Abstract
This report describes the case of an edentulous patient with an atrophic maxilla and severe class III malocclusion. Prosthetic rehabilitation was performed using CAD/CAM techniques for manufacturing an implant-supported overdenture with horizontal insertion. A vestibulo-lingual insertion overdenture is a precision prosthesis with a fixation system affording a good fit between the primary and secondary structure. Both structures exhibit passive horizontal adjustment. This treatment option requires the same number of implants as implant-supported fixed dentures. The horizontal assembly system prevents the prosthesis from loosening or moving in response to axial and non-axial forces. The technique was used to rehabilitate a patient presenting an atrophic upper maxilla, with the insertion of 8 implants. No complications were reported at follow-up 3, 6 and 12 months after fitting of the prosthesis. This system offers solutions to the clinical and laboratory complications associated with hybrid prostheses, concealing emergence of the chimneys and improving implant-prosthesis hygiene.
Keywords: Horizontal insertion prosthesis, Horizontal Denture®, Alveolar bone atrophy, Dental prosthesis design, Dental implants, Edentulous jaw
INTRODUCTION
Overdentures can be defined as full removable dentures that are combined with dental implants to improve stability in the mouth. Overdentures are the treatment of choice when edentulous patients are dissatisfied with conventional full dentures, since they offer improved retention, support and stability.1 They are also indicated in cases where implantsupported fixed dentures are not possible due to anatomical problems that preclude the placement of more implants for supporting the fixed dentures, or because of aesthetic and speech problems attributable to a lack of lip support. Since the dentures are removable, hygiene is quite simple, and although frequent maintenance visits are needed, overdentures show good acceptance among patients.2
The present article describes the Horizontal Denture® CAD/CAM, a new implant-supported prosthetic rehabilitation alternative for edentulous patients with atrophic edentulous maxillae designed to join the advantages of conventional removable overdentures and hybrid prostheses. We present the case of an edentulous patient in which this system was used to rehabilitate an atrophic upper maxilla.
DESCRIPTION OF THE TECHNIQUE
The Horizontal Denture® CAD/CAM (Laboratorio Justo Rubio, Valencia, Spain) is a new horizontal (vestibulolingual) path insertion implant-supported removable overdenture design. The horizontal insertion of the secondary structure of the prosthesis over the implant-supported primary structure is based on an anteroposterior assembly or fitting mechanism. In contrast to other overdenture designs, the secondary structure is not fitted onto the primary structure in a saddle-like manner but establishes contact only with the occlusal and vestibular surfaces - the palatine portion of the primary structure being exposed to the oral cavity.
The Horizontal Denture system can be divided into two clearly differentiated parts: (a) the implant-supported or primary structure; and (b) the superstructure or secondary structure. The primary structure is screwed onto the dental implants, and has a design in which the relationships among the different geometrical planes are very important for allowing optimum insertion and fitting of the secondary structure. The occlusal surface is flat and oriented perpendicular (angled 90 degrees) to the lateral surfaces of the bar. The occlusal surface has a series of parallel grooves oriented anteroposteriorly in the direction of insertion of the prosthesis. In this way, when the secondary structure is guided over the grooves, the prosthesis is retained and immobilized.
The secondary structure in turn has a series of geometrical elements shaped inversely to the grooves of the primary structure (i.e., representing a geometrical negative). These slightly conical elements act as stepped rails, facilitating sliding and optimum assembly between the two structures, and preventing the secondary structure from experiencing movements in response to axial or non-axial (oblique) forces. In order for the two structures to fit together correctly, the primary structure must be conical in its sagittal and horizontal planes.
Lastly, the Horizontal Denture system is equipped with a series of locking attachments or latches that afford anteroposterior retention (exerting a vestibular locking effect upon the secondary structure), and allow the patient to check correct fitting of the prosthesis.
Types of designs:
The geometrical design of the primary and secondary structures can vary, depending on the skeletal class of the patient. The differences are confined to the anterior zone, and the designs are classified as follows:
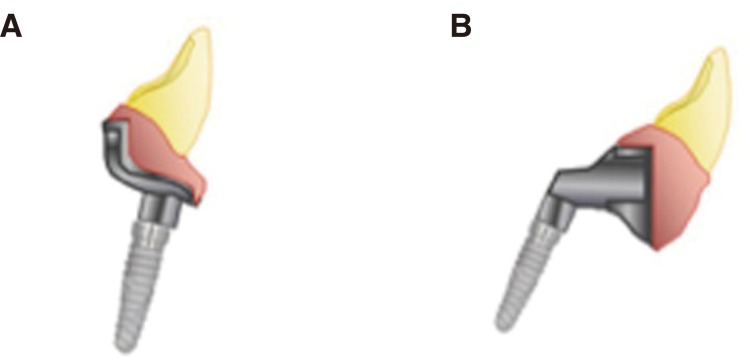
Platform design: This design is used in patients with skeletal class I and II. The anterior zone, corresponding to the incisors, has a flat surface for positioning the anterior teeth in the locations planned in the waxing study. In this way the incisors can be retruded to a position lingual to the implants. This system is ideal for cases characterized by divergent implants or for solving incorrect anterior implant placement (Fig. 1A).
Claw design: This design is used to compensate class III intermaxillary relationships, and is characterized by a facially located bar to support the secondary structure, advancing it towards the correct incisor position (Fig. 1B).
Fig. 1. Classification of the Horizontal Denture® designs, (A) Platform design (class I and II), (B) Claw design (class III).
CLINICAL CASE
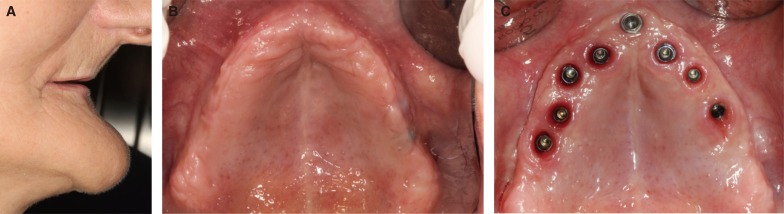
A 62-year-old woman, corresponding to ASA class I and totally edentulous for the last 25 years was seen in the Oral Surgery Teaching Unit of the Department of Stomatology (Faculty of Medicine and Dentistry, Valencia University, Spain) (Fig. 2A, Fig. 2B). She wore lower implant-retained and mucosa-supported overdentures on three intermental implants splinted with an Ackermann bar, and full upper removable dentures. The patient suffered severe atrophy of the upper maxilla (Fig. 2A), with a class III intermaxillary skeletal relationship (Fig. 2B). She complained of discomfort caused by her upper removable dentures and consulted about the possibility of rehabilitation with an implant-supported prosthesis.
Fig. 2. (A) Extraoral view of the loss of lip support of the patient without the prosthesis, (B) Intraoral view of the upper maxilla before treatment. (C) Intraoral view of the location of the 8 TSA® implants with Avantblast surface (Phibo Dental Solutions, Senmenat, Barcelona, Spain) in the maxilla.
Surgery for placement of the implants was performed under local anesthesia (4% articaine with 1:100,000 adrenalin)(Inibsa, LliçaVall, Catalonia, Spain) and sedation with 1% propofol solution. Blood pressure, pulse and oximetry were monitored by the anesthetist.
Alveolar guided bone regeneration was carried out using tricalcium beta-phosphate synthetic particulate bone grafting (Kera-Os®, Keramat®, Coruña, Spain). Six months after bone regeneration, we placed 8 Phibo TSA series 4 implants (TSA® implants, Phibo Dental Solutions, Senmenat, Barcelona, Spain).
Following an osteointegration period of 6 months without functional loading and with the implants submerged at subgingival level, second stage surgery was performed, with placement of the healing abutments (Fig. 2C). After 15 days the prosthodontic protocol for rehabilitation treatment was started.
For the prosthetic procedure a claw design Horizontal Denture® was chosen to compensate the severe class III malocclusion. A double mixture (single phase) casting technique was performed with an open cuvette containing heavy silicone (Sky Implant HeavyMix®, Sweden & Martina®, Padova, Italy) and fluid silicone (Sky Implant Light®, Sweden & Martina®, Padova, Italy), using direct to implant casting coifs. These were splinted with low-contraction acrylic resin (Piku-plast®, Bredent® GmbH, Senden, Germany). We then checked the cast and master model using a resin splint over implants prepared in the laboratory, followed by the obtainment of intermaxillary registries, craniomaxillary transfer and mounting in a semiadjustable articulator (Dentatus®ARL Articulator, Dentatus USA Ltd., New York, NY, USA), in order to perform tooth testing in wax.
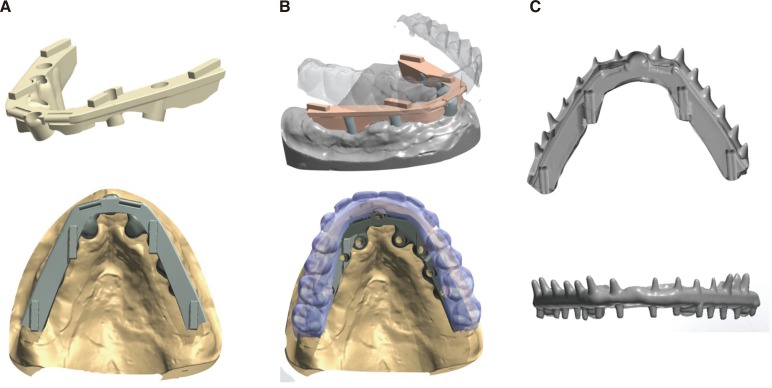
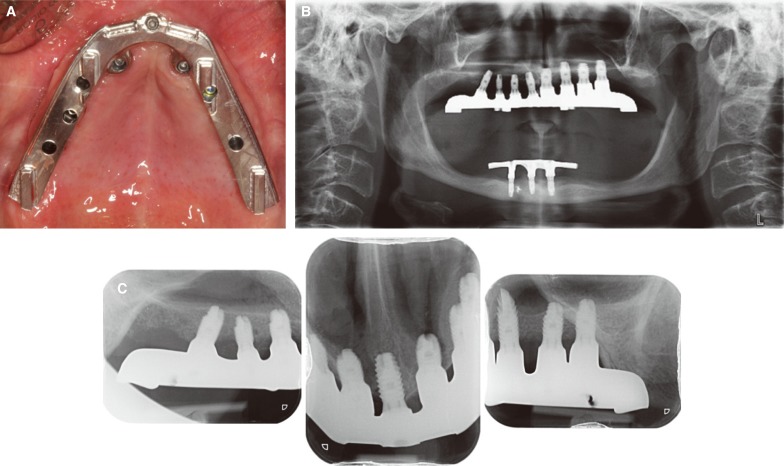
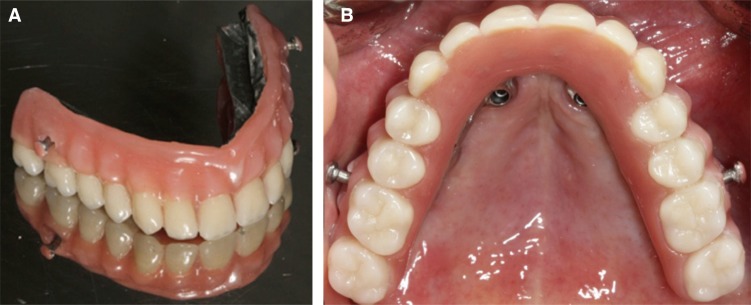
The working models were scanned with an extraoral laser scanner (D710, 3Shape, Copenhagen, Denmark), and tooth testing in wax was likewise scanned placed on the model. From the STL files obtained, we used a CAD tool (3Shape CAD Design Software, Copenhagen, Denmark) to design both the primary structure (Fig. 3A, Fig. 3B) and the secondary structure with a view to facilitating horizontal path insertion and a correct relationship among the different planes of the system, thereby ensuring adequate retention (Fig. 3C). Both structures were manufactured from a grade V titanium (TiAl6V4) block in an industrial machining center using a 5 axis milling unit (Ultrasonic 10, DMG Mori, Bielefeld, Germany). Adjustment of the primary structure was checked by two clinicians by means of the selective pressure test, the single screw test and the use of periapical X-rays (Fig. 4A, Fig. 4B, Fig. 4C). Both clinicians then checked correct fit between the primary and secondary structures (Fig. 5A, Fig. 5B), as well as occlusion and aesthetics using tooth assembly upon the secondary structure (Fig. 6). In fitting the Horizontal Denture®, we checked the occlusal engram, providing the prosthesis with bilateral balanced occlusion, with maximum reduction of the anterior guide contacts because of the mesial cantilever attributable to the class III malocclusion. The patient was instructed on how to insert and remove the overdenture, and emphasis was placed on the importance of adequate oral hygiene.
Fig. 3. (A) CAD/CAM design of the primary structure with the planes of insertion, slots and insertion groves, (B) Best fit between the primary structure with tooth testing for designing the secondary structure, (C) STL file of the design of the secondary structure, with the different grooves, slots and planes for correct coupling to the primary structure.
Fig. 4. (A) View of the Horizontal Denture® primary structure screwed directly onto the implant prosthetic platform, (B) Panoramic X-ray view showing the fit of the upper Horizontal Denture® structure, (C) Periapical X-rays showing passive fit of the primary structure.
Fig. 5. (A) Extraoral view of the Horizontal Denture® secondary structure, (B) Intraoral view of the Horizontal Denture® secondary structure fitted to the primary structure.
Fig. 6. (A) Patient smile after rehabilitation, (B) Extraoral view of the recovered lip support with the prosthesis in place.
The patient returned for follow-up visits 1, 6 and 12 months after prosthetic loading. The degree of patient satisfaction was assessed using a 10 cm visual analog scale (VAS) 6 months after prosthetic placement. This evaluation assessed general satisfaction with the implant-retained prosthesis, and specific satisfaction regarding comfort, stability, phonetics, ease of cleaning, function, aesthetics and selfesteem. The anchor words were "totally dissatisfied" and "completely satisfied." The patient marked the scale independently, though a research assistant was available to offer help or explanations as needed.
At the 12 month follow-up visit, none of the implants had failed and neither prosthetic nor biological complications were observed. The patient reported high satisfaction with the overall treatment, yielding VAS scores of 8 and 9, respectively.
DISCUSSION
This clinical report describes the manufacture of an implantsupported overdenture retained with horizontal path insertion, where the primary and secondary structures were produced using CAD/CAM techniques.
Several studies3,4 have shown the manufacture of primary structures using CAD/CAM techniques to offer better passive fit and less volumetric misfit than structures manufactured from casting techniques. Almasri et al.3 compared the volumetric misfit of CAD/CAM structures and cast structures - the results showing the CAD/CAM techniques to yield structures with less volumetric misfit. This is because the mentioned structures are manufactured in the CAM procedure with a cold milling technique from a metal alloy block, thereby avoiding the dimensional changes of the metal associated with the casting technique. Moreover, clinical studies with a follow-up period of 10 years showed a reduced number of technical complications of the CAD/CAM structures compared with casting structures.5
In our case, after evaluating the patient condition, we decided that the best option would be to use an implantsupported overdenture with horizontal path insertion manufacturing with CAD/CAM technology.
However, manufacturing this type of prosthesis can be a complex and costly when conventional casting techniques are used. Such techniques are moreover dependent upon the knowledge and skill of the laboratory technician. In our case, the prosthesis had different planes, insertion grooves and slots in the primary structure, providing an adequate guide for inserting the prosthesis and friction with the lateral walls and horizontal grooves that help keep the secondary structure in place. In this context, manufacturing using conventional casting techniques increases the cost and working time required to achieve passive fit of the primary structure and adequate adjustment between the two structures.
Prostheses of this kind can be prepared with casting techniques,6 though the dimensional changes that appear after cooling of the metal alloy can diminish the fit between the two structures, producing mechanical complications such as for example movements secondary to loss of friction or wearing of the surfaces of both structures.
At the present, we can design the slots, grooves and planes of structures of this kind using CAD/CAM techniques, with the previous production of a wax, resin or composite template, which is then scanned using an extraoral scanner. This is known as a "partial CAD/CAM product".7,8,9 In our case, we obviated the template because the new design software offers the option of fully designing the CAD/CAM structure without a previous template. The result is known as a "complete CAD/CAM product".9 With this protocol we only scan the master model and the wax trial denture, thereby reducing the economic cost and working time. A number of authors10,11,12 have used this type of protocol, with results similar to those obtained with previous production and scanning of a template structure.
The main clinical factors causing us to prefer Horizontal Denture® instead of a fixed prosthesis are:
(a) The need for lip support. Facial aesthetics are affected when adequate lip support is lacking. Prolonged edentulism of the upper maxilla gives rise to bone reabsorption in the cranial and palatine direction, and overdentures make it easier to overcome this problem.13
(b) Intermaxillary distance. When an implant-supported fixed prosthesis is used and the intermaxillary distance is excessive, the teeth of the prosthesis will be too long and there may be wide gaps between them. Overdentures are to be preferred if the mentioned distance is over 15 mm.1
(c) Hygiene of the prosthesis. Hygiene is much easier when overdentures are used.6
We use overdentures of this kind in the upper maxilla in the case of patients with important bone reabsorption, since it is easy to compensate the lack of peribuccal support.13
Due to the biomechanical requirements and poorer bone quality, the management options with Horizontal Denture® in the upper maxilla are limited to overdentures on 6 implants or overdentures on more than 6 implants. The number of implants is the same as when fixed prostheses are used to rehabilitate the maxilla, since such treatment is functionally implant-supported.
The advantages of this type of horizontal insertion design include the fact that it prevents the prosthesis from loosening or moving in response to axial and non-axial forces. Such prostheses comprise two structures - the secondary structure having the same geometry and orientations as the primary structure, though in reverse (i.e., representing a geometrical negative), thereby ensuring adequate coupling of the two structures.6
The comparative studies between conventional prostheses and overdentures found in the literature show overdentures to produce less bone reabsorption, offer better retention and stability, and thus result in better chewing effectiveness. These advantages in turn produce greater patient satisfaction and improved quality of life.14,15,16,17,18,19
Ueda et al.,20 in a 24 year follow-up of patients wearing mandibular overdentures, recorded a success rate of 85.9%, and concluded that overdentures offer successful long-term treatment results.
CONCLUSION
This implant-supported horizontal insertion overdenture design produced by CAD/CAM technology appears to be a feasible treatment option in application to the upper maxilla of patients with class III skeletal relationships, where the negative intermaxillary discrepancy must be compensated. In this context, CAD/CAM techniques allow us to produce a technically complicated prosthesis more quickly, with a lesser economic cost, and with better fit between the primary and secondary structures than when conventional casting techniques are used.
References
- 1.Slot W, Raghoebar GM, Vissink A, Huddleston Slater JJ, Meijer HJ. A systematic review of implant-supported maxillary overdentures after a mean observation period of at least 1 year. J Clin Periodontol. 2010;37:98–110. doi: 10.1111/j.1600-051X.2009.01493.x. [DOI] [PubMed] [Google Scholar]
- 2.Sadowsky SJ, Caputo AA. Effect of anchorage systems and extension base contact on load transfer with mandibular implant-retained overdentures. J Prosthet Dent. 2000;84:327–334. doi: 10.1067/mpr.2000.109378. [DOI] [PubMed] [Google Scholar]
- 3.Almasri R, Drago CJ, Siegel SC, Hardigan PC. Volumetric misfit in CAD/CAM and cast implant framework: a university laboratory study. J Prosthodont. 2011;20:267–274. doi: 10.1111/j.1532-849X.2011.00709.x. [DOI] [PubMed] [Google Scholar]
- 4.Eliasson A, Wennerberg A, Johansson A, Ortorp A, Jemt T. The precision of fit of milled titanium implant frameworks (I-Bridge) in the edentulous jaw. Clin Implant Dent Relat Res. 2010;12:81–90. doi: 10.1111/j.1708-8208.2008.00131.x. [DOI] [PubMed] [Google Scholar]
- 5.Örtorp A, Jemt T. CNC-milled titanium frameworks supported by implants in the edentulous jaw: a 10-year comparative clinical study. Clin Implant Dent Relat Res. 2012;14:88–99. doi: 10.1111/j.1708-8208.2009.00232.x. [DOI] [PubMed] [Google Scholar]
- 6.Solá-Ruíz MF, Agustin-Panadero R, Fons-Font A, Labaig-Rueda C. An implant-supported overdenture design with a horizontal path of insertion. J Prosthet Dent. 2013;110:239–242. doi: 10.1016/S0022-3913(13)00199-6. [DOI] [PubMed] [Google Scholar]
- 7.Katsoulis J, Brunner A, Mericske-Stern R. Maintenance of implant-supported maxillary prostheses: a 2-year controlled clinical trial. Int J Oral Maxillofac Implants. 2011;26:648–656. [PubMed] [Google Scholar]
- 8.Papaspyridakos P, Lal K. Computer-assisted design/computer-assisted manufacturing zirconia implant fixed complete prostheses: clinical results and technical complications up to 4 years of function. Clin Oral Implants Res. 2013;24:659–665. doi: 10.1111/j.1600-0501.2012.02447.x. [DOI] [PubMed] [Google Scholar]
- 9.Kapos T, Evans C. CAD/CAM technology for implant abutments, crowns, and superstructures. Int J Oral Maxillofac Implants. 2014;29:117–136. doi: 10.11607/jomi.2014suppl.g2.3. [DOI] [PubMed] [Google Scholar]
- 10.Tahmaseb A, De Clerck R, Aartman I, Wismeijer D. Digital protocol for reference-based guided surgery and immediate loading: a prospective clinical study. Int J Oral Maxillofac Implants. 2012;27:1258–1270. [PubMed] [Google Scholar]
- 11.Sanna AM, Molly L, van Steenberghe D. Immediately loaded CAD-CAM manufactured fixed complete dentures using flapless implant placement procedures: a cohort study of consecutive patients. J Prosthet Dent. 2007;97:331–339. doi: 10.1016/S0022-3913(07)60021-3. [DOI] [PubMed] [Google Scholar]
- 12.Komiyama A, Klinge B, Hultin M. Treatment outcome of immediately loaded implants installed in edentulous jaws following computer-assisted virtual treatment planning and flapless surgery. Clin Oral Implants Res. 2008;19:677–685. doi: 10.1111/j.1600-0501.2008.01538.x. [DOI] [PubMed] [Google Scholar]
- 13.Brånemark PI, Svensson B, van Steenberghe D. Ten-year survival rates of fixed prostheses on four or six implants ad modum Brånemark in full edentulism. Clin Oral Implants Res. 1995;6:227–231. doi: 10.1034/j.1600-0501.1995.060405.x. [DOI] [PubMed] [Google Scholar]
- 14.den Dunnen AC, Slagter AP, de Baat C, Kalk W. Adjustments and complications of mandibular overdentures retained by four implants. A comparison between superstructures with and without cantilever extensions. Int J Prosthodont. 1998;11:307–311. [PubMed] [Google Scholar]
- 15.Semper W, Heberer S, Nelson K. Retrospective analysis of bar-retained dentures with cantilever extension: marginal bone level changes around dental implants over time. Int J Oral Maxillofac Implants. 2010;25:385–393. [PubMed] [Google Scholar]
- 16.Rashid F, Awad MA, Thomason JM, Piovano A, Spielberg GP, Scilingo E, Mojon P, Müller F, Spielberg M, Heydecke G, Stoker G, Wismeijer D, Allen F, Feine JS. The effectiveness of 2-implant overdentures - a pragmatic international multicentre study. J Oral Rehabil. 2011;38:176–184. doi: 10.1111/j.1365-2842.2010.02143.x. [DOI] [PubMed] [Google Scholar]
- 17.Assunção WG, Barão VA, Delben JA, Gomes EA, Tabata LF. A comparison of patient satisfaction between treatment with conventional complete dentures and overdentures in the elderly: a literature review. Gerodontology. 2010;27:154–162. doi: 10.1111/j.1741-2358.2009.00299.x. [DOI] [PubMed] [Google Scholar]
- 18.Melilli D, Rallo A, Cassaro A. Implant overdentures: recommendations and analysis of the clinical benefits. Minerva Stomatol. 2011;60:251–269. [PubMed] [Google Scholar]
- 19.Rossetti PH, Bonachela WC, Rossetti LM. Relevant anatomic and biomechanical studies for implant possibilities on the atrophic maxilla: critical appraisal and literature review. J Prosthodont. 2010;19:449–457. doi: 10.1111/j.1532-849X.2010.00615.x. [DOI] [PubMed] [Google Scholar]
- 20.Ueda T, Kremer U, Katsoulis J, Mericske-Stern R. Long-term results of mandibular implants supporting an overdenture: implant survival, failures, and crestal bone level changes. Int J Oral Maxillofac Implants. 2011;26:365–372. [PubMed] [Google Scholar]