Abstract
Purpose
Niemann-Pick disease, type C (NPC) is a recessive, neurodegenerative, lysosomal storage disease caused by mutations in either NPC1 or NPC2. The diagnosis is difficult and frequently delayed. Ascertainment is likely incomplete due to both these factors and that the full phenotypic spectrum may not have been fully delineated. Given the recent development of a blood-based diagnostic test and development of potential therapies, it is important to understand the incidence of NPC and to define at risk patient populations.
Method
We evaluated data from four large massively parallel exome sequencing data sets. Variant sequences were identified and classified as pathogenic or non-pathogenic based on a combination of literature review and bioinformatic analysis. This methodology provided an unbiased approach to determining the allele frequency.
Results
Our data suggests an incidence rate for NPC1 and NPC2 of 1/92,104 and 1/2,858,998, respectively. However, evaluation of common NPC1 variants, suggests that there may be a late-onset NPC1phenotype with a markedly higher incidence on the order of 1/20,000–39,000.
Conclusions
We determined a combined incidence of classical NPC of 1/89,229 or 1.12 affected patients per 100,000 conceptions, but predict incomplete ascertainment of a lateonset phenotype of NPC1. This finding strongly supports the need for increased screening of potential patients.
Keywords: Next Generation sequence study, Niemann-Pick disease, type C, NPC, Allele frequency
Introduction
Niemann-Pick Type C (NPC) is an autosomal recessive, neurodegenerative lethal disorder with a clinical incidence of 1:104,0001–3. This was considered to be a minimal estimate due to incomplete ascertainment of atypical phenotypes or limitations of current diagnostic testing. NPC is caused by disruption of either NPC1 or NPC2 with mutations of NPC1 accounting for 95% of patients1; 2. Loss of function of either NPC1 or NPC2 results in the accumulation of unesterified cholesterol and glycosphingolipids within the late-endosome/lysosome of all cells. Although the clinical presentation and progression of NPC is a continuous spectrum, patients can be classified into four general categories based on age of neurological onset. These categories are early-infantile, late-infantile, juvenile and adolescent/adult-onset1. In the early infantile, late-infantile, and juvenile forms of the disease patients may initially present with neonatal cholestasis or hepatosplenomegaly. A small subset of NPC patients die of systemic liver disease usually during the neonatal period1. However in the majority of NPC patients the liver disease frequently resolves, but neurological signs and symptoms follow1; 2. Neurological symptoms are insidious and heterogeneous in nature, often initially manifesting in a non-specific manner (e.g., clumsiness or difficulty with school work) but commonly progress to include variable degrees of cerebellar ataxia, vertical supranuclear gaze palsy, gelastic cataplexy, seizures, and dementia. These neurological manifestations are invariably progressive4; 5 and ultimately result in death.
The current diagnosis of NPC is based upon filipin staining of unesterified cholesterol in cultured fibroblasts or molecular testing. Filipin staining requires a skin biopsy, is performed in only a few specialized diagnostic laboratories worldwide and is not always conclusive. Molecular testing of NPC1 and NPC2 is also available; however, molecular testing in practice also has weaknesses. It is currently still inconclusive in 12–15% of the cases, because of unknown pathogenicity of the changes, lack of study of allele segregation, existence of one (possibly 2) unidentified mutant allele. Combined with the frequently nonspecific and insidious nature of the neurological disease onset, the difficulty of diagnosis contributes to a diagnostic delay on the order of 4–5 years2 for the late infantile and juvenile forms of the disease. The diagnostic delay in the adolescent/adult-onset is likely greater but the full extent of that delay cannot be determined due to a limited number of reported cases. Recently a sensitive blood-based diagnostic test, which detects elevated oxysterols, has been developed and this blood-based test could economically and rapidly be used to screen potential patients6.
A number of therapies for NPC are actively being developed. Miglustat, a glycosphingolipid synthesis inhibitor, although not approved in the United States for treatment of NPC1, has been approved in the European Union and other countries for the treatment of NPC. 2-hydroxypropyl-β-cyclodextrin (HP-β-CD) has shown significant promise in both mouse and feline (Charles Vite personal communication) models of NPC1 and is currently in a phase 1/2 trial (NCT01747135) at the NIH. The development of HP-β-CD for NPC1 has been reviewed by Ottinger et al.7 Other potential therapies under development include HDAC inhibitors8–10, HSP70 (F. Platt), and delta-tocopherol11. Given the rapid development of potential therapeutic interventions, it is critical that the incidence of NPC and its full clinical spectrum be fully defined.
An increasing number of adult-onset NPC patients are being reported1; 12–14. Psychiatric symptoms can be prominent12–15 although affected adults without neurological manifestations have also been reported16–18. The full phenotypic spectrum of adult-onset NPC disease has yet to be delineated. This led us to question whether the incidence of NPC might be greater than previous clinical estimates due to incomplete ascertainment. To estimate the incidence of NPC in a manner that is independent of clinical recognition of cases, we sought to determine a pathogenic carrier frequency of NPC1 and NPC2 variants utilizing data from four independent massively parallel exome sequencing projects, or next generation sequencing projects. Our data indicates that the classical incidence of NPC likely occurs at the clinically predicted rate of approximately 1:90,000, and suggest that there may be a late-onset phenotype or variant form with an incidence potentially as high as 1:19,000–36,000.
Material and Methods
We have recently reported the determination of the pathogenic allele frequency of the 7-dehydrocholesterol reductase gene (DHCR7)19. We utilized a similar approach for the determination of the variant frequency in NPC.
Data Sets
Four large independent massively parallel exome sequencing projects, or next generation sequencing projects were utilized. These data sets are the NHLBI GO Exome Sequencing Project (ESP)20, V3 release of the 1000 Genomes Project21, ClinSeq®22, and a database from a NIH inter-institute collaboration on Autism (PIs: FD Porter, J Bailey-Wilson, E Tierney, A. Thurm). ESP contributed a maximum number of 13,006 chromosomes, 1000 Genome Project contributed 2,184 chromosomes, ClinSeq® contributed 1,902 chromosomes and the NIH inter-institute collaboration on Autism project contributed 662 chromosomes. Thus, a maximum total of 17,754 chromosomes were analyzed and this number was utilized as the denominator in total frequency calculations. None of these datasets included patients evaluated for NPC nor did we identify any individuals with two pathogenic mutations, so we considered them to be unbiased with respect to variation in NPC1 and NPC2.
Determination of Variant Calls and Annotation
Variant calls were downloaded for regions overlapping NPC1 and NPC2, by Perl script for every base of the coding exons plus/minus 5 base pairs of exon sequence when available. Mutations were annotated using SNPnexus23 using Refseq annotations24, pathogenicity predictions were performed using Polyphen-2,25 SIFT,26 Mutation assessor27. Intronic variations detected within 5 bases of intron exon boundaries were analyzed by MaxEntScan28. Untranslated regions variations were excluded from the analysis of these data sets.
Determination of Pathogenicity of the Variant Call
Determination of the pathogenicity of a variant allele was a multistep process that utilized both bioinformatic tools and manual curation. We began by comparing the variants found in the data sets against the professional version of the Human Gene Mutation Database (HGMD®)29 and the existing database of 78 patients with NPC1 in the NIH Cohort (PI: FD Porter) to determine which variants had been previously identified in patients known to have NPC. Since inclusion in HGMD does not require identification in a patient, primary literature was reviewed to determine the nature and manner in which the variations were detected. Variants were mapped onto known protein tertiary structures as part of the bioinformatic approach, identifying variable to conserved residues and possible interactions (Figures 1 and 2). Modeling of the variant NPC2 protein was performed using I-TASSER30.
Figure 1.
Mapping of the coding variants onto the known structure of NPC2. Probably damaging mutations are labeled with red circles. The human NPC2 structural model (from positions 20 to 149) was created using Modeller based on the bovine NPC2 structure (PDB:2HKA)37. Human NPC2 ribbon is colored according to evolutionary conservation using ConSurf server38; 39. Cholesterol sulfate (from PDB:2HKA)37 is shown in sticks. Beta strands are labeled (A to G).
Figure 2.
Mapping human N-terminal domain (NTD)-NPC1 mutants. Probably and possibly damaging mutations are labeled with red circles. The human NTD-NPC1 (PDB:3GKI)40 ribbon was colored according to evolutionary conservation using the ConSurf server39; 40. Cholesterol is shown in sticks. None of the NTD-NPC1 mutants is located at cholesterol interacting residues.
Single coding nucleotide variants were interrogated in silico by three different predictive software packages Polyphen-2,25 SIFT,26 Mutation assessor27. Polyphen-2 provides a predicted assignment of “Benign”, “Possibly Damaging”, or “Probably Damaging” as well as a false discovery rate (FDR) for each single coding nucleotide variant call. For the determination of the pathogenesis of a single coding nucleotide variants Polyphen-2 calls of “Possibly Damaging”, or “Probably Damaging” were considered pathogenic. SIFT uses the same terminology as Polyphen-2 and the same approach was used. Mutation assessor has four predictive determinants predictive nonfunctional low, non-functional neutral, functional (medium), and functional (high). Mutation assessor predictions of functional (medium), and functional (high) where considered pathogenic. When the three predictive algorithms were discrepant and no published data supporting pathogenicity was available, we accepted the prediction of two of the three programs. Potential splice variants were processed in MaxEntScan28 to provide a predictive determination of the variants affect on splicing; these were reported as “Strongly Negative”, “Negative”, or “Neutral”. Potential splice variants that were classified as Negative or Strongly Negative were considered to be pathogenic. All pathogenic variants were assumed to be fully penetrant.
Determination of predicted disease incidence
Once potential pathogenic variants were identified and a carrier frequency determined, the predicted disease incidence was calculated assuming a Hardy-Weinberg-Equilibrium (HWE). For this estimate we assumed that all pathogenic variants were fully penetrant. The HWE model also assumes that allelic variation is at equilibrium and thus not undergoing active selective pressure. Given that NPC1 is a receptor for filoviruses and its association with body mass, an assumption of neutral selection may not be correct. However, Al-Daghri et al31 concluded selective pressure on NPC1 in humans is weak to neutral. We made the assumption that allelic frequencies were consistent across different ethnic groups represented in our dataset. The potential error making this assumption is greatest for the ESP cohort given that it includes large number of individuals of either European or African descent. We evaluated our data for reduction of heterozygosity due to ethnic difference (Wahlund effect) by determining a weighted frequency; however, only negligible changes were observed for any of the NPC1 or NPC2 pathogenic alleles (data not shown). Given the negligible effect the weighted frequencies were not applied to carrier frequency calculations.
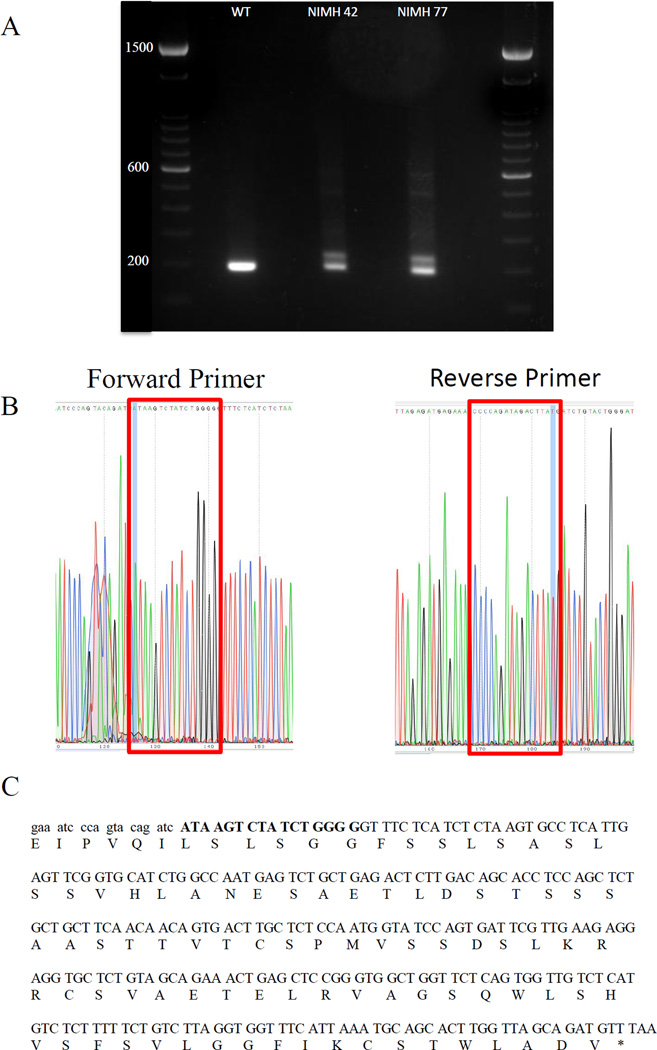
Cloning and Sequence Analysis of the c.441+1G>A Variant Discovered in NPC2
Two heterozygous Epstein-Barr virus transformed lymphoblast cell lines for the c.441+1G>A variant, NIMH 42 and NIMH 77, were identified in the NIH inter-institute collaboration on Autism. These 2 lines and one control line were grown under standard growth conditions15% fetal bovine serum in RPMI (Life Technologies) for 3 days. Cell pellets were isolated and mRNA isolated as per manufactures protocol (Qiagen). Forward primer NPC2-F3 5’-GGTGGAGTGGCAACTTCAGG-3’ and Reverse primer NPC2-R2 5’-CACTGGATACCATTGGAGAGC-3’ were used to reverse transcribe the mRNA using Superscript III One-step RT-PCR System (Life Technologies). The cDNA was visualized on a 1.5% agarose gel. One band was observed for WT and two for NIMH 42 and NIMH 77. All bands were gel purified and cloned into the TOPO TA Cloning Kit for Sequencing (Life Technologies). Isolated colonies were grown overnight in LB-ampicillin and plasmid DNA was isolated (Qiagen). Sequencing was performed on a 3500xL Genetic Analyzer (Life Technologies) using BigDye sequencing kit as per manufacturer’s protocol.
Results
Analysis of exomic sequence data from 17,754 chromosomes as compared to the human reference sequence for NPC1 and NPC2, led to the identification of 16,455 and 271 nonsynonymous sequence variants in NPC1 and NPC2, respectively. The 16,455 variants identified in NPC1 were comprised of 147 distinct variants that included 129 coding single nucleotide base variants, 9 splice site changes, and 9 insertions/deletions (Table 1). The 271 nonsynonymous variants identified in NPC2 included 14 distinct changes consisting of 12 coding single nucleotide base variants and 2 splice site changes (Table 2).
Table 1.
This table summarizes the 16,455 distinct variants detected in NPC1. Each variant has a corresponding cDNA nucleotide number, protein change, and reference SNP “RS” number when available. The majority have been assigned either a Polyphen-2, SIFT, Mutation assessor, or MaxEntScan scores, as well variants that have been previously published are noted. Variants considered non-pathogenic are shaded grey. The number of alleles analyzed for each variant and the total number of times the variant was detected are noted in conjunction with the frequency of each variant in each of the four data sets and the carrier rate for each variant.
| cDNA | Protein | rs# | Polyphen-2/MaxEntScan/Published |
|---|---|---|---|
| c.110A>G | p.D37G | BENIGN | |
| c.127G>A | p.E43K | rs138277307 | BENIGN |
| c.180G>T | p.Q60H | rs145666943 | BENIGN |
| c.181-4A>C | intronic | rs374571310 | Neutral |
| c.181-3A>G | intronic | rs371126954 | Strong Negative Effect |
| c.209A>G | p.N70S | rs200291759 | BENIGN |
| c.233G>A | p.R78Q | rs373274825 | BENIGN |
| c.346C>T | p.R116X | rs144973225 | PROBABLY DAMAGING/Published |
| c.347G>A | p.R116Q | rs140952850 | BENIGN |
| c.410C>T | p.T137M | rs372947142 | BENIGN/Published |
| c.424_425insGA | p.K142Rfs | ||
| c.442G>C | p.V148L | rs200323346 | BENIGN |
| c.445G>A | p.G149R | rs143205855 | BENIGN |
| c.449A>G | p.Q150R | rs375940577 | BENIGN |
| c.466A>G | p.M156V | rs149074243 | BENIGN |
| c.467T>C | p.M156T | rs147615070 | BENIGN |
| c.481C>T | p.R161W | rs141243713 | PROBABLY DAMAGING |
| c.520G>C | p.G174R | rs370098528 | PROBABLY DAMAGING |
| c.544G>A | p.D182N | rs201021988 | BENIGN |
| c.547G>A | p.A183T | rs111256741 | BENIGN |
| c.548C>T | p.A183V | rs192963719 | BENIGN |
| c.553A>G | p.N185D | rs139485263 | BENIGN |
| c.622G>C | p.V208L | rs372416248 | BENIGN |
| c.631G>T | p.D211Y | rs367851289 | PROBABLY DAMAGING |
| c.644A>G | p.H215R | rs1805081 | BENIGN/Known polymorphism |
| c.665A>G | p.N222S | rs55680026 | BENIGN/Published |
| c.688_693del | p.S230_V231del | Published | |
| c.695A>G | p.D232G | rs201956601 | BENIGN |
| c.709C>T | p.P237S | rs80358251 | BENIGN/Published benign |
| c.749A>C | p.K250T | BENIGN | |
| c.763C>T | p.P255S | rs373815982 | POSSIBLY DAMAGING |
| c.764C>G | p.P255R | rs371023983 | PROBABLY DAMAGING |
| c.769C>T | p.P257S | rs368776731 | BENIGN |
| c.782C>T | p.T261M | rs374169117 | BENIGN |
| c.797A>G | p.D266G | rs370188327 | POSSIBLY DAMAGING |
| c.806A>G | p.Y269C | POSSIBLY DAMAGING | |
| c.811A>G | p.I271V | rs370810779 | BENIGN |
| c.841C>T | p.L281F | rs377132020 | BENIGN |
| c.873G>T | p.W291C | rs138151007 | BENIGN |
| c.901G>A | p.E301K | rs150154006 | POSSIBLY DAMAGING |
| c.962C>T | p.A321V | rs138079168 | BENIGN |
| c.979G>A | p.V327I | rs141361998 | BENIGN |
| c.1001G>C | p.C334S | rs199693280 | BENIGN |
| c.1010G>A | p.R337Q | rs373390781 | BENIGN |
| c.1022G>C | p.R341P | rs370181667 | BENIGN |
| c.1039G>A | p.V347I | rs376741451 | BENIGN |
| c.1055G>T | p.C352F | rs149020783 | BENIGN |
| c.1094C>T | p.S365L | rs200243024 | POSSIBLY DAMAGING |
| c.1115G>A | p.R372Q | rs150053420 | BENIGN |
| c.1166G>A | p.R389H | rs373751051 | POSSIBLY DAMAGING |
| c.1208T>C | p.F403S | rs371234970 | PROBABLY DAMAGING |
| c.1211G>A | p.R404Q | rs139751448 | PROBABLY DAMAGING/Published |
| c.1232G>A | p.R411Q | rs77080672 | BENIGN |
| c.1270C>G | p.P424A | rs143797098 | BENIGN |
| c.1274C>T | p.S425L | rs140149624 | BENIGN |
| c.1300C>T | p.P434S | rs61731962 | BENIGN/Known polymorphism |
| c.1346C>T | p.A449V | rs372289265 | BENIGN |
| c.1348A>G | p.I450V | rs141892620 | BENIGN |
| c.1367C>T | p.S456F | rs374159264 | BENIGN |
| c.1412C>T | p.P471L | rs201226297 | PROBABLY DAMAGING |
| c.1421C>T | p.P474L | rs372445155 | PROBABLY DAMAGING/Published |
| c.1472G>A | p.S491N | rs370758521 | BENIGN |
| c.1480G>A | p.V494M | rs199812609 | BENIGN |
| c.1506C>G | p.D502E | rs191537721 | BENIGN |
| c.1532C>T | p.T511M | rs13381670 | PROBABLY DAMAGING |
| c.1549G>A | p.V517I | rs201791992 | BENIGN |
| c.1552C>T | p.R518W | rs377515417 | PROBABLY DAMAGING/Published |
| c.1561G>T | p.A521S | rs138184115 | BENIGN/Published |
| c.1628C>T | p.P543L | rs369368181 | PROBABLY DAMAGING/Published |
| c.1672G>T | p.A558S | rs201156397 | POSSIBLY DAMAGING/Published |
| c.1756G>A | p.E586K | rs369753548 | BENIGN |
| c.1766A>G | p.N589S | rs147021046 | BENIGN |
| c.1780_1781insT | p.Y594Lfs | ||
| c.1793A>G | p.N598S | rs201236716 | BENIGN |
| c.1870G>A | p.V624I | rs76615690 | BENIGN |
| c.1901A>G | p.Y634C | rs202140203 | PROBABLY DAMAGING/Published |
| c.1936C>T | p.R646C | rs368129141 | POSSIBLY DAMAGING |
| c.1937G>A | p.R646H | rs112387560 | BENIGN |
| c.1976C>T | p.A659V | rs140786703 | POSSIBLY DAMAGING |
| c.1990G>A | p.V664M | rs376213990 | PROBABLY DAMAGING/Published |
| c.2020_2021del | p.V674Lfs | ||
| c.2027G>C | p.S676T | PROBABLY DAMAGING | |
| c.2083C>G | p.L695V | rs370323921 | PROBABLY DAMAGING/Published |
| c.2141G>A | p.R714H | rs375047023 | PROBABLY DAMAGING |
| c.2209C>G | p.L737V | rs201100763 | PROBABLY DAMAGING |
| c.2257G>A | p.V753M | rs146874573 | BENIGN |
| c.2338G>A | p.V780M | rs193182840 | PROBABLY DAMAGING |
| c.2428G>T | p.V810L | rs145362908 | BENIGN |
| c.2428G>C | p.V810L | rs145362908 | BENIGN |
| c.2501T>C | p.M834T | rs373435883 | BENIGN |
| * c.2524T>C | p.F842L | rs190298665 | PROBABLY DAMAGING |
| c.2525T>C | p.F842S | rs374068891 | PROBABLY DAMAGING |
| c.2551G>A | p.A851T | rs139297968 | POSSIBLY DAMAGING |
| c.2572A>G | p.I858V | rs1805082 | BENIGN/Known polymorphism |
| c.2605-6_2605-3del | intronic | Neutral | |
| c.2621A>T | p.D874V | rs372030650 | POSSIBLY DAMAGING/Published |
| c.2705C>G | p.S902C | rs374656358 | BENIGN |
| c.2731G>A | p.G911S | rs34302553 | BENIGN |
| c.2796-4C>T | intronic | rs374406578 | Neutral |
| c.2800C>T | p.R934X | rs370721218 | PROBABLY DAMAGING/Published |
| c.2819C>T | p.S940L | rs143124972 | PROBABLY DAMAGING/Published |
| c.2873G>A | p.R958Q | rs120074132 | PROBABLY DAMAGING/Published |
| c.2882A>G | p.N961S | rs34084984 | BENIGN/Published |
| c.2908_2909insTT | p.S970Ffs | ||
| c.2911+4C>T | intronic | rs186588103 | Neutral |
| c.2929+4C>T | intronic | rs186588103 | Neutral |
| c.2972_2973del | p.991_fs | Published | |
| c.2974G>T | p.G992W | rs80358254 | PROBABLY DAMAGING/Published |
| c.3011C>T | p.S1004L | rs150334966 | PROBABLY DAMAGING/Published |
| c.3019C>G | p.P1007A | rs80358257 | PROBABLY DAMAGING/Published |
| c.3028A>C | p.K1010Q | rs191876836 | BENIGN |
| c.3047A>G | p.H1016R | rs140211089 | POSSIBLY DAMAGING/Published |
| c.3052G>A | p.A1018T | rs146666146 | PROBABLY DAMAGING |
| c.3059G>C | p.S1020T | rs374719153 | BENIGN |
| c.3182T>C | p.I1061T | rs80358259 | BENIGN/Published |
| c.3184G>A | p.A1062T | rs369960141 | POSSIBLY DAMAGING |
| c.3217G>A | p.G1073S | rs141440861 | BENIGN |
| c.3265G>A | p.E1089K | rs374526072 | PROBABLY DAMAGING/Published |
| c.3343G>T | p.V1115F | rs34226296 | BENIGN |
| c.3364T>C | p.W1122R | rs148571882 | BENIGN |
| c.3422T>G | p.V1141G | rs144725473 | PROBABLY DAMAGING/Published |
| c.3477+4A>G | intronic | rs114073738 | Neutral |
| c.3498+4A>G | intronic | Negative | |
| c.3506G>T | p.S1169I | rs139612110 | PROBABLY DAMAGING |
| c.3535A>G | p.M1179V | rs61731969 | BENIGN |
| c.3548G>A | p.R1183H | rs148035987 | PROBABLY DAMAGING |
| c.3550G>A | p.V1184M | POSSIBLY DAMAGING | |
| c.3556C>T | p.R1186C | rs145297180 | PROBABLY DAMAGING |
| c.3557G>A | p.R1186H | rs200444084 | PROBABLY DAMAGING/Published |
| c.3560C>T | p.A1187V | rs113371321 | POSSIBLY DAMAGING/Published |
| c.3566A>G | p.E1189G | rs369098773 | POSSIBLY DAMAGING/Published |
| c.3577C>T | p.H1193Y | rs375309094 | BENIGN |
| c.3598A>G | p.S1200G | rs35248744 | PROBABLY DAMAGING/Published |
| c.3611_3614del | p.L1204Qfs | Published | |
| c.3619T>C | p.F1207L | rs140827681 | BENIGN |
| c.3667A>G | p.I1223V | rs368658600 | BENIGN |
| c.3689T>C | p.L1230S | rs374150662 | PROBABLY DAMAGING |
| c.3741_3745A | 0 | ||
| c.3742_3745del | p.L1248Vfs | Published | |
| c.3755-5_3755-4insTC | intronic | Neutral | |
| c.3796C>T | p.R1266X | rs376164368 | PROBABLY DAMAGING |
| c.3797G>A | p.R1266Q | rs1805084 | BENIGN/Known polymorphism |
| c.3799T>G | p.Y1267D | rs373435628 | BENIGN |
| c.3811G>C | p.E1271Q | rs140527006 | POSSIBLY DAMAGING |
| c.3814C>T | p.R1272C | rs200264267 | PROBABLY DAMAGING |
| c.3818A>G | p.E1273G | rs374032318 | BENIGN |
| c.3821G>A | p.R1274Q | rs151305963 | BENIGN |
| Total Alleles | Total Variants | NHLBI | 1000 Genome | Clinseq | Autism | Rate |
|---|---|---|---|---|---|---|
| 17754 | 1 | 0 | 0 | 1 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 5 | 4 | 1 | 0 | 0 | 0.03% |
| 17754 | 2 | 2 | 0 | 0 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 1 | 0 | 1 | 0 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 2 | 2 | 0 | 0 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17266 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 2 | 0 | 2 | 0 | 0 | 0.01% |
| 17754 | 2 | 1 | 1 | 0 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 6 | 6 | 0 | 0 | 0 | 0.03% |
| 17734 | 2 | 1 | 0 | 1 | 0 | 0.01% |
| 17754 | 2 | 2 | 0 | 0 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 2 | 1 | 1 | 0 | 0 | 0.01% |
| 17754 | 7 | 4 | 3 | 0 | 0 | 0.04% |
| 17754 | 1 | 0 | 1 | 0 | 0 | 0.01% |
| 17752 | 4 | 3 | 0 | 1 | 0 | 0.02% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17696 | 5250 | 3849 | 535 | 646 | 220 | 29.67% |
| 17748 | 71 | 59 | 2 | 9 | 1 | 0.40% |
| 17226 | 3 | 3 | 0 | 0 | 0 | 0.02% |
| 17754 | 1 | 0 | 1 | 0 | 0 | 0.01% |
| 17730 | 183 | 150 | 14 | 15 | 4 | 1.03% |
| 17754 | 1 | 0 | 0 | 0 | 1 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17746 | 1 | 0 | 0 | 1 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 10 | 7 | 2 | 1 | 0 | 0.06% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17750 | 2 | 1 | 1 | 0 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 1 | 0 | 0 | 1 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 2 | 2 | 0 | 0 | 0 | 0.01% |
| 17754 | 2 | 2 | 0 | 0 | 0 | 0.01% |
| 17754 | 2 | 0 | 0 | 2 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 34 | 26 | 5 | 1 | 2 | 0.19% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17752 | 212 | 189 | 18 | 3 | 2 | 1.19% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17752 | 5 | 3 | 0 | 2 | 0 | 0.03% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 1 | 0 | 1 | 0 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 1 | 0 | 1 | 0 | 0 | 0.01% |
| 17754 | 51 | 42 | 8 | 0 | 1 | 0.29% |
| 17754 | 1 | 0 | 1 | 0 | 0 | 0.01% |
| 17754 | 2 | 2 | 0 | 0 | 0 | 0.01% |
| 17754 | 9 | 9 | 0 | 0 | 0 | 0.05% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17704 | 1 | 0 | 0 | 1 | 0 | 0.01% |
| 17754 | 2 | 2 | 0 | 0 | 0 | 0.01% |
| 17732 | 8 | 7 | 0 | 1 | 0 | 0.05% |
| 17266 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 1 | 0 | 1 | 0 | 0 | 0.01% |
| 17754 | 2 | 0 | 2 | 0 | 0 | 0.01% |
| 17752 | 1 | 0 | 0 | 1 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 7 | 4 | 3 | 0 | 0 | 0.04% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17266 | 319 | 319 | 0 | 0 | 0 | 1.85% |
| 17754 | 1 | 0 | 0 | 0 | 1 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 2 | 2 | 0 | 0 | 0 | 0.01% |
| 17754 | 1 | 0 | 0 | 1 | 0 | 0.01% |
| 17754 | 2 | 2 | 0 | 0 | 0 | 0.01% |
| 17754 | 1 | 0 | 1 | 0 | 0 | 0.01% |
| 17754 | 8 | 5 | 3 | 0 | 0 | 0.05% |
| 17752 | 1 | 0 | 0 | 1 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 1 | 0 | 1 | 0 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 2 | 2 | 0 | 0 | 0 | 0.01% |
| 17752 | 8005 | 5758 | 1100 | 864 | 283 | 45.09% |
| 17266 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 69 | 63 | 3 | 0 | 3 | 0.39% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 69 | 56 | 11 | 1 | 1 | 0.39% |
| 17266 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 3 | 3 | 0 | 0 | 0 | 0.02% |
| 17754 | 1 | 0 | 1 | 0 | 0 | 0.01% |
| 17724 | 2 | 0 | 0 | 1 | 1 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17750 | 11 | 8 | 0 | 2 | 1 | 0.06% |
| 17754 | 3 | 2 | 1 | 0 | 0 | 0.02% |
| 17754 | 1 | 0 | 1 | 0 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 2 | 2 | 0 | 0 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 5 | 5 | 0 | 0 | 0 | 0.03% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17750 | 23 | 18 | 4 | 1 | 0 | 0.13% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 43 | 34 | 7 | 0 | 2 | 0.24% |
| 17754 | 2 | 1 | 0 | 0 | 1 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 28 | 28 | 0 | 0 | 0 | 0.16% |
| 17754 | 4 | 0 | 4 | 0 | 0 | 0.02% |
| 17754 | 2 | 2 | 0 | 0 | 0 | 0.01% |
| 17694 | 61 | 54 | 5 | 2 | 0 | 0.34% |
| 17754 | 8 | 7 | 0 | 0 | 1 | 0.05% |
| 17676 | 1 | 0 | 0 | 1 | 0 | 0.01% |
| 17754 | 2 | 2 | 0 | 0 | 0 | 0.01% |
| 17754 | 2 | 1 | 1 | 0 | 0 | 0.01% |
| 17754 | 1 | 0 | 1 | 0 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 63 | 61 | 1 | 0 | 1 | 0.35% |
| 17264 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17748 | 1 | 0 | 0 | 1 | 0 | 0.01% |
| 17266 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17266 | 4 | 4 | 0 | 0 | 0 | 0.02% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 1724 | 1275 | 307 | 101 | 41 | 9.71% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 1 | 0 | 1 | 0 | 0 | 0.01% |
| 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| 17754 | 5 | 4 | 0 | 0 | 1 | 0.03% |
The asterisk indicates the one novel variant detected in the NIH patient.
Table2.
This table summarizes the 271 distinct variants detected in NPC2. Each variant has a corresponding cDNA number; protein change and reference SNP “RS” number when available. The majority have been assigned either a Polyphen-2, SIFT, Mutation assessor, or MaxEntScan score, as well variants that have been previously published are noted. Variants considered non-pathogenic are shaded grey. The number of alleles analyzed for each variant and the total number of times the variant was detected is noted in conjunction with the frequency of each variant in each of the four data sets and the carrier rate for each variant.
| cDNA | Protein | rs# | Polyphen-2/MaxEntScan/Published | Total Alleles | Total Variants | NHLBI | 1000 Genome | Clinseq | Autism | Rate |
|---|---|---|---|---|---|---|---|---|---|---|
| c.38T>C | p.L13P | rs147602717 | PROBABLY DAMAGING | 17360 | 5 | 4 | 0 | 1 | 0 | 0.03% |
| c.49G>A | p.A17T | rs145302203 | BENIGN | 17748 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| c.56C>A | p.A19D | rs369392502 | PROBABLY DAMAGING | 17748 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| c.58G>T | p.E20X | rs80358260 | Published | 17750 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| c.88G>A | p.V30M | rs151220873 | POSSIBLY DAMAGING/Published | 17252 | 34 | 25 | 1 | 4 | 4 | 0.20% |
| c.115G>A | p.V39M | rs80358261 | PROBABLY DAMAGING/Published | 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| c.212A>G | p.K71R | rs142075589 | POSSIBLY DAMAGING | 17754 | 3 | 2 | 1 | 0 | 0 | 0.02% |
| c.224A>T | p.H75L | rs369221608 | PROBABLY DAMAGING | 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| c.271G>A | p.D91N | rs148607507 | POSSIBLY DAMAGING | 17754 | 10 | 8 | 0 | 2 | 0 | 0.06% |
| c.278G>T | p.C93F | rs143960270 | PROBABLY DAMAGING/Published | 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| c.292A>C | p.N98H | rs142858704 | BENIGN | 17754 | 12 | 11 | 1 | 0 | 0 | 0.07% |
| c.340C>G | p.P114A | rs371363324 | PROBABLY DAMAGING | 17754 | 1 | 1 | 0 | 0 | 0 | 0.01% |
| c.441+1G>A | intronic | rs140130028 | Strong Negative/Published | 17752 | 96 | 83 | 0 | 6 | 7 | 0.54% |
| c.442-4A>C | intronic | rs114950106 | Neutral | 17754 | 104 | 104 | 0 | 0 | 0 | 0.59% |
The Human Gene Mutation Database HGMD®29 was queried to establishing what observed variants in this data set might be pathogenic. For NPC1 (Table 1) and NPC2 (Table 2), 33 (32 pathogenic and one benign variant) of 147 (22.4%) and 5 out of 14 (35.7%) variants, respectively, had previously been reported in HGMD®. One additional novel NPC1 variant, c.2524T>C (p.F842L), was present in the NIH cohort (Table 1). The combination of Polyphen-2, SIFT, and Mutation assessor classified 53 NPC1 and 8 NPC2 coding nucleotide variants as pathogenic by our criteria. Of the predicted pathogenic variants 27 (51%) and 6 (75%) have not been reported in HGMD® for NPC1 and NPC2 respectively. Polyphen-2 also calculates a false discovery rate (FDR). For NPC1 and NPC2 predicted variants, the average FDR for a prediction of “Probably” or “Possibly” damaging were 0.04% and 0.03% respectively. These low mean FDRs had a negligible effect on the carrier incidence estimate and thus were not applied to either NPC1 or NPC2 carrier frequency calculations.
For NPC1 and NPC2, 2 out of 9 and 1 of 2, potential splice mutations were predicted to be pathogenic. Of the nine insertion/deletions (indels) identified in NPC1, a two base pair deletion, c.2020_2021del, was observed 319 times only in the ESP data set and thus was removed as a technical artifact unique to the ESP data set. The eight other NPC1 indels result in a frameshift, and thus were considered pathogenic. No indels were identified in NPC2.
Based on the above analysis, for NPC1 we initially considered the 68 distinct variants meeting the criteria of pathogenic (54 identified by predictive software to be pathogenic, 4 indicated by the predictive software as “benign” but known to be pathogenic, the 2 splice variants, and the 8 insertion/deletions). This accounted for 371 pathogenic alleles with an estimated carrier rate of 2.09% (371/17,754) and a predicted NPC incidence of 1/9,160. Given the order of magnitude difference between this number and clinical estimates, this prediction is likely a significant overestimation. Thus we applied manual curation to the NPC1 data set. Four variants, c.665A>G (p.N222S), c.1532C>T (p.T511M), c.2882A>G (p.N961S), and c.3598A>G (p.S1200G), accounted for 254 out of the 371 (68%) predicted pathogenic alleles. Allelic frequencies for these four alleles were 0.400, 0.287, 0.389 and 0.355 percent respectively. Given that their individual allelic frequencies exceed the allelic frequency of p.I1061T (0.028%), the most commonly reported mutant allele in patients with mutations in NPC1, by more than a factor of 10 (Table 1), it is not plausible that these alleles are associated with classical NPC disease. Excluding these four high frequency variants based on this assertion left 117 pathogenic alleles or a 0.659% (117/17,754) carrier rate. This carrier rate predicts an incidence of NPC attributable to NPC1 of 1/92,104.
We further evaluated the decision to exclude the four high frequency alleles based on lack of an association with classical NPC disease. Although, all three predictive packages indicate both p.N222S and p.N961S to be non-pathogenic these two variants have been reported in “visceral-only” or adult-onset NPC1 cases. The p.N222S variant was reported in combination with a p.I1061T mutation in a single adult onset (35 yr) patient with variant filipin staining32. This patient initially presented with visceral disease (hepatosplenomegaly) and later manifested ataxia at 44 years of age. We have identified a p.N222S variant in combination with c.1402T>G, (p.C468G) in teenage sisters diagnosed based on splenomegaly. The second allele in this sib pair, p.C468G is predicted by Polyphen-2 to be “Probably” damaging. Pathological analysis of the spleen in the older sibling was suggestive of Niemann-Pick disease, but filipin staining was inconclusive. Neurological symptoms were absent and signs were very minor with deep tendon hyperreflexia and minor auditory brainstem response abnormalities noted on evaluation at 15 and 13 years of age respectively. NIH severity score for both was 14. Plasma oxysterol concentrations were consistent with a diagnosis of NPC in these two subjects. Mapping of p.N222S to the known tertiary structure provided no additional evidence for the pathogenicity of this residue (Figure 2). The p.N961S (c.2882A>C) variant has been reported in a compound heterozygous state with p.S666N, (c.1997G>A) (with a Polyphen-2 prediction of “Probably” damaging) in an adult case with subclinical hepatosplenamegaly and lymphadenopathy noted on autopsy following death due to acute pulmonary embolism and myocardial infarction16. Although no neurological symptoms were reported, brain pathology was notable for distended neurons with increased lipofuscin granules. Assuming one or both of these variants are pathogenic, fully penetrant and associated with late onset NPC disease, the total disease incidence of NPC1 would range from 1/19,077–1/36,420.
Although predicted to be probably damaging by Polyphen-2, neither p.T511M nor p.S1200G have been reported in NPC1 patients. Millat et al33 reported p.T511M as a novel nonpathological coding single nucleotide variant. The p.S1200G variant was reported in an “NPC uncertain” case in the recent ZOOM study14. This subject, patient 5 in the ZOOM study, was a compound heterozygote for p.V664M, a known NPC1 mutation, but plasma cholestane-3β,5α,6β-triol testing6 was negative. Current data do not support classification of either p.T511M or p.S1200G variants as pathogenic alleles.
Sequence analysis of NPC2 (Table 2) identified 151 potential pathogenic alleles and calculated a pathogenic carrier frequency of 0.85% (151/17,754). Again the predicted disease incidence, 1/55,297 did not appear to be realistic unless one proposed an extreme degree of under-ascertainment. Thus, we similarly applied manual curation to the NPC2 data set. Review of the NPC2 data identified two high frequency variants that dominated the frequency calculation c.441+1G>A and c.88G>A (p.V30M), both variants are reported in HMGD®. The splice variant, c.441+1G>C, was predicted to be “Strongly Negative” by MaxEntScan. Molecular analysis of independent cell lines revealed multiple splicing events. The most prominent errant splicing event results in the insertion of 16 bases that leads to the alteration of the terminal 4 amino acids and the addition of 86 additional amino acids to the protein (supplemental figure1). Multiple lines of evidence strongly indicate that this errant splicing results in a functional protein. First, the variant has not been reported in association with a patient with NPC. Second, modeling of the variant protein using I-TASSER30 found no alterations to the cholesterol binding pocket or stability of the protein (data not shown). Finally, Huang et al. have demonstrated that generation of an NPC2 fusion protein with mCherry fused to the carboxy-terminal end of the protein is fully functional and is able to correct the NPC cellular phenotype in Npc2−/− mouse embryonic fibroblasts34. As such we have excluded c.441+1G>C as a pathogenic allele. The p.V30M variant, with a allelic frequency of 0.197%, is predicted to be possibly damaging by Polyphen-2 and SIFT but considered non-pathogenic by mutation assessor. The one reported NPC subject with the p.V30M variant was classified as a phenotypic NPC variant, a second mutation was not identified and near normal levels of cholesterol esterification was reported in skin fibroblasts35. Inclusion of the p.V30M allele predicts a disease incidence of NPC attributable to NPC2 of 1/402,400 and that NPC2 should account for 18.6% of patients with NPC. This latter prediction conflicts with clinical data indicating that NPC2 account for only 2–5% of all patients with NPC1; 2. Sequence alignment and structural analyses demonstrate that the p.V30 residue is not evolutionarily conserved and is present in a structurally variable region of the NPC2 protein well away from its binding pocket (Figure 1). Furthermore, p.V30M is found at a higher frequency than any known pathogenic NPC2 allele, coupled with the lack of evidence supporting functional importance and ultimately the lack of any clinical correlation, has lead us to exclude p.V30M as a pathogenic allele. We are, therefore, left with 21 pathogenic alleles (0.118% carrier frequency) and a predicted disease incidence of 1/2,858,998 conceptions for NPC2.
Based on the above analysis of both NPC1 and NPC2, the combined incidence is predicted to be 1/89,229 or 1.12 cases per 100,000 conceptions and the fraction of NPC2 cases is predicted to be 3.1%. The predicted number of cases is slightly more than the 0.96 cases per 100,000 conceptions reported by Vanier2 when she accounted for prenatal cases and the fraction of NPC2 cases is consistent with prior clinical observation of 2–5%1–3.
Discussion
The impact of NPC1 variation on human health may be significant. Work by multiple groups has demonstrated that c.644A>G (p.H215R) is associated with obesity36. In this analysis of NPC1 variants we identified the p.H215R variant in almost a third of the NPC1 alleles. Our work now demonstrates that two relatively common NPC1 variants with a combined carrier frequency approaching 0.8% may contribute, in compound heterozygous state, to a late-onset NPC1 phenotype for which the phenotypic spectrum and clinical significance remains to be defined. This late-onset NPC1 phenotype may represent a milder manifestation of NPC1 deficiency with predominately visceral manifestations. The degree to which this late-onset NPC1 phenotype is associated with high frequency NPC1 alleles and the adult-onset NPC1 phenotype that includes significant neurological and psychological symptoms also remains to be defined.
Failure to ascertain certain alleles in patients such as the p.V30M in NPC2 or the p.T511M and p.S1200G in NPC1 could be due to prenatal lethality; however, as NPC is an autosomal recessive disorder, it is difficult to hypothesize a plausible mechanism, such as a dominant inhibitory function, by which these alleles would uniquely result in prenatal lethality.
Based on clinical case reports, one needs to consider the possibility that p.N222S and p.N961S maybe pathogenic with allelic frequencies of 0.400 and 0.389 percent respectively. The evidence for clinical relevance is strongest for p.N222S, which has been observed in two independent cases with similar visceral and delayed neurological manifestations, variant filipin staining in fibroblasts, and positive plasma oxysterol testing in the siblings. Assuming pathogenicity is related to a compound heterozygous state and full penetrance, the combined frequency of p.N222S with another pathogenic NPC1 mutation would be 1/35,667. Although only limited data are available, if one includes p.N961S based on a single report with no supporting diagnostic testing, the incidence of a late onset variant of NPC1 disease would increase to 1/19,077. Another possible to explanation of these high predicted incidences is that some individuals harboring these variants either in combination with another pathogenic allele or in the homozygous state may be asymptomatic or only manifest subclinical signs.
Leveraging existing “whole exome sequence” data we have estimated the disease incidence of NPC utilizing both bioinformatic tools and manual curation. With respect to classical NPC disease, we estimate that the incidence of NPC1 and NPC2 are on the order of 1/92,000 and 1/2,900,000, respectively, with a combined incidence of approximately 1/89,000. These estimates are in agreement with previous clinical estimates. Thus, our data does not support significant under-ascertainment of classical NPC cases. Concurrence with clinical data also suggests that we are not missing a significant number of alleles, such as large indels or intronic mutations that are not detected by “whole exome sequencing.” However, our data suggests that there may be significant under-ascertainment of a late-onset NPC1 phenotype. This late-onset phenotype may present as visceral-only or neurological mild NPC1, and with a potential incidence of 1/19,000–1/39,000. Further work is necessary to fully delineate this late-onset NPC1 phenotype, but the current study suggests that NPC should be considered in individuals with visceral lipidosis or unexplained neurological and psychiatric symptoms.
Supplementary Material
Supplemental Figure 1: Provides the molecular characterization of the c.441+1G>C NPC2 splice variant. A) Shows the products of the reverse transcription-PCR amplification of the region surrounded the exon 4/5 junction, visualized on a 1.8% agarose gel. The WT cell line presents a single 192 base band while both line heterozygous for the splice variant present with the control band and an alternately spliced prominent slightly larger band. B) Sequencing of the larger prominent alternative splice revealed the insertion of 16 nucleotides. C) Resulting sequence and frameshift as a result of the 16 base insertion.
Acknowledgements
J. L. C., J. I., C.L., A. T., S. S., J.E.B-W., L. G. B., F. D. P., and C. A. W. supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development or the National Human Genome Research Institute intramural research programs, DHHS. J.L.C. C.A.W. is a NIH/Oxford Scholar and J.L.C is a Wellcome Trust/NIH Scholar. F.M.P. is a Royal Society Wolfson Research Merit Award holder. L. G. B. is an uncompensated advisor to the Illumina Corporation and receives royalties from the Genentech Corporation; all other authors report no conflict of interest.
L. G. B. is an uncompensated advisor to the Illumina Corporation and receives royalties from the Genentech Corporation;
Footnotes
All other authors report no conflict of interest.
References
- 1.Patterson MC, Hendriksz CJ, Walterfang M, Sedel F, Vanier MT, Wijburg F Group, N.-C.G.W. Recommendations for the diagnosis and management of Niemann-Pick disease type C: an update. Molecular genetics and metabolism. 2012;106:330–344. doi: 10.1016/j.ymgme.2012.03.012. [DOI] [PubMed] [Google Scholar]
- 2.Vanier MT. Niemann-Pick disease type C. Orphanet journal of rare diseases. 2010;5:16. doi: 10.1186/1750-1172-5-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jahnova H, Dvorakova L, Vlaskova H, Hulkova H, Poupetova H, Hrebicek M, Jesina P. Observational, retrospective study of a large cohort of patients with Niemann-Pick disease type C in the Czech Republic: a surprisingly stable diagnostic rate spanning almost 40 years. Orphanet journal of rare diseases. 2014;9:140. doi: 10.1186/s13023-014-0140-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yanjanin NM, Velez JI, Gropman A, King K, Bianconi SE, Conley SK, Brewer CC, Solomon B, Pavan WJ, Arcos-Burgos M, et al. Linear clinical progression, independent of age of onset, in Niemann-Pick disease, type C. Am J Med Genet B Neuropsychiatr Genet. 2010;153B:132–140. doi: 10.1002/ajmg.b.30969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.te Vruchte D, Speak AO, Wallom KL, Al Eisa N, Smith DA, Hendriksz CJ, Simmons L, Lachmann RH, Cousins A, Hartung R, et al. Relative acidic compartment volume as a lysosomal storage disorder-associated biomarker. Journal of Clinical Investigation. 2014;124:1320–1328. doi: 10.1172/JCI72835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Porter FD, Scherrer DE, Lanier MH, Langmade SJ, Molugu V, Gale SE, Olzeski D, Sidhu R, Dietzen DJ, Fu R, et al. Cholesterol oxidation products are sensitive and specific blood-based biomarkers for Niemann-Pick C1 disease. Science translational medicine. 2010;2:56ra81. doi: 10.1126/scitranslmed.3001417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ottinger EA, Kao ML, Carrillo-Carrasco N, Yanjanin N, Shankar RK, Janssen M, Brewster M, Scott I, Xu X, Cradock J, et al. Collaborative development of 2-hydroxypropyl-beta-cyclodextrin for the treatment of Niemann-Pick type C1 disease. Current topics in medicinal chemistry. 2014;14:330–339. doi: 10.2174/1568026613666131127160118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim SJ, Lee BH, Lee YS, Kang KS. Defective cholesterol traffic and neuronal differentiation in neural stem cells of Niemann-Pick type C disease improved by valproic acid, a histone deacetylase inhibitor. Biochem Biophys Res Commun. 2007;360:593–599. doi: 10.1016/j.bbrc.2007.06.116. [DOI] [PubMed] [Google Scholar]
- 9.Munkacsi AB, Chen FW, Brinkman MA, Higaki K, Gutierrez GD, Chaudhari J, Layer JV, Tong A, Bard M, Boone C, et al. An "exacerbate-reverse" strategy in yeast identifies histone deacetylase inhibition as a correction for cholesterol and sphingolipid transport defects in human Niemann-Pick type C disease. J Biol Chem. 2011;286:23842–23851. doi: 10.1074/jbc.M111.227645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pipalia NH, Cosner CC, Huang A, Chatterjee A, Bourbon P, Farley N, Helquist P, Wiest O, Maxfield FR. Histone deacetylase inhibitor treatment dramatically reduces cholesterol accumulation in Niemann-Pick type C1 mutant human fibroblasts. Proceedings of the National Academy of Sciences of the United States of America. 2011;108:5620–5625. doi: 10.1073/pnas.1014890108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xu M, Liu K, Swaroop M, Porter FD, Sidhu R, Firnkes S, Ory DS, Marugan JJ, Xiao J, Southall N, et al. delta-Tocopherol reduces lipid accumulation in Niemann-Pick type C1 and Wolman cholesterol storage disorders. J Biol Chem. 2012;287:39349–39360. doi: 10.1074/jbc.M112.357707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zech M, Nubling G, Castrop F, Jochim A, Schulte EC, Mollenhauer B, Lichtner P, Peters A, Gieger C, Marquardt T, et al. Niemann-Pick C disease gene mutations and age-related neurodegenerative disorders. PloS one. 2013;8:e82879. doi: 10.1371/journal.pone.0082879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schicks J, Muller Vom Hagen J, Bauer P, Beck-Wodl S, Biskup S, Krageloh-Mann I, Schols L, Synofzik M. Niemann-Pick type C is frequent in adult ataxia with cognitive decline and vertical gaze palsy. Neurology. 2013;80:1169–1170. doi: 10.1212/WNL.0b013e31828869f9. [DOI] [PubMed] [Google Scholar]
- 14.Bauer P, Balding DJ, Klunemann HH, Linden DE, Ory DS, Pineda M, Priller J, Sedel F, Muller A, Chadha-Boreham H, et al. Genetic screening for Niemann-Pick disease type C in adults with neurological and psychiatric symptoms: findings from the ZOOM study. Human molecular genetics. 2013;22:4349–4356. doi: 10.1093/hmg/ddt284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bonnot O, Klunemann HH, Sedel F, Tordjman S, Cohen D, Walterfang M. Diagnostic and treatment implications of psychosis secondary to treatable metabolic disorders in adults: a systematic review. Orphanet journal of rare diseases. 2014;9:65. doi: 10.1186/1750-1172-9-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dvorakova L, Sikora J, Hrebicek M, Hulkova H, Bouckova M, Stolnaja L, Elleder M. Subclinical course of adult visceral Niemann-Pick type C1 disease. A rare or underdiagnosed disorder? Journal of inherited metabolic disease. 2006;29:591. doi: 10.1007/s10545-006-0330-z. [DOI] [PubMed] [Google Scholar]
- 17.Fensom AH, Grant AR, Steinberg SJ, Ward CP, Lake BD, Logan EC, Hulman G. An adult with a non-neuronopathic form of Niemann-Pick C disease. Journal of inherited metabolic disease. 1999;22:84–86. doi: 10.1023/a:1005463718823. [DOI] [PubMed] [Google Scholar]
- 18.Frohlich E, Harzer K, Heller T, Ruhl U. [Ultrasound echogenic splenic tumors: nodular manifestation of type C Niemann-Pick disease] Ultraschall in der Medizin. 1990;11:119–122. doi: 10.1055/s-2007-1011543. [DOI] [PubMed] [Google Scholar]
- 19.Cross JL, Iben J, Simpson C, Thurm A, Swedo S, Tierney E, Bailey-Wilson J, Biesecker LG, Porter FD, Wassif CA. Determination of the Allelic Frequency in Smith-Lemli-Opitz Syndrome by Analysis of Massively Parallel Sequencing Data Sets. Clinical genetics. 2014 doi: 10.1111/cge.12425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Exome Variant Server, NHLBI GO Exome Sequencing Project (ESP) Seattle, WA: [Google Scholar]
- 21.Genomes Project C, Abecasis GR, Auton A, Brooks LD, DePristo MA, Durbin RM, Handsaker RE, Kang HM, Marth GT, McVean GA. An integrated map of genetic variation from 1,092 human genomes. Nature. 2012;491:56–65. doi: 10.1038/nature11632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Biesecker LG, Mullikin JC, Facio FM, Turner C, Cherukuri PF, Blakesley RW, Bouffard GG, Chines PS, Cruz P, Hansen NF, et al. The ClinSeq Project: piloting large-scale genome sequencing for research in genomic medicine. Genome research. 2009;19:1665–1674. doi: 10.1101/gr.092841.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chelala C, Khan A, Lemoine NR. SNPnexus: a web database for functional annotation of newly discovered and public domain single nucleotide polymorphisms. Bioinformatics. 2009;25:655–661. doi: 10.1093/bioinformatics/btn653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Haas D, Garbade SF, Vohwinkel C, Muschol N, Trefz FK, Penzien JM, Zschocke J, Hoffmann GF, Burgard P. Effects of cholesterol and simvastatin treatment in patients with Smith-Lemli-Opitz syndrome (SLOS) Journal of inherited metabolic disease. 2007;30:375–387. doi: 10.1007/s10545-007-0537-7. [DOI] [PubMed] [Google Scholar]
- 25.Adzhubei IA, Schmidt S, Peshkin L, Ramensky VE, Gerasimova A, Bork P, Kondrashov AS, Sunyaev SR. A method and server for predicting damaging missense mutations. Nature methods. 2010;7:248–249. doi: 10.1038/nmeth0410-248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kumar P, Henikoff S, Ng PC. Predicting the effects of coding non-synonymous variants on protein function using the SIFT algorithm. Nature protocols. 2009;4:1073–1081. doi: 10.1038/nprot.2009.86. [DOI] [PubMed] [Google Scholar]
- 27.Reva B, Antipin Y, Sander C. Predicting the functional impact of protein mutations: application to cancer genomics. Nucleic acids research. 2011;39:e118. doi: 10.1093/nar/gkr407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yeo G, Burge CB. Maximum entropy modeling of short sequence motifs with applications to RNA splicing signals. Journal of computational biology : a journal of computational molecular cell biology. 2004;11:377–394. doi: 10.1089/1066527041410418. [DOI] [PubMed] [Google Scholar]
- 29.Stenson PD, Mort M, Ball EV, Howells K, Phillips AD, Thomas NS, Cooper DN. The Human Gene Mutation Database: 2008 update. Genome medicine. 2009;1:13. doi: 10.1186/gm13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Roy A, Kucukural A, Zhang Y. I-TASSER: a unified platform for automated protein structure and function prediction. Nature protocols. 2010;5:725–738. doi: 10.1038/nprot.2010.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Al-Daghri NM, Cagliani R, Forni D, Alokail MS, Pozzoli U, Alkharfy KM, Sabico S, Clerici M, Sironi M. Mammalian NPC1 genes may undergo positive selection and human polymorphisms associate with type 2 diabetes. BMC medicine. 2012;10:140. doi: 10.1186/1741-7015-10-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tangemo C, Weber D, Theiss S, Mengel E, Runz H. Niemann-Pick Type C disease: characterizing lipid levels in patients with variant lysosomal cholesterol storage. Journal of lipid research. 2011;52:813–825. doi: 10.1194/jlr.P013524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Millat G, Bailo N, Molinero S, Rodriguez C, Chikh K, Vanier MT. Niemann-Pick C disease: use of denaturing high performance liquid chromatography for the detection of NPC1 and NPC2 genetic variations and impact on management of patients and families. Molecular genetics and metabolism. 2005;86:220–232. doi: 10.1016/j.ymgme.2005.07.007. [DOI] [PubMed] [Google Scholar]
- 34.Huang L, Pike D, Sleat DE, Nanda V, Lobel P. Potential Pitfalls and Solutions for Use of Fluorescent Fusion Proteins to Study the Lysosome. PloS one. 2014;9 doi: 10.1371/journal.pone.0088893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Park WD, O'Brien JF, Lundquist PA, Kraft DL, Vockley CW, Karnes PS, Patterson MC, Snow K. Identification of 58 novel mutations in Niemann-Pick disease type C: correlation with biochemical phenotype and importance of PTC1-like domains in NPC1. Human mutation. 2003;22:313–325. doi: 10.1002/humu.10255. [DOI] [PubMed] [Google Scholar]
- 36.Meyre D, Delplanque J, Chevre JC, Lecoeur C, Lobbens S, Gallina S, Durand E, Vatin V, Degraeve F, Proenca C, et al. Genome-wide association study for early-onset and morbid adult obesity identifies three new risk loci in European populations. Nat Genet. 2009;41:157–159. doi: 10.1038/ng.301. [DOI] [PubMed] [Google Scholar]
- 37.Xu S, Benoff B, Liou HL, Lobel P, Stock AM. Structural basis of sterol binding by NPC2, a lysosomal protein deficient in Niemann-Pick type C2 disease. J Biol Chem. 2007;282:23525–23531. doi: 10.1074/jbc.M703848200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Landau M, Mayrose I, Rosenberg Y, Glaser F, Martz E, Pupko T, Ben-Tal N. ConSurf 2005: the projection of evolutionary conservation scores of residues on protein structures. Nucleic acids research. 2005;33:W299–W302. doi: 10.1093/nar/gki370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Glaser F, Rosenberg Y, Kessel A, Pupko T, Ben-Tal N. The ConSurf-HSSP database: The mapping of evolutionary conservation among homologs onto PDB structures. Proteins. 2005;58:610–617. doi: 10.1002/prot.20305. [DOI] [PubMed] [Google Scholar]
- 40.Kwon HJ, Abi-Mosleh L, Wang ML, Deisenhofer J, Goldstein JL, Brown MS, Infante RE. Structure of N-terminal domain of NPC1 reveals distinct subdomains for binding and transfer of cholesterol. Cell. 2009;137:1213–1224. doi: 10.1016/j.cell.2009.03.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure 1: Provides the molecular characterization of the c.441+1G>C NPC2 splice variant. A) Shows the products of the reverse transcription-PCR amplification of the region surrounded the exon 4/5 junction, visualized on a 1.8% agarose gel. The WT cell line presents a single 192 base band while both line heterozygous for the splice variant present with the control band and an alternately spliced prominent slightly larger band. B) Sequencing of the larger prominent alternative splice revealed the insertion of 16 nucleotides. C) Resulting sequence and frameshift as a result of the 16 base insertion.