Abstract
Purpose
To examine bereavement mental health service use, barriers to use, and factors associated with use in parents bereaved by cancer.
Patients and Methods
A multicenter, cross-sectional study of 120 parents bereaved by cancer between 6 months and 6 years after their loss was performed. Parents completed self-report assessments of mental health service use and barriers, prolonged grief, depression, anxiety, attachment styles, and sense of meaning by phone, in person, or on their own.
Results
Forty-one percent of bereaved parents were currently using mental health services (talk therapy, psychotropic medication, and/or a support group), most commonly within the first 2 years after their loss. Talk therapy was the most frequently used service, although 36% of parents who discontinued therapy did so because it was not helpful. Forty percent of parents who wanted bereavement support reported they were not receiving services. The most common barriers to service use were that it was too painful to speak about the loss (64%) and too difficult to find help (60%). Factors associated with current mental health service use included more recent loss, prior mental health service use, subclinical/increased depression, insecure attachment styles, and a decreased sense of meaning. Minority parents were more likely to have unmet needs than nonminority parents.
Conclusion
Parents appear to need, want, and often access bereavement mental health services, which could be offered in oncology settings. However, barriers to service use must be addressed, particularly for those with more debilitating grief symptoms and for minorities. High treatment dropout rates suggest the importance of improving retention, training providers, and developing effective grief interventions.
INTRODUCTION
It is widely accepted that grief after the loss of a child is more intense and persistent than after other types of bereavement.1–3 Given this, bereaved parents are believed to be at heightened risk for psychological distress, including prolonged grief disorder (PGD),4,5 a syndrome characterized by unremitting, severe, and debilitating grief. This has implications for service provision, particularly in pediatric oncology settings. Pediatric cancer care facilities have the opportunity to provide continuity of care to the family, but because staff and time are often limited, questions are common about how much of the available resources should be devoted to bereavement aftercare and for how long.6 This study describes mental health service use (MHSU) and common barriers to accessing services in a sample of parents bereaved by cancer to contribute to the discussion on how best to provide bereavement aftercare to grieving parents.
It is commonly believed that, despite the psychosocial challenges they face, bereaved parents underuse mental health services after the death of their child.7–9 However, studies of rates of MHSU in bereaved parents are limited. We hypothesize that an important barrier to parents seeking services is treatment fearfulness,10 especially those who are experiencing debilitating grief reactions such as PGD, who may avoid psychosocial services because the thought of confronting the unacceptable reality that their child has died and tolerating the intense pain associated with their loss is so aversive.
In fact, some believe that parents who lost a child to cancer do not seek services affiliated with the institution at which their child was treated to avoid painful reminders of their loss. However, parents often develop close relationships with the staff during their child's intensive treatment,11,12 so it is not surprising that studies have shown that parents bereaved by cancer commonly want continued connection with the hospital following their loss.11,13 The absence of continued care by hospital providers may be an additional loss to grieve.11,13,14
Factors that impact mental health service underuse in the general population are likely also at play among bereaved parents who may not be using services because of financial limitations, the general stigma of MHSU, lack of readiness to change, the unavailability of professional services, or the availability of support from nonprofessional sources.10 A further deterrent for bereaved parents may be a belief that service providers cannot do much to assist them; indeed, past research has suggested that few bereaved parents who used mental health services in the first year of bereavement found them to be helpful.1
Understanding whether and under what circumstances bereaved parents use services is critical to the development of hospital-based and community bereavement programs and to improving access to bereavement services for this vulnerable population. However, there is limited research on rates of and barriers to MHSU and factors associated with use in bereaved parents15 and none focusing specifically on parents bereaved by cancer. This study aimed to address that gap and to examine our hypothesis that treatment fearfulness is a barrier to MHSU.
PATIENTS AND METHODS
Study Procedures
Bereaved parents whose child was treated for cancer at Memorial Sloan Kettering Cancer Center or the National Cancer Institute Pediatric Oncology Branch were recruited for this cross-sectional study from November 2009 through September 2012. Parents were mailed invitation letters approved by an institutional review board for a study of grief, meaning, and adjustment in parents bereaved by cancer. The letter stated that they would receive a phone call from research staff and included a self-addressed, stamped postcard to return if they preferred not to be further contacted. Consenting parents were given the option of completing study measures in person, by telephone, or on their own. Participants received $25 compensation.
Participants
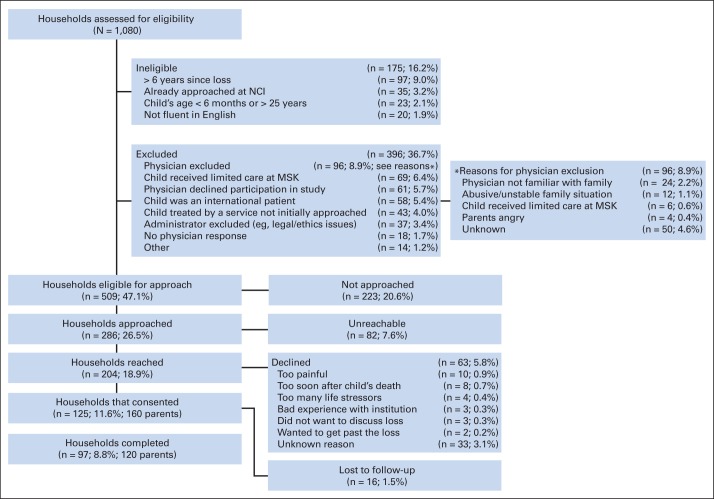
Biologic, adoptive, and step-parents were eligible if they had lost a child age 6 months to 25 years to cancer, were 6 months to 6 years postloss, and spoke English fluently. One or both parents in a given household could participate. We screened the medical records of 1,080 deceased children. Some households were excluded by hospital administrators (n = 37; 3%) or the child's treating physician (n = 96; 9%). We contacted households only when the treating physician provided explicit approval, resulting in invitations to 286 households, although not all contact information on record was accurate. We ultimately reached 204 households, and 160 parents from 125 households consented (61% response rate). Sixty-three households (31% of those reached) declined participation, providing either no reason (n = 33) or the following reasons: too painful (n = 10), too soon (n = 8), too many life stressors (n = 4), bad experience with treating institution (n = 3), do not want to discuss the loss (n = 3), and want to get past the loss (n = 2).
Sixteen households were lost to follow-up (Appendix Fig A1, online only). The average time since loss was significantly lower for parents who declined (mean, 1.9 years; standard deviation, 1.7 years) than for study completers (mean, 2.4 years; standard deviation, 1.6 years; t[df, 179], 2.09; P = .04); there were no significant differences in the child's age, type of cancer, or geographic location (Ps > .10).
Of the 160 parents who consented, 120 completed study measures (90 from the Memorial Sloan Kettering Cancer Center; 30 from the National Cancer Institute Pediatric Oncology Branch; 75% participation rate). The majority of participants were married white mothers (Table 1). Twenty-three couples (46 parents; 38%) participated.
Table 1.
Participant Characteristics, Mental Health Challenges, and Need for Services
| Characteristic | All Parents (N = 120) |
|||
|---|---|---|---|---|
| No. | % | Mean | SD | |
| Female sex | 84 | 70 | ||
| Has surviving child* | 103 | 87 | ||
| Race/ethnicity | ||||
| White | 99 | 83 | ||
| Black | 11 | 9 | ||
| Hispanic | 4 | 3 | ||
| Asian | 4 | 3 | ||
| Other | 2 | 2 | ||
| Marital/living status | ||||
| Married/living with partner | 98 | 82 | ||
| Divorced/widowed/separated | 16 | 13 | ||
| Never married/unspecified | 6 | 5 | ||
| Religion | ||||
| Catholic | 48 | 40 | ||
| Protestant | 25 | 21 | ||
| Other Christian | 15 | 13 | ||
| Jewish | 11 | 9 | ||
| Other | 5 | 4 | ||
| None | 16 | 13 | ||
| Geographic region of the United States | ||||
| Northeast | 75 | 63 | ||
| Southeast | 21 | 18 | ||
| Midwest | 17 | 14 | ||
| Southwest | 4 | 3 | ||
| West | 2 | 2 | ||
| Puerto Rico | 1 | 0.8 | ||
| Child's diagnosis | ||||
| Sarcoma | 48 | 40 | ||
| Brain tumor | 27 | 23 | ||
| Neuroblastoma | 22 | 18 | ||
| Leukemia/lymphoma | 18 | 15 | ||
| Other | 5 | 4 | ||
| Mental health challenges | ||||
| Subclinical/increased level | ||||
| Depression† | 34 | 29 | ||
| Anxiety† | 14 | 12 | ||
| Grief* | 36 | 30 | ||
| Depression, anxiety, or grief† | 52 | 44 | ||
| Clinical level | ||||
| Depression† | 16 | 14 | ||
| Anxiety† | 7 | 6 | ||
| Grief* | 14 | 12 | ||
| Depression, anxiety, or grief† | 27 | 23 | ||
| Need for services | ||||
| Expressed need‡ | 53 | 47 | ||
| Those with need not using services§ | 20 | 40 | ||
| Symptom-based need† | 27 | 23 | ||
| Those with need not using services | 10 | 37 | ||
| Age, years§ | 47.4 | 7.9 | ||
| Years of education§ | 15.6 | 3.0 | ||
| Four-year college education or greater | 67 | 57 | ||
| Child's age at death | 13.0 | 7.0 | ||
| Years as caregiver‖ | 3.3 | 2.8 | ||
| Depression (population-adusted T score)† | 59.1 | 8.6 | ||
| Anxiety (population-adjusted T score)† | 55.6 | 6.7 | ||
| Grief (PG-13 score)* | 28.7 | 9.4 | ||
| Anxious Attachment (ECR-R score)† | 2.3 | 1.2 | ||
| Avoidant Attachment (ECR-R score)† | 2.8 | 1.2 | ||
| Existential Vacuum (LAP-R score)§ | 26.8 | 9.1 | ||
| Personal Meaning (LAP-R score)§ | 74.5 | 17.3 | ||
| Time since loss, years† | 2.4 | 1.6 | ||
| 6 months to 1 year | 23 | 20 | ||
| 1-2 | 40 | 34 | ||
| 2-4 | 34 | 29 | ||
| > 4 | 21 | 18 | ||
NOTE. Measure scores were calculated with mean replacement of missing responses if at least 80% of responses contributing to a participant's score were provided. Less than 1% of responses were missing and replaced. Percentages may not equal 100% because of rounding.
Abbreviations: ECR-R, Experiences in Close Relationships-Revised; LAP-R, Life Attitude Profile-Revised; MHSU, mental health service use; PG-13, Prolonged Grief-13 (13-item self-report scale).
Missing one response.
Missing two responses.
Missing six responses.
Missing three responses.
Missing five responses.
Measures
Demographics, MHSU, and perceived barriers.
A 63-item survey was used to obtain demographic information and included items used in previous studies of MHSU,16 reasons for discontinuing use, level of interest in getting help to cope with their loss, and barriers to service use.17 MHSU was defined as use of talk therapy, psychotropic medication, and/or support groups. Participants also rated how much various factors (identified by previous investigators10,17,18 and our research group) contributed to why they had not accessed services on a 5-point Likert-type scale. Factors rated 3 or higher were considered endorsed barriers to MHSU.
Prolonged grief symptoms.
Prolonged grief symptoms were measured using the PG-13,19 a reliable 13-item self-report measure that evaluates the frequency and intensity of PGD symptoms on a 5-point Likert-type scale.19 Scores range from 12 to 60. Parents who scored 34 or above were considered to have increased levels of prolonged grief symptoms based on a sensitivity analysis which showed that these parents had significantly more mental health problems than those scoring lower than 34 (ps < .05). A threshold of 34 was similarly used to recruit participants for a preventive intervention trial.20 Clinical levels were identified by using the diagnostic algorithm provided in the PG-13.19
Attachment styles.
The Experience of Close Relationships-Revised (ECR-R) is a well-validated, reliable 36-item measure of anxious and avoidant attachment.21,22 Items assess how respondents experience close relationships by using a 7-point Likert scale. Higher scores on each subscale indicate a stronger expression of anxious or avoidant attachment.
Depression and anxiety symptoms.
The Adult Self-Report (ASR) is a well-validated, 126-item instrument that provides normed scores in several mental health functioning areas.23 We focus on the DSM Depressive Problems and DSM Anxiety Problems scales, which reflect Diagnostic and Statistical Manual for Mental Disorders, Fourth Edition (DSM-IV) diagnoses.24 T scores 70 and above were considered in the clinical range, and scores from 65 to 69 were considered subclinical.23
Meaning and purpose in life.
Sense of meaning and purpose in life were assessed by using the well-validated, reliable 48-item Life Attitude Profile-Revised (LAP-R),25 which includes the Personal Meaning Index and Existential Vacuum subscales. Items are rated on a 7-point Likert-type scale. Higher scores reflect a higher degree of a given subscale.
Data Analysis
Analyses were performed by using IBM SPSS version 22 (IBM, Armonk, NY). Descriptive statistics were used to characterize demographics, MHSU, and barriers to service use. Because of the potential correlation between responses of parents of the same child, generalized estimating equations (GEEs)26 were used to estimate associations. Multivariable models examined associations between each mental health variable and current MHSU, controlling for variables commonly associated with MHSU, including sex, partner status, minority status, college education, other child/children, religion, time since loss, parent's age, and child's age. As Vittinghoff and McCulloch27 recommended, the 10 outcome events per predictor variable rule was relaxed. Prior MHSU as a predictor of current MHSU was examined separately and not included as a covariate in the other models because its inclusion resulted in quasi-separation in the data, which prevented many models from running successfully, and because of multicollinearity concerns. Because MHSU is a dichotomous variable, odds ratios (ORs) and 95% CIs were calculated.
RESULTS
Who Needs and Wants Help?
Table 1 details the percentages of parents who met subclinical/increased and clinical symptom thresholds and who wanted or may have needed mental health services. Forty-seven percent of parents indicated a wish for at least “a moderate amount of assistance,” which we defined as expressed need. Twenty-three percent of parents reported clinical levels of prolonged grief, depression, and/or anxiety, which we defined as symptom-based need. It is also important to highlight that, although 12% of parents met full criteria for PGD, 77% endorsed longing or yearning for their child on at least a daily basis. Thus, many parents were profoundly missing their children despite not having clinical or increased levels of prolonged grief.
MHSU Since the Loss: Who Has Gotten Help?
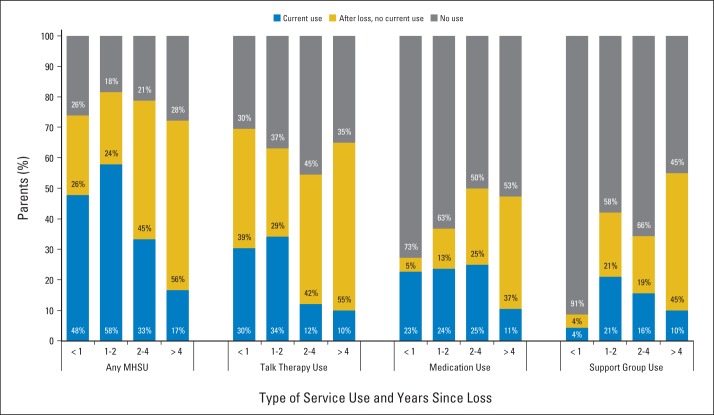
Seventy-eight percent of parents were either currently using services (41%) or had used services since their loss (37%). Figure 1 presents rates of MHSU by service type. Talk therapy was the most commonly used service, and rates of support group use were lowest. Given that parents' need and desire for bereavement support may change over time, we also examined MHSU as a function of the amount of time that had passed since their child's death (Fig 2; note that Table 1 contains data on the number of parents in each time-since-loss category; missing data vary by service used.). Although the study was cross sectional, parents who lost their child from 6 months to 6 years ago were represented. Nearly half of parents less than 1 year after their loss were currently using services, and rates were even higher in the second year (58%). Notably, more parents had discontinued therapy within the first year after their loss (39%) than were currently in therapy (30%).
Fig 1.
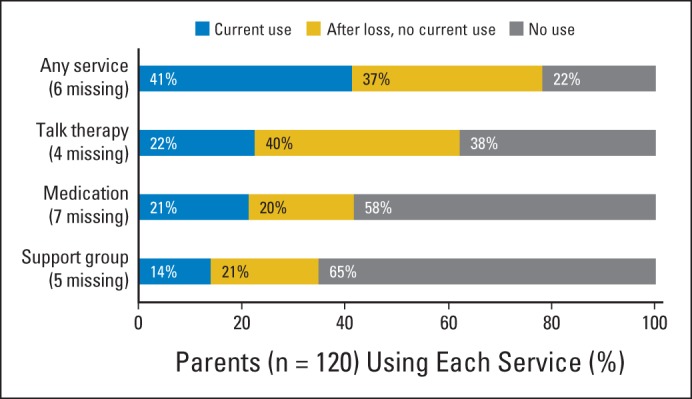
Mental health service use by type. Percentages may not equal 100% because of rounding.
Fig 2.
Mental health service use and time since loss. Percentages may not equal 100% because of rounding.
What Factors Are Associated With Current MHSU?
Table 2 presents ORs from bivariate and multivariable GEE models that estimated associations between mental health variables and current MHSU, controlling for background variables (note that details on missing data for each of the variables listed are provided in Table 1). Multivariable models showed that depression symptoms, anxious and avoidant attachment styles, existential vacuum, and decreased meaning were associated with current MHSU. In models that were able to successfully run with prior MHSU included, the only predictors that were no longer significantly associated with current MHSU were anxious attachment and existential vacuum.
Table 2.
Factors Associated With Current Mental Health Service Use
| Factor | OR (95% CI) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| MHSU |
Talk Therapy |
Medications |
Support Groups |
Unmet Expressed Need |
||||||
| Bivariate | Multivariable | Bivariate | Multivariable | Bivariate | Multivariable | Bivariate | Multivariable | Bivariate | Multivariable | |
| Background variable | ||||||||||
| Female sex | 1.06 (0.50 to 2.25) | 1.14 (0.45 to 2.90) | 0.81 (0.37 to 1.79) | 0.78 (0.24 to 2.50) | 0.58 (0.23 to 1.42) | 0.57 (0.19 to 1.74) | 1.75 (0.48 to 6.47) | 2.32 (0.36 to 14.92) | 2.67 (0.70 to 10.29) | 4.62 (0.80 to 26.89) |
| Partnered | 0.73 (0.28 to 1.92) | 0.58 (0.17 to 1.94) | 0.55 (0.19 to 1.57) | 0.30 (0.71 to 1.24) | 0.71 (0.26 to 2.50) | 0.79 (0.16 to 3.81) | 1.03 (0.27 to 3.93) | 0.67 (0.15 to 3.03) | 1.30 (0.35 to 4.89) | 2.57 (0.48 to 13.89) |
| Minority status | 0.74 (0.27 to 2.02) | 0.75 (0.24 to 2.32) | 0.88 (0.26 to 3.00) | 0.80 (0.19 to 3.48) | 0.66 (0.17 to 2.51) | 0.92 (0.22 to 3.81) | 0.69 (0.16 to 3.07) | 0.42 (0.06 to 2.97) | 2.64 (0.97 to 7.17) | 3.25 (1.04 to 10.15)* |
| Four-year college education | 1.20 (0.53 to 2.69) | 1.12 (0.45 to 2.80) | 1.98 (0.78 to 4.99) | 2.75 (0.76 to 9.90) | 0.98 (0.40 to 2.44) | 1.13 (0.41 to 3.15) | 1.19 (0.41 to 3.49) | 0.65 (0.17 to 2.55) | 1.29 (0.47 to 3.56) | 0.86 (0.29 to 2.53) |
| Has surviving child | 0.79 (0.23 to 2.76) | 1.14 (0.35 to 3.67) | 0.57 (0.16 to 2.08) | 0.81 (0.24 to 2.72) | 0.67 (0.16 to 2.78) | 1.01 (0.23 to 4.41) | 2.34 (0.32 to 17.24) | 2.43 (0.35 to 17.03) | 0.89 (0.25 to 3.10) | 0.53 (0.16 to 1.75) |
| Identified religion | 1.57 (0.56 to 4.37) | 2.01 (0.55 to 7.35) | 1.47 (0.36 to 6.08) | 2.80 (0.31 to 25.50) | 1.76 (0.39 to 8.05) | 2.08 (0.40 to 10.82) | 1.09 (0.24 to 5.04) | 1.40 (0.19 to 10.20) | 2.87 (0.37 to 22.10) | 1.22 (0.19 to 8.11) |
| Time since loss (1 year) | 0.67 (0.50 to 0.89)† | 0.63 (0.44 to 0.88)† | 0.71 (0.50 to 1.01) | 0.68 (0.46 to 1.00) | 0.78 (0.58 to 1.07) | 0.76 (0.53 to 1.08) | 0.97 (0.72 to 1.30) | 0.82 (0.48 to 1.40) | 0.89 (0.65 to 1.22) | 0.83 (0.59 to 1.17) |
| Parent's age (5 years) | 1.20 (0.92 to 1.56) | 1.40 (0.90 to 2.16) | 1.34 (1.04 to 1.72)* | 1.36 (0.87 to 2.12) | 1.35 (0.96 to 1.90) | 1.25 (0.74 to 2.12) | 0.89 (0.66 to 1.22) | 1.57 (0.77 to 3.17) | 0.76 (0.57 to 1.02) | 0.90 (0.52 to 1.56) |
| Child's age at death (5 years) | 1.15 (0.87 to 1.52) | 0.82 (0.49 to 1.37) | 1.27 (0.93 to 1.74) | 1.03 (0.58 to 1.83) | 1.34 (0.93 to 1.93) | 1.07 (0.57 to 1.98) | 0.66 (0.47 to 0.92)* | 0.45 (0.18 to 1.11) | 0.79 (0.56 to 1.13) | 0.82 (0.43 to 1.57) |
| Prior mental health service use‡ | 1.93 (0.84 to 4.41) | 4.07 (1.45 to 11.37)† | 1.77 (0.67 to 4.69) | 2.76 (0.87 to 8.77) | 3.70 (1.34 to 10.22)* | 4.97 (1.52 to 16.28)† | 4.65 (1.37 to 15.82)* | 9.31 (1.12 to 77.43)* | 2.67 (0.70 to 10.29) | 1.18 (0.38 to 3.72) |
| Mental health variables | ||||||||||
| ASR Subclinical Depression | 3.70 (1.67 to 8.20)† | 4.27 (1.68 to 10.82)† | 4.34 (1.76 to 10.81)† | 9.19 (2.65 to 31.84)† | 5.99 (2.08 to 17.23)† | 7.87 (2.46 to 25.23)† | 2.11 (0.73 to 6.11) | 2.13 (0.49 to 9.22) | 1.55 (0.55 to 4.40) | 1.23 (0.30 to 5.02) |
| ASR Subclinical Anxiety | 2.70 (0.93 to 7.89) | 3.59 (0.95 to 13.60) | 2.13 (0.66 to 6.89) | 3.04 (0.76 to 12.07) | 3.28 (1.06 to 10.14)* | 3.51 (1.16 to 10.57)* | 1.69 (0.40 to 7.18) | 2.16 (0.39 to 11.86) | 0.83 (0.16 to 4.38) | 0.33 (0.04 to 2.84) |
| PG-13 Elevated Grief | 2.14 (0.91 to 5.03) | 2.07 (0.74 to 5.80) | 2.69 (1.10 to 6.58) | 3.61 (0.95 to 13.77) | 1.49 (0.59 to 3.81) | 1.39 (0.43 to 4.49) | 1.02 (0.33, 3.17) | 0.72 (0.19, 2.71) | 2.29 (0.83, 6.32) | 2.08 (0.67, 6.46) |
| ECR-R Anxious Attachment (1 unit) | 1.59 (1.14 to 2.22)† | 1.51 (1.02 to 2.25)* | 1.49 (1.09 to 2.04)* | 1.36 (0.94 to 1.96) | 1.72 (1.17 to 2.51)† | 1.71 (1.14 to 2.55)† | 0.99 (0.62, 1.60) | 1.02 (0.65, 1.60) | 1.41 (0.94, 2.13) | 1.40 (0.82, 2.37) |
| ECR-R Avoidant Attachment (1 unit) | 1.59 (1.17 to 2.16)† | 1.64 (1.14 to 2.34)† | 1.11 (0.87 to 1.43) | 1.07 (0.77 to 1.49) | 1.82 (1.27 to 2.62)† | 1.92 (1.27 to 2.91)† | 1.20 (0.81 to 1.77) | 1.26 (0.79 to 2.00) | 1.27 (0.87 to 1.86) | 1.17 (0.71 to 1.92) |
| LAP-R Existential Vacuum (10 units) | 1.51 (1.00 to 2.26)* | 1.67 (1.01 to 2.76)* | 1.77 (1.06 to 2.94)* | 2.23 (1.18 to 4.22)* | 2.07 (1.19 to 3.61)† | 2.21 (1.17 to 4.15)* | 1.14 (0.68 to 1.92) | 1.28 (0.61 to 2.72) | 1.57 (1.02 to 2.43)* | 1.44 (0.83 to 2.51) |
| LAP-R Personal Meaning (15 units) | 0.60 (0.42 to 0.87)† | 0.60 (0.39 to 0.93)* | 0.64 (0.44 to 0.93)* | 0.63 (0.40 to 0.98)* | 0.68 (0.49 to 0.94)* | 0.61 (0.40 to 0.94)* | 0.81 (0.52 to 1.28) | 0.71 (0.43 to 1.17) | 0.85 (0.59 to 1.21) | 0.84 (0.52 to 1.36) |
NOTE. Odds ratios (ORs) presented in the multivariable columns for each background variable reflect results for a multivariable generalized estimating equations model including all background variables as predictors except prior mental health service use (MHSU). ORs for prior mental health service use and each mental health variable reflect results only for that particular variable in models controlling for all demographic variables. Unless otherwise indicated by a scale, all variables are binary (yes/no). For continuous predictor variables, units used for the OR calculations are in parentheses next to the row head. Models exclude parents' missing data for any predictor or response variables. Models include between 104 and 116 parents.
Abbreviations: ASR, Adult Self-Report; ECR-R, Experiences in Close Relationships-Revised; LAP-R, Life Attitude Profile-Revised; PG-13, Prolonged Grief-13 (13-item self-report scale).
P < .05.
P < .01.
Prior use of the same type of service (eg, models predicting current talk therapy use include specifically prior talk therapy use). Prior use of any mental health service is used for models predicting any current use and unmet expressed need.
Unmet Need: Who Needs Help but Is Not Getting It, and What Gets in the Way?
Parents who had either expressed or symptom-based need but were not using mental health services were categorized as having unmet need. We found that unmet need was prevalent, with 40% of parents (n = 20) with expressed need not receiving services, and 38% of parents (n = 10) with symptom-based need not receiving services.
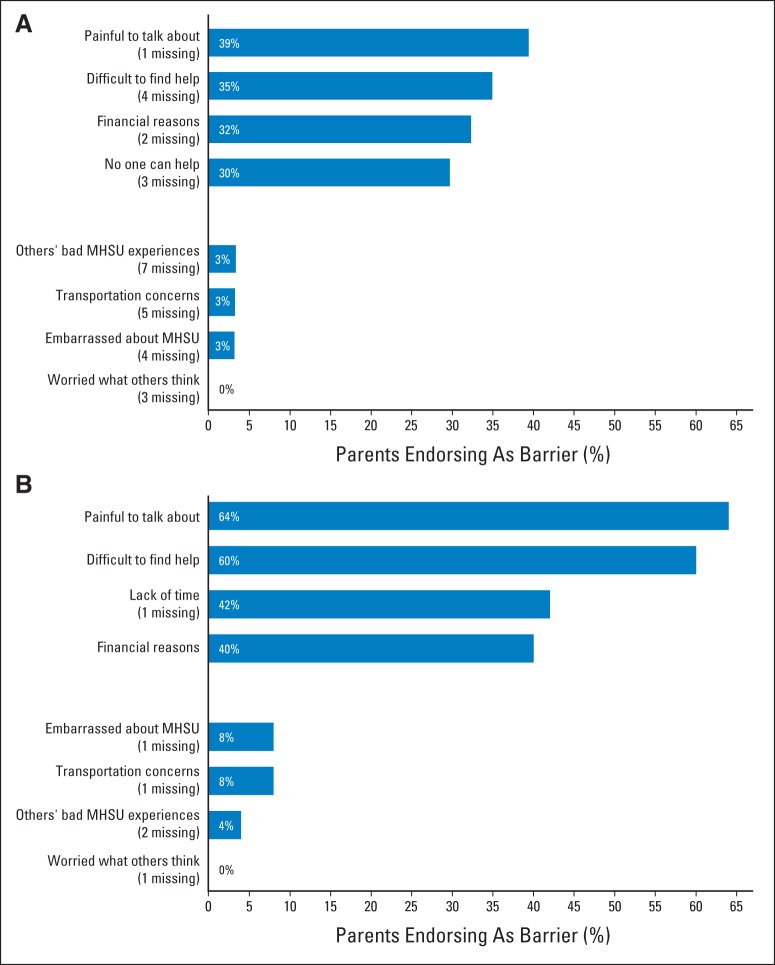
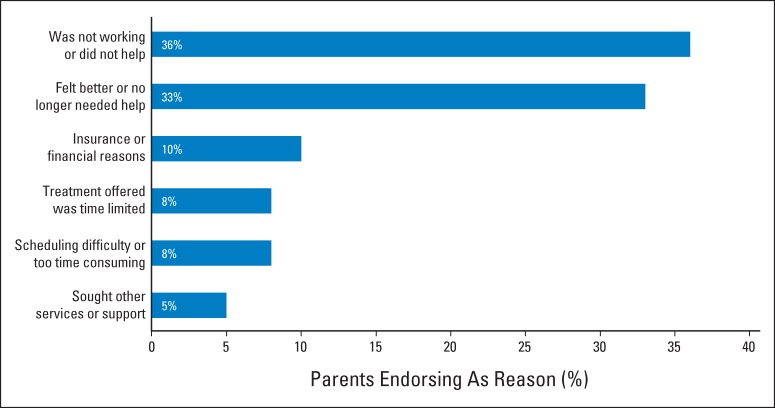
Among those with unmet need, the most common service use barriers (Fig 3) were that it was too painful to speak about their loss (64%) and it was difficult to find help (60%). Increased prolonged grief was associated with it being too painful to discuss their child's death (OR, 6.94; 95% CI, 2.13 to 22.67; P < .001) and feeling like no one can help with coping with the loss (OR, 3.18; 95% CI, 1.00 to 10.07; P < .05). Among the 40% who had been in therapy but stopped (Fig 4), the most common reason for discontinuing therapy was that it was not helpful (36%).
Fig 3.
Most and least common barriers to mental health service use (MHSU). Among parents (A) not currently using services (n = 67) and (B) with unmet expressed or symptom-based need (n = 25).
Fig 4.
Reasons for discontinuing talk therapy among parents who used talk therapy after loss and were not currently using it (n = 39 parents; 46 qualifying parents, seven of whom did not report a reason).
A multivariable GEE model showed that minority parents were more likely than nonminority parents to have unmet expressed need. Barriers to service use among minority and nonminority parents were generally similar, but 69% of minority parents who were not using services reported that it was too painful to discuss their loss compared with 32% of nonminority parents (OR, 4.00; 95% CI, 1.42 to 11.29; P = .009).
DISCUSSION
This study examined MHSU in a sample of parents who lost a child to cancer. We found that MHSU occurred most commonly within the first 2 years after their loss, with rates highest in the second year after their loss. Indeed, many parents report that “the second year is harder” with respect to their grief, because the defenses and informal support that initially protected them from the profound pain of their loss begin to wane.11 It may also be that parents do not view persistent grief as a problem until the second year.28
The desire for support services was quite common, with nearly half of bereaved parents expressing a wish for assistance with coping with their loss. Unfortunately, 40% of these parents were not receiving services. Similarly, among the 23% of parents reporting clinical levels of psychological symptoms, 37% were not receiving services. In short, a significant subset of bereaved parents' need was not being met.
These findings are consistent with research on general MHSU, which similarly showed that the uptake of services is “disturbingly low” in other populations.29 This literature has suggested that being younger, non-Hispanic white, previously married, not having low income, and not living in a rural area are associated with increased service use.29 We did not find significant associations between demographic variables and MHSU in exploratory multivariable models, but we did find that parents were more likely to use services if their loss was more recent, they had an insecure attachment style, they had previously used services, and they were experiencing at least subclinical depression symptoms. Parents who reported decreased meaning in life also tended to want and use services more, suggesting the importance of developing meaning-centered interventions for this population.30
We found that, similar to our previous work,31 the presence of increased prolonged grief symptoms was not an independent predictor of service use in multivariable analyses. Notably, despite the fact that 89% of parents with increased PGD symptoms reported they would like help with their coping, only 56% were actually using mental health services. The magnitude of the emotional pain parents experience in the wake of their loss appears to impede service use, supporting our hypothesis that treatment fearfulness is an important barrier. In fact, the most frequently cited barrier among those with unmet support needs was that it was too painful to speak about their loss, which nearly two thirds of this subsample endorsed when asked to what extent various factors contributed to why they had not accessed services. Furthermore, parents with increased levels of prolonged grief were more likely to identify communicating about their loss being too painful and believing no one could help as barriers to service use. Unlike prior research,32 we did not find stigma to be a barrier to accessing services in our sample, perhaps because obtaining support after the devastating loss of a child is generally socially acceptable. Instead, what may have a greater impact on MHSU and dropout in grieving parents is treatment fearfulness or finding it too painful to engage in treatment.
As expected, dropout seems to be related to the efficacy of the services received. Although talk therapy was the most used service by bereaved parents in our sample, it was also the most frequently discontinued: 33% discontinued because they were feeling better, but 36% dropped out of treatment because they felt the therapy was not helping or that providers did not get (understand) their pain. In fact, of all parents using talk therapy after their loss, a total of 40% dropped out for a reason other than symptom improvement. This appears to be increased compared with the general population; Edlund et al32 found a treatment dropout rate of 19% in a community sample.
This study should be interpreted with its methodologic limitations in mind, including the cross-sectional design and the exploratory, hypothesis-generating nature of the analytic approach, which could have resulted in spurious findings because of the number of models run and in reduced statistical power because of the large number of predictors included in the multivariable models. In addition, because parents who were excluded from or declined participation (explicitly or passively) may have been more distressed, resulting in a healthy selection bias, the need observed may be an underestimate. There was also limited racial/ethnic diversity in the sample. It should be noted that the data collected was self-report without clinician assessments, and thus formal psychiatric diagnoses could not be made; rather, the symptoms were suggestive of diagnoses. Finally, this study did not examine the quality of mental health services received or the needs of surviving siblings, which may influence when and how parents reach out for professional support.
Clinical Implications and Future Research
So if we build it, will they come? Our data suggest that parents need, want, and often access bereavement mental health services. Hospital-based programs offer continuity of care and are appreciated by parents.11,33 Yet bereavement programs seem to be underused.9 These services could be improved to promote access for those with more debilitating grief symptoms and to increase perceived effectiveness.
This study's findings have several implications. First, screening efforts need to be improved. Such efforts should continue at least through the second year postloss, and ideally beyond, because we observed that 47% of parents expressed need 2 to 4 years postloss. Minority parents in this study were more likely to have unmet expressed need and treatment fearfulness, indicating the importance of greater outreach to bereaved minority parents. Prior research has suggested strategies to decrease racial/ethnic disparities in MHSU, including facilitating access to quality care and a diverse community of providers and improving patient and clinician education.34 Emotional and logistical barriers to accessing care might be addressed through inclusion of bereaved parents who report they are coping well in intervention development and outreach efforts and through the use of telemedicine.11 Finally, our finding that more than one third of parents dropped out of talk therapy because they did not find it helpful, with some feeling that providers could not understand the intensity of their pain, suggests the importance of improving the quality of bereavement care6 and increasing providers' sensitivity to bereaved parents' yearning for their child and their ability to foster parents' sense of hope about the future. In addition to efforts to replicate our findings, future research might therefore focus on developing adequate screening tools, evaluating the use of technology to reduce barriers to accessing care, and developing effective, tailored grief interventions with input from bereaved parents.
Acknowledgment
We are deeply indebted to the bereaved parents who participated in and shared so much for this study. We thank those colleagues who gave their time, ideas, and support to this study, including Alberta Aikin, RN; Kristin Baird, MD; Abraham Bartell, MD; Tara Bohn, BA; Farid Boulad, MD; Ira Dunkel, MD; Maria Farberov, MPH; Cynthia Gerhardt, MD; Stephen Gilheeney, MD; Yasmin Khakoo, MD; Julia Kearny, MD; Nancy Kernan, MD; Rachel Kobos, MD; Melinda Merchant, MD, PhD; Paul Meyers, MD; Shakeel Modak, MD; Robert Neimeyer, PhD; Jamie Ostroff, PhD; Nina Pickett; Richard O'Reilly, MD; Elyse Shuk, MA; Neerav Shukla, MD; Trudy Small, MD (deceased); Peter Steinherz, MD; Katherine Warren, MD; and Leonard Wexler, MD.
Appendix
Fig A1.
Recruitment flowchart. MSKCC, Memorial Sloan Kettering Cancer Center; NCI, National Cancer Institute Pediatric Oncology Branch.
Footnotes
Supported by National Cancer Institute Grants No. R03 CA139944 (W.G.L.), K07 CA172216 (W.G.L.), T32 CA009461, and P30 CA08748-48, which provides partial support for the Behavioral Research Methods Core Facility used in conducting this investigation.
Presented in part at the 9th Annual Conference of the American Psychosocial Oncology Society, Miami, FL, February 23-25, 2012; the 36th Annual Conference of the Association of Death Education and Counseling, Baltimore, MD, April 23-26, 2014; the University of North Carolina Lineberger Comprehensive Cancer Center Comprehensive Cancer Support Program Grand Rounds, Chapel Hill, NC, June 4, 2014; and the National Cancer Institute Pediatric Oncology Branch Research Seminar Series, Bethesda, MD, April 23, 2015.
Authors' disclosures of potential conflicts of interest are found in the article online at www.jco.org. Author contributions are found at the end of this article.
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Disclosures provided by the authors are available with this article at www.jco.org.
AUTHOR CONTRIBUTIONS
Conception and design: Wendy G. Lichtenthal, Yuelin Li, William Breitbart, David W. Kissane, Holly G. Prigerson
Administrative support: Corinne R. Sweeney
Provision of study materials or patients: Lori Wiener
Collection and assembly of data: Wendy G. Lichtenthal, Geoffrey W. Corner, Corinne R. Sweeney, Lori Wiener, Kailey E. Roberts
Data analysis and interpretation: Wendy G. Lichtenthal, Geoffrey W. Corner, Corinne R. Sweeney, Kailey E. Roberts, Raymond E. Baser, Yuelin Li, David W. Kissane
Manuscript writing: All authors
Final approval of manuscript: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Mental Health Services for Parents Who Lost a Child to Cancer: If We Build Them, Will They Come?
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or jco.ascopubs.org/site/ifc.
Wendy G. Lichtenthal
No relationship to disclose
Geoffrey W. Corner
No relationship to disclose
Corinne R. Sweeney
No relationship to disclose
Lori Wiener
No relationship to disclose
Kailey E. Roberts
No relationship to disclose
Raymond E. Baser
No relationship to disclose
Yuelin Li
No relationship to disclose
William Breitbart
No relationship to disclose
David W. Kissane
No relationship to disclose
Holly G. Prigerson
No relationship to disclose
REFERENCES
- 1.Arnold J, Gemma PB, Cushman LF. Exploring parental grief: Combining quantitative and qualitative measures. Arch Psychiatr Nurs. 2005;19:245–255. doi: 10.1016/j.apnu.2005.07.008. [DOI] [PubMed] [Google Scholar]
- 2.Kreicbergs UC, Lannen P, Onelov E, et al. Parental grief after losing a child to cancer: Impact of professional and social support on long-term outcomes. J Clin Oncol. 2007;25:3307–3312. doi: 10.1200/JCO.2006.10.0743. [DOI] [PubMed] [Google Scholar]
- 3.Talbot K. Mothers now childless: Survival after the death of an only child. Omega: Journal of Death and Dying. 1997;34:177–189. [Google Scholar]
- 4.Ginzburg K, Geron Y, Solomon Z. Patterns of complicated grief among bereaved parents. Omega: Journal of Death and Dying. 2002;45:119–132. [Google Scholar]
- 5.Prigerson HG, Horowitz MJ, Jacobs SC, et al. Prolonged grief disorder: Psychometric validation of criteria proposed for DSM-V and ICD-11. PLoS Med. 2009;6:e1000121. doi: 10.1371/journal.pmed.1000121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Donovan L, Wakefield CE, Russell V, et al. Hospital-based bereavement services following the death of a child: A mixed study review. Palliat Med. 2015;29:193–210. doi: 10.1177/0269216314556851. [DOI] [PubMed] [Google Scholar]
- 7.Institute of Medicine. When Children Die: Improving Palliative and End-of-Life Care for Children and Their Families. Washington, DC: The National Academies Press; 2003. [Google Scholar]
- 8.Thompson AL, Miller KS, Barrera M, et al. A qualitative study of advice from bereaved parents and siblings. J Soc Work End Life Palliat Care. 2011;7:153–172. doi: 10.1080/15524256.2011.593153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Johnston DL, Nagel K, Friedman DL, et al. Availability and use of palliative care and end-of-life services for pediatric oncology patients. J Clin Oncol. 2008;26:4646–4650. doi: 10.1200/JCO.2008.16.1562. [DOI] [PubMed] [Google Scholar]
- 10.Kushner MG, Sher KJ. The relation of treatment fearfulness and psychological service utilization: An overview. Prof Psychol Res Pr. 1991;22:196–203. [Google Scholar]
- 11.Darbyshire P, Cleghorn A, Downes M, et al. Supporting bereaved parents: A phenomenological study of a telephone intervention programme in a paediatric oncology unit. J Clin Nurs. 2013;22:540–549. doi: 10.1111/j.1365-2702.2012.04266.x. [DOI] [PubMed] [Google Scholar]
- 12.Downar J, Barua R, Sinuff T. The desirability of an Intensive Care Unit (ICU) clinician-led bereavement screening and support program for family members of ICU Decedents (ICU Bereave) J Crit Care. 2014;29:311.e9–e16. doi: 10.1016/j.jcrc.2013.11.024. [DOI] [PubMed] [Google Scholar]
- 13.D'Agostino NM, Berlin-Romalis D, Jovcevska V, et al. Bereaved parents' perspectives on their needs. Palliat Support Care. 2008;6:33–41. doi: 10.1017/S1478951508000060. [DOI] [PubMed] [Google Scholar]
- 14.Prigerson HG, Jacobs SC. Perspectives on care at the close of life: Caring for bereaved patients—“all the doctors just suddenly go”. JAMA. 2001;286:1369–1376. doi: 10.1001/jama.286.11.1369. [DOI] [PubMed] [Google Scholar]
- 15.Feigelman W, Jordan JR, McIntosh JL, et al. Devastating Losses: How Parents Cope With the Death of a Child to Suicide or Drugs. New York, NY: Springer Publishing; 2012. [Google Scholar]
- 16.Vanderwerker LC, Laff RE, Kadan-Lottick NS, et al. Psychiatric disorders and mental health service use among caregivers of advanced cancer patients. J Clin Oncol. 2005;23:6899–6907. doi: 10.1200/JCO.2005.01.370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wong EC, Marshall GN, Schell TL, et al. Barriers to mental health care utilization for U.S. Cambodian refugees. J Consult Clin Psychol. 2006;74:1116–1120. doi: 10.1037/0022-006X.74.6.1116. [DOI] [PubMed] [Google Scholar]
- 18.Sareen J, Jagdeo A, Cox BJ, et al. Perceived barriers to mental health service utilization in the United States, Ontario, and the Netherlands. Psychiatr Serv. 2007;58:357–364. doi: 10.1176/ps.2007.58.3.357. [DOI] [PubMed] [Google Scholar]
- 19.Prigerson HG, Vanderwerker LC, Maciejewski PK. A case for inclusion of prolonged grief disorder in DSM-V. In: Stroebe MS, Hansson RO, Schut H, et al., editors. Handbook of Bereavement Research and Practice: Advances in Theory and Intervention. Washington, DC: American Psychological Association; 2008. pp. 165–186. [Google Scholar]
- 20.Litz BT, Schorr Y, Delaney E, et al. A randomized controlled trial of an internet-based therapist-assisted indicated preventive intervention for prolonged grief disorder. Behav Res Ther. 2014;61:23–34. doi: 10.1016/j.brat.2014.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fraley RC, Waller NG, Brennan KA. An item response theory analysis of self-report measures of adult attachment. J Pers Soc Psychol. 2000;78:350–365. doi: 10.1037//0022-3514.78.2.350. [DOI] [PubMed] [Google Scholar]
- 22.Sibley CG, Fischer R, Liu JH. Reliability and validity of the revised experiences in close relationships (ECR-R) self-report measure of adult romantic attachment. Pers Soc Psychol Bull. 2005;31:1524–1536. doi: 10.1177/0146167205276865. [DOI] [PubMed] [Google Scholar]
- 23.Achenbach TM, Rescorla LA. Manual for the ASEBA Adult Forms & Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families; 2003. [Google Scholar]
- 24.American Psychiatric Association. DSM-IV: Diagnostic & Statistical Manual of Mental Disorders, Edition 4. Washington, DC: American Psychiatric Publishing; 1994. [Google Scholar]
- 25.Reker GT. Manual of the Life Attitude Profile-Revised (LAP-R) Peterborough, ON, Canada: Student Psychologists Press; 1992. [Google Scholar]
- 26.Hanley JA, Negassa A, Edwardes MD, et al. Statistical analysis of correlated data using generalized estimating equations: An orientation. Am J Epidemiol. 2003;157:364–375. doi: 10.1093/aje/kwf215. [DOI] [PubMed] [Google Scholar]
- 27.Vittinghoff E, McCulloch CE. Relaxing the rule of ten events per variable in logistic and Cox regression. Am J Epidemiol. 2007;165:710–718. doi: 10.1093/aje/kwk052. [DOI] [PubMed] [Google Scholar]
- 28.Penman EL, Breen LJ, Hewitt LY, et al. Public attitudes about normal and pathological grief. Death Stud. 2014;38:510–516. doi: 10.1080/07481187.2013.873839. [DOI] [PubMed] [Google Scholar]
- 29.Wang PS, Lane M, Olfson M, et al. Twelve-month use of mental health services in the United States: Results from the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:629–640. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- 30.Lichtenthal WG, Breitbart W. The central role of meaning in adjustment to the loss of a child to cancer: Implications for the development of meaning-centered grief therapy. Curr Opin Support Palliat Care. 2015;9:46–51. doi: 10.1097/SPC.0000000000000117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lichtenthal WG, Nilsson M, Kissane DW, et al. Underutilization of mental health services among bereaved caregivers with prolonged grief disorder. Psychiatr Serv. 2011;62:1225–1229. doi: 10.1176/appi.ps.62.10.1225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Edlund MJ, Wang PS, Berglund PA, et al. Dropping out of mental health treatment: Patterns and predictors among epidemiological survey respondents in the United States and Ontario. Am J Psychiatry. 2002;159:845–851. doi: 10.1176/appi.ajp.159.5.845. [DOI] [PubMed] [Google Scholar]
- 33.Russo C, Wong AF. The bereaved parent. J Clin Oncol. 2005;23:8109–8111. doi: 10.1200/JCO.2005.01.6865. [DOI] [PubMed] [Google Scholar]
- 34.McGuire TG, Miranda J. New evidence regarding racial and ethnic disparities in mental health: Policy implications. Health Aff (Millwood) 2008;27:393–403. doi: 10.1377/hlthaff.27.2.393. [DOI] [PMC free article] [PubMed] [Google Scholar]