Introduction
Acute hospitalizations in patients with cancer are a major driver of the cost of cancer care, accounting for nearly half advanced cancer spending.1 Reducing acute hospitalizations is a potentially important strategy for improving the quality, value, and patient-centeredness of cancer care. The Agency for Healthcare Research and Quality has endorsed a set of administrative measures to identify potentially avoidable hospitalizations, however these measures do not apply to patients with cancer.2 We sought to evaluate the proportion of hospitalizations in cancer patients that are viewed as potentially avoidable by clinicians directly involved in patient care.
Methods
We studied patients with solid tumor malignancies who were admitted to the medical oncology service at the Brigham and Women's Hospital between May 2013 and January 2014. Eligible patients were age 18 years or older and had two or more outpatient visits with a medical oncologist in the six months preceding hospitalization.
For each hospitalization, we conducted semi-structured interviews with three clinicians from the patient's medical care team, including the outpatient medical oncologist, the inpatient attending physician (also a medical oncologist), and the admitting resident physician or physician assistant. Clinicians gave oral consent for participation. Clinician interviews were required to be completed within 30 days of hospital admission, and the majority were completed within 14 days. Clinicians answered two questions regarding the avoidability of hospitalization: (1) On the day of admission, could the patient have been safely and effectively managed as an outpatient? and (2) Was hospitalization preventable with different medical management over the 30 days prior to admission? Responses of ‘probably’ or ‘definitely’ for either question were used to identify potentially avoidable hospitalizations. Interviewees answered additional questions about factors leading to hospitalization and patient psychosocial attributes.
The primary study outcome was the proportion of hospitalizations identified as potentially avoidable by two or more evaluators. Secondary analysis compared characteristics of patients who experienced potentially avoidable hospitalization with those who did not using the chi-squared test or the Wilcoxon non-parametric test. The study was approved by the Dana-Farber/Harvard Cancer Center IRB.
Results
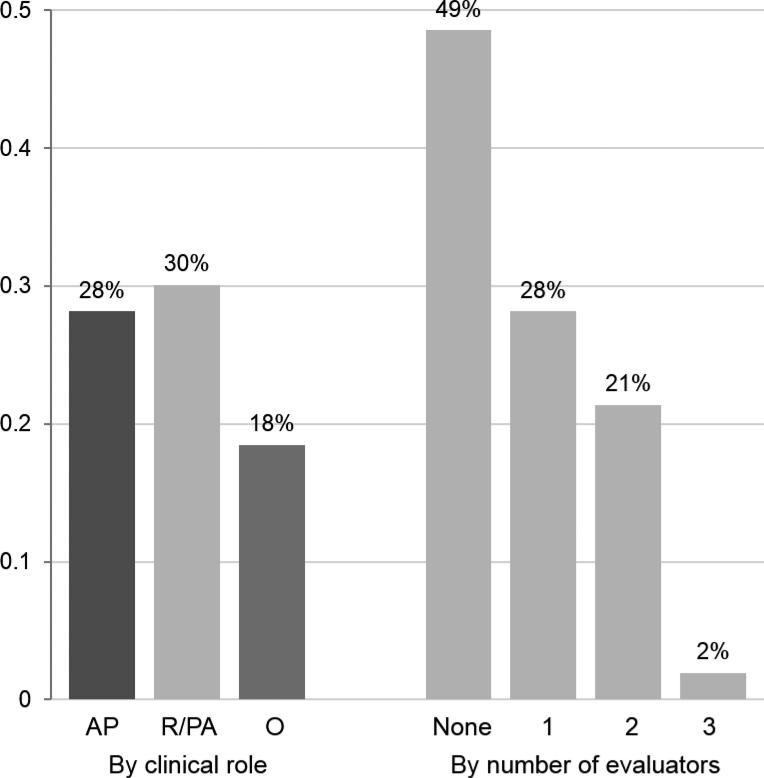
Complete interview data from three clinician interviewees were obtained for 103 eligible hospitalizations. 79% of patients had metastatic cancer, and additional patient characteristics are shown in Table 1. Twenty-four hospitalizations (23%) were identified as potentially avoidable by two or more clinicians, meeting the study definition of potentially avoidable hospitalization. Figure 1 shows the proportion of hospitalizations rated as potentially avoidable, stratified by clinical role and by the number of concurring clinicians.
Table 1.
Clinical characteristics and outcomes for hospitalized patients with solid tumor malignancies
| Patients (n = 103) | Potentially avoidable hospitalization | P-valuea | ||
|---|---|---|---|---|
| Yes (n = 24) | No (n = 77) | |||
| Age | ||||
| Median (range), years | 64 (25-86) | 67 (47 - 86) | 63 (25 - 83) | - |
| Mean, years | 62.5 | 67.2 | 61.0 | 0.05 |
| Female sex | 55 (53) | 12 (50) | 43 (54) | 0.70 |
| Metastatic cancer | 81 (79) | 19 (79) | 62 (78) | 0.94 |
| Primary cancer site | 0.07 | |||
| Lung | 18 (17) | 8 (33) | 10 (13) | |
| Breast | 12 (12) | 1 (4) | 11 (14) | |
| Colon or rectum | 11 (11) | 2 (8) | 9 (11) | |
| Otherb | 62 (60) | 13 (54) | 49 (48) | |
| Interval since last outpatient visit | ||||
| Median (range), days | 7 (0 - 88) | 6 (0 - 88) | 7 (0 - 81) | - |
| Mean, days | 13.0 | 13.0 | 12.9 | 0.97 |
| Reason for hospitalization | 0.02 | |||
| Cancer-related symptom | 58 (56) | 11 (45) | 47 (59) | |
| Side-effect of cancer treatment | 29 (28) | 7 (29) | 22 (28) | |
| Non-cancer medical condition | 7 (7) | 5 (21) | 2 (3) | |
| Planned hospitalization | 9(9) | 1 (4) | 8 (10) | |
| Clinical status prior to hospitalization | ||||
| ECOG performance status 2 or >c | 33 (32) | 11 (46) | 22 (28) | 0.10 |
| Appropriate for hospicec | 21 (21) | 6 (25) | 15 (20) | 0.80 |
| Enrolled in hospice | 3 (3) | 1 (4) | 2 (3) | 0.64 |
| Psychosocial attributesc | ||||
| Below- average social support | 14 (14) | 4 (17) | 10 (13) | 0.62 |
| Below- average illness coping | 25 (25) | 6 (26) | 19 (24) | 0.84 |
| Below- average illness understanding | 16 (16) | 5 (21) | 11 (14) | 0.42 |
| Pyschosocial factors contributed to the reason for hospitalizationd | 27 (26) | 12 (50) | 15 (19) | 0.003 |
| Hospitalization outcomes | ||||
| Length of stay | ||||
| Median (range), days | 4 (<1 – 23) | 2 (<1 – 11) | 4 (<1 – 23) | - |
| Mean, days | 5.3 | 3.5 | 5.8 | 0.02 |
| 30-day readmissions | 29 (28) | 5 (21) | 24 (30) | 0.36 |
| 30-day deaths | 17 (17) | 3 (13) | 14 (18) | 0.55 |
Values expressed as number (percentage), except where noted otherwise.
Between-group comparisons were performed using the chi-squared test or the Wilcoxon non-parametric test. Associations were considered statistically significant when the p-value was less than 0.05.
All other primary cancer sites represented less than 10% of patients.
As assessed by the patient's outpatient oncologist.
As identified by two or more of three interviewed clinicians.
Figure 1. Percentage of hospitalizations considered to be potentially avoidable.
The y-axis shows the percentage of hospitalizations that were considered to be potentially avoidable. N = 103 hospitalizations. AP, inpatient attending physician; R/PA, resident/physician assistant, O, outpatient oncologist.
We tested the association between potentially avoidable hospitalization and social support, illness coping skills, and illness understanding, finding no significant associations (Table 1). However, clinician identification of psychosocial factors as contributing to the reason for hospitalization was significantly associated with potentially avoidable hospitalization (p = 0.003, Table 1). Anxiety/depression and inadequate home support were the two psychosocial factors most commonly identified as contributing to hospitalization in an exploratory qualitative analysis. Potentially avoidable hospitalization was associated with shorter length of stay, but not 30-day readmissions or mortality (Table 1).
Discussion
Direct identification of avoidable or preventable hospitalizations in patients with cancer is challenging, and administrative measures are lacking. In a prior study, retrospective medical record review identified 19% of hospitalizations in patients with gastrointestinal cancer as potentially avoidable.3 Here, we demonstrate that clinicians directly involved in caring for patients with cancer agree that nearly one in four hospitalizations (23%) are potentially avoidable. Anxiety/depression and inadequate home support were frequently identified as triggers of potentially avoidable hospitalization. Still, all three clinicians agreed about the avoidability of hospitalization only 51% of the time, demonstrating that clinician perspectives are subjective and may vary by clinical role. Future efforts to study avoidable hospitalizations in cancer patients should test specific interventions to enhance the delivery of outpatient cancer care, evaluating the effect of these interventions on hospitalization rates.
Acknowledgments
Gabriel Brooks had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Dr. Brooks was supported by a Young Investigator Award from the Conquer Cancer Foundation of the American Society of Clinical Oncology and by a program grant from the National Cancer Institute of the National Institutes of Health (R25CA09220). The contents of this publication are the sole responsibility of the authors, and do not necessarily represent the official views of the National Cancer Institute, the National Institutes of Health, or the American Society of Clinical Oncology. Funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, and approval of the manuscript.
Footnotes
The authors report no relevant conflicts of interest.
References
- 1.Brooks GA, Li L, Uno H, Hassett MJ, Landon BE, Schrag D. Acute hospital care is the chief driver of regional spending variation in Medicare patients with advanced cancer. Health Aff. (Millwood) doi: 10.1377/hlthaff.2014.0280. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Agency for Healthcare Research and Quality [October 2, 2014];Prevention quality indicators overview. http://www.qualityindicators.ahrq.gov/modules/pqi_overview.aspx.
- 3.Brooks GA, Abrams TA, Meyerhardt JA, et al. Identification of Potentially Avoidable Hospitalizations in Patients With GI Cancer. J. Clin. Oncol. 2014 Feb 20;32(6):496–503. doi: 10.1200/JCO.2013.52.4330. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]