treatment (when patients are typically healthy enough to reengage in school).
MEND also values a heavy focus on the child's peer mesosystem. While some of the promising psychosocial interventions for chronic illness are ecological in nature (such as MST), they often overlook the crucial role of the child's peer mesosystem in leveraging adaptive stress response patterns. For example, chronically ill children are more likely to miss school or be homeschooled (Baldwin-Gracey & Ward, 2012; Kaffenberger, 2006). We know that children learn a great deal about stress and coping from peer relationships (Gifford-Smith & Brownell, 2003). As chronically ill children are limited in their exposure to peers, MEND purposely integrates group therapy with other chronically ill children. In addition, MEND has an open enrollment policy so that more senior participants play the role of “mentor” and help teach and intervene with the new participants. This allows for the chronically ill child to practice age-appropriate peer relationships, but more importantly the more tenured child receives important boosts to their self-confidence and self-efficacy when they assume a leadership or teaching role for newer children. This is important as a sense self-efficacy has been noted as a key factor in producing lifelong self-management skills within chronically ill children (Armstrong et al., 2011). There is also evidence that multifamily groups can be useful in working with chronic illness (Lopez-Larrosa, 2013). Specifically multifamily groups have been seen to increase a sense of hope and optimism within the family, which offers a better family environment for the chronically ill patient. MEND incorporates multifamily groups into the program to help support the child's family, but also to provide the family with opportunities for learning from each other as well as challenging each other.
MEND also addresses the microsystem of the child through an evaluation of cognitive functioning. This is an important distinction because it is known that both parents and children often feel overwhelmed by the treatment regime (Armstrong et al., 2011; Lewandowski & Drotar, 2007; Miller & Drotar, 2007), which likely leads to reduced treatment adherence. MEND posits that stress not only limits adherence, but also may interfere with the child's or parent's cognition, which prevents them from comprehending the complex treatment regimen. In other words, it is not that the child is consciously choosing to reject the treatment regimen, but rather emotional processes take over and impair the child's comprehension and memory regarding the specific details of their treatment regimen. Because of this, MEND assumes that a change in adherence will not occur until the stress response patterns within the meso- and microsystem levels are shifted and the brain has ample time to recover the necessary cognitive processes. Thus, MEND does not expect the biological effects of adherence to set in until the final phase of the program.
Introception
A central focus of MEND includes the patient's mind–body connection. The mind–body connection is the interconnected process by which the patient learns how their emotional and thought processes contribute to their physical health. The primary mind–body connection focused on in MEND is the connection between psychological, cognitive, and emotional processes with the Sympathetic Nervous System (SNS). The SNS is the system which triggers the biochemical and physiological changes brought about by a stress response.
MEND assumes that it is important for patients to be intune with their own bodies as patients will have significant disconnects from a body they may feel has failed them. This disconnect is often experienced in the chronically ill child both physically and emotionally. Physically the child has learned to distance himself from the pain of the illness, the discomfort of the treatment, and the uncomfortable side effects. Emotionally too the child may distance himself from illness meanings, which are laden with guilt and shame. This disconnect often results in patients being unaware of their physiological and emotional experiences.
The process of attending to the internal responses of one's body is termed introception. In other words, introception involves looking inward to learn how to identify emotional processes which inform MEND patients of their overall well-being. Paying attention to the physical cues of the body, such as pain, tenseness, or changes in respiration, MEND patients begin to align information from their emotional state and their physiological experience and move closer toward a congruent state. Once MEND patients learn the ability to accurately read their body's responses to emotional processes, they can take that information and better understand and manage their mind– body connection, thus maintaining mind–body congruence. Therefore, congruence refers to the accurate outward behavioral responses to internal emotional processes. MEND assumes that when patients practice introception and learn to become congruent, change begins to be facilitated internally which allows for larger mesosystem level systemic changes.
Shifting patterns through shifting meaning
The foundation of MEND not only incorporates an ecological lens and introspection, it also includes language and illness narratives as agents of change. The role of language changes depending on the phase of the program. In the beginning, the therapist assesses the language used by the patient and family members. Learning the patient and family member's language assists in better understanding the family's perceived meanings given to the illness. In addition, certain maladaptive meanings of illness can facilitate maladaptive coping strategies, which can cause further stress and negative disease responses (Petrie, Jago, & Devcich, 2007). Therefore, the meaning the family gives to the illness can play a powerful role in a child's behavior. Once the therapist has elicited the family's illness story, the therapist can assess whether this meaning facilitates adaptive or maladaptive stress patterns within the family system. More often in families referred to MEND, the illness story supports a stress response pattern that has become maladaptive in that it perpetuates a pattern within the family that leads to further stress and decreased treatment regimen adherence by the child.
While illness stories carry a unique contextual component for every family, there are often common elements, or themes, across families with pediatric chronic illness. Because of this phenomenon of shared themes, MEND is able to develop a common language between patients and family members, which is used in the mesosystem to promote change. A key feature in MEND is that the therapist teaches this common language within the groups, which helps the children and the families quickly identify and challenge stress response patterns. For example, a therapist will often use the term “congruent”. As we noted before, this term is used to illuminate the lack of connection between physical and emotional cues expressed by patients. An example of a noncongruent moment would be a child verbalizing an emotion of happiness, while their nonverbal cues show stress or even frustration. At first, a therapist might point out this situation to the child and state that their words and the body are “incongruent”. Later on the child's peers will have learned this language and will challenge each other by noting in group that “Sara is not being congruent”. In a similar way the word “burdens” carries a special meaning in the groups. Many chronically ill children within MEND understand their illness story in ways that place burdensome levels of responsibility or even shame onto them as the identified patient. In this case, the chronically ill child might feel that they are solely responsible for the stressors within the family such as: family relational stress, financial stress, parent feeling overwhelmed, and sibling feeling like they receive less attention than the chronically ill child. All of these are common stories for MEND kids and the “burden” of this emotional response can, and often does, fuel maladaptive stress response patterns within the child and the larger family system. Having a shared language about this within the larger MEND group gives the children a medium to interact with each other which they may have never had before due to their limitations in developing age-appropriate peer relationships.
These three principles of MEND guide the conceptual framework of MEND and are continually addressed through multiple interventions and through all four stages of MEND.
Schedule, Daily Routine, and Phases of MEND
As MEND is located at an academic medical center, it conforms to state standards and guidelines for structuring an intensive outpatient program. Therefore, MEND consists of three sessions a week for a total of 7 weeks (21 sessions). Each session is 3 hours in duration. Each day begins with 8 to 10 children gathering in a group for a check-in time. During this first hour, the children discuss their progress in managing appropriate stress responses, their current level of stress, and disease-specific treatment adherence goals.
Following this check-in time, the children move on to a group therapy process. Given the open enrollment of the program, the curriculum cycles through topics and activities that are relevant across all of the four phases. Although each day has a prescribed curriculum, all sessions contain activities focused on managing stress and identifying maladaptive stress response patterns using a combination of talk and art therapy techniques. While the children are in their peer group session with one of the therapists, parents are engaged in education and process groups with one of the other therapists from the MEND team. In the final hour of the session, the children and the parents come together for multifamily groups.
Outside of the regular 3-hour sessions, MEND patients may participate in additional individual and family sessions. The necessity of this action is based on whether the therapist has requested a case consult with the physician, if the parents have requested this action, or if the therapy team has concerns about the child or family not meeting the needed developmental milestones, which are outlined below.
While each session follows this structure, the overall course of treatment is guided by the following four phases: Orientation and Assessment, Introception and Congruence, Meaning and Expression, and Generalization (see Table 1 below).
Table 1. Overview of MEND Phases of Treatment.
| Phases | Steps | Interventions | Goal |
|---|---|---|---|
| Phase I | Orient to MEND, assess child learn child's language | ||
| Orientation and Assessment |
|
|
|
| Phase II | Introspect and create congruence for child and family | ||
| Introception and Congruence |
|
|
|
| Phase III | Solidify positive illness meaning and expression of change | ||
| Meaning child and family and Expression |
|
|
|
| Phase IV | Generalize | ||
| Generalization |
|
|
The four phases are very much in parallel to other adolescent family therapy approaches such as Functional Family Therapy (Sexton & Alexander, 2003), MST (Sheidow, Henggeler, & Schoenwald, 2003), BSFT-D (Szapocznik, Hervis, & Schwartz, 2003), and MultiDimensional Family Therapy (Liddle, 2002). According to Blow and Distelberg (2006), in their summary of these four evidence-based models, a common trajectory across each of these models is a process beginning with an expanded family system engagement phase, then an ecological assessment, followed by a process of creating a shared view of the problem, and finally, a phase of maintaining the change and generalization ends the program.
Phase I: Orientation, assessment, and language
The first phase of MEND begins with a process of orienting the family to the program as well as engaging the family in treatment (Blow & Distelberg, 2006; Sprenkle & Blow, 2004). In the first session, the therapist familiarizes the child and the family with the rules and expectations of the program as well as the therapeutic format including the peer relationships that guide the treatment. While much of the work is under the guise of orientation, the goal is on building acceptance for the possibility of change. Through this trust building and engagement, a relationship is built between the child, family, therapist, and peers which in turn becomes the fulcrum for change throughout the program.
Once a therapist assists the child and family in developing a sense of trust and expectancy for change, the therapist will begin assessing the family system at multiple ecological levels. As a therapist progresses through an assessment process with the family, he is also charged with learning the language and meaning given to the illness for each family system. This is essential to the therapeutic treatment as each individual child has a different illness story. The therapist must fully understand this story before attempting to change the associated stress patterns. This process of learning the language is meant not only to provide an assessment, but also to elicit a sense of connection and shared understanding between the therapist and the family system.
Phase II: Introception and congruence
The goal of the second phase is to encourage an understanding of stress response patterns within the child and family and create a shared view of the problem (Blow & Distelberg, 2006). In this phase, much of the work is informative and focused on helping the patient identify stress response patterns within themselves and their family system. Ultimately, this phase seeks to generate what MEND calls psychogenic congruence. Simply put, in this phase the therapist begins assessing the family system to determine whether the child's outward behavioral responses to stress are congruent with the emotional processes within the child. When incongruence exists, the therapist will probe for this disconnect and encourage the child to modify their language in such a way that their emotional, verbal, and psychological responses to stress match their physiological responses. For example, a child may state that their illness does not impact them at all, but will show signs of anxiety or discomfort through tapping their foot or a look of sadness across their face. The therapist would inquire about this incongruence and encourage more accurate expression.
Before leaving this phase, MEND therapists continually evaluate whether the family is maintaining the changes they began to experience or if they are reverting back into the maladaptive stress response processes that they exhibited before entering this phase. Reverting behavior is indicative of the child still holding onto negative meanings related to his illness and subsequent identity. A key sign that the child is ready for the next phase of MEND is that she experiences accurate and consistent congruence and begins to adopt new meanings to both her illness and the stress she experiences.
Phase III: Meaning and expression of change
The third phase contains two specific goals: solidifying the change and assessing for sustainability. In regard to the first goal, the therapist shifts the focus from teaching and learning the child's stress response patterning to considering the effects of the change on the larger family system as well as the larger context in which the family exists. More specifically, the therapist will reevaluate whether the family system is able to respond in new ways toward the child when the child seeks to have his emotional needs met. It is important for families at this point to support the development of healthy needs-directed behavior and self-management skills even if such behavior is initially beyond what is considered acceptable for the family system. For example, although a child in the past may have exaggerated symptoms to get his mother's attention, the child would now be encouraged to directly ask for one-on-one time with his mother. Hence, if the therapist is able to help prepare the family for alterations in their child's process and the child receives consistent acceptance in their growth the change is likely to continue.
Once the therapist is confident that the family system has realigned to the new stress coping processes with members having changed their meaning about the illness, she will shift to explore for evidence of sustainability. Testing sustainability involves the therapist intentionally stressing the system to determine whether new or additional stress can be experienced by the child and family without the system reverting back to old maladaptive beliefs, meanings, or stress response patterns. In this case, the therapist hopes to see that new skills are mastered not only by the child but also by the family system; specifically, that maladaptive meanings, identified in phase I, have changed and the family becomes more supportive of the child's continued age-appropriate developmental progression. In addition, when the therapist, through the process of sustainability testing, sees that the individual and their system are using the new skills acquired in phase II consistently over time, the therapist can feel confident that the system will be able to successfully move forward and meet challenges after the end of the MEND program.
This testing of sustainability is done multiple times in this phase, as well as in multiple settings. A common example of this process involves reintroducing previously identified topics (within phase I) charged with emotional energy. In this case, the child may have been dealing with depression and in phase I was asked to paint pictures that illustrate these emotions. Here in phase III, the therapist may ask the child to share the painting and its meaning with her parents or in a multifamily setting. In doing this the therapist creates an environment with greater levels of intensity. In this exercise, the therapist would be looking for the child to maintain a congruent position, demonstrating new skills learned in phase II, while reporting to the family or group. Also, the therapist is also watching to see that the family does not reengage in old maladaptive stress response patterns during these exercises. Although the presentation is important, the true test comes from the therapist increasing the intensity in this exercise by interjecting challenges. Specifically the child will report meanings and emotions of the picture, but from this newly learned congruent state which they acquired in phase II. Here, the therapist will ask questions or pose challenges that tempt the child to revert back to maladaptive response to emotional stress. Specifically, the therapist will interject stress response patterns identified in phases I. The goal is to see that the child is able to stay with the stress and not revert back to the old stress response patterns or return to old belief systems (such as believing that they are a burden).
If this child and the family are able to sustain the change in the face of these challenges, the therapist will turn up the heat even farther by challenging the child's ability to reengage in school and other similar activities. For example, in a multifamily group or in a family therapy session, the child might report their desire and confidence to return to school and meet new friends and be academically successful. At this stage, the therapist may present as confused and question the child as to how they believe they can be successful in these new goals when they are broken or sick. The therapist will even express significant concerns that the child might not be ready to take on such a significant step. In this test, the therapist is watching to see how fast the child is able to respond to this challenge without reverting back to maladaptive stress patterns or negative belief systems. The quicker the child and the family support the goal of returning to school, the more solidified the change has become.
It is important to note that this process of testing the sustainability by stressing the system is not done in a harsh combative manner. It is experienced as intense and stressful. But this intensity is allowed due to the nature of the therapeutic relationship which has been developed over phases I and II.
Phase IV: Change generalization and reintegration/Mastery and maintenance
The final phase of MEND is the process of generalization. Much like the four evidence-based approaches to adolescent family therapy (Blow & Distelberg, 2006), MEND therapists spend the last phase of the program facilitating generalization. During this phase, the family acknowledges that they have made a significant change, but that at times of greater stress they may fall back on old maladaptive processes. To safely observe and somewhat guide these inevitable situations, the therapist will help the child reintegrate into their academic and social environments. This is a time where (if the child has been previously out of school due to his illness) the therapist will work with the family, the medical team, and the school to reengage the child back in school. This is often a significant stressor for the family and a key indicator that the family either is or is not ready to conclude the program.
Finally, the MEND therapist creates a discharge plan with the family. While each plan is unique for the child and their chronic illness, common elements include: a time of reflecting with the family about the progress they made; reminding them to expect future stress; and preparing them to identify, acknowledge, and respond to these events.
Case Example
While we gave illustrations throughout this article, to further illustrate the principles and phases of MEND we provide the following case example.
Maria was a 13-year-old postheart transplant patient. She came to MEND because she had not been taking her medication regularly, which was concerning for her physicians and her mother. This resulted in Maria having weekly trips to the emergency room and an increased threat of the rejection of her transplant. Maria's mother knew Maria needed to begin taking ownership of her medication adherence and was frustrated because her daughter would often go to bed without taking her medications. Maria's mother had tried everything to help her daughter remember to take her medications, but was now at a loss as to what to do.
During the peer group session in phase I Maria was encouraged to share her experiences about her medical and family history. In this exercise, the therapist noted that her expressed stories were somewhat exaggerated (based on previous knowledge of this disease-specific treatment protocol and based on conversations with Maria's family and medical team). The therapist hypothesized that Maria's stories were attempts to gain acceptance from her peers, but they were also poorly executed for her age. In this case, Maria's ability to read and accurately respond to social cues was somewhat delayed, and in addition they were void of emotional content. To test Maria's incongruent state as well as aid in the language learning process, the therapist asked Maria to paint any image she wanted that represented her story. Maria chose to paint an image from her story that involved her lying in a hospital bed while her family was in separate rooms of the house. In another room sat her two younger siblings crying because they were left alone as mom and dad fought in another room. The therapist reviewed the content of the intervention with Maria and asked her to tell the story of the image. The therapist used these three pieces of the picture to teach Maria the construct of congruence. As Maria began to express the emotions associated with each image her affect began to change, her eyes dropped to the floor, and the cadence of her story slowed as her voice got softer; as this happened, the therapist called Maria's attention to this change. Then, in the peer group session, Maria presented this picture and began to cry as she expressed to the group that it is her fault her parents fight because she was sick and the illness burdened her family. This event brought to light the role of the burden Maria felt and gave the beginnings of insight into Maria's, as well as her family's, stress response pattern.
Over additional sessions, the therapist worked with Maria to help her identify and explicitly express the emotions she felt about her illness and her family. During this process, Maria reported “I'm mad. My mom doesn't tuck me in because she's busy with my sisters”. This was a significant step forward for Maria as she was finally able to express an emotion and have this expression be congruent with her physiological expressions. The therapist commended Maria and processed her anger with her in the peer group. At first, Maria expressed anger for her sisters (as they were getting attention from mom and not Maria), but through processing this story Maria was able to realize that she was not angry at her sisters, rather she was frustrated that she wanted her mother to bring her medications at night and tuck her in. However, Maria did not feel that she could ask for this attention because she already felt as though she was a significant burden to her mother and her family. The therapist continued to process this situation with Maria and explored times when Maria felt connected with her mother. Maria reported that she felt close to her mother when they were together waiting in the emergency room. Soon it became apparent that Maria's stress response pattern was triggered by a sense of limited time spent with her mother. To resolve this emotional stress, Maria would do something to specifically highlight her illness and therefore force her mother to drop everything and attend to her.
With this understanding, the therapist explored how this pattern within Maria interacted with the larger ecological system. While processing this situation with Maria and her family it was clear that the family was stressed financially; both Maria's mother and father had to work full-time jobs while also having to set aside time for Maria's multiple trips to the ER. In addition, Maria noted that she felt like her illness was a burden on the family and she felt like her need for attention from her mother was just one more burden she brought to the family. Therefore, Maria found a way to ask for attention from mom without feeling the guilt of directly asking for this attention.
This insight was a huge shift for the family. They were able to quickly see the maladaptive qualities of this situation and, with the help of their therapist, worked to develop more adaptive processes, such as explicating stating new rules for how Maria could seek attention from her mother. But maintaining this shift was not easy and Maria often reverted back to her old pattern. In phase II, the therapist (as well as the other families within the multifamily group) helped support Maria's mother in maintaining the new rules they had implemented and over time Maria was able to fully participate in the agreed upon patterns of relating.
At this point, in phase III, the therapist stressed the system to see if the change was indeed sustainable. Specifically, the therapist stressed the system by setting up a session between Maria and her family. In this session, Maria was asked to present and explain a recent event where she felt her family did not support or meet her needs. This was a previous stressor identified by the therapist in phase I. Here, the therapist was testing whether the family would employ the strategies they learned in phase II when he tried to tempt Maria back into her old beliefs and meanings about being a burden and being isolated from her family. Maria explained in detail a recent example where she felt disconnected from the family. Maria was able to express significant emotions from this experience and the family was able to support her even in the face of the therapist offering challenges for Maria to revert back to feeling like a burden. Through this exercise, Maria allowed herself to express her honest needs and fears, while family members processed how they could work together to help support Maria in more adaptable ways. The family then employed a number of new strategies based on this experience and they were able to adjust to these new patterns which included Maria being more explicit about her needs and the family responding to these needs, as well as Maria learning to cope with her emotions when the family was not able to immediately meet these needs. The therapist took the family through a number of similar stressors in the multifamily groups as well as in the peer groups. After successful completion of these tests, the therapist transitioned Maria and her family on to phase IV.
In the fourth and final phase, the therapist facilitated conversations with Maria and her family about where the family began and how far they had come. In this process, Maria was able to express what she had learned that will help her maintain healthy behaviors in the future. In addition, situations that may come up were discussed, specifically how Maria would handle going back to school and how she would recognize whether she was asking for her needs to be met directly or indirectly. These conversations helped Maria and her family to acknowledge the skills they had learned and prepared them for situations that will likely arise in the future. Before leaving MEND Maria had been consistent in taking her medications, she had not been back to the emergency room, and was already beginning school.
Preliminary Evaluation
MEND has collected evaluation and outcomes data that are regularly collected from program participants as part of ongoing program monitoring. The following section presents the evaluation of 22 chronically ill children who were referred to MEND by their primary care or specialty physician. All referrals were made due to the children's limited adherence to their treatment regimen. To monitor changes over time from entry to MEND to graduation, we used the systemic and multidimensional health-related quality of life (HRQOL) measures for the child as well as the family system.
Methodology
Sample
We utilized a retrospective design, reviewing existing chart data from MEND program attendees collected in the natural clinical setting. The sample included 22 adolescents diagnosed with a chronic illness. Patients were referred to the program by their primary or specialty physician if they determined that the patient was not adhering to their defined treatment regimen. Table 2 below summarizes the demographic information of this sample.
Table 2. Summary of Sample Demographics.
| Freq | Percentage | |
|---|---|---|
| Disease type | ||
| Type I diabetes | 6 | 27 |
| Chronic kidney disease | 3 | 14 |
| Rheumatoid arthritis | 1 | 4.5 |
| Cancer | 2 | 9.1 |
| Other | 10 | 46 |
| Marital status | ||
| Married | 13 | 59.1 |
| Single | 2 | 9.1 |
| Divorced/Seperated | 7 | 31.8 |
| Gender | ||
| Male | 9 | 41 |
| Female | 13 | 59 |
| Ethnicity | ||
| Black | 4 | 19 |
| Hispanic | 5 | 24 |
| White | 11 | 52 |
| Other | 1 | 5 |
| Education level | ||
| High school or less | 4 | 18.1 |
| Some college | 12 | 54.5 |
| College | 5 | 22.7 |
| Graduate degree | 1 | 4.5 |
| Funding | ||
| Insured | 11 | 50 |
| Scholarship | 11 | 50 |
|
| ||
| Mean (SD) | Median (Interquartile range) | |
|
| ||
| Child's age | 14.3 (2.6) | 15 (13–16) |
| TX duration (No. of sessions) | 24.5 (5.1) | 24 (20–28) |
| N = 22 | ||
Patients with a wide range of chronic illnesses participated in MEND including type I diabetes, chronic kidney disease, and rheumatoid arthritis. While quite diverse (19% Black and 24% Hispanic), most participants self-reported as white (52%). The average patient's age was approximately 14 years at the start of the program with 75% of the sample ranging from 13 to 16. (The youngest individual was 8 years old while the oldest was 18.) In addition, the majority of families consisted of two married parents. These families were of moderate to lower SES background with the majority having less than a college degree (72.6%). Furthermore, to help families cover the cost of the program, half of the families qualified to receive funding for MEND through a need-based internal scholarship program. To qualify for this program the family must demonstrate that they do not have current access to private insurance and have a family adjusted annual income that is less than 200% of the area adjusted poverty line.
As noted above, the program is not considered “completed” until the disease-specific biomarkers indicate an improved treatment adherence. Also, all participants and their parent(s)/legal guardian(s) attended all of the MEND sessions. While the MEND program calls for a protocol of 21 sessions/7 weeks, the MEND team can increase the treatment length when needed. In this regard, the average number of sessions in this sample was 24 with 75% of the sample ranging in duration from 20 to 28 sessions. The longest duration was 36 sessions.
Measures
As part of standard treatment evaluation, a battery of surveys was administered to participating children and parents at the first and last days of treatment. Measures included a demographic survey (e.g., diagnosis, ethnicity, age) as well as questions that measure the impact of the chronic illness on the child and family. For example, one question asked “over the last 30 days, how many days has your child missed school due to their illness?” Similar questions were asked about the number of days the child was unable to play due to their illness, how many days the parents had to recruit an additional caregiver to help out at home, and how many days the illness interfered with the parents' ability to work.
In addition, participants completed the Pediatric Health-Related Quality of Life (Peds-QL 4.0 generic core scales) survey. The PedsQL (Varni, Seid, & Kurtin, 2001) is designed to measure pediatric HRQOL across a number of domains. These domains are Physical, Emotional, Social, and School functioning. PedsQL also includes an overall (or total) score as well as a total psychosocial score. Domains are assessed by the child as well as the parent as a corresponding proxy report. The items for each form are essentially identical. The instructions ask how much of a problem a series of issues were during the past month. A five-point response scale is used (0 = never a problem, 4 = almost always a problem). Items are reverse scored and linearly transformed to a 0–100 scale (0 = 100, 1 = 75, 2 = 50, 3 = 25, and 4 = 0), so that higher scores indicate better HRQOL. Scale scores are computed as the sum of the items divided by the number of items answered. Each of the subscales has been shown to have high reliability and validity (Varni et al., 2003). A precursor to the PedsQL 4.0 (PedQL 3.0) also contained a cognitive functioning scale and was included in this study as well.
We also analyzed a PedsQL subscale that measures the impact of the chronic illness on the family system. The PedsQL Family Impact Module (Varni, Sherman, Burwinkle, Dickinson, & Dixon, 2004) operates the same way as the generic core scales for scoring, but is specific to the effect of the illness on the family itself. This module offers seven subscales (Physical, Emotional, Social, Cognitive, Communication, Worry, Daily Activity, and Friendship Impacts). Each scale has high published reliability (α > 0.70). This scale is somewhat newer than the Core scales of the PedsQL and therefore has more limited use in the literature in comparison to the extensive use of the Core scales.
Procedures
The study utilized the data on the sample of 22 patients and their families. To evaluate whether MEND provided significant improvement in the HRQL domains for the child and the family, the measures were grouped into the “Impact on the Child” and the “Impact on the Family System”. For the impact on the child, the analysis utilized repeated measures t tests on the subscales and total score for the PedsQL 4.0 Generic Core measures. In addition, we included child impact items available in the MEND intake packet (e.g., number of days of school missed and the number of days the child was too sick to play). We then identified available normative data from a healthy population to determine whether the impact on the child after MEND was statistically similar to the healthy population scores on the PedsQL 4.0. To understand if the program had a significant effect on the family system, we utilized the same process as above, except with the Family Impact Module no comparable normative studies were accessible for use in this study.
Results
Research Question 1: MEND Reduces the Negative Impact of the Chronic Illness on the Child
Table 3 summarizes the baseline and posttreatment measures for each subscale with the associated t-test statistics. This table also compares the measures to a normative population of healthy families. The program significantly improved the overall HRQOL of the child. Both the Child Report and the Parent Proxy Report showed a significant improvement in the TOTAL HRQOL (Child: MD = 19.1, SE = 5.2 [8.2, 30.0] r2 = .39. Parent: MD = 22.3, SE = 3.9 [14.1, 30.4] r2 = .6). Also, each subscale measure showed a medium to strong effect.
Table 3. Summary of MEND Baseline and PostTreatment as well as a Comparison of the MEND Graduates to a Healthy Population.
| Healthy Sampleb | |||||||
|---|---|---|---|---|---|---|---|
|
|
|||||||
| Measure | Baseline M (SD) | Post M (SD) | T-Valuea | r-Sq | M (SE) | T1-M | T2-M |
| Child report | |||||||
| Physical functioning | 67.5 (25.9) | 82.6 (22.1) | 2.66* | 0.25 | 89.39 (12.64) | −21.9† | −6.8 |
| Emotional functioning | 53.0 (22.6) | 80.3 (23.9) | 4.26† | 0.46 | 80.88 (17.84) | −27.9† | −58 |
| Social functioning | 71.8 (23.0) | 83.7 (23.0) | 2.11* | 0.18 | 87.11 (15.74) | −15.3** | −3.4 |
| School functioning | 50.3 (18.5) | 72.4 (24.4) | 4.41† | 0.48 | 81.68 (16.04) | −31.4† | −9.3 |
| Cognitive functioning | 55.6 (28.5) | 73.9 (21.0) | 3.58† | 0.38 | n.a. | – | – |
| Psychosocial functioning | 58.4 (18.5) | 78.8 (22.5) | 3.87† | 0.42 | 83.24 (13.60) | −24.9† | −4.5 |
| Total HRQOL | 60.6 (18.3) | 79.8 (21.7) | 3.64† | 0.39 | 85.34 (12.04) | −24.7† | −5.6 |
| Parent report | |||||||
| Physical functioning | 58.6 (24.4) | 76.7 (20.1) | 3.29† | 0.34 | 87.21 (17.80) | −28.6† | −10.5* |
| Emotional functioning | 38.3 (19.6) | 63.9 (17.4) | 5.32† | 0.57 | 81.98 (16.50) | −43.6† | −18.0† |
| Social functioning | 54.2 (18.1) | 77.3 (18.9) | 5.00† | 0.54 | 85.19 (18.37) | −31.0† | −7.9 |
| School functioning | 48.3 (21.9) | 70.5 (18.9) | 4.28† | 0.47 | 78.59 (18.73) | −30.3† | −8.1 |
| Cognitive functioning | 55.6 (28.5) | 73.9 (21.0) | 3.58† | 0.38 | n.a. | – | – |
| Psychosocial functioning | 46.9 (16.4) | 70.6 (15.8) | 6.05† | 0.64 | 81.95 (14.90) | −35.0† | −11.4** |
| Total HRQOL | 49.8 (16.4) | 72.1 (15.0) | 5.67† | 0.60 | 83.79 (14.42) | −34.0† | − 11.7** |
| Days of school missed (over 30 days) | 11.83 (10.9) | 2.33 (4.13) | 4.28† | 0.50 | |||
| Days too sick to play | 5.47 (8.1) | 0.71 (1.65) | 2.47** | 0.26 | |||
Note. HRQOL = health-related quality of life.
Repeated measures t test.
Health sample from Varni et al. (2008). Between sample comparison estimated by one sample t test.
p < .05,
p < .01,
p < .001.
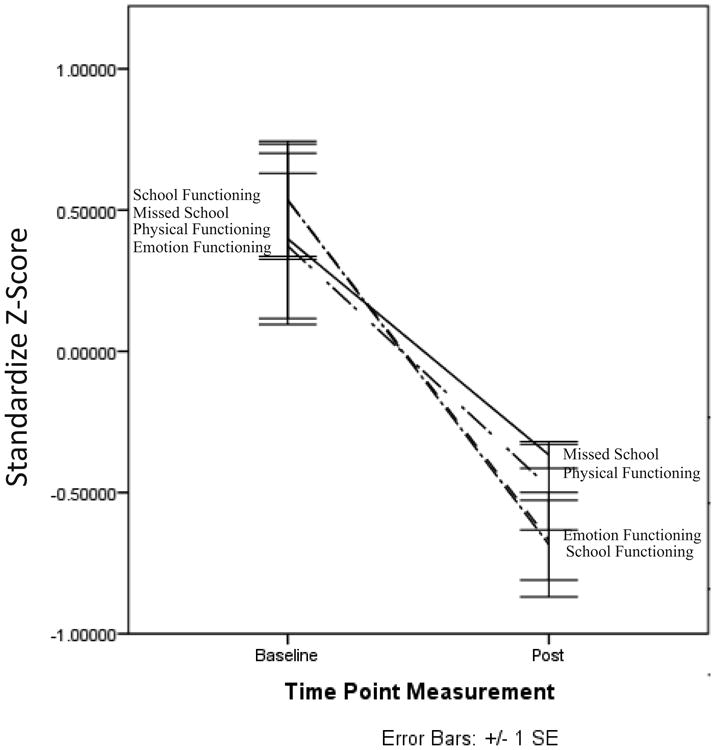
Furthermore, the number of school days missed in a month and the number of days the child was too sick to play also significantly improved. On average, a child will miss approximately 11 days of school in a month before entering the program and approximately 2 days at the end of the program (MD = −9.50, SE = 2.2 [4.8, 14.2] r2 = .50). Thus, the program reduced the number of missed school days in a month by 9.5 days or an 80% reduction. Similarly the number of days the child was too sick to play was reduced by 87% with children missing 5.47 days per months before MEND and .71 days after MEND (MD = −4.76, SE = 1.93 [.67, 8.86] r2 = .26). Figure 1 below visually displays MEND's effect on the impact of the illness on the child (note: values were standardized to z-scores and the PedsQL scores were reversed to show a decrease in the impact of each domain so that the additional items and the PedsQL items could be displayed in the same conceptual direction and within the same scale).
Figure 1. Decreased Child Impact Baseline and PostTest.
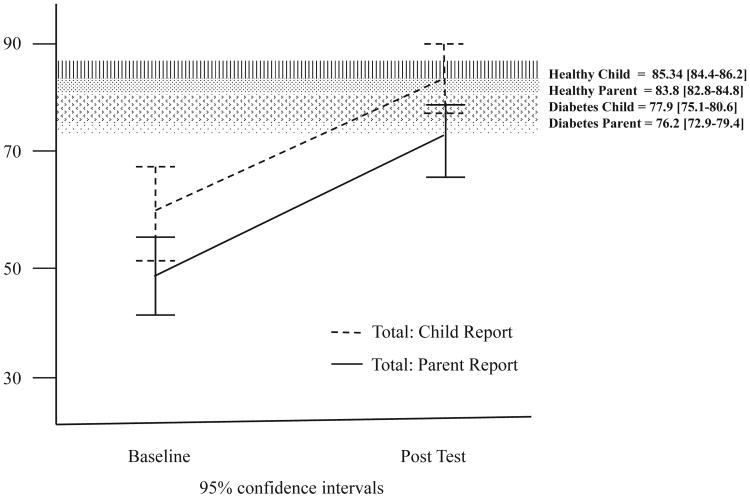
Next, we compared the PedsQL values at baseline and posttreatment to a normative “healthy” population to determine whether the improvements seen in the program elevated the children to scores typically seen in “healthy” children. To accomplish this, we accessed the data from one of the most recent and largest PedsQL normative studies (Varni, Bryant, Limbers, Wilson, & Burwinkle, 2008) with data on 695 children and 834 parents. The authors report that this population was a normative population from the United States and without any known health limitations. Table 3 above shows the means and standard errors of each PedsQL subscale as well as the mean difference between this population and the baseline and posttreatment measures of the MEND patients. Results from this comparison are mixed between the child report and the parent proxy report.
For the child report, the MEND patients began the program with HRQOL scores that, as expected, were significantly lower than those of the healthy normative comparison population. Notably, however at the completion of the program, MEND patients had scores similar to healthy children. (Child Total Score T1: MD = −24.7, 95% CI [−32.8, − 16.6]: T2: MD = −1.2, 95% CI [−15.3, 4.00]). While similar pretest results were seen for the parent's report, with parents reporting a significantly lower level of HRQOL prior to MEND (Parent Total Score T1: MD = −33.96, 95% CI [−41.2, −26.71]) improvements at program completion were significant, but did not improve, overall, to a comparable level to that reported by a parent with a healthy child (Parent Total Score T2: MD = −11.69, 95% CI [−18.32, −5.058]). Instead most of the posttreatment scores were lower than the healthy sample except in the case of Social and School functioning. In these two measures, the MEND kids did conclude MEND with comparable social and school functioning. To explore this issue further, we also compared our parental scores to another population within the same study (Varni et al., 2008), in this case, a population diagnosed with type I diabetes. In this comparison, the MEND Parents reported a posttreatment improvement that was equal to the diabetes report (Parent Total Score T2: MD = 4.5, 95% CI [−11.15, 2.12]). In other words, MEND parents report significantly lower levels of HRQOL before MEND, but at program end, report a significant increase, which happens to be equal to normative level seen in type I diabetes. In the case of social and school functioning, the scores were higher than the type I diabetes normative values and comparable to a healthy population.
Overall, the children and the parents in MEND tend to report a HRQOL that is lower (worse) than that of a healthy population and a type I diabetes population before entering MEND. After completing MEND, the children report scores that are equal to the healthy population and higher than the type I diabetes population. Parents, on the other hand, reported HRQOL improvements which equaled a normative type I diabetes population, but slightly lower than a healthy population. Therefore, both the parents and the child reported a significant increase in the child's HRQOL. These findings are visually displayed in Figure 2 below.
Figure 2. Improved Child Impact in Comparison to a Healthy and Diabetes Population.
Research Question 2: MEND Reduces the Negative Impact of the Chronic Illness on the Family
While the primary objective of MEND is to improve the child's functioning, the theoretical grounding of the program also hypothesizes that the child's outcomes are interdependent with the family's functioning and therefore MEND will reduce the negative effects of chronic illness within the family. As can be seen in Table 4, this family impact hypothesis was fully supported. MEND families reported a significant improvement in their physical, emotional, social, and cognitive functioning. They also reported a significant improvement in communication, a reduction in worry, improved family relationships, and a significant reduction in the impact of the child's illness on their daily activities. Overall, the total negative impact on the family as a whole was reduced significantly (MD = 15.3, SE = 3.0, 95% CI [−21.6, −9.1], r2 = .55).
Table 4. Summary of Family Impact Measures and Comparison to Outpatient Sample.
| Measure | Baseline M (SD) | Post M (SD) | T-Valuea | r-Sq |
|---|---|---|---|---|
| Family impact | ||||
| Physical functioning | 53.9 (25.1) | 73.5 (18.7) | 4.24† | 0.46 |
| Emotional functioning | 50.8 (21.4) | 71.6 (19.2) | 4.51† | 0.49 |
| Social functioning | 60.6 (23.2) | 78.1 (20.6) | 3.92† | 0.42 |
| Cognitive functioning | 67.8 (27.8) | 80.9 (21.0) | 2.59** | 0.24 |
| Communication | 62.6 (21.8) | 79.2 (20.9) | 3.08** | 0.31 |
| Worry | 41.5 (24.2) | 66.1 (19.2) | 4.39† | 0.48 |
| Daily activity | 50.4 (23.3) | 72.3 (22.2) | 3.95† | 0.43 |
| Family relationship | 43.9 (20.6) | 66.4 (21.7) | 3.85† | 0.41 |
| Total | 48.4 (15.0) | 63.7 (13.9) | 5.10† | 0.55 |
| Days needing a caregiver | 14.11 (13.93) | 3.22 (7.66) | 3.24** | 0.36 |
| Interferes with work routine | 2.50 (1.09) | 1.00 (1.04) | 3.31** | 0.46 |
| Interferes with work concentration | 2.36 (1.28) | 1.14 (1.10) | 3.32** | 0.46 |
Note.
Repeated measures t test.
p < .01,
p < .001.
The additional items also support this conclusion. In general parents required additional caregiving help 14.11 days in the month before MEND, but only 3.2 days after MEND (MD = 10.89, SE = 3.36, 95% CI [3.8, 18.0]). Therefore, the number of days a parent needs additional help was reduced by 77%. Similar reductions were seen with the number of days the child's illness takes concentration away from the parent's work and their daily routine in their job.
Discussion
In summary, MEND is a psychosocial program grounded in family system and ecological theories, which is delivered in an intensive outpatient setting. MEND was created to serve a broad range of chronic illnesses as seen in the diversity of diagnoses found in our preliminary evaluation study. MEND is an intensive program in that sessions are 3 hours and the total program is 21 sessions in length, which specifically targets treatment adherences as the first order goal. Given the systemic grounding of MEND, the second order goal for MEND is the stress response patterns within the individual, micro- and mesosystem.
The evaluation of the preliminary data showed that MEND is able to reduce the impact of the chronic illness on the child's functioning across a broad variety of measures. Using the multidimensional HRQOL measure (Varni et al., 2001), this evaluation demonstrated a significant improvement on physical, emotional, social, cognitive, and school functioning. MEND also performed well in its aim as a systemic approach and provides significant reductions in the negative impact of the chronic illness on the larger family system. Moreover, the normative comparisons of the HRQOL measures suggest that MEND improves the HRQOL of the child to levels seen in healthy functioning families.
MEND offers a number of strengths that are worth noting. First, very few psychosocial programs currently exist which fully incorporate the family system within the intervention (Eccleston et al., 2012). We agree with both Eccleston et al. (2012) as well as others (Santos et al., 2012; Woods & McWey, 2012) who highlight the need for more interventions that incorporate multiple levels of the child's ecology. The positive program results from the preliminary data are an especially encouraging first step in building and testing a program that answers this call. In addition, this study, along with other evaluations of multifamily group programs for chronic illness (Lopez-Larrosa, 2013), provides evidence for the inclusion of peer and multifamily groups in the treatment of chronic illness.
While we believe that the evaluation results support the effectiveness of MEND, there are notable limitations that must be addressed in future studies. The preliminary results are based on a rather small sample size and normative comparisons for the PedQL Family Impact Module were difficult to obtain given the limited literature on this issue (which in itself suggests the strong need to conduct these types of studies). Similarly, given the secondary data analyses approach of this evaluation, there was not a true control condition and therefore normative published results were used for comparisons and benchmarking.
A second limitation is the lack of a long-term evaluation. As noted above, while many of the existing treatments have been shown to be effective in the short run, the vast majority of interventions have yet to demonstrate longer term sustainable effects. Within the current environment where few family systems approaches exist, we first wanted to explore the preliminary effectiveness of the program before justifying a larger and more involved study aimed at measuring the sustainability of the outcomes. Furthermore, we believe that the current evidence of the sustainability effect within family system approaches (e.g., Ellis, Templin, Naar-King, et al., 2007) is due to the ecological focus within these approaches. As MEND offers a similar ecological intervention and the evaluation data showed a significant effect on the family system level, we believe it is likely that MEND will also show a sustainable effect in future studies.
A final limitation in this study is the natural clinical setting of this study. Because this study used data from a natural clinical site it did not have control over the specific number of sessions a family received; rather, MEND advertises a 21-session structure, but the majority of families received more than 21 sessions. Therefore, it is not completely clear whether MEND is best utilized in a 21-session structure or whether more sessions are required. In addition, families self-selected into the program after a physician referral; because of this, some families may have not followed through with the referral due to the rigorous nature of the program (all family members must attend all 21 sessions). Future studies will need to examine the most appropriate dosage (number of sessions) as well as the effect of the self-selection into a rigorous and time demanding program.
Given these limitations, we note the following steps for future research and program development in the area of pediatric chronic illness. First, we believe that studies like this, as well as the research on adherence and family systems interventions for chronic illness, highlight the importance of the family system in creating a sense of self-efficacy within the adolescent and ultimately helping the family develop self-management skills. These are clearly a prerequisite to better health outcomes later on in life. Because of this, we agree with Eccleston et al. (2012) as well as Santos et al. (2012) and Woods and McWey (2012) who strongly encourage systems minded family practitioners to develop more programs and interventions for this population. In other words, the need is great and few programs are able to meet this need. Without more access to quality, systemic programs, these families will lack the support they need, or worse spend their limited resources investing in programs that have failed to produce significant and sustainable change (Eccleston et al., 2012).
Acknowledgments
This publication was in part supported by the National Institute of Health Disparities and Minority Health of the National Institutes of Health under award number P20MD006988.
References
- Armstrong B, Mackey ER, Streisand R. Parenting behavior, child functioning and health behaviors in preadolescents with type 1 diabetes. Journal of Pediatric Psychology. 2011;36(9):1052–1061. doi: 10.1093/jpepsy/jsr039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baldwin-Gracey B, Ward WL. Assisting with school absences for pediatric health conditions. Journal of Pediatric Health Care. 2012;26(5):374–379. doi: 10.1016/j.pedhc.2012.05.001. [DOI] [PubMed] [Google Scholar]
- Barlow JH, Ellard DR. Psycho-educational interventions for children with chronic disease, parent and siblings: An overview of the research evidence base. Child Care Development. 2004;30(6):637–645. doi: 10.1111/j.1365-2214.2004.00474.x. [DOI] [PubMed] [Google Scholar]
- Beale IL. Scholarly literature review: Efficacy of psychological interventions for pediatric chronic illness. Journal of Pediatric Psychology. 2005;31(5):437–451. doi: 10.1093/jpepsy/jsj079. [DOI] [PubMed] [Google Scholar]
- Blow AJ, Distelberg B. Common factors in four evidence-based family therapy approaches; Paper presented at the National Council on Family Relations Annual Conference; Minneapolis, MN. 2006. [Google Scholar]
- Dashiff C, Bartolucci A, Wallander J, Abdullatif H. The relationship of family structure, maternal empowerment and family conflict with self-care adherence of adolescents with type I diabetes. Families, Systems & Health. 2005;23(1):66–79. [Google Scholar]
- Eccleston C, Palermo TM, Fisher E, Law E. Psychological interventions for parents of children and adolescents with chronic illness (Review) Cochrane Library. 2012;8:1–139. doi: 10.1002/14651858.CD009660.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis DA, Frey MA, Naar-King S, Templin T, Cunningham PB, Cakan N. Use of multisystemic therapy to improve regimen adherence among adolescents with type 1 diabetes in chronic poor metabolic control: A randomized controlled trial. Diabetes Care. 2005;28:1604–1610. doi: 10.2337/diacare.28.7.1604. [DOI] [PubMed] [Google Scholar]
- Ellis DA, Templin T, Naar-King S, Frey M, Cunningham PB, Podolski C, Cakan N. Multisystemic Therapy for adolescents with poorly controlled type I diabetes: Stability of treatment effects in a randomized controlled trial. Journal of Consulting and Clinical Psychology. 2007;75(1):168–174. doi: 10.1037/0022-006X.75.1.168. [DOI] [PubMed] [Google Scholar]
- Ellis DA, Naar-King N, Chen X, Moltz K, Cunningham PB, Idalski-Carcone A. Multisystemic therapy compared to telephone support for youth with poorly controlled diabetes: Findings from a randomized controlled trial. Annals of Behavioral Medicine. 2012;44:207–215. doi: 10.1007/s12160-012-9378-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gifford-Smith ME, Brownell CA. Childhood peer relationships: Social acceptance, friendships, and peer networks. Journal of School Psychology. 2003;41:235–284. [Google Scholar]
- Halfon N, Newacheck PW. Evolving notions of childhood chronic illness. Journal of the American Medical Association. 2010;303(7):665–666. doi: 10.1001/jama.2010.130. [DOI] [PubMed] [Google Scholar]
- Kaffenberger C. School reentry for students with chronic illness: A role for professional counselors. Professional School Counseling. 2006;9:223–230. [Google Scholar]
- La Greca AM, Auslander WF, Greco P, Spetter D, Fisher EB, Santiago JV. I get by with a little help from my family and friends: Adolescents' support for diabetes care. Journal of Pediatric Psychology. 1995;20:449–476. doi: 10.1093/jpepsy/20.4.449. [DOI] [PubMed] [Google Scholar]
- Lewandowski A, Drotar D. The relationship between parent-reported social support and adherence to medical treatment in families of adolescents with type 1 diabetes. Journal of Pediatric Psychology. 2007;32(4):427–436. doi: 10.1093/jpepsy/jsl037. [DOI] [PubMed] [Google Scholar]
- Liddle HA. Multidimensional family therapy for adolescent cannabis users, cannabis youth treatment series, volume 5 DHHS Pub No 02–3660. Rockville, MD: Center for Substance Abuse Treatment, Substance Abuse and Mental Health Services Administration; Available from: 2002. http://www.kap.samhsa.gov/products/manuals/cyt/pdfs/cyt5.pdf. [Google Scholar]
- Lopez-Larrosa S. Quality of life, treatment adherence, and locus of control: The multiple family groups for chronic medical illnesses. Family Process. 2013;52(4):685–696. doi: 10.1111/famp.12034. [DOI] [PubMed] [Google Scholar]
- McBroom LA, Enriquez M. Review of family-centered interventions to enhance the health outcomes of children with type 1 diabetes. The Diabetes Educator. 2009;35(3):428–438. doi: 10.1177/0145721709332814. [DOI] [PubMed] [Google Scholar]
- Miller VA, Drotar D. Decision-making competence and adherence to treatment in adolescents with diabetes. Journal of Pediatric Psychology. 2007;32(2):178–188. doi: 10.1093/jpepsy/jsj122. [DOI] [PubMed] [Google Scholar]
- Minuchin S, Baker L, Rosman BL, Liebman R, Milman L, Todd TC. A conceptual model of psychosomatic illness in children: Family organization and family therapy. Archives of General Psychiatry. 1975;32:1031–1038. doi: 10.1001/archpsyc.1975.01760260095008. [DOI] [PubMed] [Google Scholar]
- Minuchin S, Fishman HC. Family therapy techniques. Cambridge, MA: Harvard University Press; 1981. [Google Scholar]
- Modi AC, Pai AL, Hommel KA, Hood KK, Cortina S, Hilliard ME, Guilfoyle SM, et al. Pediatric self-management: A framework for research, practice and policy. Pediatric. 2012;129(2):e473–e485. doi: 10.1542/peds.2011-1635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrie KJ, Jago LA, Devcich DA. The role of illness perceptions in patients with medical conditions. Current Opinion in Psychiatry. 2007;20(2):163–167. doi: 10.1097/YCO.0b013e328014a871. [DOI] [PubMed] [Google Scholar]
- Possemato K, Geller PA, Ouimette P. Posttraumatic stress and quality of life in kidney transplant recipients. Traumatology. 2009;15(3):34–39. [Google Scholar]
- Santos S, Crespo C, Silva N, Canavarro MC. Quality of life and adjustment in youths with asthma: The contributions of family rituals and the family environment. Family Process. 2012;51:557–569. doi: 10.1111/j.1545-5300.2012.01416.x. [DOI] [PubMed] [Google Scholar]
- Scholten L, Willeman AM, Last BF, Maurice-Stam H, van Dijk EM, Ensink E, et al. Efficacy of psychosocial group intervention for children with chronic illness and their parents. Pediatrics. 2013;131(4):E1196–E1203. doi: 10.1542/peds.2012-2222. [DOI] [PubMed] [Google Scholar]
- Sexton TL, Alexander JF. Functional family therapy: A mature clinical model for working with at-risk adolescents and their families. In: Sexton TL, Weeks GR, Robbins MS, editors. Handbook of family therapy. New York: Brunner-Routledge; 2003. pp. 323–348. [Google Scholar]
- Sheidow AJ, Henggeler SW, Schoenwald SK. Multisystemic therapy. In: Sexton TL, Weeks GR, Robbins MS, editors. Handbook of family therapy. New York: Brunner-Routledge; 2003. pp. 323–348. [Google Scholar]
- Sprenkle D, Blow AJ. Common factors and our sacred models. Journal of Marital and Family Therapy. 2004;30:113–129. doi: 10.1111/j.1752-0606.2004.tb01228.x. [DOI] [PubMed] [Google Scholar]
- Szapocznik J, Hervis O, Schwartz S. NIDA Treatment Manual Series #5. Rockville, MD: National Institute on Drug Abuse; 2003. Brief strategic family therapy for adolescent drug abuse (NIH Publication No. 03-4751) [Google Scholar]
- Varni JW, Bryant WP, Limbers CA, Wilson DP, Burwinkle TM. The ePedsQL™ in Type I and Type 2 diabetes: Feasibility, reliability and validity of the Pediatric Quality of Life Inventory™ internet administration. Diabetes Care. 2008;31(4):672–677. doi: 10.2337/dc07-2021. [DOI] [PubMed] [Google Scholar]
- Varni JW, Gottschalk M, Burwinkle TM, Kaufman F, Jacobs JR, Jones KL. The PedsQL™ in type I and type 2 diabetes: Reliability and validity of the Pediatric Quality of Life Inventory™ Generic Core Scales and Type I Diabetes Module. Diabetes Care. 2003;26(6):631–637. doi: 10.2337/diacare.26.3.631. [DOI] [PubMed] [Google Scholar]
- Varni JW, Seid M, Kurtin PS. The PedsQL 4.0: Reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Medical Care. 2001;39:800–810. doi: 10.1097/00005650-200108000-00006. [DOI] [PubMed] [Google Scholar]
- Varni JW, Sherman SA, Burwinkle TM, Dickinson PE, Dixon P. The PEdsQL™ family impact module: Preliminary reliability and validity. Health and Quality of Life Outcomes. 2004;2(55) doi: 10.1186/1477-7525-2-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward BW, Schiller JS. Prevalence of multiple chronic conditions among US adults: Estimates from the national health interview survey. Preventing Chronic Disease. 2013;19:1–15. doi: 10.5888/pcd10.120203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood BL. Beyond the ‘psychosomatic family’: A biobehavioral family model of pediatric illness. Family Process. 1993;32:261–278. doi: 10.1111/j.1545-5300.1993.00261.x. [DOI] [PubMed] [Google Scholar]
- Wood BL, Klebba KB, Miller BD. Evolving the biobehavioral family model: The fit of attachment. Family Process. 2000;39(3):319–344. doi: 10.1111/j.1545-5300.2000.39305.x. [DOI] [PubMed] [Google Scholar]
- Woods SB, McWey LM. A biopsychosocial approach to asthma in adolescents encountering child protective services. Journal of Pediatric Psychology. 2012;37(4):404–413. doi: 10.1093/jpepsy/jsr104. [DOI] [PubMed] [Google Scholar]
- Wysocki T, Harris MA, Buckloh LM, et al. Randomized trial of behavioral family systems therapy for diabetes: Maintenance of effects on diabetes outcomes in adolescents. Diabetes Care. 2007;30:555–560. doi: 10.2337/dc06-1613. [DOI] [PubMed] [Google Scholar]