Highlights
-
•
Rosai–Dorfman diseasе (RDD) is a rare histiocytic disorder оf unclear etiology.
-
•
RDD is characterized by emperipolesis and presence of S-100 positive histiocytes.
-
•
RDD usually presents as a massive, bilateral enlargement of the neck lymph nodes.
-
•
Localization of RDD in the liver and gallbladder is extremely rare.
-
•
Treatment is recommended in cases with symptomatic localized or extended RDD.
Abbreviations: RDD, Rosai–Dorfman disease; CT, computer tomography; H&E, hematoxylin and eosin
Keywords: Rosai–Dorfman disease, Extranodal disease, Liver, Gallbladder, Sinus histiocytosis
Abstract
Introduction
Rosai–Dorfman disease (RDD), also known as sinus histiocytosis with massive lymphadenopathy, is a rare histiocytic disorder of unclear etiology. Lymphadenopathy commonly affects the lymph nodes of the neck and the head, but extranodal involvement has been observed too.
Presentation of case
We describe an unusual case of RDD with involvement of the gallbladder, liver and cystic lymph node, clinically manifested as an exacerbated cholecystitis. The patient underwent a cholecystectomy with atypical liver resection because the finding was macroscopically suspected of gallbladder cancer. The diagnosis of RDD was confirmed by immunohistochemical study.
Discussion
Histological features of RDD include histiocytic proliferation, emperipolesis and positive immunostaining for S-100 protein and typically negative for CD1a. Gastrointestinal localization of RDD, especially in the liver and pancreas, is extremely rare. Typically, the liver is affected as a part of systematic spread of RDD. We have not found reports for involvement of the gallbladder.
Conclusion
The presented case is valuable due to its rarity and difficulty in differential diagnosis.
1. Introduction
Rosai–Dorfman disease (RDD), also known as sinus histiocytosis with massive lymphadenopathy, is a rare histiocytic disorder of unclear etiology [1,3,4]. It was described for the first time by Destombes in 1965 [1], but Rosai and Dorfman determined it as a distinct clinicopathological disorder in 1969 [2]. Histological features of RDD include histiocytic proliferation, emperipolesis and positive immunostaining for S-100 protein and typically negative for CD1a [2–4]. RDD usually presents as a painless, massive, bilateral enlargement of the neck lymph nodes, often combined with fever and leukocytosis [3]. Lymphadenopathy more frequently affects the lymph nodes of the neck and the head, but extranodal involvement has been observed too. The most common extranodal sites are the skin, upper respiratory tract and soft-tissue. Involvement of central nervous system, kidney, breast, thyroid gland and testis has been also reported [3,4]. Gastrointestinal localization of RDD, especially in the liver and pancreas, is extremely rare [3–6]. We have not found reports for involvement of the gallbladder. We describe a rare case of RDD presented with tumor mass involved the cystic lymph node, gallbladder and liver and clinically mimicking the exacerbated cholecystitis.
2. Presentation of case
A 58-year-old female patient presented with intermittent complaints including pain in right upper abdominal quadrant, nausea, vomiting and fever for approximately 3 years. The symptoms had started after consuming high-fat and spicy food. Previous ultrasound imaging revealed gallbladder stones. So the patient was admitted to our clinic for surgical treatment. The last symptomatic episode was 3 months before hospitalization. The physical examination demonstrated an afebrile patient with mild abdominal pain in the right hypohondrium and negative Murphy’s symptom. No lymphadenopathy was noted. Results from laboratory tests were in reference values, excluding the white blood cell count – 10,89 × 109 cells/L (reference 3,5–10,5 × 109 cells/L). The ultrasound investigation revealed liver steatosis and a folded gallbladder with thickened walls, blurred outlines and presence of small stones in the lumen (Fig. 1).
Fig. 1.
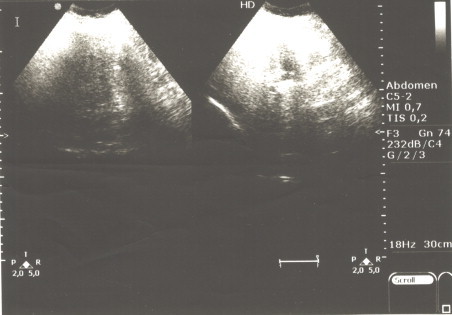
Preoperative ultrasound image of the liver/gallbladder of the patient.
On the basis of a presumptive clinical diagnosis of exacerbated cholecystitis with gallstones the patient underwent surgical treatment. The intraoperative exploration revealed severe adhesions surrounding the gallbladder, which was with almost intrahepatic location, thickened walls and palpable small stones inside it. The wall of the gallbladder in the infundibular part was extremely thickened and ocher colored. Because of the suspected gallbladder cancer we performed a cholecystectomy with atypical liver resection of IVth and Vth liver segments in macroscopically negative margins. The express histological examination rejected the malignant diagnosis. The permanent histological examination revealed Rosai–Dorfman disease with involvement of cystic lymph node, which lied in the angle formed by the cystic and common hepatic ducts (Mascagni’s lymph node), pericystic tissues, liver and gallbladder (Fig. 2). Immunohistochemical labeling of the histiocytes for S-100 protein was positive (Fig. 3) and negative for CD1a. The microscopic resection margins were negative.
Fig. 2.
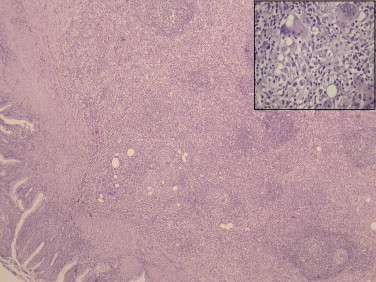
Tumor mass involving cystic lymph node and the gallbladder (H&E,10×) Inset (upper right H&E, 20×) – histiocytes with emperipolesis; H&E = hematoxylin and eosin.
Fig. 3.
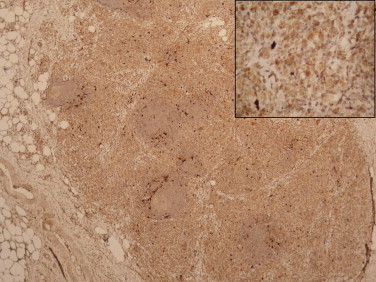
Lymph node; strong immunoreactivity of histiocytes for S-100 protein; inset (upper right, 10×).
Postoperative period was uneventful. Because of the histological findings we performed a full CT scan of the patient – there were no enlarged lymph nodes or lesions in other organs. One year after the operation the patient was in good health without clinical, ultrasound and CT imaging data for recurrent disease.
3. Discussion
Rosai–Dorfman disease is a rare disorder characterized by emperipolesis (lymphocytic penetration of and movement into the histiocyte), massive sinusoidal dilatation in affected lymph nodes containing histiocytes with an abundant pale eosinophilic cytoplasm, lymphocytes and plasma cells [2–4,7]. Immunohistochemically RDD histiocytes are positive for S100 and are typically negative for CD1a [3].
Etiology of the disease is still unclear and controversial. Some studies have demonstrated that pathogenesis of RDD is related to viral infections, such as human herpesvirus (HHV), parvovirus B19, and Epstein–Barr virus (EBV) [3,4,8]. However, other studies have not confirmed these results [3,9]. RDD has been reported in patients with immunoglobulin (Ig) G4-related disease, but there is no clear evidence that these disorders have a common etiopathogenesis [3,4,10].
Commonly, RDD occurs during the first or second decade of life, but any age group can be affected [8]. African Americans are more frequently affected [2,3,8]. Lymphadenopathy usually affects the lymph nodes of the neck and the head. Extranodal involvement by RDD was initially thought to be uncommon, but some recent reports suggest that it may be present in up to 40% of cases [3,11]. Gastrointestinal localization of RDD, especially in the liver and pancreas, is extremely rare [3–6]. Typically, the liver is affected as a part of systematic spread of RDD with nodal and wide extranodal involvement, like the 5 cases reported by Lauwers et al. [6,7]. Di Tommaso et al. presented a case of RDD exclusively involved the liver, but in several focuses and the disease was synchronous with non- Hodgkin lymphoma [6]. We have not found any reports for RDD with isolated affection of the gallbladder. Our case is unusual, because RDD was limited in cystic lymph node, the surrounding liver parenchyma and the gallbladder, and manifested by the clinical picture of exacerbated cholecystitis.
The differential diagnosis of RDD in this specific case is with other rare histiocytic diseases involving the liver and gallbladder cancer. Microscopically, there are no difficulties RDD and gallbladder cancer to be distinguished. In regards to Langerhans’ cell histiocytosis, it is a systematic disease with proliferation of positive to S100, CD1a and langherin histiocytes combined with an intense inflammatory infiltrate [4,6]. The phenomenon of emperipolesis is not observed [4,6]. Xanthogranulomatosis also can be mistaken with RDD because of the the accumulation of lipid-laden, foamy histiocytes, but they are S100 negative [4,6]. It should also be noted that focal RDD-like changes can sometimes be seen in lymph nodes involved by other processes, such as Hodgkin’s or non-Hodgkin’s lymphoma [15].
Treatment for the RDD is recommended only in patients who are symptomatic or have vital organ or systemic involvement [3]. Sometimes, in 20% of cases the disease is self-limited and shows spontaneous regression [3,12]. Complete surgical resection, like in our case, is the best option for treatment of the localized RDD [3]. In symptomatic cases of extensive RDD steroids are the first-line therapeutic option [3]. Radiotherapy can be used in cases with orbital, airway, and central nervous system involvement but till now no guidelines have been established for that management [3,13]. In cases of disseminated RDD or those refractory to surgery or other modalities, chemotherapy has been used with varying degrees of success [3,14].
4. Conclusion
We have presented a unique case of RDD presenting as a mass involving cystic lymph node, gallbladder and the surrounding liver parenchyma and clinically mimicking the exacerbated cholecystitis. This case is valuable due to its rarity and difficulty in differential diagnosis.
Conflicts of interest
The authors declare that they have no conflicts of interest to disclose.
Funding
None.
Ethical approval
The patient’s approval has been given for this case report.
Consent
An informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this Journal on request”.
Author contribution
Elena Arabadzhieva wrote the paper. Dimitar Bulanov collected the literature for the review in the report. Sasho Bonev analysed the review. Atanas Yonkov and Ivanka Taneva performed the operation of the patient described in this report. Tatyana Pirdopska performed the histological examination. Ivan Terziev carried out the immunohistochemical study and confirmed the diagnosis. Violeta Dimitrova revised the manuscript for important intellectual content and technical details. All authors have read and approved the final manuscript.
Research registry
UIN: researchregistry190.
Guarantor
Violeta Dimitrova, MD, PhD, DMSc and Atanas Yonkov, MD, PhD would be the guarantors.
References
- 1.Destombes P. Adenitis with lipid excess, in children or young adults, seen in the Antilles and in Mali. (4 cases) Fre. Bull. Soc. Pathol. Exot. Filiales. 1965;58(6):1169–1175. [PubMed] [Google Scholar]
- 2.Rosai J., Dorfman R.F. Sinus histiocytosis with massive lymphadenopathy. A newly recognized benign clinicopathological entity. Arch. Pathol. 1969;87(1):63–70. [PubMed] [Google Scholar]
- 3.Dalia S., Sagatys E., Sokol L., Kubal T. Rosai–Dorfman disease: tumor biology, clinical features, pathology, and treatment. Cancer Control. 2014;21(4):322–327. doi: 10.1177/107327481402100408. [DOI] [PubMed] [Google Scholar]
- 4.Zhao M., Li C., Zheng J. Extranodal Rosai–Dorfman disease involving appendix and mesenteric nodes with a protracted course: report of a rare case lacking relationship to IgG4-related disease and review of the literature. Int. J. Clin. Exp. Pathol. 2013;6(11):2569–2577. [PMC free article] [PubMed] [Google Scholar]
- 5.Romero Arenas M.A., Singhi A.D., Hruban R.H., Cameron A.M. Rosai–Dorfman disease (sinus histiocytosis with massive lymphadenopathy) of the pancreas: third reported occurrence. J. Gastrointest. Cancer. 2012;43:626–629. doi: 10.1007/s12029-012-9424-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Di Tommaso L., Rahal D., Bossi P., Roncalli M. Hepatic Rosai–Dorfman disease with coincidental lymphoma: report of a case. Int. J. Surg. Pathol. 2010;18(6):540–543. doi: 10.1177/1066896908329590. [DOI] [PubMed] [Google Scholar]
- 7.Lauwers G., Perez-Atayde A., Dorfman R., Rosai J. The digestive system manifestations of Rosai–Dorfman disease (sinus histiocytosis with massive lymphadenopathy): review of 11 cases. Hum. Pathol. 2000;31:380–385. doi: 10.1016/s0046-8177(00)80254-3. [DOI] [PubMed] [Google Scholar]
- 8.Foucar E., Rosai J., Dorfman R. Sinus histiocytosis with massive lymphadenopathy (Rosai–Dorfman disease): review of the entity. Semin. Diagn. Pathol. 1990;7(1):19–73. [PubMed] [Google Scholar]
- 9.Ortonne N., Fillet A.M., Kosuge H. Cutaneous destombes-Rosai–Dorfman disease: absence of detection of hhv-6 and hhv-8 in skin. J Cutan Pathol. 2002;29(2):113–118. doi: 10.1034/j.1600-0560.2002.290209.x. [DOI] [PubMed] [Google Scholar]
- 10.Liu L., Perry A.M., Cao W. Relationship between Rosai–Dorfman disease and IgG4-related disease: study of 32 cases. Am. J. Clin. Pathol. 2013;140(3):395–402. doi: 10.1309/AJCPFH0SJ6YILXJU. [DOI] [PubMed] [Google Scholar]
- 11.Frater J.L., Maddox J.S., Obadiah J.M. Cutaneous Rosai–Dorfman disease: comprehensive review of cases reported in the medical literature since 1990 and presentation of an illustrative case. J. Cutan. Med. Surg. 2006;10(6):281–290. doi: 10.2310/7750.2006.00067. [DOI] [PubMed] [Google Scholar]
- 12.Lima F.B., Barcelos P.S., Constâncio A.P. Rosai–Dorfman disease with spontaneous resolution: case report of a child. Rev. Bras. Hematol. Hemoter. 2011;33(4):312–314. doi: 10.5581/1516-8484.20110083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Toguri D., Louie A.V., Rizkalla K. Radiotherapy for steroid-resistant laryngeal Rosai–Dorfman disease. Current Oncol. 2011;18(3):158–162. doi: 10.3747/co.v18i3.761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Horneff G., Jürgens H., Hort W. Sinus histiocytosis with massive lymphadenopathy (Rosai–Dorfman disease): response to methotrexate and mercaptopurine. Med. Pediatr. Oncol. 1996;27(3):187–192. doi: 10.1002/(SICI)1096-911X(199609)27:3<187::AID-MPO10>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 15.Falk S., Stutte H.J., Frizzera G. Hodgkin’s disease and sinus histiocytosis with massive lymphadenopathy like changes. Histopathology. 1991;19:221–224. doi: 10.1111/j.1365-2559.1991.tb00025.x. [DOI] [PubMed] [Google Scholar]


