Abstract
PURPOSE
The purpose of this study was to find out the effect of immediate dentin sealing (IDS) on bond strength of ceramic restoration under various thermocycling periods with DBA (dentin bonding agent system).
MATERIALS AND METHODS
Fifty freshly extracted human mandibular third molars were divided into 5 groups (1 control and 4 experimental groups) of 10 teeth. We removed enamel layer of sound teeth and embedded them which will proceed to be IDS, using All Bond II. A thermocycling was applied to experimental groups for 1, 2, 7, 14 days respectively and was not applied to control group. IPS Empress II for ceramic was acid-etched with ceramic etchant (9.5% HF) and silane was applied. Each ceramic disc was bonded to specimens with Duo-link, dual curable resin cement by means of light curing for 100 seconds. After the cementation procedures, shear bond strength measurement and SEM analysis of the fractured surface were done. The data were analyzed with a one-way ANOVA and Tukey multiple comparison test (α=.05).
RESULTS
There were no statistically significant differences between 4 experimental groups and control group, however the mean value started to decrease in group 7d, and group 14d showed the lowest mean bond strength in all groups. Also, group 7d and 14d showed distinct exposed dentin and collapsed hybrid layer was observed in SEM analysis.
CONCLUSION
In the present study, it can be concluded that ceramic restorations like a laminate veneer restoration should be bonded using resin cement within one week after IDS procedure.
Keywords: Immediate dentin sealing, SEM analysis, Dentin bonding, Thermocycling, Ceramic restoration
INTRODUCTION
Patient expect for improved esthetics has driven the advancement of ceramic for use with fixed partial prostheses.1 Many clinical studies demonstrate excellent long-term success of ceramic restorations. In recent year, strong ceramic cores unioning esthetic veneering porcelains have become popular as all ceramic restorations which have compensated the brittleness of porcelain and unesthetic metal substructure. The clinical success of all ceramic prosthesis depends on a number of factors, such as composition of the ceramic material and the cementation procedure.2 Hence, bonding to ceramic requires strict attention to detail for optimal clinical outcomes.3
A vital importance is due to the adhesive strength and durability of the complex formed between the three different components: the resin cement, the ceramic surface and the tooth surface especially in anterior laminate veneers.4,5 In some cases, significant amounts of exposed dentin is usually unavoidable during the preparation of anterior teeth,1,6 the protection is required during the period between preparation and cementation for prevention of post-operative sensitivity and bacterial invasion.2 They suggested the application of the dentin bonding agent immediately after tooth preparation. This new technique of dentin bonding agent application prevents the bacterial invasion and dentin sensitivity during the provisional states, and the technique is concerned with increased bond strength in vitro.7 Magne (2005) also recommended application of dentin adhesive to the freshly cut dentin when a significant area of dentin has been exposed during preparation for indirect restoration. The dentin could be sealed immediately after tooth preparation with IDS prior to impression taking.3
IDS is the application of dentin bonding agent to freshly cut dentin when it is exposed during tooth preparation for indirect restorations. IDS protects the dentin against bacterial leakage and tooth sensitivity before cementation of final prosthesis. An advanced protocol, IDS is devised to address the challenges of preparation, provisionalization, and the final cementation of indirect restorative procedures. The general protocol of IDS includes the use of filled three-step total etch systems, two-step total-etch systems, and two-step self-etch systems incorporating low elastic liners.8
Especially prosthodontic patients, complex inlay, onlay and veneer situations may require longer periods with provisional restoration until the final ceramic restoration is delivered.9 The provisional restoration must protect the pulp from thermal changes as well as from invasive microorganisms in the mouth. However, it is difficult to takestable and sealed provisionals as they detached easily during temporary states, allowing microleakage of bacteria and sensitivity.10 In addition, the bond strength between resin composite and a pre-treated ceramic restoration has been described to be negatively affected by external factors such as thermocycling, fatigue and water sorption.11 Also, cement breakdown can bring about results as microleakage, marginal discoloration, debonding, secondary caries, pulpal irritation, and decreased fracture load.12
We pose the clinical assumption that the dentin surface after IDS procedure is exposed to the oral environment and factors that could result in fatigue may influence the physical and mechanical properties of dentin bond strength. There are no studies available concerning the dentin bond strength on exposed sealed dentin with a long delay under thermocycling.
The aim of this study was to evaluate the effect of IDS on dentin bond strength of lithium disilicate ceramic (IPS Empress II, Ivoclar) under various thermocycling periods of 1, 2, 7, 14 days.
MATERIALS AND METHODS
For tooth preparation, freshly extracted sound human mandibular third molars stored in solution saturated with thymol were used. The midcoronal dentin surfaces were created after the removal of the occlusal half of the crown using a low-speed diamond saw (Isomet: Buehler Ltd., Lake Bluff, IL, USA). Each specimen was individually secured to a silicon mold (diameter: 25 mm, height: 15 mm) and self-curing polyester resin (CH-304, Aekyung Chemical Co., Ltd., Seoul, Korea) was poured to create a resin-embedded specimen block. The surface was wet polished to create hybrid layer with 320, 400 and 600 grit SiC abrasive papers. Total 50 specimens were prepared. The experimental groups were divided into four groups (10 specimens per group) according to the thermocycling period (1, 4, 7, 14 days). The control group consisted of 10 specimens without thermocycling.
A total of 50 ceramic discs (diameter: 4 mm, height: 2 mm) of lithium disilicate ceramic (IPS Empress II ingot, shade A1, Ivoclar Vivadent AG, Schaan, Liechtenstein) were fabricated. The surfaces were etched with 9.5% hydrofluoric acid (HF) (Porcelain etchant, Bisco Inc., Schaumburg, IL, USA) for 90 seconds and one layer of silane coupling agent (Porcelain primer, Bisco Inc., Schaumburg, IL, USA) was applied and allowed to air dry for thirty seconds at room temperature. The surface treatments of the ceramic discs were according to the manufacturer's instruction. The materials used in this study are shown in Table 1.
Table 1. Materials used in this study.
| Materials | Product name | Composition | Manufacturer |
|---|---|---|---|
| DBA system | All Bond II | 4th Generation: 3-step total etching system | Bisco Inc., Shaumburg, USA |
| Resin cement | Duo-link | Dual cure resin cement | Bisco Inc., Shaumburg, USA |
| Etchant | UNI-ETCH | 32% Phosphoric acid (15 sec) | Bisco Inc., Shaumburg, USA |
| Ceramic disc | IPS Empress II | Lithium disilicate glass-ceramic | Ivoclar Vivadent AG, Schaan, Liechtenstein |
| Ceramic etchant | Porcelain etchant | 9.5% Hydrofluoric acid (90 sec) | Bisco Inc., Shaumburg, USA |
| Silane | Porcelain primer | Coupling agent (30 sec) | Bisco Inc., Shaumburg, USA |
*DBA: Dentin Bonding Agent
For immediate dentin sealing procedure, the dentin surface was etched with 32% phosphoric acid (H3PO4) for 15 seconds, followed by rinsing with distilled water and air drying for 5 seconds. Then, five coat of dentin bonding primer (3-step etch-rinse adhesive system; All Bond II, Bisco Inc., Shaumburg, IL, USA) with a light brushing motion for 30 seconds was applied to the surface and air thinning for 3 seconds. After one coat of Pre-bond resin, the layer was light polymerized (VIP Junior light curing unit, Bisco Inc., Schaumburg, IL, USA) for 20 seconds at 600mW/cm2. Ceramic disc was attached with dual-cured resin cement (Duo-link, Bisco Inc., Shaumburg, IL, USA) on IDS treated dentin surface.
After then, the specimens of experimental groups were submitted to 1500 thermal cycles between 5℃ and 55℃ (dwell time of 30 seconds) in a thermal cycling machine (Thermocycling testing machine, CDM-127, CDM, Korea) for 1, 2, 7, 14 day (group 1d, 2d, 7d, 14d) (Table 2).13,14 Control group (0d) was not thermocycled and the specimens were stored for 14 days in deionized water at room temperature.
Table 2. Experimental design and groups used in this study (d; day).
| Thermocycling time | Group |
|---|---|
| 0 day (immediate) | 0d (control) |
| 1 day | 1d |
| 2 days | 2d |
| 7 days | 7d |
| 14 days | 14d |
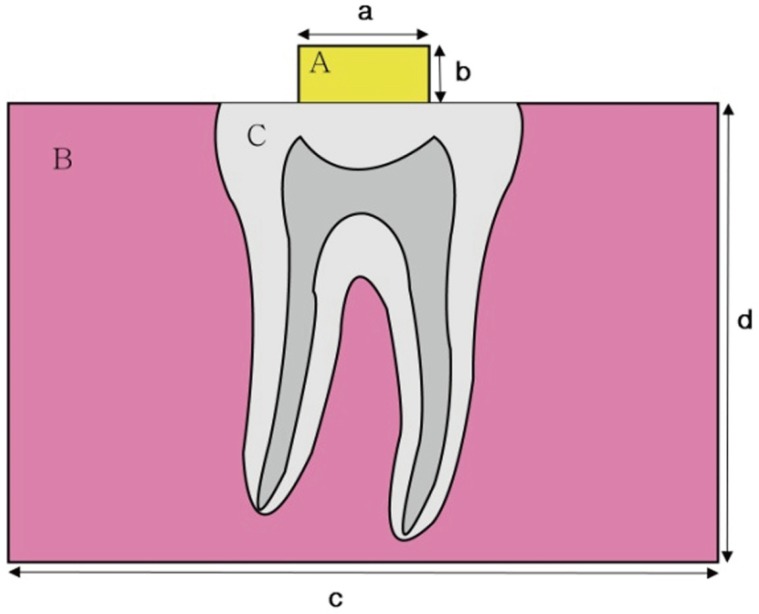
Ceramic discs after surface treatment with ceramic etchant and silane coupling agent were cemented to the surfaces of specimens with or without thermocycling with dual-cured resin cement (Duo-link, Bisco Inc., Shaumburg, IL, USA) (Fig. 1). The excess cement was removed with a disposable microbrush, followed by light curing (VIP Junior light curing unit, Bisco Inc., Schaumburg, IL, USA) with a light intensity of 600 mW/cm2. The light was applied for 100 seconds (20 seconds each from occusal, buccal, lingual, mesial and distal aspects).
Fig. 1. A diagram of specimen (A: porcelain disc, B: polyester resin, C: lower molar with exposed dentin, a: diameter; 4 mm, b: height; 2 mm, c: diameter; 25 mm, d: height; 15 mm).
The extrusion shear bond strength test (SBST)15,16 represents a confinement situation for the composite, and the resulting interface would be more likely to present defects that resemble clinical conditions. After the cementation procedures, the specimens of control group and thermocycled groups were stored in distilled water for 24 hours at 37℃. The SBST was conducted in a universal testing machine (Instron, Shimadzu, Japan) at a crosshead speed of 1.0 mm/min.
For the scanning electron microscopy (SEM) analysis, the dentin surfaces of specimens from each group were air dried and gold coated with a sputter coater (IB-3 ION coater, Elko Co., Tokyo, Japan) and examined under scanning electron microscope (Scanning Electron Microscopy, S-2300, Hitachi, Co., Ltd., Tokyo, Japan). The specimens were vertically sectioned using a low-speed diamond saw under water lubrication to observe the interface of dentinresin-ceramic.
Bond strength values were analyzed using one-way analysis of variance and followed by Tukey's HSD multiple comparison tests. Statistical analysis was conducted using SAS software version 9.1 for windows (SAS Institute Inc., Cary, NC, USA). The significance level for all statistical tests was set at 0.05.
RESULTS
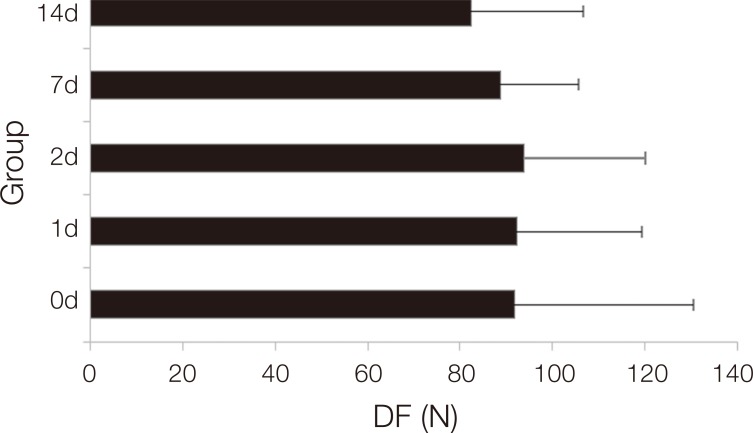
The values of the shear bond strength recorded in debonding force (DF) for the specimens in all groups. The mean values and standard deviation of shear bond strength are shown in Fig. 2. Two thermocycled groups had lower mean values than the control group. The analysis of variance indicated no statistically significant difference in shear bond strength between all groups, however the mean value started to decrease in group 7d, and group 14d showed the lowest mean bond strength in all groups.
Fig. 2. Mean value and Standard deviation of shear bond strength (unit; N). The 1 way ANOVA showed no statistical difference was found among groups, but 14d group showed significantly lower mean bond strength than the control (d; day, DF; DebondingForce).
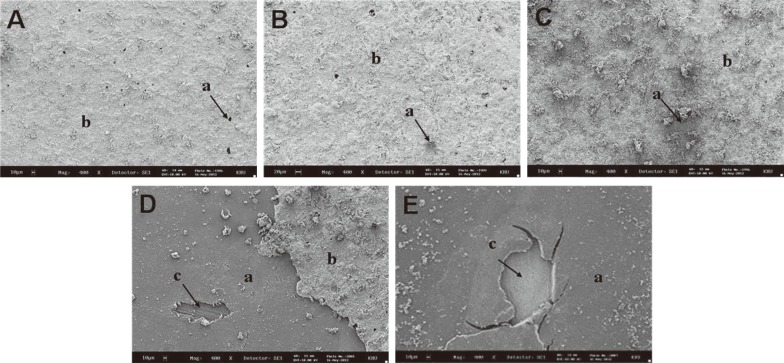
SEM micrograph of fractured surface of dentin side after SBST (original magnification ×100) are shown in Fig. 3. SEM analysis of fractured surface in the control group, thermocycled 1d and 2d groups demonstrated mostly undamaged interface of overlaying resin cement on IDS surface (Fig. 3A, Fig. 3B, Fig. 3C). It confirmed that dentin was completely covered with dentin bonding and adhesive resin cement, suggesting failure was not occurred between IDS surface and resin cement. At the group 7d (Fig. 3D), two distinct areas were observed, there were exposed IDS surface and resin cement. Areas with detached resin cement has increased and founded widely. As shown in the Fig. 3E, most of resin cement has been detached from IDS surface.
Fig. 3. SEM micrograph of fractured surface after SBST (original magnification ×100). (a; detached surface of resin cement, b; resin cement) (A) Group 0d, typical SEM micrograph of fractured surface after SBST from control group. (B) Group 1d, mostly unharmed interface of overlaying resin cement is on dentin surface. (C) Group 2d, most of exposed dentin is covered with resin cement (b), while detached surface of resin cement (a) is found in a small portion. (D) Group 7d, dentin surface has increased due to larger detached surface of resin cement (a). (E) Group 14d, Most of resin cement has detached from dentin surface.
A representative SEM images of fractured surface of dentin side after SBST (original magnification ×400) are shown in Fig. 4, and showed similar pattern to SEM views for original magnification ×100 (Fig. 3). The specimens of groups 0d, 1d and 2d showed very small portion of detached resin cement and there were undamaged interface of overlaying resin cement on IDS surface (Fig. 4A, Fig. 4B, Fig. 4C). While in group 7d (Fig. 4D), showed a mixed failure surface, areas with remained resin cement and exposed IDS surface were found at the same time. In group 14d (Fig. 4E), extensive area of IDS surface was found. Most of resin cement has been detached from IDS surface, suggesting failure between existing resin cement and IDS surface. Especially, group 7d and 14d (Fig. 4D, Fig. 4E), showed distinct exposed dentin, which suggests adhesion failure between dentin and adhesive.
Fig. 4. SEM micrograph of fractured surface after SBST (original magnification ×400). Closer examination shows similar pattern to SEM views for original magnification ×100. (a; detached surface of resin cement, adhesive, b; resin cement, c; exposed dentin) (A) Group 0d, typical SEM micrograph of fractured surface after SBST from control group. (B) Group 1d, small portion of detached resin cement and unharmed interface of overlaying resin cement is on dentin surface. (C) Group 2d, most of exposed dentin is covered with resin cement (b), while detached surface of resin cement (a) is found in a small portion. (D) Group 7d, larger detached surface of resin cement (a) reveals adhesive. (E) Group 14d, most of resin cement has detached from dentin surface coated by adhesive (a). Exposed dentin (c), which suggests failure in dentin, is clearly detectable in groups 7d and 14d.
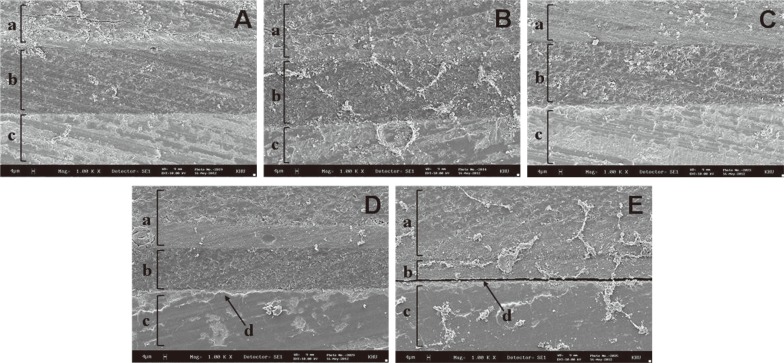
In Fig. 5, adhesive-resin cement (b) was found between ceramic disc (a) and dentin covered with adhesive (c). The specimens of groups 0d, 1d and 2d, uniform and thin adhesive-resin cement layers were observed (Fig. 5A, Fig. 5B, Fig. 5C). An almost imperceptible transition seemed to take place at the ceramic disc-resin cement-dentin interface, where no gap was observed despite of some stresses generated by thermocycling. In group 7d (Fig. 5D), as compared with above three groups, thickening and peeling of adhesive-resin cement layer (b) was found. In group 14d (Fig. 5E), partially visible discontinuity of interface and linear detachment between IDS surface and resin cement was observed.
Fig. 5. SEM micrograph of cross section of bonded porcelain disc to the specimen (original magnification, ×100). (a; porcelain disc, b; adhesive-resin cement layer, c; dentin covered with adhesive) (A) Group 0d, (B) Group 1d, (C) Group 2d. A uniform and thin adhesive-resin cement layer (b) is observed (A-C). (D) Group 7d, as compared with other groups, thickening and peeling of adhesive-resin cement layer (b) is found. (E) Group 14d, linear discontinuity between adhesive-resin cement layer and dentin was observed.
In Fig. 6, adhesive-resin cement (b) was found between porcelain disc (a) and dentin covered with adhesive (c). Higher magnification examination shows similar pattern to SEM views for original magnification ×100. Between group 0d (control group) and thermocycled group 1d and 2d, no differences were found between adhesive-resin cement layers (b) with regard to form and thickness (Fig. 6A, Fig. 6B, Fig. 6C). Adhesive interface remained intact and complete continuity was observed. In group 7d (Fig. 6D), perceptible changes appeared in adhesion interface, in group 14d (Fig. 6E), obvious gap between adhesive-resin cement layer (b) and dentin (c) was found. It showed adhesive failure between the IDS surface and resin cement.
Fig. 6. SEM micrograph of cross section of bonded porcelain disc to the specimen (original magnification ×1000). Closer examination shows similar pattern to SEM views for original magnification ×100. (a; porcelain disc, b; adhesiveresin cement layer, c; exposed dentin, d; gap) (A) Group 0d, (B) Group 1d, (C) Group 2d, there are no differences between adhesive-resin cement layers (b) of these groups in terms of form and thickness (A-C) (D) Group 7d, perceptible changes appeared in IDS surface, (E) Group 14d, gap (d) is clearly detectable between adhesive-resin cement layer (b) and dentin (c).
DISCUSSION
Over the past twenty years, the field of esthetic prosthodontics has substantially expanded to satisfy the needs of the patients.8 Bonded ceramic restorations are a predictable and durable treatment option to re-establish the strength and function of the teeth as well as esthetic.3 Especially, the success of the ceramic veneer is highly dependent on the strength and durability of the bond formed between the three different components of the bonded veneer complex, as there are; the tooth surface, the luting composite and the ceramic veneer.9 There have been no studies regarding the dentin bond strength and SEM analysis of immediate sealed dentin that is exposed with an extended delay under thermocycling.
Phosphoric acid etching causes dissolution of interprismatic material in the enamel, producing a roughened enamel surface, and forms enamel resin tags. In recent years, the research of increasing the bond strength between the dental materials and dental hard tissues have been proceeded, although most adhesive systems have provided clinically acceptable bond strengths.11 Mechanical adhesion requires roughening to create sufficient surface activation. Common surface treatment methods include sandblasting with alumina, grinding, and abrasion with diamond instrument,10,12 and acid etchingwith HF solution or ammonium bifluoride.17,18
The sequential application of silane coupling agents to previously HF-etched ceramic surface provides a chemical bonding. Chemical bonding of silane is shown to be in correlation with increased durability of long-term bond potential and less with immediate mechanical bond strengths.19,20 The preferred procedure for predictable bonding to silicabased ceramics is acid etching with HF and the subsequent application of silane coupling agents. With the improvement of esthetic restoration material, newly developed resin cement which can provide both mechanical and chemical bonding has been introduced.13,21,22,23 Application of a silane coupling agent to HF-etched ceramic surfaces provides a strong chemical covalent bond between the hydroxyl group of silane coupling agent and that of the silica of ceramic. When the silane primer is applied onto the porcelain surface, two hydroxyl groups (one from and silane and one from the porcelain) will react slowly while liberating a water molecule to form a stable siloxane. The most commonly used medium and high leucite-containing feldspathic porcelains is etched with HF and makes preferential etching of the glass phase of ceramic, leaving the less soluble crystalline phase of leucite composition. This forms micromechanically retentive surfaces on porcelain. The preferential etching provides many hydroxyl (OH) groups that can be coupled with silane coupling agent for improved chemical bonding with resin materials.24
When preparing teeth for indirect bonded restorations, IDS with a 3-step etch-and-rinse DBA, before impression taking, leads to increased microtensile bond strength compared to delayed dentin sealing (DDS). The failure site was observed with microscope (×30) and failure mode of cementation was determined. If the failure was occurred entirely between the adhesive and dentin or continued from the adhesive into either the composite resin or dentine, it was classified as an interfacial failure. And if the failure occurred exclusively within the resin composite or dentin, it was classified as a substrate failure. IDS groups showed interfacial failure that was generally two areas as typically mixed, with both areas of failed adhesive resin and areas of cohesively failed dentin. For DDS specimens, it was hard to decide the exact nature of interfacial failure as the similar nature of the filled adhesive and hybrid layer.1 Magne (2005) demonstrated that several reasonable motives supporting IDS. First, immediately exposed dentin after preparation has an ideal surface for dentin bonding.1 Confoun-ding results have been reported when the shear bond strength of dentin bonding agents was measured on dentin that had been contaminated with provisional cements prior to the bonding procedure.2 Freshly cut dentin exists only immediately after tooth preparation. Secondly, Precuring of the DBA results in increased bond strength. In recent studies on bond strength of DBA, the infiltrating resin and adhesive layer are generally polymerized first (precuring), before composite resin is incremented, which represents to generate increased bond strength. If exposed dentin is sealed without delay, the DBA being covered and cured immediately after the finish of tooth preparations, before the final impression, generated higher bond strength25,26,27 and fewer gap formations.28,29
IDS allows stress-free dentin bond development. When indirect bonded restorations proceeded with IDS, because of postponed placement of the restoration (intrinsic to indirect techniques), the dentin bonding strengths can be improved without stress, resulting in considerably developed restoration adaptation.30 In addition, IDS reduced bacterial infiltration and sensitivity to dentin during provisional restoration. Based on the fact that provisional restorations enable bacterial leakage and dentin sensitivity, previous researcher suggested dentin sealing in crown preparations.31 This suggestion demonstrates even more advantages when using bonded ceramic restoration (e.g., veneers) given the specific difficulty to obtain sealed and stable provisionals. An important element in IDS is the advancement of an efficient resin-to resin bond between the new luting composite resin and the adhesive resin coating. This condition is somewhat similar to a composite resin-composite resin repair.5
For years, many believed that an oxygen-inhibited layer is essential prior to bonding additional layers of composite. The general understanding regarding the oxygen-inhibited layer has been documented. Suh32 reported that an oxygen-inhibited layer is not necessary for bonding with composite resin and Papachini33 identified that oxygen inhibition layer is not crucial to the success of composite-composite bond. A previously placed resin matrix is naturally cohesive with monomers in freshly placed composite resin.32,33 Magne et al.,5 reported that the bond strength of IDS teeth was not affected by up to 12 weeks of elapsed time prior to placement of the definitive restoration.
In this present study, there was no statistically significant difference in shear bond strength between all groups. As demonstrated by the shear strength bond results, the mean shear bond strength varied from 82.7 to 93.93 N. The mean value started to decrease at day 7 and markedly decreased at day 14. In most of the studies regarding IDS, teeth were restored with provisional restoration material and left in place for a certain period of time. However, in this study, we hypothesized that all-ceramic restoration such as laminate veneer crown is likely to be contaminated with a wide variety of things including temporary cement residues, saliva and bacteria. We attempt to mimic extreme clinical conditions when the provisional restoration is fractured or dislodged before the delivery of the final restoration. In our study, after immediate dentin sealing, teeth were immersed in saline solution without provisional restoration. Thus, the result of shear bond strength in this study shows difference from that of previous studies.
In conventional glass-ceramic restorations for prosthesis, the adhesive technique is crucial for successful bonding. Considering limited flexural strength and the brittleness of glass ceramics, final adhesive cementation with luting composite resin should be used to improve the fracture resistance. In this present study, IPS Empress II was tested which is widely used as a ceramic material of laminate veneer crown. IPS Empress II (Ivoclar Vivadent, Schaan, Liechtenstein) is a lithium-disilicate glass ceramic (SiO2-Li2O) manufactured through a combination of the lost-wax and heat-compression techniques. A glass-ceramic ingot is plasticized at 920℃ and pressed into an investment mold under pressure and vacuum. Its predecessor, IPS Empress (Ivoclar Vivadent), is a leucite-reinforced glass ceramic (SiO2-Al2O3-K2O) and is restricted in use of single unit complete-coverage crown restoration due to its limited strength. IPS Empress 2 has increased flexural strength by a factor of 3 over IPS Empress, and enables the use of 3-unit FPDPs in the anterior area, and the second premolar area.34,35,36
One way of evaluating the physical and mechanical properties of the material is to subject them to an in vitro simulation of the aging that would occur in the medium in which they are used, by means of anaccelerated aging test by thermocycling. Chang et al.37 reported that bond strength of various adhesive systems is influenced by thermocycling. The adverse effect of thermal cycling on the adhesive combination can be explained by the fact that materials with different lineal thermal expansion coefficients (LTEC) also presented different degrees of shrinkage and expansion. That process facilitates the fatigue phenomenon of the materials, leading to rupture of the union between them.38 Mechanical fatigue alone could not deteriorate the interface between the cements and the ceramic materials as much as it could for the humid condition with the presence of stress corrosion.39 Sobrinho et al. proved a reduction in strength after fatigue in a wet environment for In-Ceram and IPS Empress ceramic in comparison to the dry condition.40 Considering that final restoration is delivered one or two weeks after the tooth preparation, the specimens were submitted to thermocycling until 14 days. At the groups 1d, 2d, 7d and 14d, the specimens were thermocycled 1,500 cycles (1 day), 3,000 cycles (2 days), 10,500 cycles (7 days), 21,000 cycles (14 days) in baths at 5C and 55C, with 30-second dwell times. The results of the present study demonstrated that thermal cycling negatively influenced the quality of adhesive resistance, promoting the decrease in union values when the number of thermal cycles was increased.14,38,41,42,43,44 Qualtrough et al. reported that there was a deterioration in marginal quality at the porcelain inlay/composite resin interface as a result of thermocycling.45
In the present study, cross-sectional SEM analysis of dentin surface in magnification of ×100 and ×1000 demonstrated that the thermocycled group until 2 days did not show a difference from the control group with regard to shape and morphology: uniform and thin layer of adhesive-resin cement layer was observed. In thermocycled group 7d, thickening and peeling of adhesive-resin cement layer was appeared, and in thermocycled group 14d, distinctive failure on IDS surface were observed. SEM analysis of dentin surface showed dentin is almost completely covered with adhesive-resin cement layer in thermocycled groups 1d and 2d, and small fragment of detached resin was observed. In thermocycled group 7d, largely detached resin and extensive area of dentin were observed, and in thermocycled group 14d, most of the adhesive resin was detached.
The limitation of this study is that quantitative assessment of the size of the ceramic discs was not performed. In this study, a large standard deviation of shear bond strength indicates that there exists a delicate difference in adhesive areas of porcelain discs due to little difference in the size of porcelain discs. Further studies should be conducted to evaluate shear bond strength per unit area.
CONCLUSION
In conclusion, among the specimens of thermocylced groups (1 day, 2 days, 7 days, 14 days) after IDS procedure, the bond strength started to decrease in the thermocycled 7 days group and noticeably decreased in the thermocycled 14 days group. The SEM micrographs on dentin surface of adhesively failed specimens revealed that the thermocycled 7 days group showed a mixed failure surface areas with remained resin cement and exposed IDS surface, and also the largest area of detached resin cement and exposed dentin were identified in the thermocycled 14 days group. The SEM micrographs of cross-section demonstrated partial detachment and thickening of resin cement layer in thermocycled 7 days group, and distinct linear gap between resin cement layer and the dentin in the thermocycled 14 days group. Therefore, the bond of definitive ceramic restorations such as inlay/onlay and laminate veneer should be bonded within one week after IDS procedure.
Footnotes
This work was supported by the Basic Science Research Program of the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT & Future Planning (NRF-2013R1A1A1061129).
References
- 1.Magne P. Immediate dentin sealing: a fundamental procedure for indirect bonded restorations. J Esthet Restor Dent. 2005;17:144–154. doi: 10.1111/j.1708-8240.2005.tb00103.x. [DOI] [PubMed] [Google Scholar]
- 2.Paul SJ, Scharer P. The dual bonding technique: a modified method to improve adhesive luting procedures. Int J Periodontics Restorative Dent. 1997;17:536–545. [PubMed] [Google Scholar]
- 3.Park DJ, Yang JH, Lee JB, Kim SH, Han JS. Esthetic improvement in the patient with one missing maxillary central incisor restored with porcelain laminate veneers. J Adv Prosthodont. 2010;2:77–80. doi: 10.4047/jap.2010.2.3.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xie J, Powers JM, McGuckin RS. In vitro bond strength of two adhesives to enamel and dentin under normal and contaminated conditions. Dent Mater. 1993;9:295–299. doi: 10.1016/0109-5641(93)90046-s. [DOI] [PubMed] [Google Scholar]
- 5.Magne P, So WS, Cascione D. Immediate dentin sealing supports delayed restoration placement. J Prosthet Dent. 2007;98:166–174. doi: 10.1016/S0022-3913(07)60052-3. [DOI] [PubMed] [Google Scholar]
- 6.Christensen GJ. Resin cements and postoperative sensitivity. J Am Dent Assoc. 2000;131:1197–1199. doi: 10.14219/jada.archive.2000.0357. [DOI] [PubMed] [Google Scholar]
- 7.Gresnigt M, Ozcan M, Kalk W. Esthetic rehabilitation of worn anterior teeth with thin porcelain laminate veneers. Eur J Esthet Dent. 2011;6:298–313. [PubMed] [Google Scholar]
- 8.Moon JE, Kim SH, Han JS, Yang JH, Lee JB. Esthetic restorations of maxillary anterior teeth with orthodontic treatment and porcelain laminate veneers: a case report. J Adv Prosthodont. 2010;2:61–63. doi: 10.4047/jap.2010.2.2.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Usumez A, Ozturk AN, Usumez S, Ozturk B. The efficiency of different light sources to polymerize resin cement beneath porcelain laminate veneers. J Oral Rehabil. 2004;31:160–165. doi: 10.1046/j.0305-182x.2003.01219.x. [DOI] [PubMed] [Google Scholar]
- 10.Nagayassu MP, Shintome LK, Uemura ES, Araujo JE. Effect of surface treatment on the shear bond strength of a resinbased cement to porcelain. Braz Dent J. 2006;17:290–295. doi: 10.1590/s0103-64402006000400005. [DOI] [PubMed] [Google Scholar]
- 11.Rosenbach G, Cal-Neto JP, Oliveira SR, Chevitarese O, Almeida MA. Effect of enamel etching on tensile bond strength of brackets bonded in vivo with a resin-reinforced glass ionomer cement. Angle Orthod. 2007;77:113–116. doi: 10.2319/111705-402R.1. [DOI] [PubMed] [Google Scholar]
- 12.Correia SL, Dienstmann G, Folgueras MV, Segadaes AM. Effect of quartz sand replacement by agate rejects in triaxial porcelain. J Hazard Mater. 2009;163:315–322. doi: 10.1016/j.jhazmat.2008.06.094. [DOI] [PubMed] [Google Scholar]
- 13.Ibarra G, Johnson GH, Geurtsen W, Vargas MA. Microleakage of porcelain veneer restorations bonded to enamel and dentin with a new self-adhesive resin-based dental cement. Dent Mater. 2007;23:218–225. doi: 10.1016/j.dental.2006.01.013. [DOI] [PubMed] [Google Scholar]
- 14.Guarda GB, Correr AB, Goncalves LS, Costa AR, Borges GA, Sinhoreti MA, Correr-Sobrinho L. Effects of surface treatments, thermocycling, and cyclic loading on the bond strength of a resin cement bonded to a lithium disilicate glass ceramic. Oper Dent. 2013;38:208–217. doi: 10.2341/11-076-L. [DOI] [PubMed] [Google Scholar]
- 15.Braga RR, Ballester RY, Daronch M. Influence of time and adhesive system on the extrusion shear strength between feldspathic porcelain and bovine dentin. Dent Mater. 2000;16:303–310. doi: 10.1016/s0109-5641(00)00023-3. [DOI] [PubMed] [Google Scholar]
- 16.Drummond JL, Sakaguchi RL, Racean DC, Wozny J, Steinberg AD. Testing mode and surface treatment effects on dentin bonding. J Biomed Mater Res. 1996;32:533–541. doi: 10.1002/(SICI)1097-4636(199612)32:4<533::AID-JBM6>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 17.Kato H, Matsumura H, Ide T, Atsuta M. Improved bonding of adhesive resin to sintered porcelain with the combination of acid etching and a two-liquid silane conditioner. J Oral Rehabil. 2001;28:102–108. doi: 10.1046/j.1365-2842.2001.00627.x. [DOI] [PubMed] [Google Scholar]
- 18.Kato H, Matsumura H, Atsuta M. Effect of etching and sandblasting on bond strength to sintered porcelain of unfilled resin. J Oral Rehabil. 2000;27:103–110. doi: 10.1046/j.1365-2842.2000.00489.x. [DOI] [PubMed] [Google Scholar]
- 19.Chen JR, Oka K, Kawano T, Goto T, Ichikawa T. Carbon dioxide laser application enhances the effect of silane primer on the shear bond strength between porcelain and composite resin. Dent Mater J. 2010;29:731–737. doi: 10.4012/dmj.2009-106. [DOI] [PubMed] [Google Scholar]
- 20.Matsumura H, Nakamura M, Nakabayashi N, Tanaka T, Atsuta M. Effect of a silane coupling agent and ferric chloride on the bonding of porcelain, quartz and alumina with 4-META/MMA-TBB resin. Dent Mater J. 1987;6:135–139. doi: 10.4012/dmj.6.135. [DOI] [PubMed] [Google Scholar]
- 21.Choi YS, Cho IH. An effect of immediate dentin sealing on the shear bond strength of resin cement to porcelain restoration. J Adv Prosthodont. 2010;2:39–45. doi: 10.4047/jap.2010.2.2.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dozic A, Tsagkari M, Khashayar G, Aboushelib M. Color management of porcelain veneers: influence of dentin and resin cement colors. Quintessence Int. 2010;41:567–573. [PubMed] [Google Scholar]
- 23.Witzel MF, Braga RR, Singer Jde M, Azevedo CL. Bond strength between polymer resin-based cement and porcelaindentin surfaces: influence of polymerization mode and early cyclic loading. Int J Prosthodont. 2003;16:145–149. [PubMed] [Google Scholar]
- 24.Madani M, Chu FC, McDonald AV, Smales RJ. Effects of surface treatments on shear bond strengths between a resin cement and an alumina core. J Prosthet Dent. 2000;83:644–647. [PubMed] [Google Scholar]
- 25.Dietschi D, Monasevic M, Krejci I, Davidson C. Marginal and internal adaptation of class II restorations after immediate or delayed composite placement. J Dent. 2002;30:259–269. doi: 10.1016/s0300-5712(02)00041-6. [DOI] [PubMed] [Google Scholar]
- 26.Dietschi D, Herzfeld D. In vitro evaluation of marginal and internal adaptation of class II resin composite restorations after thermal and occlusal stressing. Eur J Oral Sci. 1998;106:1033–1042. doi: 10.1046/j.0909-8836.1998.eos106609.x. [DOI] [PubMed] [Google Scholar]
- 27.Ozturk N, Aykent F. Dentin bond strengths of two ceramic inlay systems after cementation with three different techniques and one bonding system. J Prosthet Dent. 2003;89:275–281. doi: 10.1067/mpr.2003.37. [DOI] [PubMed] [Google Scholar]
- 28.Jayasooriya PR, Pereira PN, Nikaido T, Tagami J. Efficacy of a resin coating on bond strengths of resin cement to dentin. J Esthet Restor Dent. 2003;15:105–113. doi: 10.1111/j.1708-8240.2003.tb00325.x. [DOI] [PubMed] [Google Scholar]
- 29.Rueggeberg FA, Margeson DH. The effect of oxygen inhibition on an unfilled/filled composite system. J Dent Res. 1990;69:1652–1658. doi: 10.1177/00220345900690100501. [DOI] [PubMed] [Google Scholar]
- 30.Park JW, Ferracane JL. Measuring the residual stress in dental composites using a ring slitting method. Dent Mater. 2005;21:882–889. doi: 10.1016/j.dental.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 31.Pashley EL, Comer RW, Simpson MD, Horner JA, Pashley DH, Caughman WF. Dentin permeability: sealing the dentin in crown preparations. Oper Dent. 1992;17:13–20. [PubMed] [Google Scholar]
- 32.Suh BI. Oxygen-inhibited layer in adhesion dentistry. J Esthet Restor Dent. 2004;16:316–323. doi: 10.1111/j.1708-8240.2004.tb00060.x. [DOI] [PubMed] [Google Scholar]
- 33.Papacchini F, Dall'Oca S, Chieffi N, Goracci C, Sadek FT, Suh BI, Tay FR, Ferrari M. Composite-to-composite microtensile bond strength in the repair of a microfilled hybrid resin: effect of surface treatment and oxygen inhibition. J Adhes Dent. 2007;9:25–31. [PubMed] [Google Scholar]
- 34.Fradeani M, Redemagni M. An 11-year clinical evaluation of leucite-reinforced glass-ceramic crowns: a retrospective study. Quintessence Int. 2002;33:503–510. [PubMed] [Google Scholar]
- 35.Oh SC, Dong JK, Luthy H, Scharer P. Strength and microstructure of IPS Empress 2 glass-ceramic after different treatments. Int J Prosthodont. 2000;13:468–472. [PubMed] [Google Scholar]
- 36.Nakamura T, Ohyama T, Imanishi A, Nakamura T, Ishigaki S. Fracture resistance of pressable glass-ceramic fixed partial dentures. J Oral Rehabil. 2002;29:951–955. doi: 10.1046/j.1365-2842.2002.00929.x. [DOI] [PubMed] [Google Scholar]
- 37.Chang JC, Koh SH, Powers JM, Duong JH. Tensile bond strengths of composites to a gold-palladium alloy after thermal cycling. J Prosthet Dent. 2002;87:271–276. doi: 10.1067/mpr.2002.121583. [DOI] [PubMed] [Google Scholar]
- 38.Andreatta Filho OD, Araujo MA, Bottino MA, Nishioka RS, Menezes MM. Study of thermocycling effect on the bond strength between an aluminous ceramic and a resin cement. J Appl Oral Sci. 2005;13:53–57. doi: 10.1590/s1678-77572005000100011. [DOI] [PubMed] [Google Scholar]
- 39.Borges GA, Caldas D, Taskonak B, Yan J, Sobrinho LC, de Oliveira WJ. Fracture loads of all-ceramic crowns under wet and dry fatigue conditions. J Prosthodont. 2009;18:649–655. doi: 10.1111/j.1532-849X.2009.00498.x. [DOI] [PubMed] [Google Scholar]
- 40.Sobrinho LC, Glover RH, Knowles JC, Cattell MJ. Comparison of the wet and dry fatigue properties of all ceramic crowns. J Mater Sci Mater Med. 1998;9:517–521. doi: 10.1023/a:1008887805177. [DOI] [PubMed] [Google Scholar]
- 41.Geerts SO, Seidel L, Albert AI, Gueders AM. Microleakage after thermocycling of three self-etch adhesives under resinmodified glass-ionomer cement restorations. Int J Dent. 2010;2010:728453. doi: 10.1155/2010/728453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Do Nascimento C, Tiossi R, Hallak Regalo SC, Siessere S, Da Gloria Chiarello De Mattos M, Mardegan Issa JP. Adhesive bond strength between a ceramic system and composite resin bonded by resinous cement submitted or not to thermocycling process. Minerva Stomatol. 2008;57:103–107. [PubMed] [Google Scholar]
- 43.Arici S, Arici N. Effects of thermocycling on the bond strength of a resin-modified glass ionomer cement: an in vitro comparative study. Angle Orthod. 2003;73:692–696. doi: 10.1043/0003-3219(2003)073<0692:EOTOTB>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 44.Andreatta Filho OD, Bottino MA, Nishioka RS, Valandro LF, Leite FP. Effect of thermocycling on the bond strength of a glass-infiltrated ceramic and a resin luting cement. J Appl Oral Sci. 2003;11:61–67. doi: 10.1590/s1678-77572003000100011. [DOI] [PubMed] [Google Scholar]
- 45.Qualtrough AJ, Cramer A, Wilson NH, Roulet JF, Noack M. An in vitro evaluation of the marginal integrity of a porcelain inlay system. Int J Prosthodont. 1991;4:517–523. [PubMed] [Google Scholar]