Abstract
An understanding of the mechanisms of personality development provides a systematic way to promote health as an integrated state of physical, mental, social, and spiritual well-being. Individual differences in personality are causal antecedents of the full range of psychopathology. The maturation with integration of personality appears to be an important mechanism by which diverse modalities of treatment promote wellness and reduce illness. First, the authors review the relationship between personality and a wide range of psychiatric disorders. Second, the authors evaluate the impact of character structure on a wide range of measures of well-being, including positive emotions, negative emotions, life satisfaction, perceived social support, and perceived health. Third, the authors describe a practical and inexpensive clinical method for facilitating the maturation and integration of personality based on an understanding of the processes of human thought, which underlie changes in personality and well-being.
The major problem limiting the effectiveness of mental health care is the failure to promote well-being due to an excessive contemporary focus on deficits symptomatic of mental ill-being. Our treatments focus on symptoms rather than on causes of dysfunction and fail to promote healthy functioning. As a result, improvements in treatment are usually weak, incomplete, and temporary, whether based on psychopharmacology or psychotherapy (1). In contrast, randomized controlled trials of treatments designed to promote well-being have been shown to reduce dropout, relapse, and recurrence rates compared with treatments for symptoms of disorder (2–4). In addition, psychiatric care to promote well-being reduces the stigma and increases recovery of mental health. In other words, mental health care appears to be more effective than mental illness care.
An understanding of personality development provides a systematic way to promote health, which can be defined as an integrated state of physical, mental, social, and spiritual well-being, rather than merely the absence of disease or infirmity (5, 6). More specifically, mental health has been described as “A state of well-being in which the person realizes and uses his or her own abilities, can cope with the normal stresses of life, can work productively and fruitfully, and is able to contribute to his or her community” (6). This definition of mental health corresponds closely to the description of maturity of personality, particularly the character traits of self-directedness, cooperativeness, and self-transcendence, which allow a person to work, love, and serve others. In fact, there is extensive data indicating that individual differences in personality are causal antecedents contributing to the full range of psychopathology (7).
Mental health professionals and educators use a wide variety of methods for the development of character and well-being. The traditional mainstays of psychiatric treatment have been various forms of pharmacotherapy and psychotherapy, but there are also many other effective evidence-based treatments that promote greater mind-body awareness by means of work on physical exercise, diet, sleep hygiene, deep breathing exercises, guided imagery, muscular relaxation, or meditation (8–10). The effects of conventional and alternative methods are often indistinguishable, suggesting that some common mechanism is being influenced by complementary pathways (11). How do these diverse biological, psychological, and social interventions influence well-being? One clear answer has been given to this question by sages throughout history (1). Well-being and the integration of personality depend fundamentally on self-awareness, as summarized in the Delphic injunction to “Know Yourself.” Rather than relying on the authority of ancient sages, however, here we will consider evidence to evaluate the possibility that character development can be facilitated by diverse methods that enhance a person’s awareness of any aspect of their being, including their body, thoughts, or psyche. To do so, we must evaluate ways of measuring the different aspects of being and well-being. Each of these terms and their aspects need to be clearly defined and measured in ways that can be implemented efficiently in clinical practice, as we will describe in detail. We must also consider the mechanisms by which increasing awareness may promote increased well-being and reduced ill-being.
First, we review the relationship between personality and a wide range of psychiatric disorders. Second, we evaluate the impact of character structure on a wide range of measures of well-being, including positive emotions, negative emotions, life satisfaction, perceived social support, and perceived health. Third, we describe a practical and inexpensive clinical method for facilitating the maturation and integration of personality based on an understanding of the processes of human thought, which underlie changes in personality and well-being.
The complexity of personality and psychopathology
Remember that most psychopathology has a complex or multifactorial causation and that it develops as a nonlinear dynamic system. This means that disorders depend on combinations of multiple genetic and environmental variables and that the same factor may contribute to many different disorders and that the same disorder may arise from interactions of different sets of causes. The effect of a variable can be very different, depending on which other variables it is combined with. As a result, we should not expect simple linear chains of development from molecular variables to clinical syndromes, even though contrary claims are made frequently and just as frequently fail to be confirmed. Complexity of pathogenesis is another way of talking about the “equifinality” and “multifinality” properties of development observed consistently for personality and psychopathology (12, 13).
The complexity of personality and psychopathology has been amply confirmed by etiological research. We have no laboratory tests for any psychiatric disorder. Genetic variables, when found, have weak and inconsistent effects when evaluated one at a time because their effects depend on other unmeasured genetic and environmental variables with which they are combined. There are no algorithmic formulae or shortcuts for understanding the complex biopsychosocial processes involved in the development of well-being and its disorders.
The relationship of personality and psychopathology
Personality traits are an important component of the complex development of the full range of psychopathology but do not explain most of the variance in risk for psychiatric disorders. The incomplete determination of psychopathology by personality is partly related to the incompleteness of what is traditionally called personality. A fuller account of all aspects of a person needs to include sexuality, physicality, emotionality, intellect, and spirituality in an integrated developmental perspective (14). Furthermore, the development of psychiatric disorders depends on internal and external variables that pull on the self, such as the appropriateness of a person’s life style, goals, and values within the personal, social, and cultural setting in which they live (15). We cannot separate the self or the whole person from their family or culture any more than we can separate a person’s body and mind. Efforts to do so result in “brainless” or “mindless” perspectives, which eventually lead to confusion rather than understanding (16, 17).
As a result of such complexity, we must be modest about the extent to which personality explains the etiology of psychopathology. Yet it is also clear that personality variables contribute to most psychopathology and that the integration of personality allows such improved adaptation that people can enjoy the way they have learned to live well with the strengths that they always had or the abilities that they can acquire with experience or treatment. This is the modest etiological but hopeful therapeutic claim that we think is justified by what we know about personality development: Nearly all human beings have enough capacity for self-awareness to allow them to learn how to live well—with satisfaction, purpose, and a sense of meaning greater than their individual selves, even if their self-awareness is initially limited. Some randomized controlled trials have been done to directly support this claim using diverse methods to increase awareness of the body, thoughts, and psyche of a person (2, 4, 8–11), but much more is needed before this claim can be considered well-documented. Our limited knowledge of the science of well-being is a well-known reality that every practicing psychiatrist already faces daily with each patient encountered. What all mental health professionals need is a practical way to help people make their lives better. So here we will review the facts that are available to guide such a hopeful person-centered approach to well-being.
The similarity of personality variants and major clinical syndromes
Psychiatrists have been divided by interest and training into schools that emphasize the importance of major categories of illness, as described on axis I of DSM, or the development of personality traits, as described on axis II of DSM. Sometimes these distinctions have been confounded with the belief that neurobiology or nature causes the major categories of illness, whereas psychosocial development or nurture causes personality traits. The dichotomies of nature or nurture, neurobiology or psychosocial development, and category or trait are no longer scientifically tenable perspectives (17). The brain does not have centers for different categories of illness; it is modular, with each module having functions that participate in a variety of integrative processes in combination with other modules to allow purposeful adaptation to internal and external events. These modules are extensively interconnected, like the Internet, so that communication operates as a nonlinear dynamic system with quantum-like properties (1). The dynamics of shifts in brain states is depicted in Figure 1. The two brain states, A and B, in Figure 1 represent different configurations of a person’s brain modules. The two brain states or configurations of personality differ in their level of information content and well-being. These states are technically described as “metastable”: a person can be stuck in the less well configuration A because the only way to reach the more well configuration A is by temporarily giving up some of the advantages or pleasures associated with configuration B. In clinical terms, people must face who they are and recognize both the advantages and disadvantages of their current way of living and of other potential attitudes toward life before they can change without self-defeating conflict. As a result of such relative stability, configurations of traits can appear to be a categorical disorder temporarily until they radically transform, usually in the flash of a moment of insight leading to a change in outlook.
Figure 1.
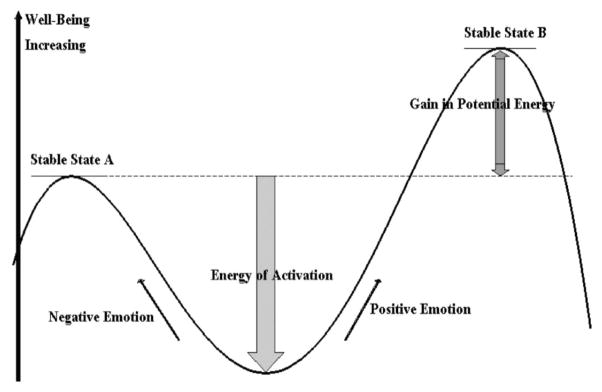
The Nonlinear Dynamics of Shifts in Brain States Differing in Level of Well-being or Integration of Information Content.
(Reproduced with Permission of the Washington University Center for Well-Being.)
It is important for clinicians of all perspectives to recognize that there is substantial similarity in diagnosis and treatment whether viewed through the lens of major clinical syndromes, personality disorders, or the traits they share in common. The similarity between major syndromes and personality disorders is illustrated in Table 1. Although it may seem surprising to people accustomed to a biomedical model, even the major syndromes of schizophrenia, bipolar disorder, and major depressive disorder are strongly influenced by premorbid personality traits (18–21). As previously mentioned, temperament and character may not explain all of the components of a clinical syndrome, but their contribution is usually sufficient to effect recovery by understanding the personality configuration that led to vulnerability to the disorder.
Table 1.
Phenotypic Similarity between Major Clinical Syndromes and Personality Disorders
| Axis I Disorders: Major Variant | Axis II Disorders: Minor Variants | Shared Traits of Personality and Emotionality |
|---|---|---|
| Schizophrenia spectrum | Schizoid PD Schizotypal PD |
Anxiety-proneness, aloofness, magical thinking |
| Delusional disorder | Paranoid PD | Suspiciousness |
| Major depression | Depressive PD Borderline PD |
Proneness to depressed mood; proneness to self-destruction |
| Cyclothymia Bipolar disorder Mania |
Narcissistic PD Histrionic PD Antisocial PD |
Mood swings; impulsivity |
| Obsessive-compulsive disorder | Obsessive-compulsive PD | Hypochondriasis; inflexibility |
| Social phobia | Avoidant PD | Shyness; avoidant behavior |
| Panic disorder with agoraphobia | Dependent PD | Dependency |
PD, personality disorder.
Personality configurations in psychopathological syndromes
The components of temperament and character that are most strongly associated with different major psychiatric disorders are summarized in Table 2. A personality dimension is only indicated as high (+) or low (−) when it is regularly observed and useful for therapeutic intervention. The strongest effects are denoted as very high (++) or very low (− −). Table 2 gives the observations that are of practical utility for a clinician interested in diagnosis and treatment, and more details are given in the references cited in the text.
Table 2.
Personality Traits That Are Highly Likely to Be High (+) or Low (−) in Different Mental Disorders and States of Mental Health
| Mental Disorder | HA | NS | RD | PS | SD | CO | ST |
|---|---|---|---|---|---|---|---|
| Schizophrenia | + | − | − − | − | ++ | ||
| Mood Disorder | |||||||
| Depression | ++ | − | − | − | |||
| Bipolar | ++ | ++ | − | − | − | ||
| Anxiety Disorder | |||||||
| GAD, Panic | ++ | ||||||
| OCD | ++ | − | − | − | − | − | |
| Social anxiety | ++ | − | + or − | − | |||
| Eating disorder | |||||||
| Anorexia | ++ | ++ | |||||
| Bulimia | ++ | ++ | − − | ++ | |||
| Substance dependence | ++ | − − | − | ||||
| Personality disorder | |||||||
| OCPD | + | − | ++ | − − | − | ||
| Cluster A | − − | − − | − | + | |||
| Cluster B | ++ | − − | − | ||||
| Cluster C | ++ | − − | − | ||||
| Mental order | |||||||
| Positive emotionality | ++ | + | ++ | ||||
| Social well-being | ++ | ++ | |||||
| Perceived health | ++ | ||||||
| Well sibling of depressive | ++ | ||||||
| Well sibling of schizophrenic | ++ | + | |||||
| Resilience to stress | − | + | + | + | + | + | + |
HA, harm avoidance; NS, novelty seeking; RD, reward dependence; PS, persistence; SD, self-directedness; CO, cooperativeness; ST, self-transcendence; GAD, generalized anxiety disorder; OCD, obsessive-compulsive disorder; OCPD, obsessive-compulsive personality disorder.
Schizophrenia
Extensive findings about temperament and character configurations contributing to schizophrenia have recently been reviewed (21, 22). Perceptual aberrations and magical thinking characterize the character configuration of low self-directedness and high self-transcendence because such people have poor reality testing (i.e., low self-directedness) combined with vivid fantasy (i.e., high self-transcendence). The full schizotypal or disorganized character configuration also includes social intolerance, hostility, and distrust (i.e., low cooperativeness). Schizophrenics also are asocial because they are both anxiety-prone (i.e., high in harm avoidance) and emotionally aloof (i.e., low reward dependence). In a study of schizophrenics and their non-psychotic siblings, asociality was found to be a mediating variable leading to schizophrenia only when combined with schizotypal character traits or with the neurocognitive deficits typical of schizophrenics, such as poor working memory and low crystallized intelligence (21). More importantly, high self-directedness was strongly correlated with the absence of neurocognitive deficits, such as low crystallized intelligence, in the nonpsychotic siblings of schizophrenics, whereas it is not correlated with intelligence in the general population. In other words, high self-directedness is protective against neurocognitive deficits and psychosis in siblings of schizophrenics (21). High self-directedness is also strongly associated with measures of well-being among schizophrenics in treatment (23).
Mood disorders
Patients with major depressive disorders and their siblings have a personality structure different from that of healthy control subjects and their siblings (18). Study of people with major depression and their siblings has allowed a rigorous evaluation of the heritable trait effects of personality as well as the extent to which they are influenced by mood states. The causal importance of personality in major depression can be tested in a sibling study because both personality and major depression are heritable. In the families of patients with major depression, the Temperament and Character Inventory (TCI) personality traits are all moderately heritable (18), just as they are in samples of healthy people in the general population (24). Likewise the risk of major depression was increased in the siblings of patients with depression compared with the siblings of healthy control subjects. The current level of depressed mood was correlated with high harm avoidance, low novelty seeking, and low self-directedness, indicating some state effect of mood on self-reports of personality. People with past histories of recurrent depression had particularly high harm avoidance scores, suggesting severity of predisposition and/or scarring from past episodes. Well siblings of patients with depression who have never had depression were lower in harm avoidance, higher in novelty seeking and reward dependence, and lower in cooperativeness. Persistence, cooperativeness, and self-transcendence did not influence the risk of depression in siblings. Other studies confirm the strong impact of high harm avoidance and low self-directedness on risk of depression (25–27). Higher harm avoidance scores reduce the response to antidepressant drugs, so that treatment responses are poorer and slower, and outcomes are worse at 6 and 18 months (28–30). Higher harm avoidance is associated with earlier onset, a greater number of past depressive episodes, and higher future recurrence risks (20, 29, 31, 32). Temperament configuration influences drug response and can be used to guide choice of drug, dosage, and adjunctive medications according to some studies (33, 34). Both tricyclic antidepressants and selective serotonin reuptake inhibitors reduce harm avoidance scores, which mediates a reduction in depression (30, 34, 35). Lowering harm avoidance increases serotonergic activity (30, 36) and enhances connectivity between the amygdala and the anterior cingulate cortex, which serves as a crossroads to enable emotional regulation, cognitive planning, and purposeful activity (37). Antidepressants and cognitive behavior therapy both increase self-directedness, which protects against relapse over the long term (31).
Patients with bipolar disorder have a personality structure different from that of those with unipolar depression or healthy control subjects. In terms of temperament, people with mania are higher in both novelty seeking and harm avoidance than are control subjects, whereas those with unipolar depression are usually higher only in harm avoidance (19, 38, 39) unless they have some comorbid feature such as substance abuse or suicide attempts (20, 40). The strong association of novelty seeking with bipolar disorder in adults is also observed in milder variants such as hyperthymia or cyclothymia (41, 42) and in prepubertal and adolescent bipolar disorder (43, 44). The full personality profile is usually made up of a sensitive (NHR) or explosive (NHr) temperament and a cyclothymic (sCT) or disorganized (scT) character, which are associated with emotional lability and immaturity, respectively. (In the personality profile, lower case letter refer to low scores and capital letters refer to high scores for the following traits: N, novelty seeking; H, harm avoidance; R, reward dependence; S, self-directedness; C, cooperativeness; T, self-transcendence.) Unfortunately, it is impossible to disentangle the effects of mood state on reporting in the absence of a sibling study in which mood is measured. When patients with euthymic bipolar disorder have been studied, they have consistently been found to have low persistence (45, 46), but sometimes also high harm avoidance (47) or low novelty seeking (46). However, high novelty seeking predicts a failure to recover euthymia in prospective studies (48, 49), so those who recover to stable euthymia may differ in their antecedent personality traits. Findings about comorbidity also indicate that bipolar disorder cannot be considered as a homogeneous category: bipolar patients with comorbid anxiety have higher harm avoidance and lower self-directedness than other bipolar patients, and bipolar patients with comorbid alcoholism have lower persistence (19). In summary, people with low persistence (i.e., easily discouraged and frustrated) or both harm avoidance and novelty seeking (i.e., conflicting needs for security and excitement) are vulnerable to bipolar disorder, particularly when their character is immature so that they cannot regulate their emotional conflicts, frustration, and disappointments.
Anxiety disorders
High harm avoidance is a strong and sensitive predictor of the presence and severity of anxiety disorders in adult and child psychiatric patients and in the general population (50–55), but not everyone with high harm avoidance develops a clinical anxiety disorder (53). Essentially, high harm avoidance increases a person’s sensitivity to and difficulty coping with the impact of negative life events (56–58). For example, high harm avoidance augments startle responses when a person’s prestimulus outlook is negative, whereas low harm avoidance reduces startle responses when a person’s prestimulus outlook is positive (59, 60). As a result of differences in sensitivity to internal and external events, the form of any clinical disorder depends not only on harm avoidance but also on other personality traits that influence the perception of life events (1, 61).
Except for obsessive-compulsive disorder (OCD), which is quite distinct in terms of personality, there is much overlap among the other anxiety disorders in both symptoms and personality configurations. Generalized anxiety disorder is most often associated with only high harm avoidance, whereas panic disorder and social anxiety disorder are somewhat more likely to occur in people who are both high in harm avoidance and low in novelty seeking (32, 62). In addition, people with social anxiety disorder are also unlikely to be average in reward dependence—they are likely to be either high in reward dependence (so that they are avoidant and rejection-sensitive) or low in reward dependence (so that they are cautious and aloof). Of course, any of these temperament profiles can be associated with weak development of character traits, particularly low self-directedness, which is moderately correlated with high harm avoidance (62–64). Patients who are higher in character development have pure anxiety disorders that respond better to antidepressants or cognitive therapy than those with less character development (63, 65).
Obsessive-compulsive disorder (OCD) has a distinct personality configuration compared with that of healthy control subjects and of those with other anxiety disorders. Adult and child patients with OCD and their first-degree relatives have a methodical temperament with very much higher harm avoidance, lower novelty seeking, and lower reward dependence (designated as an nHr temperament profile) compared with healthy control subjects and first-degree relatives of control subjects (66, 67) and are high in persistence (68). In terms of character, patients with OCD usually are low in self-directedness and cooperativeness (65, 69, 70). Personality traits are differentially associated with severity and type of symptoms among patients with OCD: greater symptom severity is correlated with low self-directedness and low cooperativeness, whereas hoarding is associated with higher persistence and/or higher harm avoidance (69–72). Patients with chronic fatigue syndrome have a premorbid personality configuration similar to that seen in OCD except that they are not likely to be low in reward dependence (73).
Substance dependence
High novelty seeking and low self-directedness are the two personality traits most consistently associated with alcohol and drug abuse. High novelty seeking involves impulsive thrill-seeking and experimentation with new things, such as experimenting with alcohol, cigarettes, or recreational drugs at an early age (74–77). Low self-directedness is just as strongly associated with substance abuse because it involves inadequate executive control of a person’s emotional drives (78). Thus, both high novelty seeking and low self-directedness contribute to difficulty inhibiting, delaying, or otherwise controlling impulsive behaviors, such as substance abuse, pathological gambling, or binging (79–82).
Novelty seeking interacts with other personality and familial variables in influencing the development of alcohol abuse (74). If a person has one or more alcohol-dependent parents, then high novelty seeking is an even stronger predictor of alcohol dependence in the child than if the child had no alcoholic parent (83). On the other hand, low novelty seeking protects children from developing alcoholism if they have alcoholic parents. Essentially novelty seeking serves as a nonlinear moderator of the familial risk of alcoholism, like an intrinsic ability to either expose a person to risk (if novelty seeking is high) or to protect them from risk (if novelty seeking is low).
Likewise the risk of alcohol abuse is increased if a person is extremely high or extremely low in harm avoidance or extremely high or extremely low in reward dependence, but the overall effects of novelty seeking and self-directedness are predominant in most circumstances (74). The overall effect of the extreme deviations of harm avoidance and reward dependence are missed if only group averages are compared. Nevertheless, if individuals low in novelty seeking begin to use alcohol to cope with stress, they may become dependent, particularly if they are high in harm avoidance and/or low in self-directedness, as often occurs in people who begin to drink during a depressive episode.
The impact of social pressure and cultural attitudes on substance dependence is particularly evident in the changing relationships between personality and cigarette smoking over the past 50 years. Initiation of regular cigarette smoking is usually associated with high novelty seeking combined with high persistence and low reward dependence (84, 85). Some people initiate smoking to relieve anxiety if they are high in harm avoidance and want to relieve negative affect or stress. Likewise, the withdrawal from cigarettes in regular smokers is not a consistent physiological syndrome, but one that depends substantially on personality. Smokers high in novelty seeking experience greater abstinence-induced increases in nicotine withdrawal, negative affect, and cigarette craving than smokers low in novelty seeking. In contrast, smokers high in harm avoidance report greater abstinence-induced increases in negative affect and urges to smoke to relieve stress (84). Reward dependence is not associated with abstinence effects. Cessation of cigarette smoking is strongly moderated by character traits, so that individuals who are highly self-directed are much more likely to succeed in quitting smoking when they decide to do so. In people born before 1950, cigarette smoking was a prosocial behavior and was correlated with high cooperativeness, particularly in men. However, when some people began to regard smoking as an antisocial behavior, it became correlated with low self-directedness and low cooperativeness, as is seen in many people born after 1950 (78). This example illustrates the importance of understanding psychopathology as the expression of dysfunction in a complex dynamic system regulating biopsychosocial adaptation (15). Personality assessment provides a systematic way to understand the motives of a person and the internal and external influences that pull on the self in an ever-changing biological, social, and cultural context. Adequate clinical understanding of mental disorders requires awareness of the meaning of desires, feelings, relationships, and events in relation to the goals and values of a person and the collective expectations of the society within which the person functions.
Eating disorders
Eating disorders provide well-defined clinical subgroups of individuals, who differ objectively in their weight, subjective features such as body image, and patterns of behavior such as restrictive dieting, binging, and/or purging. Temperament and character traits have been extensively studied in eating disorders and show strong utility for both differential diagnosis and treatment planning (86–88). High harm avoidance and low self-directedness are typical characteristics shared by all groups of patients with eating disorders compared with healthy control subjects, both before and after recovery (88). Restrictor anorexic individuals are perfectionistic and have high harm avoidance, high persistence, and relatively higher self-directedness compared with patients with other eating disorders. In contrast, binging bulimic individuals have approach-avoidance conflicts and are high in harm avoidance and novelty seeking along with lower self-directedness and lower cooperativeness (89–94). Anorexic individuals who also binge or purge are most like bulimic individuals in personality but may be high in persistence like restrictive anorectic patients (87, 93, 94). Likewise obese patients, whether they have food binges or not, are usually like normal-weight bulimic individuals in that they are high in harm avoidance and novelty seeking and low in self-directedness (80, 81). Not all patients with anorexia have the restrictive pattern with high persistence, however; some anorexic individuals are withdrawn and avoidant without enthusiasm for eating, as in individuals who are high in harm avoidance (H) and low in novelty seeking (n), combined with a depressive character structure [low in all three characters (sct)] (95). Hence the structure of personality can reveal more than the subdivision of eating disorders according to weight and eating behaviors alone. The temperament and character traits appear to have a causal role in the pathogenesis of eating disorders because they are heritable, expressed early in development, moderately stable throughout life, not explained by mood or metabolic status, and present before treatment and after recovery (86, 88).
The role of each personality trait in eating disorders has been examined in relation to different attitudes toward eating and weight. High novelty seeking is correlated with impulsivity and disinhibition, whereas low self-directedness is related to overall restraint in eating and susceptibility to hunger (96). Low self-directedness is the strongest predictor of severity of vomiting in bulimic individuals (97). People with both low self-directedness and high self-transcendence are prone to excessive fantasy and seem to be particularly reactive and susceptible to unrealistic societal messages about slenderness (96).
Temperament and character are also important predictors of prognosis in prospective longitudinal studies. Cognitive behavior therapy in bulimic individuals resulted in a reduction of harm avoidance and an elevation of self-directedness compared with pretreatment, but the values for the bulimic individuals continued to differ from the values for healthy control subjects (86, 88). High self-directedness at intake predicts rapid improvement with cognitive behavior therapy and sustained recovery at 1 year in bulimic individuals (86). Dropout rates from brief psychotherapy are high for patients with eating disorders who have borderline features, including high novelty seeking, high harm avoidance, low reward dependence (NHr) and disorganized character traits of low self-directedness, low cooperativeness, and high self-transcendence (scT) (98). Mature character development greatly facilitates treatment by helping with the emotional regulation of anger and frustration (99). Anorexic patients who are high in both self-directedness and cooperativeness at intake are more likely to recover fully with cognitive behavior therapy, whereas those who do not improve are higher in harm avoidance and lower in self-directedness (100). High self-directedness and high persistence are also strong predictors of sustained weight loss in morbidly obese people after gastric banding (101, 102).
These findings about the role of personality in the differential diagnosis and treatment of psychopathology indicate that the assessment of personality provides more information than is available from efforts to subdivide patients into categorical groups. The clinical syndromes remain useful because the same personality profile may lead to different problems under different conditions. Yet the personality configurations add much information to help in understanding the pathogenesis of the disorder, in prognostication of outcome, and in planning effective treatment interventions that are individually tailored to the patient’s resources and interests.
Anticipating and understanding comorbidity
Remember that personality traits occur in all possible combinations, whereas clinicians are accustomed to thinking as if a person has only one basic diagnosis. In fact, we know that there is extensive overlap among the major clinical syndromes, so that having a mood disorder or schizophrenia does not provide any protection from having other disorders. The phenomenon of comorbidity has revealed the fundamental inadequacy of categorical diagnosis (103). Once a clinician realizes that the syndromes are not mutually exclusive diseases and that they actually share many functional components, then the clinical utility of multidimensional personality assessment becomes clear. Our diagnostic and treatment processes are greatly facilitated by having a way to understand the patterns of comorbidity that we observe in people by knowing what their personality structure is. Once we know the personality structure, we can often anticipate what other problems individuals may have even if they did not volunteer the information in their initial presenting complaints.
For example, the TCI profile allows clear prediction of what comorbid syndromes are present in people presenting with any diagnosis, such as a major depressive disorder or bipolar disorder (19, 50, 104). If persons presenting with a mood disorder has high harm avoidance, which they usually do, then they are likely to have comorbid anxiety and somatization. If patients with major depression have high novelty seeking, they are likely to have comorbid syndromes associated with poor impulse control such as substance dependence, bulimia, binge eating, or pathological gambling. And vice versa, if patients with depression has substance dependence we should investigate whether they are high in novelty seeking. If patients with major depression are low in cooperativeness, we can anticipate that they will have problems with hostility or suspiciousness. The structure of personality forms a clear scaffold on which we can systematically organize our thinking about the functional interactions that occur over the course of people’s lives as they shape and adapt to an ever-changing internal and external environment. We can see that every component of personality is always important in adapting rather than trying to oversimplify human motivation by reducing it to a fuzzy set of idealized categories that are really metastable configurations of dynamic functional processes by which people seek health and happiness with more or less success (105).
Personality and well-being
In addition to understanding the relationship of personality to psychopathology, a mental health professional also needs to understand the relationship of personality to health as a state of physical, mental, social, and spiritual well-being (6). To proceed scientifically, we must be able to measure these aspects of well-being in a reliable way. We studied personality with the TCI and related it to well-validated measures of well-being in 1,102 consecutive community volunteers from the Sharon region of Israel (106). The measures of well-being we used were the Positive and Negative Affect Scale (107), the Satisfaction with Life Scale (108), and the Multidimensional Perceived Social Support Scale (109). Perceived health was also rated on a five-point Likert scale based on the item “How would you rate your health over the past 30 days?” from the 12-item General Health Questionnaire (110). Table 3 summarizes the correlations among these measures. Positive and negative affectivity were largely uncorrelated (r=−0.09), which reminds us that the presence of positive affect (i.e., happiness) is not at all the same as the absence of negative affect (i.e., not being depressed or upset). Scores for life satisfaction, perceived social support, and perceived health were weakly but positively correlated with one another (r=+0.23–+0.31), so we formed a Composite Health Index (CHI) as the mean of these three measures. Table 3 shows that each measure of health was strongly correlated with the CHI (r=+0.7–+0.8). These findings show that health and happiness are correlated but made up of distinguishable components of physical, mental, and social well-being, as suggested by the World Health Organization definition of health (WHO, 1946).
Table 3.
Correlations ×100 among Measures of Aspects of Well-Being: Positive Emotionality, Negative Emotionality, Life Satisfaction, Perceived Social Support, Perceived Health, and a Composite Health Index
| Composite Health | Perceived Health | Social Support | Life Satisfaction | Negative Affect | Positive Affect | |
|---|---|---|---|---|---|---|
| Positive Affect | 43 | 22 | 37 | 37 | −9 | (100) |
| Negative Affect | −42 | −30 | −23 | −41 | (100)- | |
| Life Satisfaction | 81 | 31 | 23 | (100) | ||
| Social Support | 77 | 23 | (100) | |||
| Perceived Health | 68 | (100) | ||||
| Composite Health | (100) |
All correlations are significant at p=0.000 except positive and negative affect (r=−0.09, p=0.005).
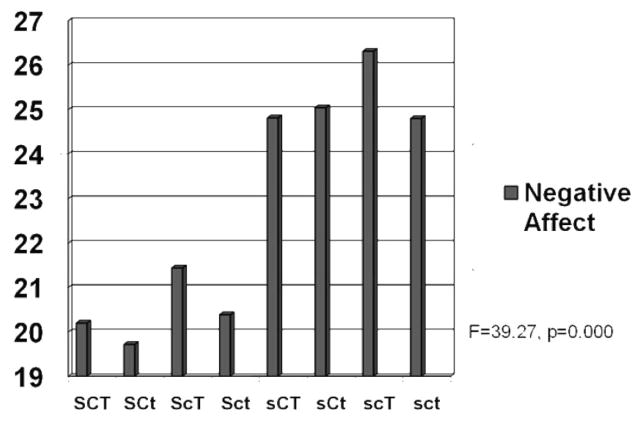
Next we began to consider the way a person’s character profile influenced these components of well-being. From prior work reviewed in the preceding section, we knew that recovery from mental disorders in prospective treatment studies involved greater maturity or adaptability of TCI character traits. In contrast, measures of well-being have little relationship to temperament traits except for harm avoidance (111). Prior work had suggested that a gradient in adaptiveness of character could be described along an approximate gradient shown in Figure 2 from the creative character (designated as SCT) with high self-directedness, high cooperativeness, and high self-transcendence to the depressive character (designated as sct) with low self-directedness, low cooperativeness, and low self-transcendence. Therefore, we sought to evaluate the relationship between character configuration and well-being for each of the measures of well-being in Table 3.
Figure 2.
Variation in Negative Affect as a Function of Character Profile.
Overall results are summarized in Table 2 for well-being in a format that parallels that for mental disorders. We will consider each of the measures in sequence to describe the way each character trait has distinct functional effects while interacting with the other traits.
First, let’s consider the relationship of character structure to the differences between individuals in negative affect (“unhappy”), as depicted in Figure 2. All four character configurations with high self-directedness had less negative affect than those with lower self-directedness, demonstrating a strong association of self-directedness with lower negative affect. Cooperativeness had a weak association when self-transcendence was high: higher cooperativeness was associated with lower negative affect in the contrast between moody and disorganized profiles (sCT versus scT) and between creative and fanatical profiles (SCT versus ScT). Self-transcendence was not associated with lower negative affect in any contrast.
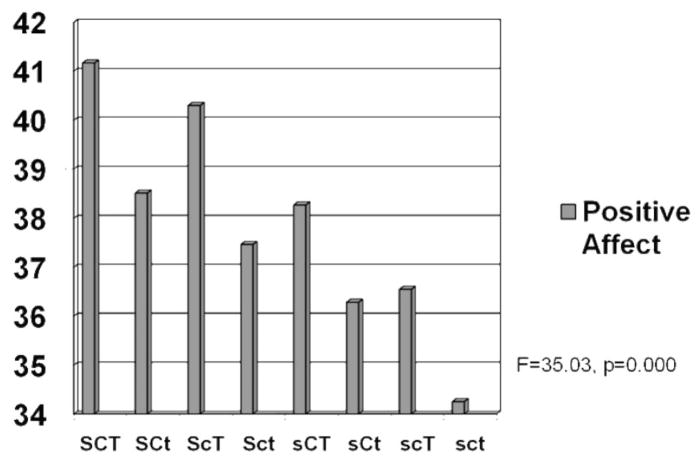
The interactions of character dimensions on positive affect, depicted in Figure 3, were different from those observed for negative affect. Higher self-transcendence was consistently associated with higher positive affect for each of the four possible configurations of self-directedness and cooperativeness (SCT versus SCt, ScT versus Sct, sCT versus sCt, and scT versus sct). Likewise, higher self-directedness was consistently associated with higher positive affect for each of the possible configurations of the other two characters. The association of higher cooperativeness with positive affect was also highly significant when self-directedness was low: higher cooperativeness was associated with higher positive affect than lower cooperativeness in the contrast of moody versus disorganized profiles (sCT versus scT) and for dependent versus depressive profiles (sCt versus sct). When self-directedness was high, higher cooperativeness was weakly associated with higher positive affect (SCt versus Sct and SCT versus ScT). In other words, the association of character profiles with positive affect was dependent on specific combinations of traits.
Figure 3.
Variation in Positive Affect as a Function of Character Profile.
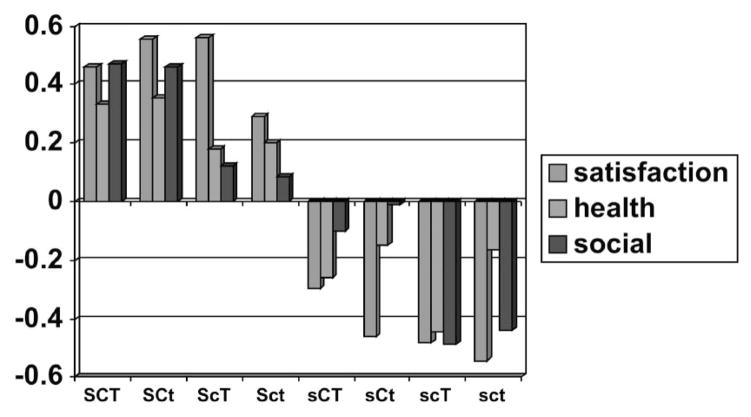
Likewise we evaluated the relationship between character profiles and the other measures of well-being shown in Figure 4. Profiles with higher self-directedness were again consistently associated with better life satisfaction, perceived social support, and perceived health than those with lower self-directedness. In addition, profiles with higher cooperativeness were associated with greater perceived social support than those with lower cooperativeness.
Figure 4.
Variation in Life Satisfaction, Perceived Health, and Perceived Social Support as a Function of Character Profile.
Another way to recognize the impact of character structure is to examine the proportion of people with each configuration who are in the top sixth and the bottom sixth of the population in overall health as measured by the CHI. Figure 5 illustrates the strong impact of self-directedness on health.
Figure 5.
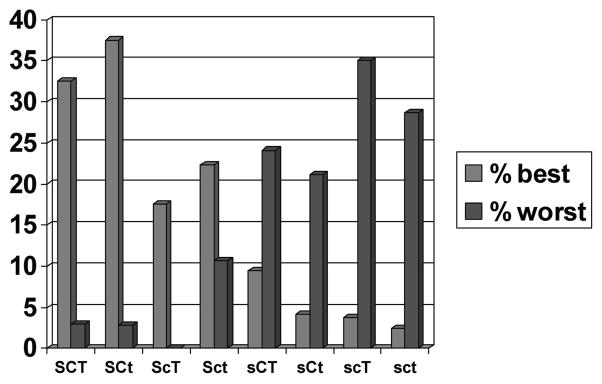
Comparison of Percentage of People in Each Character Configuration Who are in the Top One-sixth (“Best Health”) and Bottom One-sixth (“Worst Health”) of the Total Israeli Sample on the CHI.
As summarized in Table 2, high self-directedness is consistently associated with all our measures of well-being: lower negative affect, higher positive affect, greater life satisfaction, greater perceived social support, and better health. Accordingly, highly self-directed people are typically described as hopeful. Cooperativeness is associated with greater social well-being as measured by perceived social support. Accordingly, highly cooperative people are typically described as loving. Self-transcendence is associated with greater positive affect, so self-transcendent people are often described as exuberant or joyful. Self-directedness has pervasive importance for the development of well-being, but each aspect of character makes a unique contribution.
These results in a general community sample confirm the results of work reviewed in the prior section showing that character development has a crucial role in recovery from ill-being and the development of well-being. How then can character and well-being be systematically developed?
A psychobiological approach to the cultivation of well-being
Today many psychiatrists have limited time for psychotherapy, but nevertheless there is a great unmet need for ways to help facilitate character development. Personality assessment methods such as the TCI do enhance a clinician’s practice by promoting a person-centered therapeutic dialogue (112). However, additional methods need to be integrated with personality assessment to promote character development and well-being in a systematic way. We are proposing use of a multi-method psychoeducational course developed by C. R. Cloninger in consultation with the Anthropedia Foundation for the purpose of promoting growth in self-awareness (2). The course, available on a set of DVDs (Anthropedia, http://anthropedia.org) integrates experiences and practices that promote growth in self-awareness with evidence-based techniques from a wide variety of therapeutic approaches (cognitive-behavioral, person-centered, psychodynamic, logotherapy, well-being therapy, positive psychology, and others) and engages patients in practices that stimulate the development of the prefrontal cortex and lead to well-being (1, 2). The course combines assessment of temperament and character with a self-directed exploration of personal well-being.
The course contains five distinct modules or sections (Table 4). In the first module, a patient takes the TCI along with other brief measures of emotionality and life satisfaction to provide a baseline assessment and to stimulate reflection (107, 108). The patient reflects on what has provided lasting personal satisfaction in the past to improve his or her self-knowledge and become more likely to work toward satisfying goals. This self-exploration can help motivate the patient for constructive change, as well as help to establish a therapeutic alliance (112–115). Self-observation about attitudes characteristic of well-being (1) and related evidence-based exercises that promote satisfaction, such as practicing acts of kindness, suggest ways for the patient to begin to know himself or herself better (116). Functional brain imaging shows that such exercises activate the medial and anterior prefrontal cortex (Brodmann areas 8, 9, and 10), which is implicated in self-aware processes characteristic of self-directedness, cooperativeness, and self-transcendence (1, 117–120).
Table 4.
The Know Yourself Course
| Main Content | |
|---|---|
| Part 1 Exploring Personality |
|
| Part 2 Understanding Thought |
|
| Parts 3–5 Psychobiological Exercises |
|
(Anthropedia Foundation, 2009)
The second part of the course requires the patient to examine the steps of thought to understand the processes of thought that can lead to greater life satisfaction (Table 5). This extends cognitive-behavioral descriptions of thought to recognize the three major systems of learning and memory that have evolved in the long evolutionary history of human beings (14, 121). Once patients have begun to reflect on and identify what they find satisfying and to realize that their current habits of thinking may be interfering with their health and happiness, modules three to five of the course provide meditations and exercises to help patients activate their prefrontal cortex so that they can be more aware. Each exercise builds on the other but focuses on a different aspect of the being and a different system of learning. Specifically, patients first learn a simple meditation for relaxing the body and calming the emotional brain and then observing their own flow of thoughts to understand without judging or blaming. With this introduction, most people can begin to experience mindfulness and let go of judging and blaming (1, 122, 123). Then the next two modules help to enhance this natural ability.
Table 5.
Functional Properties, Information Processing, and Awareness of the Three Major Steps in Thought in Self-aware Consciousness
| Step in Thought (Functional Properties) | Information Processing | Conditions for Awareness |
|---|---|---|
| Step 1 – The Initial Perception (Colored by outlook, triggered by myriad internal and external cues, subliminal branding, or other powerful social situations) | Episodic Learning – Pre-verbal intuitions direct attention and organize responses schematically according to one’s outlook. These colored and biased responses are experienced as a perception in self-aware consciousness. Sometimes called apperception. | Meta-perception – Usually initial perception is largely unconscious but it is more accessible in contemplation and self-observation of specific situations, which allows perception of shifts in your own outlook and awareness of the triggers of those shifts and their perceptual biases |
| Step 2 – Words (Logical, algorithmic, but supposed facts and propositions are dependent on biases and assumptions inherent in the outlook and initial perception) | Semantic Learning – Verbal labels are produced as interpretations based on the outlook and perception of events in context, sometimes modified by logical rules of inference or social and cultural influences in semantic learning. | Meta-cognition – The interpretive process and retrieval of labels may be subconscious or it may be conscious and declared, and is accessible in states of mindfulness without judging or blaming |
| Step 3 – Automatisms (Alogical, determined by emotional drives and past conditioning varying in strength according to degree of habit formation) | Behavioral Conditioning – The words start to function automatically to produce associatively conditioned feelings and actions. Their repetition leads to further conditioning of habits. | Relaxation – Automatic conditioned responses are prelogical and rooted in past conditions, so they may be inappropriate or self-defeating in the present. These feelings may be quieted by relaxation and letting go. |
(Adapted from Cloninger, 2004 and Know Yourself, Anthropedia Foundation, 2009)
A second meditation is introduced to stimulate perception using all five senses in a way that is harmonious and joyful. Such voluntary activation of integrative sensory processing is designed to facilitate the perception of unity and harmony, which activates the medial and anterior prefrontal cortex and facilitates the development of rational intuition and emotional regulation. Use of rational intuition without judging or blaming is associated with deactivation of dorsolateral prefrontal cortex along with activation of the medial and anterior prefrontal cortex (124). Syntactical functions of self-aware consciousness, such as the perception of harmony and improvisation in music (124, 125), depend on the maturity of the late-myelinating terminal association areas in prefrontal, inferior temporal, and inferior parietal cortex (126, 127). Accordingly, patients are encouraged to practice integrative sensory awareness exercises regularly in a wide variety of their daily activities to promote the perception of unity and connectedness while acting spontaneously, as well as to reduce feelings of loneliness and isolation.
The final meditation focuses on deepening awareness of one’s outlook on life, which is the backdrop that colors a person’s perceptions. The ability to shift outlook on situations or temporal viewpoint is a function of contextual “mental time travel” that depends on self-awareness (124, 128). Enhanced awareness of one’s outlook and its triggers helps a person become free of the momentum of past conditioning and attitudes, thereby facilitating self-transformation. Essentially the meditations provide exercises that instill calm and awareness of each of the three steps in thought. Each meditation helps in this process until a person is aware of all the steps in thought, which reduces his or her vulnerability to unnecessary conflict and dissatisfaction, as described in more detail elsewhere (1, 112).
The practice of most psychiatrists and mental health professionals often permits only short visits and limited time for psychotherapy. The availability of materials such as the Know Yourself course and assessment methods such as the TCI can help to enhance what clinicians can do in their office and help patients by having access to materials that intensify and elevate their clinical experience. We welcome communication and suggestions about how we can further assist you to incorporate a person-centered approach to well-being in your own clinical work.
Footnotes
No relevant financial relationships to disclose.
Contributor Information
C. Robert Cloninger, Director, Center for Well-Being, Washington University School of Medicine, St. Louis, MO
Ada H. Zohar, Chair of Psychology, Department of Behavioral Sciences, Ruppin Academic Center, Israel
Kevin M. Cloninger, President, Anthropedia Foundation, New York
References
- 1.Cloninger CR. Feeling Good: The Science of Well-Being. New York: Oxford University Press; 2004. [Google Scholar]
- 2.Cloninger CR. The science of well-being: an integrated approach to mental health and its disorders. World Psychiatry. 2006;5:71–76. [PMC free article] [PubMed] [Google Scholar]
- 3.Fava GA, Ruini C. Development and characteristics of a well-being enhancing psychotherapeutic strategy: well-being therapy. J Behav Ther Exp Psychiatry. 2003;34:45–63. doi: 10.1016/s0005-7916(03)00019-3. [DOI] [PubMed] [Google Scholar]
- 4.Fava GA, Tomba E. Increasing psychological well-being and resilience by psychotherapeutic methods. J Pers. 2009;77:1903–1934. doi: 10.1111/j.1467-6494.2009.00604.x. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization. Definition of Health in Preamble to the Constitution of the World Health Organization. 2. Geneva, Switzerland: World Health Organization; 1946. [Google Scholar]
- 6.World Health Organization. Mental Health: New Understanding, New Hope. Geneva, Switzerland: World Health Organization; 2001. [Google Scholar]
- 7.Cloninger CR, editor. Personality and Psychopathology (American Psychopathological Association Series) Washington, DC: American Psychiatric Press; 1999b. [Google Scholar]
- 8.Bertisch SM, Wee CC, Phillips RS, McCarthy EP. Alternative mind-body therapies used by adults with medical conditions. J Psychosom Res. 2009;66:511–519. doi: 10.1016/j.jpsychores.2008.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chiesa A, Serretti A. A systematic review of neurobiological and clinical features of mindfulness meditations. Psychol Med. 2009:1–14. doi: 10.1017/S0033291709991747. [DOI] [PubMed] [Google Scholar]
- 10.Servan-Schreiber D. Healing Without Freud or Prozac. London: Rodale International; 2005. [Google Scholar]
- 11.Targ EF, Levine EG. The efficacy of a mind-body-spirit group for women with breast cancer: a randomized controlled trial. Gen Hosp Psychiatry. 2002;24:238–248. doi: 10.1016/s0163-8343(02)00191-3. [DOI] [PubMed] [Google Scholar]
- 12.Cicchetti D, Rogosch FA. Equifinality and multifinality in developmental psychopathology. Dev Psychopathol. 1996;8:597–600. [Google Scholar]
- 13.Cloninger CR, Svrakic NM, Svrakic DM. Role of personality self-organization in development of mental order and disorder. Dev Psychopathol. 1997;9:881–906. doi: 10.1017/s095457949700148x. [DOI] [PubMed] [Google Scholar]
- 14.Cloninger CR. The evolution of human brain functions: the functional structure of human consciousness. Aust NZ J Psychiatry. 2009;43:994–1006. doi: 10.3109/00048670903270506. [DOI] [PubMed] [Google Scholar]
- 15.Eisenberg L. The social construction of mental illness. Psychol Med. 1988;18:1–9. doi: 10.1017/s0033291700001823. [DOI] [PubMed] [Google Scholar]
- 16.Eisenberg L. Mindlessness and brainlessness in psychiatry. Br J Psychiatry. 1986;148:497–508. doi: 10.1192/bjp.148.5.497. [DOI] [PubMed] [Google Scholar]
- 17.Eisenberg L. Is psychiatry more mindful or brainier than it was a decade ago? Br J Psychiatry. 2000;176:1–5. doi: 10.1192/bjp.176.1.1. [DOI] [PubMed] [Google Scholar]
- 18.Farmer A, Mahmood A, Redman K, Harris T, Sadler S, McGuffin P. A sib-pair study of the Temperament and Character Inventory scales in major depression. Arch Gen Psychiatry. 2003;60:490–496. doi: 10.1001/archpsyc.60.5.490. [DOI] [PubMed] [Google Scholar]
- 19.Nery FG, Hatch JP, Glahn DC, Nicoletti MA, Monkul ES, Najt P, Fonseca M, Bowden CL, Cloninger CR, Soares JC. Temperament and character traits in patients with bipolar disorder and associations with comorbid alcoholism or anxiety disorders. J Psychiatr Res. 2008;42:569–577. doi: 10.1016/j.jpsychires.2007.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nery FG, Hatch JP, Nicoletti MA, Monkul ES, Najt P, Matsuo K, Cloninger CR, Soares JC. Temperament and character traits in major depressive disorder: influence of mood state and recurrence of episodes. Depress Anxiety. 2009;26:382–388. doi: 10.1002/da.20478. [DOI] [PubMed] [Google Scholar]
- 21.Smith MJ, Cloninger CR, Harms MP, Csernansky JG. Temperament and character as schizophrenia-related endophenotypes in non-psychotic siblings. Schizophr Res. 2008;104:198–205. doi: 10.1016/j.schres.2008.06.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cortés MJ, Valero J, Gutiérrez-Zotes JA, Hernández A, Moreno L, Jariod M, Martorell L, Vilella E, Labad A. Psychopathology and personality traits in psychotic patients and their first-degree relatives. Eur Psychiatry. 2009;24:476–482. doi: 10.1016/j.eurpsy.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 23.Eklund M, Hansson L, Bengtsson-Tops A. The influence of temperament and character on functioning and aspects of psychological health among people with schizophrenia. Eur Psychiatry. 2004;19:34–41. doi: 10.1016/j.eurpsy.2003.07.008. [DOI] [PubMed] [Google Scholar]
- 24.Gillespie NA, Cloninger CR, Heath AC, Martin NG. The genetic and environmental relationship between Cloninger’s dimensions of temperament and character. Pers Individ Differences. 2003;35:1931–1946. doi: 10.1016/S0191-8869(03)00042-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Abrams KY, Yune SK, Kim SJ, Jeon HJ, Han SJ, Hwang J, Sung YH, Lee KJ, Lyoo IK. Trait and state aspects of harm avoidance and its implication for treatment in major depressive disorder, dysthymic disorder, and depressive personality disorder. Psychiatry Clin Neurosci. 2004;58:240–248. doi: 10.1111/j.1440-1819.2004.01226.x. [DOI] [PubMed] [Google Scholar]
- 26.de Winter RF, Wolterbeek R, Spinhoven P, Zitman FG, Goekoop JG. Character and temperament in major depressive disorder and a highly anxious-retarded subtype derived from melancholia. Compr Psychiatry. 2007;48:426–435. doi: 10.1016/j.comppsych.2007.04.002. [DOI] [PubMed] [Google Scholar]
- 27.Hansenne M, Reggers J, Pinto E, Kjiri K, Ajamier A, Ansseau M. Temperament and Character Inventory (TCI) and depression. J Psychiatr Res. 1999;33:31–36. doi: 10.1016/s0022-3956(98)00036-3. [DOI] [PubMed] [Google Scholar]
- 28.Joffe RT, Bagby RM, Levitt AJ, Regan JJ, Parker JD. The Tridimensional Personality Questionnaire in major depression. Am J Psychiatry. 1993;150:959–960. doi: 10.1176/ajp.150.6.959. [DOI] [PubMed] [Google Scholar]
- 29.Mulder RT, Joyce PR, Frampton CM, Luty SE, Sullivan PF. Six months of treatment for depression: outcome and predictors of the course of illness. Am J Psychiatry. 2006;163:95–100. doi: 10.1176/appi.ajp.163.1.95. [DOI] [PubMed] [Google Scholar]
- 30.Quilty LC, Godfrey KM, Kennedy SH, Bagby RM. Harm avoidance as a mediator of treatment response to antidepressant treatment of patients with major depression. Psychother Psychosom. 2010;79:116–122. doi: 10.1159/000276372. [DOI] [PubMed] [Google Scholar]
- 31.Mulder RT, Frampton CM, Luty SE, Joyce PR. Eighteen months of drug treatment for depression: predicting relapse and recovery. J Affect Disord. 2009;114:263–270. doi: 10.1016/j.jad.2008.08.002. [DOI] [PubMed] [Google Scholar]
- 32.Ongur D, Farabaugh A, Iosifescu DV, Perlis R, Fava M. Tridimensional personality questionnaire factors in major depressive disorder: relationship to anxiety disorder comorbidity and age of onset. Psychother Psychosom. 2005;74:173–178. doi: 10.1159/000084002. [DOI] [PubMed] [Google Scholar]
- 33.Joyce PR, Mulder RT, Cloninger CR. Temperament predicts clomipramine and desipramine response in major depression. J Affect Disord. 1994;30:35–46. doi: 10.1016/0165-0327(94)90149-x. [DOI] [PubMed] [Google Scholar]
- 34.Tome MB, Cloninger CR, Watson JP, Isaac MT. Serotonergic autoreceptor blockade in the reduction of antidepressant latency: personality variables and response to paroxetine and pindolol. J Affect Disord. 1997;44:101–109. doi: 10.1016/s0165-0327(97)00030-x. [DOI] [PubMed] [Google Scholar]
- 35.Hruby R, Nosalova G, Ondrejka I, Preiss M. Personality changes during antidepressant treatment. Psychiatr Danub. 2009;21:25–32. [PubMed] [Google Scholar]
- 36.Kaye W, Gendall K, Strober M. Serotonin neuronal function and selective serotonin reuptake inhibitor treatment in anorexia and bulimia nervosa. Biol Psychiatry. 1998;44:825–838. doi: 10.1016/s0006-3223(98)00195-4. [DOI] [PubMed] [Google Scholar]
- 37.Pezawas L, Meyer-Lindenberg A, Drabant EM, Verchinski BA, Munoz KE, Kolachana BS, Egan MF, Mattay VS, Hariri AR, Weinberger DR. 5-HT-TLPR polymorphism impacts human cingulate-amygdala interactions: a genetic susceptibility mechanism for depression. Nat Neurosci. 2005;8:828–834. doi: 10.1038/nn1463. [DOI] [PubMed] [Google Scholar]
- 38.Janowsky DS, Morter S, Hong L, et al. Myers Briggs Type Indicator and Tridimensional Personality Questionnaire differences between bipolar patients and unipolar depressed patients. Bipolar Disord. 1999;1:98–108. doi: 10.1034/j.1399-5618.1999.010207.x. [DOI] [PubMed] [Google Scholar]
- 39.Young LT, Bagby RM, Cooke RG, Parker JD, Levitt AJ, Joffe RT. A comparison of Tridimensional Personality Questionnaire dimensions in bipolar disorder and unipolar depression. Psychiatry Res. 1995;58:139–143. doi: 10.1016/0165-1781(95)02684-o. [DOI] [PubMed] [Google Scholar]
- 40.Csorba J, Dinya E, Ferencz E, Steiner P, Bertalan G, Zsadon A. Novelty seeking: difference between suicidal and non-suicidal Hungarian adolescent outpatients suffering from depression. J Affect Disord. 2010;120:217–220. doi: 10.1016/j.jad.2009.03.008. [DOI] [PubMed] [Google Scholar]
- 41.Akiskal HS, Mendlowicz MV, Jean-Louis G, Rapaport MH, Kelsoe JR, Gillin JC, Smith TL. TEMPS-A: validation of a short version of a self-rated instrument designed to measure variations in temperament. J Affect Disord. 2005;85:45–52. doi: 10.1016/j.jad.2003.10.012. [DOI] [PubMed] [Google Scholar]
- 42.Maremmani I, Akiskal HS, Signoretta S, Liguori A, Perugi G, Cloninger R. The relationship of Kraepelian affective temperaments (as measured by TEMPS-I) to the tridimensional personality questionnaire (TPQ) J Affect Disord. 2005;85:17–27. doi: 10.1016/S0165-0327(03)00099-5. [DOI] [PubMed] [Google Scholar]
- 43.Olvera RL, Fonseca M, Caetano SC, Hatch JP, Hunter K, Nicoletti M, Pliszka SR, Cloninger CR, Soares JC. Assessment of personality dimensions in children and adolescents with bipolar disorder using the Junior Temperament and Character Inventory. J Child Adolesc Psychopharmacol. 2009;19:13–21. doi: 10.1089/cap.2008.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tillman R, Geller B, Craney JL, Bolhofner K, Williams M, Zimerman B, Frazier J, Beringer L. Temperament and character factors in a prepubertal and early adolescent bipolar disorder phenotype compared to attention deficit hyperactive and normal controls. J Child Adolesc Psychopharmacol. 2003;13:531–543. doi: 10.1089/104454603322724922. [DOI] [PubMed] [Google Scholar]
- 45.Osher Y, Cloninger CR, Belmaker RH. TPQ in euthymic manic-depressive patients. J Psychiatr Res. 1996;30:353–357. doi: 10.1016/0022-3956(96)00023-4. [DOI] [PubMed] [Google Scholar]
- 46.Osher Y, Lefkifker E, Kotler M. Low persistence in euthymic manic-depressive patients: a replication. J Affect Disord. 1999;53:87–90. doi: 10.1016/s0165-0327(98)00075-5. [DOI] [PubMed] [Google Scholar]
- 47.Savitz J, van der Merwe L, Ramesar R. Dysthymic and anxiety-related personality traits in bipolar spectrum illness. J Affect Disord. 2008;109:305–311. doi: 10.1016/j.jad.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 48.Strakowski SM, Stoll AL, Tohen M, Faedda GL, Goodwin DC. The Tridimensional Personality Questionnaire as a predictor of six-month outcome in first episode mania. Psychiatry Res. 1993;48:1–8. doi: 10.1016/0165-1781(93)90107-r. [DOI] [PubMed] [Google Scholar]
- 49.Strakowski SM, Dunayevich E, Keck PE, Jr, McElroy SL. Affective state dependence of the Tridimensional Personality Questionnaire. Psychiatry Res. 1995;57:209–214. doi: 10.1016/0165-1781(95)02655-g. [DOI] [PubMed] [Google Scholar]
- 50.Conrad R, Wegener I, Imbierowicz K, Liedtke R, Geiser F. Alexithymia, temperament and character as predictors of psychopathology in patients with major depression. Psychiatry Res. 2009;165:137–144. doi: 10.1016/j.psychres.2007.10.013. [DOI] [PubMed] [Google Scholar]
- 51.Cowley DS, Roy-Byrne PP, Greenblatt DJ, Hommer DW. Personality and benzodiazepine sensitivity in anxious patients and control subjects. Psychiatry Res. 1993;47:151–162. doi: 10.1016/0165-1781(93)90045-i. [DOI] [PubMed] [Google Scholar]
- 52.Pfohl B, Black D, Noyes R, Jr, Kelley M, Blum N. A test of the tridimensional personality theory: association with diagnosis and platelet imipramine binding in obsessive-compulsive disorder. Biol Psychiatry. 1990;28:41–46. doi: 10.1016/0006-3223(90)90430-a. [DOI] [PubMed] [Google Scholar]
- 53.Rettew DC, Doyle AC, Kwan M, Stanger C, Hudziak JJ. Exploring the boundary between temperament and generalized anxiety disorder: a receiver operating characteristic analysis. J Anxiety Disord. 2006;20:931–945. doi: 10.1016/j.janxdis.2006.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Starcevic V, Uhlenhuth EH, Fallon S, Pathak D. Personality dimensions in panic disorder and generalized anxiety disorder. J Affect Disord. 1996;37:75–79. doi: 10.1016/0165-0327(95)00058-5. [DOI] [PubMed] [Google Scholar]
- 55.Stein MB, Chartier MJ, Lizak MV, Jang KL. Familial aggregation of anxiety-related quantitative traits in generalized social phobia: clues to understanding “disorder” heritability? Am J Med Genet. 2001;105:79–83. [PubMed] [Google Scholar]
- 56.Gothelf D, Aharonovsky O, Horesh N, Carty T, Apter A. Life events and personality factors in children and adolescents with obsessive-compulsive disorder and other anxiety disorders. Compr Psychiatry. 2004;45:192–198. doi: 10.1016/j.comppsych.2004.02.010. [DOI] [PubMed] [Google Scholar]
- 57.Hofmann SG, Bitran S. Sensory-processing sensitivity in social anxiety disorder: relationship to harm avoidance and diagnostic subtypes. J Anxiety Disord. 2007;21:944–954. doi: 10.1016/j.janxdis.2006.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kennedy BL, Schwab JJ, Hyde JA. Defense styles and personality dimensions of research subjects with anxiety and depressive disorders. Psychiatr Q. 2001;72:251–262. doi: 10.1023/a:1010353116016. [DOI] [PubMed] [Google Scholar]
- 59.Corr PJ, Wilson GD, Fotiadou M, Kumari V, Gray NS, Checkley S, Gray JA. Personality and affective modulation of the startle reflex. Pers Individ Differences. 1995;19:543–553. [Google Scholar]
- 60.Corr PJ, Kumari V, Wilson GD, Checkley S, Gray JA. Harm avoidance and affective modulation of the startle reflex: a replication. Pers Individ Differences. 1997;22:591–593. [Google Scholar]
- 61.Brans B, van den Eynde F, Audenaert K, Vervaet M, van Daele K, van Heeringen C, Dierckx RA. Depression and anxiety during isolation and radionuclide therapy. Nucl Med Commun. 2003;24:881–886. doi: 10.1097/01.mnm.0000084586.29433.83. [DOI] [PubMed] [Google Scholar]
- 62.Lochner C, Hemmings S, Seedat S, Kinnear C, Schoeman R, Annerbrink K, Olsson M, Eriksson E, Moolman-Smook J, Allgulander C, Stein DJ. Genetics and personality traits in patients with social anxiety disorder: a case-control study in South Africa. Eur Neuropsychopharmacol. 2007;17:321–327. doi: 10.1016/j.euroneuro.2006.06.010. [DOI] [PubMed] [Google Scholar]
- 63.Marchesi C, De Panfilis C, Cantoni A, Giannelli MR, Maggini C. Effect of pharmacological treatment on temperament and character in panic disorder. Psychiatry Res. 2008;158:147–154. doi: 10.1016/j.psychres.2006.08.009. [DOI] [PubMed] [Google Scholar]
- 64.Wachleski C, Salum GA, Blaya C, Kipper L, Paludo A, Salgado AP, Manfro GG. Harm avoidance and self-directedness as essential features of panic disorder patients. Compr Psychiatry. 2008;49:476–481. doi: 10.1016/j.comppsych.2008.03.003. [DOI] [PubMed] [Google Scholar]
- 65.Prasko J, Houbová P, Novák T, Záleský R, Espa-Cervená K, Pasková B, Vyskocilová J. Influence of personality disorder on the treatment of panic disorder—comparison study. Neuro Endocrinol Lett. 2005;26:667–674. [PubMed] [Google Scholar]
- 66.Calvo R, Lázaro L, Castro-Fornieles J, Font E, Moreno E, Toro J. Obsessive-compulsive personality disorder traits and personality dimensions in parents of children with obsessive-compulsive disorder. Eur Psychiatry. 2009;24:201–206. doi: 10.1016/j.eurpsy.2008.11.003. [DOI] [PubMed] [Google Scholar]
- 67.Ettelt S, Grabe HJ, Ruhrmann S, Buhtz F, Hochrein A, Kraft S, Pukrop R, Klosterkötter J, Falkai P, Maier W, John U, Freyberger HJ, Wagner M. Harm avoidance in subjects with obsessive-compulsive disorder and their families. J Affect Disord. 2008;107:265–269. doi: 10.1016/j.jad.2007.08.017. [DOI] [PubMed] [Google Scholar]
- 68.Zohar AH, Ebstein RP, Pauls DL. TPQ profiles of patients with OCD and GTS and their first degree relatives. World J Biol Psychiatry. 2005;6:151–152. [Google Scholar]
- 69.Alonso P, Menchón JM, Jiménez S, Segalàs J, Mataix-Cols D, Jaurrieta N, Labad J, Vallejo J, Cardoner N, Pujol J. Personality dimensions in obsessive-compulsive disorder: relation to clinical variables. Psychiatry Res. 2008;157:159–168. doi: 10.1016/j.psychres.2006.06.003. [DOI] [PubMed] [Google Scholar]
- 70.Cruz-Fuentes C, Blas C, Gonzalez L, Camarena B, Nicolini H. Severity of obsessive-compulsive symptoms is related to self-directedness character trait in obsessive-compulsive disorder. CNS Spectr. 2004;9:607–612. doi: 10.1017/s1092852900002789. [DOI] [PubMed] [Google Scholar]
- 71.Kim SJ, Kang JI, Kim CH. Temperament and character in subjects with obsessive-compulsive disorder. Compr Psychiatry. 2009;50:567–572. doi: 10.1016/j.comppsych.2008.11.009. [DOI] [PubMed] [Google Scholar]
- 72.Lyoo IK, Lee DW, Kim YS, Kong SW, Kwon JS. Patterns of temperament and character in subjects with obsessive-compulsive disorder. J Clin Psychiatry. 2001;62:637–641. doi: 10.4088/jcp.v62n0811. [DOI] [PubMed] [Google Scholar]
- 73.Fukuda S, Kuratsune H, Tajima S, Takashima S, Yamagutchi K, Nishizawa Y, Watanabe Y. Premorbid personality in chronic fatigue syndrome as determined by the Temperament and Character Inventory. Compr Psychiatry. 2010;51:78–85. doi: 10.1016/j.comppsych.2009.02.002. [DOI] [PubMed] [Google Scholar]
- 74.Cloninger CR, Sigvardsson S, Bohman M. Childhood personality predicts alcohol abuse in young adults. Alcohol Clin Exp Res. 1988;12:494–505. doi: 10.1111/j.1530-0277.1988.tb00232.x. [DOI] [PubMed] [Google Scholar]
- 75.Cloninger CR, Sigvardsson S, Przybeck TR, Svrakic DM. Personality antecedents of alcoholism in a national area probability sample. Eur Arch Psychiatry Clin Neurosci. 1995;245:239–244. doi: 10.1007/BF02191803. [DOI] [PubMed] [Google Scholar]
- 76.Grucza RA, Przybeck TR, Cloninger CR. Screening for alcohol problems: an epidemiological perspective and implications for primary care. Mo Med. 2008;105:67–71. [PMC free article] [PubMed] [Google Scholar]
- 77.Howard MO, Kivlahan D, Walker RD. Cloninger’s tridimensional theory of personality and psychopathology: applications to substance use disorders. J Stud Alcohol. 1997;58:48–66. doi: 10.15288/jsa.1997.58.48. [DOI] [PubMed] [Google Scholar]
- 78.Cloninger CR. The genetics of substance abuse. In: Galanter M, Kleber HD, editors. Textbook of Substance Dependence. Washington, DC: American Psychiatric Press; 1999. pp. 59–66. [Google Scholar]
- 79.Cunningham-Williams RM, Grucza RA, Cottler LB, Cottler LB, Womack SB, Books SJ, Przybeck TR, Spitznagel EL, Cloninger CR. Prevalence and predictors of pathological gambling: results from the St. Louis personality, health and lifestyle (SLPHL) study. J Psychiatr Res. 2005;39:377–390. doi: 10.1016/j.jpsychires.2004.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Fassino S, Leombruni P, Pierò A, Daga GA, Amianto F, Rovera G, Rovera GG. Temperament and character in obese women with and without binge eating disorder. Compr Psychiatry. 2002;43:431–437. doi: 10.1053/comp.2002.35906. [DOI] [PubMed] [Google Scholar]
- 81.Grucza RA, Przybeck TR, Cloninger CR. Prevalence and correlates of binge eating disorder in a community sample. Compr Psychiatry. 2007;48:124–131. doi: 10.1016/j.comppsych.2006.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kim SW, Grant JE. Personality dimensions in pathological gambling disorder and obsessive-compulsive disorder. Psychiatry Res. 2001;104:205–212. doi: 10.1016/s0165-1781(01)00327-4. [DOI] [PubMed] [Google Scholar]
- 83.Grucza RA, Robert Cloninger C, Bucholz KK, Constantino JN, Schuckit MI, Dick DM, Bierut LJ. Novelty seeking as a moderator of familial risk for alcohol dependence. Alcohol Clin Exp Res. 2006;30:1176–1183. doi: 10.1111/j.1530-0277.2006.00133.x. [DOI] [PubMed] [Google Scholar]
- 84.Leventhal AM, Waters AJ, Boyd S, Moolchan ET, Heishman SJ, Lerman C, Pickworth WB. Associations between Cloninger’s temperament dimensions and acute tobacco withdrawal. Addict Behav. 2007;32:2976–2989. doi: 10.1016/j.addbeh.2007.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Pomerleau CS, Pomerleau OF, Flessland KA, Basson SM. Relationship of Tridimensional Personality Questionnaire scores and smoking variables in female and male smokers. J Subst Abuse. 1992;4:143–154. doi: 10.1016/0899-3289(92)90014-o. [DOI] [PubMed] [Google Scholar]
- 86.Anderson CB, Joyce PR, Carter FA, McIntosh VV, Bulik CM. The effect of cognitive-behavioral therapy for bulimia nervosa on temperament and character as measured by the temperament and character inventory. Compr Psychiatry. 2002;43:182–188. doi: 10.1053/comp.2002.32359. [DOI] [PubMed] [Google Scholar]
- 87.Fassino S, Amianto F, Gramaglia C, Facchini F, Abbate Daga G. Temperament and character in eating disorders: ten years of studies. Eat Weight Disord. 2004;9:81–90. doi: 10.1007/BF03325050. [DOI] [PubMed] [Google Scholar]
- 88.Klump KL, Strober M, Bulik CM, Thornton L, Johnson C, Devlin B, Fichter MM, Halmi KA, Kaplan AS, Woodside DB, Crow S, Mitchell J, Rotondo A, Keel PK, Berrettini WH, Plotnicov K, Pollice C, Lilenfeld LR, Kaye WH. Personality characteristics of women before and after recovery from an eating disorder. Psychol Med. 2004;34:1407–1418. doi: 10.1017/s0033291704002442. [DOI] [PubMed] [Google Scholar]
- 89.Bachner-Melman R, Zohar AH, Ebstein RP. An examination of cognitive versus behavioral components of recovery from anorexia nervosa. J Nerv Ment Dis. 2006;194:697–703. doi: 10.1097/01.nmd.0000235795.51683.99. [DOI] [PubMed] [Google Scholar]
- 90.Diaz-Marsa M, Carrasco JL, Saiz J. A study of temperament and personality in anorexia and bulimia nervosa. J Pers Disord. 2000;14:352–359. doi: 10.1521/pedi.2000.14.4.352. [DOI] [PubMed] [Google Scholar]
- 91.Fassino S, Abbate-Daga G, Amianto F, Leombruni P, Boggio S, Rovera GG. Temperament and character profile of eating disorders: a controlled study with the Temperament and Character Inventory. Int J Eat Disord. 2002;32:412–425. doi: 10.1002/eat.10099. [DOI] [PubMed] [Google Scholar]
- 92.Fassino S, Abbate-Daga G, Amianto F, Facchini F, Rovera GG. Eating psychopathology and personality in eating disorders. Epidemiol Psichiatr Soc. 2003;12:293–300. doi: 10.1017/s1121189x00003109. [DOI] [PubMed] [Google Scholar]
- 93.Kleifield EI, Sunday S, Hurt S, Halmi KA. The Tridimensional Personality Questionnaire: an exploration of personality traits in eating disorders. J Psychiatr Res. 1994;28:413–423. doi: 10.1016/0022-3956(94)90001-9. [DOI] [PubMed] [Google Scholar]
- 94.Vervaet M, van Heeringen C, Audenaert K. Personality-related characteristics in restricting versus binging and purging eating disordered patients. Compr Psychiatry. 2004;45:37–43. doi: 10.1016/j.comppsych.2003.09.008. [DOI] [PubMed] [Google Scholar]
- 95.Karwautz A, Troop NA, Rabe-Hesketh S, Collier DA, Treasure JL. Personality disorders and personality dimensions in anorexia nervosa. J Pers Disord. 2003;17:73–85. doi: 10.1521/pedi.17.1.73.24057. [DOI] [PubMed] [Google Scholar]
- 96.Gendall KA, Joyce PR, Sullivan PF, Bulik CM. Personality and dimensions of dietary restraint. Int J Eat Disord. 1998;24:371–379. doi: 10.1002/(sici)1098-108x(199812)24:4<371::aid-eat4>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 97.Abbate-Daga G, Pierò A, Gramaglia C, Fassino S. Factors related to severity of vomiting behaviors in bulimia nervosa. Psychiatry Res. 2005;134:75–84. doi: 10.1016/j.psychres.2004.01.013. [DOI] [PubMed] [Google Scholar]
- 98.Fassino S, Abbate-Daga G, Pierò A, Leombruni P, Rovera GG. Dropout from brief psychotherapy within a combination treatment in bulimia nervosa: role of personality and anger. Psychother Psychosom. 2003;72:203–210. doi: 10.1159/000070784. [DOI] [PubMed] [Google Scholar]
- 99.Fassino S, Daga GA, Pierò A, Leombruni P, Rovera GG. Anger and personality in eating disorders. J Psychosom Res. 2001;51:757–764. doi: 10.1016/s0022-3999(01)00280-x. [DOI] [PubMed] [Google Scholar]
- 100.Bulik CM, Sullivan PF, Fear JL, Pickering A. Outcome of anorexia nervosa: eating attitudes, personality, and parental bonding. Int J Eat Disord. 2000;28:139–147. doi: 10.1002/1098-108x(200009)28:2<139::aid-eat2>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 101.De Panfilis C, Cero S, Torre M, Salvatore P, Dall’Aglio E, Adorni A, Maggini C. Utility of the temperament and character inventory (TCI) in outcome prediction of laparoscopic adjustable gastric banding: preliminary report. Obes Surg. 2006;16:842–847. doi: 10.1381/096089206777822278. [DOI] [PubMed] [Google Scholar]
- 102.Leombruni P, Pierò A, Dosio D, Novelli A, Abbate-Daga G, Morino M, Toppino M, Fassino S. Psychological predictors of outcome in vertical banded gastroplasty: a 6 months prospective pilot study. Obes Surg. 2007;17:941–948. doi: 10.1007/s11695-007-9173-4. [DOI] [PubMed] [Google Scholar]
- 103.Cloninger CR. Implications of comorbidity for the classification of mental disorders: the need for a psychobiology of coherence. In: Maj M, Gaebel W, López-Ibor JJ, Sartorius N, editors. Psychiatric Diagnosis and Classification. New York: John Wiley & Sons; 2002. pp. 79–105. [Google Scholar]
- 104.Battaglia M, Przybeck TR, Bellodi L, Cloninger CR. Temperament dimensions explain the comorbidity of psychiatric disorders. Compr Psychiatry. 1996;37:292–298. doi: 10.1016/s0010-440x(96)90008-5. [DOI] [PubMed] [Google Scholar]
- 105.Cloninger CR. Foreword. In: O’Donohue WT, Fowler KA, Lilienfeld SO, editors. Personality Disorders: Toward the DSM-V. Los Angeles: Sage Publications; 2007. pp. vii–xvi. [Google Scholar]
- 106.Zohar AH, Cloninger CR. Psychometric properties of the TCI-R140 in Hebrew. Eur J Pers Assess. doi: 10.1207/s15327752jpa8501_04. (in press) [DOI] [PubMed] [Google Scholar]
- 107.Watson D, Clark LA, Carey G. Positive and negative affectivity and their relation to anxiety and depressive disorders. J Abnorm Psychol. 1988;97:346–353. doi: 10.1037//0021-843x.97.3.346. [DOI] [PubMed] [Google Scholar]
- 108.Pavot W, Diener E. Review of the Satisfaction with Life Scale. Psychol Assess. 1993;5:149–161. [Google Scholar]
- 109.Zimet GD, Powell SS, Farley GK, Werkman S, Berkoff KA. Psychometric characteristics of the Multidimensional Scale of Perceived Social Support. J Pers Assess. 1990;55:610–617. doi: 10.1080/00223891.1990.9674095. [DOI] [PubMed] [Google Scholar]
- 110.Knauper B, Turner PA. Measuring health: improving the validity of health assessments. Qual Life Res. 2003;12(Suppl 1):81–89. doi: 10.1023/a:1023589907955. [DOI] [PubMed] [Google Scholar]
- 111.Ruini C, Ottolini F, Rafanelli C, Tossani E, Ryff CD, Fava GA. The relationship of psychological well-being to distress and personality. Psychother Psychosom. 2003;72:268–275. doi: 10.1159/000071898. [DOI] [PubMed] [Google Scholar]
- 112.Wong KM, Cloninger CR. A person-centered approach to clinical practice. Focus. 2010;8:199–215. doi: 10.1176/foc.8.2.foc199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Finn SE, Tonsager ME. Therapeutic effects of providing MMPI-2 test feedback to college students awaiting therapy. Psychol Assess. 1992;4:278–287. [Google Scholar]
- 114.Finn SE, Tonsager ME. Information-gathering and therapeutic models of assessment: complementary paradigms. Psychol Assess. 1997;9:374–385. [Google Scholar]
- 115.Hilsenroth MJ, Peters EJ, Ackerman SJ. The development of therapeutic alliance during psychological assessment: patient and therapist perspectives across treatment. J Pers Assess. 2004;83:332–344. doi: 10.1207/s15327752jpa8303_14. [DOI] [PubMed] [Google Scholar]
- 116.Diener E, Biswas-Diener R. Happiness: Unlocking the Secrets of Psychological Wealth. Malden, MA: Blackwell Publishing; 2008. [Google Scholar]
- 117.Gusnard DA, Akbudak E, Shulman GL, Raichle ME. Medial prefrontal cortex and self-referential mental activity: relation to a default mode of brain function. Proc Natl Acad Sci USA. 2001;98:4259–4264. doi: 10.1073/pnas.071043098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Koechlin E, Corrado G, Pietrini P, Grafman J. Dissociating the role of the medial and lateral anterior prefrontal cortex in human planning. Proc Natl Acad Sci USA. 2000;97:7651–7656. doi: 10.1073/pnas.130177397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Limb CJ, Braun AR. Neural substrates of spontaneous musical performance: an FMRI study of jazz improvisation. PLoS One. 2008;3:e1679. doi: 10.1371/journal.pone.0001679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Moll J, Krueger F, Zahn R, Pardini M, de Oliveira-Souza R, Grafman J. Human fronto-mesolimbic networks guide decisions about charitable donation. Proc Natl Acad Sci USA. 2006;103:15623–15628. doi: 10.1073/pnas.0604475103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Tulving E. Multiple memory systems and consciousness. Hum Neurobiol. 1087;6:67–80. [PubMed] [Google Scholar]
- 122.Krasner MS, Epstein RM, Beckman H, Suchman AL, Chapman B, Mooney CJ, Quill TE. Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA. 2009;302:1284–1293. doi: 10.1001/jama.2009.1384. [DOI] [PubMed] [Google Scholar]
- 123.Teasdale JD, Segal ZV, Williams JM, Ridgeway VA, Soulsby JM, Lau MA. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. J Consult Clin Psychol. 2000;68:615–623. doi: 10.1037//0022-006x.68.4.615. [DOI] [PubMed] [Google Scholar]
- 124.Lind S, Bowler D. Episodic memory and autonoetic consciousness in autism specrum disorders: the roles of self-awareness, representation abilities, and temporal cognition. In: Boucher JM, Bowler DM, editors. Memory in Autism: Theory and Evidence. Cambridge, UK: Cambridge University Press; 2008. pp. 166–187. [Google Scholar]
- 125.Schellenberg EG, Bigand E, Poulin-Charronnat B, Garnier C, Stevens C. Children’s implicit knowledge of harmony in Western music. Dev Sci. 2005;8:551–566. doi: 10.1111/j.1467-7687.2005.00447.x. [DOI] [PubMed] [Google Scholar]
- 126.Fehr E, Bernhard H, Rockenbach B. Egalitarianism in young children. Nature. 2008;454:1079–1083. doi: 10.1038/nature07155. [DOI] [PubMed] [Google Scholar]
- 127.Levine B. Autobiographical memory and the self in time: brain lesion effects, functional neuroanatomy, and lifespan development. Brain Cogn. 2004;55:54–68. doi: 10.1016/S0278-2626(03)00280-X. [DOI] [PubMed] [Google Scholar]
- 128.Tulving E. Episodic memory: from mind to brain. Annu Rev Psychol. 2002;53:1–25. doi: 10.1146/annurev.psych.53.100901.135114. [DOI] [PubMed] [Google Scholar]