Abstract
Background
Antiretroviral therapy (ART) markedly reduces HIV transmission, and testing and treatment programs have been advocated as a method for decreasing transmission at the population level. Little is known, however, about the extent to which sexually transmitted infections (STIs), which increase the HIV infectiousness of untreated individuals, may decrease the effectiveness of treatment as prevention.
Methods
We searched major bibliographic databases to August 12th, 2014 and identified studies reporting differences in HIV transmission rate or in viral load between individuals on ART who either were or were not co-infected with another STI. We used hierarchical Bayesian models to estimate viral load differences between individuals with and without STI co-infections.
Results
The search strategy retrieved 1630 unique citations of which 14 studies (reporting on 4607 HIV viral load measurements from 2835 unique individuals) met the inclusion criteria. We did not find any suitable studies that estimated transmission rates directly in both groups. Our meta-analysis of HIV viral load measurements among treated individuals did not find a statistically significant effect of STI co-infection; viral loads were, on average, 0.11 log10 (95 % CI −0.62 to 0.83) higher among co-infected versus non-co-infected individuals.
Conclusions
Direct evidence about the effects of STI co-infection on transmission from individuals on ART is very limited. Available data suggests that the average effect of STI co-infection on HIV viral load in individuals on ART is less than 1 log10 difference, and thus unlikely to decrease the effectiveness of treatment as prevention. However, there is not enough data to rule out the possibility that particular STIs pose a larger threat.
Electronic supplementary material
The online version of this article (doi:10.1186/s12879-015-0961-5) contains supplementary material, which is available to authorized users.
Background
A large body of evidence suggests that antiretroviral therapy (ART), particularly with newer treatment regimens, markedly reduces the risk of sexual transmission of HIV. Recent systematic reviews have estimated that ART causes a more than ten-fold reduction in the incidence rate within discordant couples, to less than 0.5 per 100 person-years [1–6].
These sharp reductions have inspired the idea of antiretroviral treatment as prevention—aggressive programs to identify and treat HIV-positive individuals could substantially reduce HIV incidence at the population level, by reducing the infectiousness of HIV-infected individuals [5, 7]. However, increased infectiousness when treated individuals are co-infected with one or more other sexually transmitted infections (STIs) could potentially undercut the effectiveness of treatment as prevention programs. Concern with the effects of co-infection on HIV transmission is exemplified in the 2008 “Swiss Statement,” which argues that HIV sexual transmission risk is of no concern within stable discordant relationships in which: an HIV-positive partner is adhering to treatment under the care of a physician; the viral load has been suppressed for at least six months; and no other STIs are infecting the HIV-positive partner [8].
Although the biological mechanisms underlying this increased risk are not fully understood, many STIs have been associated with higher risks of both HIV acquisition and sexual transmission [9–15]. Increased HIV transmission may be underpinned by higher HIV viral load resulting from larger concentration of HIV-infected immune cells in genital secretions induced by an inflammatory response and/or additional pathways caused by genital ulcers [16]. Similarly, inflammatory STIs, by recruiting immune cells, may provide additional targets for HIV virions, increasing HIV acquisition risk. Ulcerative STIs may present additional entry points for HIV infection [15].
Studies of HIV-STI interactions have been conducted mostly on individuals not receiving ART. Less is known about the impact of STI co-infections on HIV shedding from treated individuals. STI prevalence is high among HIV-infected individuals [17] and the proportion of these individuals on ART is quickly rising [18]. Thus, any potential increased HIV infectiousness due to STI co-infections among treated individuals could have important epidemiological consequences as treatment as prevention becomes more widespread.
Disentangling the many interacting factors at play is challenging: many STIs are suspected of affecting HIV shedding [9] and it remains unclear whether how these effects interact in people with more than one such infection; the viral load response to ART is regimen- and gender-specific [19]; numerous (not necessarily consistent) methods are used to sample and quantify HIV viral load [20, 21]; viral load measurements can vary between anatomical sites within an infected individual [22]; and HIV viral loads exhibit substantial temporal variation [23]. When considering transmission events in discordant couples, isolating the effect of STI co-infections is challenging because concomitance of STI infections in both partners (that could affect both HIV susceptibility and infectiousness) and HIV transmission are often not practical to ascertain.
Here, we conduct a systematic review and meta-analysis of the available evidence to assess whether STI co-infections affect the risk of HIV transmission from individuals on ART. We searched for studies that estimated transmission directly, and also for studies that measured viral load, which we intended to use as a proxy for transmission if the direct evidence was insufficient.
Methods
This systematic review and meta-analysis followed the guidelines from the PRISMA statement [24] (see Additional file 1). A protocol was prospectively registered in the PROSPERO database (see Additional file 2). Published peer-reviewed observational studies and randomized controlled trials were considered for inclusion. We included studies of sexually active HIV-infected participants on ART that were further classified into two subgroups: participants whose only known STI was HIV (the “mono-infected group”) and those with HIV and co-infected with another STI (the “co-infected group”). Studies were eligible for inclusion if they measured HIV viral loads among HIV-infected participants, or if they observed at least monthly HIV transmission events and STI infection status in discordant couples. An individual was considered co-infected only if the STI was laboratory confirmed. Individuals with ongoing treatment for the co-infecting STI were not included.
We searched for all relevant studies in Medline (Ovid), EMBASE (Ovid), PubMed, CINAHL and the Cochrane Library from inception to August 12th, 2014. Subject headings and text words associated with the risk of HIV sexual transmission, ART and STIs were included in the search strategies. We included STIs commonly discussed in the context of HIV transmission: Chlamydia trachomatis, chancroid (H. ducreyi), any type of Human Papilloma Virus, Herpes Simplex Virus 2, Neisseria gonorrhoeae, syphilis (T. pallidum) and Trichomoniasis (T. vaginalis). We also included bacterial vaginosis and candidal vaginitis, although these are not known to result directly from sexual transmission, and urethritis, which can be associated with more than one STI. The search did not impose any language or geographical restrictions on studies. The STI positivity definitions are given in Additional file 3 and full search strategies in Additional file 4.
All retrieved abstracts were read by three authors (DC, CS and SH). Eligibility assessment was performed independently by two authors for each abstract, using pre-defined guidelines. Disagreement between authors was resolved by consensus after discussion. Data from eligible studies were extracted independently by two authors (DC and SH).
We sought to assess how two primary outcomes of interest, HIV viral loads and HIV transmission rates within discordant couples, varied between HIV-infected participants on ART with and without STI co-infections. We sought additional data to assess potential sources of bias within and between studies including STI diagnostic methods; anatomical sites sampled for HIV viral load measurements; HIV assays; interval between STI co-infection diagnosis and HIV viral load measurement; ART regimen, treatment length and adherence; study design; HIV-infected participant age, gender, and sexual orientation; and, for serodiscordant couple studies, concomitance of STI co-infection in HIV-uninfected partner and HIV genetic linkage following secondary partner seroconversion. Within studies, we excluded individuals not explicitly known to be on ART and, when this information was available, those who had been on ART for less than 30 days. We probed study quality by summarizing variables and methods (Tables 1 and 2), and with forest and funnel plots (Figs. 3 and 4).
Table 1.
Summary table of studies included in the meta-analysis
| Study | Study objective | Country | Population | Coverage period | Study design | STI | STI assessment method | Number of participants | Individuals included in meta-analysis | HIV viral load measure | HIV VL anatimical site |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Adolf 2012 [31] | Prevalence and risk factors for syphilis among HIV+ | Brazil | Females and males; STI/HIV clinic patients-SoBrHIV cohort | 1991–2008 | Case-control | Tp | VDRL, FTA | 1012 | 759 | Not reported | Blood plasma |
| Anderson 2008 [32] | Association between presence of inflammatory | USA | Females; STI/HIV clinic patients | Not reported | Prospective cohort | Bv Ct Cv Ng Tp Tv | Bv: Amsel | 97 | 41 | RNA | Blood and CVL |
| Ct, Ng: culture | |||||||||||
| Cv: visual exam | |||||||||||
| Tv: wet mount | |||||||||||
| Tp: RPR | |||||||||||
| Conley 2010 [33] | Prevalence and risk factors for abnormal anal cytology among HIV+ | USA | Females and males; STI/HIV clinic patients - SUN study | 2004–2006 | Prospective cohort | Ct HPV HSV Ng Tp Tv | HPV, Ng, Ct: NAAT, cytological | 621 | 147 | RNA | Not reported |
| Tv: NAAT | |||||||||||
| HSV2: serology | |||||||||||
| Chan 2008 [12] | Correlation between HIV VL in blood and semen among men both ART naive and experienced | Australia | Males; STI/HIV clinic patients | 2003–2006 | Prospective cohort | Ct Ng Tp | Ct: NAAT | 119 | 81 | RNA | Blood and semen |
| Ng: culture | |||||||||||
| Tp: Fabs + RPR | |||||||||||
| Cu-Uvin 2001 [26] | Impact of genital tract infections on HIV cervicovaginal shedding | USA | Females; STI/HIV clinic patients | Not reported | Prospective cohort | Bv Cv Tv | Bv: Amsel | 108 | 61 | RNA | Blood and CVL |
| Cv, Tv: culture | |||||||||||
| Graham 2011 [34] | Impact of genital ulcerations on HIV genital shedding | Kenya | Females; STI/HIV clinic patients | 2004–2008 | Prospective cohort nested | Bv Ct Cv Hd Ng Tp Tv | Tv: wet mount | 145 | 37 | RNA | Cervix and vagina |
| Bv: Nugent | |||||||||||
| Cv: not reported | |||||||||||
| Ng: culture + NAAT | |||||||||||
| Ct: NAAT | |||||||||||
| Hd: culture | |||||||||||
| Tp: serology | |||||||||||
| Jarzebowski 2012 [35] | Impact of syphilis on CD4 and HIV VL | France | Males; MSM-FHDH cohort | 1998–2006 | Case-control | Tp | Not reported | 1515 | 1271 | RNA | Blood plasma |
| Kofoed 2006 [36] | Impact of Syphilis infection on CD4, HIV VL and response after anti-treponemal treatment | Denmark | Males; MSM | 2003–2004 | Prospective experimental | Tp | Dark field, serology | 38 | 34 | RNA | Blood plasma |
| Madeddu 2014 [41] | HPV screening should be done even on HIV-positive women on ART | Italy | Females; STI/HIV clinic patients | 2008–2009 | Prospective cohort | HPV | NAAT | 57 | 52 | RNA | Blood plasma |
| Politch 2012 [37] | Prevalence of seminal HIV shedding among MSM on ART | USA | Males; MSM | Not reported | Prospective cohort | Ct HSV Ng Tp NGU | HSV: serology | 101 | 96 | DNA and RNA free and RNA assoc | Semen |
| Ct, Ng, Tp: not reported | |||||||||||
| Sadiq 2002 [38] | Effect of urethritis on seminal HIV VL for patients on ART | UK | Males; MSM | 1998–2000 | Prospective cohort | Ct Ng NGU | Ng: culture | 40 | 39 | RNA and DNA | Blood and semen |
| Ct: NAAT | |||||||||||
| Sha 2005 [39] | Association of Bv and Bv-associated bacteria with HIV genital VL | USA | Females; STI/HIV clinic patients | 1994–1997 | Prospective cohort | Bv Ct Cv HPV HSV Ng Tp Tv | Bv: Amsel + Nugent | 362 | 107 | RNA | Blood and CVL |
| Tp: symptoms + DFA | |||||||||||
| Ct, Ng: culture + pap | |||||||||||
| HSV: symptoms + pap | |||||||||||
| HPV: NAAT | |||||||||||
| Sudenga 2012 [40] | HSV2 epidemiology in HIV+/at risk adolescents | USA | Females and males; adolescent; REACH cohort | 1996–2000 | Case-control | Bv Ct Hd HPV HSV Ng Tp Tv | HSV2: serology | 513 | 60 | RNA | Blood plasma |
| Ct, Ng, HPV: NAAT | |||||||||||
| Bv: gram stain + clinical criteria | |||||||||||
| Tv: culture | |||||||||||
| Winter 1999 [10] | Impact of asymptomatic urtethritis on HIV VL in semen | UK | Males; STI/HIV clinic patients | Not reported | Prospective cohort | Ct Ng NGU | Ng: Gram stain, culture | 94 | 53 | RNA cell free | Blood and semen |
| Ct: NAAT |
MSM: men who have sex with men
Bv Bacterial vaginosis, Cv Candidal vaginitis, Ct Chlamydia trachomatis, HPV, human papillomavirus, HSV human simplex virus type 2, Ng Neisseria gonorrhoeae, Tp Treponema pallidum, Tv Trichomonas vaginalis, Ur urethritis
Table 2.
Assessment of risk of bias within studies
| Study | Number of STIs tested | Sampling site for HIV | ART adherence reported |
|---|---|---|---|
| Adolf 2012 [31] | 1 | Blood plasma | No |
| Anderson 2008 [32] | 6 | Blood and CVL | No |
| Conley 2010 [33] | 6 | Not reported | No |
| Chan 2008 [12] | 3 | Blood and semen | No |
| Cu-Uvin 2001 [26] | 3 | Blood and CVL | No |
| Graham 2011 [34] | 7 | Cervix and vagina | Yes |
| Jarzebowski 2012 [35] | 1 | Blood plasma | No |
| Kofoed 2006 [36] | 1 | Blood plasma | No |
| Madeddu 2014 [41] | 1 | Blood plasma | Yes |
| Politch 2012 [37] | 4 | Semen | No |
| Sadiq 2002 [38] | 2 | Blood and semen | No |
| Sha 2005 [39] | 8 | Blood and CVL | No |
| Sudenga 2012 [40] | 8 | Blood plasma | Yes |
| Winter 1999 [10] | 2 | Blood and semen | No |
Studies reporting a large number of STIs tested, ART adherence and measuring HIV, VL viral load in genital secretions are less likely to bias estimates of the effect of STI co-infection on HIV transmission, CVL cervicovaginal lavage
Fig. 3.
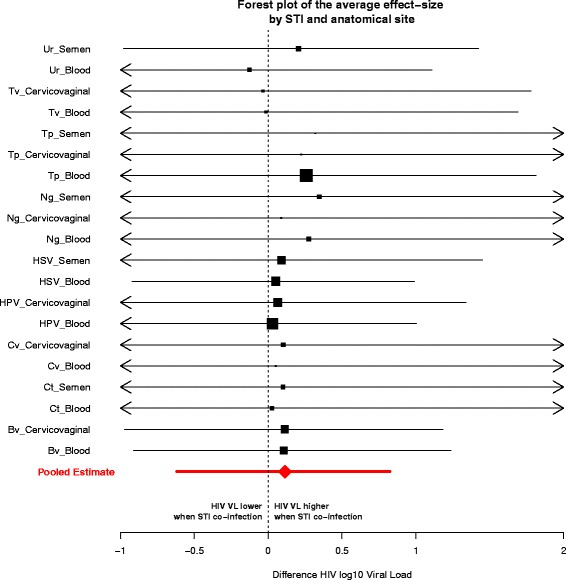
Forest plot for a given STI/anatomical site pair. Posterior means and 95 % credible intervals of the effect size for each study included in the meta-analysis. The effect size is expressed as the difference of HIV viral load (log10) between an individual HIV positive, co-infected with an STI and an individual only infected with HIV. The black square represents the mean of the distribution, its area is proportional to the number of data points associated with the specific STI/anatomical site pair; segments represent the 95 % credible intervals (CI). The red diamond shows the mean of the pooled effect (across all studies, STIs and anatomical sites) and the segment its 95 % CI. Bv: Bacterial vaginosis; Ct: Chlamydia trachomatis; Cv: Candidal vaginitis; Bacterial vaginosis; HPV: human papillomavirus; HSV: human simplex virus type 2; Ng: Neisseria gonorrhoeae; Tp: Treponema pallidum; Tv: Trichomonas vaginalis; Ur: urethritis
Fig. 4.
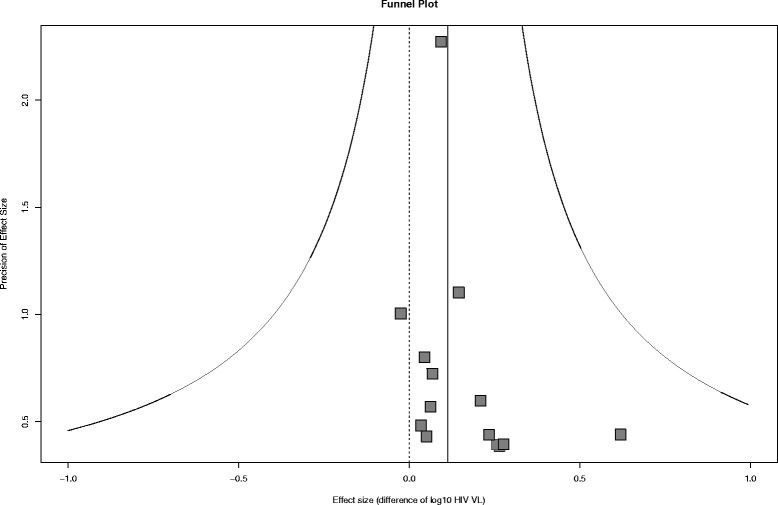
Funnel plot. The horizontal axis represents the mean posterior effect size for each study (the log10 HIV viral load between HIV positive individuals with and without STI co-infection), the vertical axis is the effect size precision (inverse of the standard deviation) of the associated study. Each point represents a study. The solid vertical line represents the mean effect size and the solid curved lines represent its 95 % CI. The dashed vertical line represents a null effect size (no HIV viral load difference)
Planned measures of effect were: the difference in log10 HIV viral load between the mono- and co-infected groups, for a given anatomical site and STI; and the relative HIV transmission rate between HIV-discordant couples with the infected partner belonging to the mono- versus co-infected group.
Statistical analysis
This review aims to gather all available evidence regarding the effect of STI on HIV infectiousness, whether this was the primary objective of a study or not. Hence, heterogeneity in study design is inevitable. For example, HIV viral load can be measured at different anatomical sites, with different sampling techniques, for patients with different STI co-infections. Estimating a single summary statistic for such heterogeneous effects is challenging. Adopting a classical approach to conduct the meta-analysis would make it difficult to fit all the studies into one modelling framework. For example it might be necessary to choose a threshold and dichotomize data from studies providing continuous HIV viral load in order to compare them with the ones providing dichotomous data only. Hierarchical Bayesian models offer a flexible framework to coherently incorporate heterogeneous variables that theoretically relate to a common effect while providing estimates of the variability at each conceptual level [25].
We therefore used a Bayesian hierarchical model to estimate—across heterogeneous studies—an overall effect of STI co-infection on HIV viral load, while also estimating how this effect differed depending on the anatomical site sampled for viral load measurements and on the specific STI co-infection. Similarly, we also estimated how the effect of STI co-infection differed between studies and included individual-level random effects for longitudinal studies. Studies where the only outcome available was dichotomous (HIV viral load above or below a stated threshold) [10, 12, 26] were combined with studies that provided continuous outcomes by introducing latent variables [27]. We used uninformative priors for all effect sizes and their variances [28]. The details of the model and our prior choices are provided in Additional file 5. The model was developed in R version 3.0.2 [29] with package RSTAN version 2.2.0 [30]. Code is available upon request.
Results
Systematic review
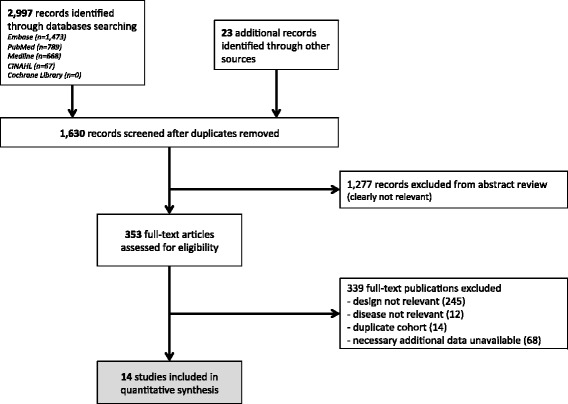
Our database searches identified 2997 citations. In addition, 23 records were identified outside the database search (mostly via references cited in the publications retrieved from the database search). After duplicates were removed, 1630 records were assessed for eligibility (Fig. 1). We excluded 1277 records with abstracts that obviously did not meet our inclusion criteria, leaving 353 to be assessed with a full-text review. When studies appeared to have obtained but not published data relevant to our meta-analysis, we requested them from the original investigators. Of 73 investigators contacted for additional data, 21 responded and 10 provided data. This second screening identified 14 studies with sufficient information to be included in the meta-analysis [10, 12, 26, 31–41]. All studies included in our meta-analysis were approved by an ethics committee.
Fig. 1.
Flow chart of the selection process
Table 1 summarizes the main characteristics of each eligible study. No studies involving discordant couples were eligible because none of them monitored HIV incidence and STI status at least monthly (our threshold to ascertain concomitance). Hence our findings are limited to an indirect measurement of HIV-infectiousness as measured by viral load at various anatomical sites. Of these 14 studies, two studies included participants from resource-limited countries [31, 34]; four studies focused on MSM [35–38]; and two reported on ART adherence [34, 40]. Syphilis, chlamydia and gonorrhea were the most reported STIs in the eligible studies. We provide further detail on the STI co-infections tested for and the anatomical sites sampled by each study in the Additional file 6.
Three studies included in this review [31, 33, 40] did not focus on differences in HIV infectiousness between STI co-infected and HIV mono-infected groups as a primary outcome. Among the 11 other studies, 7 suggest that co-infection with another genital infection may be associated with an increase in HIV viral load [10, 26, 35–39].
Table 2 outlines the main features from studies that could bias our estimates. The more STIs tested, the smaller the risk of incorrectly categorizing individuals as mono-infected. Six studies [32–34, 37, 39, 40] out of 14 reported on testing more than 4 STIs (in addition to HIV). Reporting adherence to ART reduces statistical misattribution of the reasons for increases in HIV viral load. Three studies [20, 34, 41] out of 14 explicitly reported adherence to ART. Because of HIV compartmentalization [42] (viral concentration may substantially differ between different anatomical sites within the same individual at a given time), measuring HIV viral load in genital or anal secretions is most relevant when considering sexual transmission. Eight out of 14 studies measured HIV viral load in such anatomical sites [10, 12, 26, 32, 34, 37–39].
Meta-analysis
The 14 studies included in the meta-analysis represent 4607 visits from 2835 unique individuals (Table 3). The posterior distributions of effect sizes for each study, averaged across the associated STIs and anatomical sites, are shown in Fig. 2. We estimated that, among HIV-infected individuals on ART, the presence of another STI co-infection was associated with an HIV viral load 0.11 log10 (95 % CI −0.62 to 0.83) higher than in HIV mono-infected individuals, averaging over both anatomical sites and different STIs. Thus, we did not find a statistically significant effect of STI co-infection on the viral load of HIV-infected individuals on ART. Similarly, we did not find any statistically significant effect of STI co-infections on viral load when examining the effect on viral load as measured at a particular anatomical site, or for a particular STI co-infection, although we note that most of the posterior distributions for the effects of co-infection on viral load had positive means (Fig. 3).
Table 3.
Number of HIV viral loads measurements included in the meta-analysis by STI co-infection and anatomical sites
| STI | Blood | Cervicovaginal | Semen | Total |
|---|---|---|---|---|
| Bv | 51 | 52 | n/a | 103 |
| Ct | 9 | 0 | 9 | 18 |
| Cv | 2 | 9 | n/a | 11 |
| HPV | 260 | 76 | 0 | 336 |
| HSV | 86 | 0 | 60 | 146 |
| Ng | 9 | 2 | 9 | 20 |
| Tp | 656 | 2 | 2 | 660 |
| Tv | 4 | 4 | 0 | 8 |
| Ur | 9 | n/a | 12 | 21 |
| none | 2915 | 192 | 177 | 3284 |
| Total | 4001 | 337 | 269 | 4607 |
Category “none” means there was no STI (other than HIV) co-infecting the patient
Bv bacterial vaginosis, Cv candidal vaginitis, Ct Chlamydia trachomatis, HPV human papillomavirus, HSV human simplex virus type 2, Ng Neisseria gonorrhoeae, Tp Treponema pallidum, Tv Trichomonas vaginalis, Ur urethritis, n/a not applicable
Fig. 2.
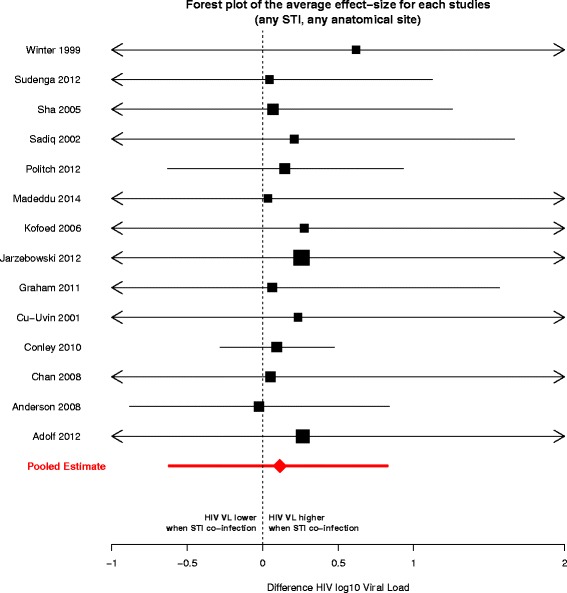
Posterior means and 95 % credible intervals of the effect size for each study included in the meta-analysis. The effect size is expressed as the difference of HIV viral load (log10) between an individual HIV positive, co-infected with any other STI and an individual only infected with HIV. The black square represents the posterior mean, with its area proportional to study sample size. The red diamond and arrows reflect estimates of the pooled effect (i.e., across all studies, STIs and anatomical sites)
Figure 4 shows a funnel plot of included studies and doesn’t exhibit a strong asymmetry, hence suggests no obvious publication bias. Another risk of bias across studies could have been introduced if temporal changes in STI prevalence and ART regimens were not adequately captured by the model.
The impact of heterogeneity between studies on the summary effect size (using the I2 statistic [43]) could not be reliably captured because of the large variance associated with our estimates (see Additional file 5). Three studies [31, 39, 40] exhibited HIV viral loads indicative of incomplete viral suppression in a non-negligible proportion of participants (i.e. HIV viral load above 4 log10). We did a sensitivity excluding these studies and did not find any qualitative differences in our results (see Additional file 7).
Visits where patients were co-infected with two or more STIs other than HIV (381 out of 4219 total visits) were not used in the main analysis because our model structure specified unique effects for each type of STI co-infection; we used a sensitivity analysis to explore the effects of this exclusion and found no qualitative impact on our results (see Additional file 7).
Discussion
In the absence of qualifying studies that measured transmission risk directly, we conducted a meta-analysis of all available evidence of increased HIV viral load due to STI co-infection of individuals on ART, as a proxy for increased infection risk. Pooling information from all available studies, anatomical sites, and co-infections, we estimated that the average difference in viral load due to STI co-infection of individuals on ART was 0.11 log10 (95 % CI −0.62 to 0.83) greater than HIV mono-infected individuals.
Although our study provides some evidence for a small effect of STI co-infection on viral loads, we cannot rule out the possibility of no effect, or the possibility of a moderately large effect (the upper credible interval is 0.83 log10). Importantly, we are also not able to rule out the possibility that certain STIs (or certain combinations of STIs and anatomical site) have a much larger effect (see Fig. 3). Nonetheless, based on our analysis, we cautiously posit that ART manages—on average—to sustain its effectiveness at keeping HIV viral loads low during STI co-infection episodes, at the anatomical sites considered in this review (blood plasma, semen and cervicovaginal), and thus would be expected to maintain its effectiveness at preventing transmission.
Even with nearly 5000 data points used in this meta-analysis, realistic consideration of the variation between studies, STIs and anatomical sites reduces the statistical power considerably. There are other limitations that need to be highlighted.
Because eligible studies only estimated HIV viral loads, not transmission rates in discordant couples, our summary effect size is a proxy for HIV infectiousness and might not be an accurate representation of the actual sexual transmission risk. There were no eligible studies measuring rectal HIV viral load, so our estimate may not be applicable in assessing change in HIV infectiousness from receptive anal intercourse.
Not all studies tested for all STIs, hence we may have misclassified some co-infected individuals. This misclassification is likely, given the high prevalence rate of other STIs in the HIV-infected population [17]. Such misclassification could bias our estimates of the effect of STI on HIV viral load downwards.
Our study focused on whether STIs could interfere with viral suppression, and we therefore excluded HIV VL measurement done within 30 days of ART initiation. It seems likely that the effects of STIs on HIV viral load early in treatment are comparable to the effects before treatment begins and decline gradually through time, in an STI-specific fashion. We did not find any studies that could provide evidence bearing directly on the effect of STIs when ART has been initiated recently.
Adherence to ART was rarely reported or measured in the studies we used. Since the effect of STI co-infection on viral load would be stronger in people with poorly controlled viral loads, this effect is likely to bias our result. This bias will be exacerbated if co-infected individuals exhibit lower adherence (or could be reduced, or even reversed, if they are more likely to adhere, perhaps due to symptoms from the other STIs).
Most HIV viral load observations included in this meta-analysis were measured in blood plasma, not in genital secretions, which may limit the interpretation of our effect size to actual sexual transmission risk. Indeed, while plasma and genital HIV viral loads are correlated [44], evidences of HIV compartmentalization in some treated patients where viral loads as measured in genital secretions remain compatible with a non-negligible risk of transmission despite very low blood plasma viral loads [37, 45, 46].
We did not estimate gender-specific effects to avoid further complicating our model. It is possible that gender confounds our results to some extent. We note, however, that such confounding would be limited to blood measurements, since gender is implicitly accounted for in the other anatomical sites studied. Also, our estimate did not include a potential effect of menstrual cycle on genital HIV viral load, but we note that a recent study did not observe such effect [47].
If STIs were indeed an escape route for treatment as prevention, one could argue this should have shown up during large trials studying transmission rate among HIV discordant couples (for example [5]). But such trials do not provide complete reassurance, since trial participants are given STI monitoring and treatment not available to the general population.
The number of HIV-infected individuals receiving ART has dramatically increased during the last 10 years—from less than half a million in 2003 to about 13 million in 2013—and will increase further [18, 48]. The extended life expectancy associated with ART and the potentially higher exposure to STIs of the HIV-infected population may increase the prevalence of STI co-infections, particularly with public awareness of the decreased infectiousness of HIV while on ART and a potentially consequential decrease in condom usage. Hence, understanding the effects of such co-infections on HIV sexual transmission is an important public health issue.
Our study provides some insights into whether STI co-infections can undercut treatment as prevention efforts. Pooling available data, we estimate the degree to which STI co-infection may increase or decrease HIV shedding among treated individuals. We found a 95 % upper bound corresponding to a 0.83 log10 increase, which suggests that elevation of viral load by STI co-infections is unlikely to have a major impact on the ability of ART to reduce of HIV sexual transmission from patients on effective ART (as opposed to what could be observed in populations not on ART).
It is important to note that our results do not undercut the importance of control and treatment of STIs, not only for the well-being of infected individuals, but also for reducing HIV sexual transmission at the whole population level, which still has a majority of HIV infected individuals not on effective ART [18].
We did not have sufficient data to single out the effect of a specific STI on HIV viral load at a given anatomical site. Given the heterogeneous effect of STIs on HIV infectiousness, our analysis may have failed to identify epidemiologically relevant effects of particular STIs.
Hence, an important finding of our systematic review is that there is a paucity of available data with a sufficient level of detail to ascertain the effects of STI co-infection on the risk of HIV sexual transmission risk for individuals on ART. Future studies considering either transmission rate or HIV viral load may wish to consider the following suggestions: (i) given the possible high prevalence of co-infections among HIV-infected individuals, a broadest spectrum of relevant STIs should be tested; for transmission studies, testing should be performed frequently in both partners; (ii) HIV viral load should be measured in genital/rectal secretions, not blood plasma only; (iii) ART regimens and adherence should be reported, ideally at the patient level. We recognize that these suggestions may not always be practical, but when they can be followed they will help clarify the potentially important effects of STI-coinfection on the risk of HIV sexual transmission.
Conclusions
Our findings suggest that, on average, ART maintains its effectiveness at controlling HIV viral load during STI co-infections. However, with currently available data, we cannot rule out the possibility that certain STI co-infections have a larger effect. More high-quality studies specifically aimed at investigating the impact of STI co-infection on HIV sexual transmission from individuals on ART are needed.
Acknowledgments
We are very grateful to the original investigators who spent time and efforts to retrieve additional data that greatly improved the quality of this meta-analysis and particularly to Sophie Grabar, Joseph Politch, Colleen Kelley, Allison Delong, John T Brooks, Lois Conley, Tim Bush, Rafael Adolf, Ruth Deya, Kaveh Manavi, Susan Graham, Andrea Low, Kate Buchacz, Beverly Sha, Kristian Kofoed. We would also like to thank the librarians at the Health and Science Library in McMaster University for their help with the search strategies; Ben Bolker and Steve Walker for statistical advices.
Funding
James S. McDonnell Foundation, the Canadian Institutes of Health Research, the Canadian Natural Sciences and Engineering Research Council, National Institute of General Medical Sciences (Models of Infectious Disease Agent Study).
Additional files
PRISMA check list.
A protocol was prospectively registered in the PROSPERO database and is available at the following link: http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42013006056.
STI positivity definitions.
Searches strategies.
Statistical model.
Figures summarizing meta-analysis data.
Sensitivity analysis.
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
Conceived the study: DC and JD. Designed the study: DC, JD, SB, WD, MS. Searched the scientific literature: DC, CFS, SH. Statistical analysis: DC and JD. Drafted the report: DC and JD. Interpretation, revisions to the draft report and approval of final manuscript: all co-authors.
References
- 1.Baggaley RF, White RG, Hollingsworth TD, Boily M-C. Heterosexual HIV-1 infectiousness and antiretroviral Use:systematic review of prospective studies of discordant couples. Epidemiology. 2013;24:110–21. doi: 10.1097/EDE.0b013e318276cad7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Loutfy MR, Wu W, Letchumanan M, et al. Systematic review of HIV transmission between heterosexual serodiscordant couples where the HIV-positive partner is fully suppressed on antiretroviral therapy. PLoS One. 2013;8 doi: 10.1371/journal.pone.0055747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Attia S, Egger M, Müller M, Zwahlen M, Low N. Sexual transmission of HIV according to viral load and antiretroviral therapy: systematic review and meta-analysis. AIDS. 2009;23:1397–404. doi: 10.1097/QAD.0b013e32832b7dca. [DOI] [PubMed] [Google Scholar]
- 4.Reynolds SJ, Makumbi F, Nakigozi G, et al. HIV-1 transmission among HIV-1 discordant couples before and after the introduction of antiretroviral therapy. AIDS. 2011;25:473–7. doi: 10.1097/QAD.0b013e3283437c2b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cohen MS, Chen YQ, McCauley M, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365:493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Anglemyer A, Rutherford GW, Horvath T, Baggaley RC, Egger M, Siegfried N. The Cochrane Collaboration. 2012. Antiretroviral therapy for prevention of HIV transmission in HIV-discordant couples (Review) pp. 1–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Granich RM, Gilks CF, Dye C, De Cock KM, Williams BG. Universal voluntary HIV testing with immediate antiretroviral therapy as a strategy for elimination of HIV transmission: a mathematical model. Lancet. 2009;373:48–57. doi: 10.1016/S0140-6736(08)61697-9. [DOI] [PubMed] [Google Scholar]
- 8.Vernazza PL, Hirschelb B, Bernasconic E, Fleppd M. Les personnes séropositives ne souffrant d’aucune autre MST et suivant un traitement antirétroviral efficace ne transmettent pas le VIH par voie sexuelle. Bulletin des médecins suisses| Schweizerische Ärztezeitung| Bollettino dei medici svizzeri. 2008;89:5. [Google Scholar]
- 9.Johnson LF, Lewis DA. The effect of genital tract infections on HIV-1 shedding in the genital tract: a systematic review and meta-analysis. Sex Transm Dis. 2008;35:946–59. doi: 10.1097/OLQ.0b013e3181812d15. [DOI] [PubMed] [Google Scholar]
- 10.Winter AJ, Taylor S, Workman J, et al. Asymptomatic urethritis and detection of HIV-1 RNA in seminal plasma. Genitourin Med. 1999;75:261–3. doi: 10.1136/sti.75.4.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Røttingen J-A, Cameron DW, Garnett GP. A systematic review of the epidemiologic interactions between classic sexually transmitted diseases and HIV: how much really is known? Sex Transm Dis. 2001;28:579–97. doi: 10.1097/00007435-200110000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Chan DJ, McNally L, Batterham M, Smith DE. Relationship between HIV-RNA load in blood and semen in antiretroviral-naïve and experienced men and effect of asymptomatic sexually transmissible infections. Curr HIV Res. 2008;6:138–42. doi: 10.2174/157016208783885074. [DOI] [PubMed] [Google Scholar]
- 13.Boily M-C, Baggaley RF, Wang L, et al. Heterosexual risk of HIV-1 infection per sexual act: systematic review and meta-analysis of observational studies. Lancet Infect Dis. 2009;9:118–29. doi: 10.1016/S1473-3099(09)70021-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rotchford K, Strum WA, Wilkinson D. Effect of coinfection with STDs and of STD treatment on HIV shedding in genital-tract secretions: systematic review and data synthesis. Sex Transm Dis. 2000;27:243–8. doi: 10.1097/00007435-200005000-00001. [DOI] [PubMed] [Google Scholar]
- 15.Naresh A, Beigi R, Woc-Colburn L, Salata RA. The bidirectional interactions of human immunodeficiency virus-1 and sexually transmitted infections: a review. Infect Dis Clin Pract. 2009;17:362–73. doi: 10.1097/IPC.0b013e3181aba461. [DOI] [Google Scholar]
- 16.Galvin SR, Cohen MS. The role of sexually transmitted diseases in HIV transmission. Nat Rev Micro. 2004;2:33–42. doi: 10.1038/nrmicro794. [DOI] [PubMed] [Google Scholar]
- 17.Kalichman SC, Pellowski J, Turner C. Prevalence of sexually transmitted co-infections in people living with HIV/AIDS: systematic review with implications for using HIV treatments for prevention. Sex Transm Infect. 2011;87:183–90. doi: 10.1136/sti.2010.047514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.The GAP report. Geneva: UNAIDS; 2014.
- 19.Taylor S, Davies S. Antiretroviral drug concentrations in the male and female genital tract: implications for the sexual transmission of HIV. Curr Opin HIV AIDS. 2010;5:335–43. doi: 10.1097/COH.0b013e32833a0b69. [DOI] [PubMed] [Google Scholar]
- 20.Anderson BL, Cu-Uvin S. Determinants of HIV shedding in the lower genital tract of women. Curr Infect Dis Rep. 2008;10:505–11. doi: 10.1007/s11908-008-0082-z. [DOI] [PubMed] [Google Scholar]
- 21.Pasquier C, Andreutti C, Bertrand E, et al. Multicenter assessment of HIV-1 RNA quantitation in semen in the CREAThE network. J Med Virol. 2011;84:183–7. doi: 10.1002/jmv.23194. [DOI] [PubMed] [Google Scholar]
- 22.Iglesias-Ussel MD, Romerio F. HIV reservoirs: the new frontier. AIDS Rev. 2011;13:13–29. [PubMed] [Google Scholar]
- 23.Lee PK. HIV-1 viral load blips are of limited clinical significance. J Antimicrob Chemother. 2006;57:803–5. doi: 10.1093/jac/dkl092. [DOI] [PubMed] [Google Scholar]
- 24.Moher D, Liberati A, Tetzlaff J, Altman DG. The PRISMA Group (2009) Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 6(7): e1000097. doi:10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed]
- 25.Sutton AJ, Abrams KR. Bayesian methods in meta-analysis and evidence synthesis. Stat Methods Med Res. 2001;10:277–303. doi: 10.1191/096228001678227794. [DOI] [PubMed] [Google Scholar]
- 26.Cu-Uvin S, Hogan JW, Caliendo AM, Harwell J, Mayer KH, Carpenter CC. Association between bacterial vaginosis and expression of human immunodeficiency virus type 1 RNA in the female genital tract. Clin Infect Dis. 2001;33:894–6. doi: 10.1086/322613. [DOI] [PubMed] [Google Scholar]
- 27.Dominici F, Parmigiani G. Combining studies with continuous and dichotomous responses: a latent-variables approach. In: Stangl DK, Berry DA, editors. Meta-analysis in medicine and health policy. New-York: Marcel Dekker; 2000. [Google Scholar]
- 28.Gelman A, Carlin JB, Stern HS, Dunson DB, Vehtari A, Rubin DB. Bayesian data analysis, Third Edition. Boca Raton, Florida: CRC Press; 2013.
- 29.R Core Team. R: a language and environment for statistical computing. R Foundation for Statistical Computing. http://www.R-project.org/.
- 30.Stan Development Team . Stan: A C++ library for probability and sampling,version 2.2. 2014. [Google Scholar]
- 31.Adolf R, Bercht F, Aronis ML, Lunardi LW, Schechter M, Sprinz E. Prevalence and risk factors associated with syphilis in a cohort of HIV positive individuals in Brazil. AIDS Care. 2011;24:(2)1-7. [DOI] [PubMed]
- 32.Anderson BL, Wang CC, DeLong AK, et al. Genital tract leukocytes and shedding of genital HIV Type 1 RNA. Clin Infect Dis. 2008;47:1216–21. doi: 10.1086/592303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Conley L, Bush T, Darragh TM, et al. Factors associated with prevalent abnormal anal cytology in a large cohort of HIV-infected adults in the United States. J Infect Dis. 2010;202:1567–76. doi: 10.1086/656775. [DOI] [PubMed] [Google Scholar]
- 34.Graham SM, Masese L, Gitau R, et al. Genital ulceration does not increase HIV-1 shedding in cervical or vaginal secretions of women taking antiretroviral therapy. Sex Transm Infect. 2011;87:114–7. doi: 10.1136/sti.2010.045369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jarzebowski W. Effect of early syphilis infection on plasma viral load and CD4 cell count in human immunodeficiency virus–Infected men. Arch Intern Med. 2012;172:1237. doi: 10.1001/archinternmed.2012.2706. [DOI] [PubMed] [Google Scholar]
- 36.Kofoed K, Gerstoft J, Mathiesen LR, Benfield T. Syphilis and Human Immunodeficiency Virus (HIV)-1 Coinfection: influence on CD4 T-cell count, HIV-1 viral load, and treatment response. Sex Transm Dis. 2006;33:143–8. doi: 10.1097/01.olq.0000187262.56820.c0. [DOI] [PubMed] [Google Scholar]
- 37.Politch JA, Mayer KH, Welles SL, et al. Highly active antiretroviral therapy does not completely suppress HIV in semen of sexually active HIV-infected men who have sex with men. AIDS. 2012;26:1535–43. doi: 10.1097/QAD.0b013e328353b11b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sadiq ST, Taylor S, Kaye S, et al. The effects of antiretroviral therapy on HIV-1 RNA loads in seminal plasma in HIV-positive patients with and without urethritis. AIDS. 2002;16:219–25. doi: 10.1097/00002030-200201250-00011. [DOI] [PubMed] [Google Scholar]
- 39.Sha BE, Zariffard MR, Wang QJ, et al. Female genital-tract HIV load correlates inversely with Lactobacillus species but positively with bacterial vaginosis and Mycoplasma hominis. J Infect Dis. 2005;191:25–32. doi: 10.1086/426394. [DOI] [PubMed] [Google Scholar]
- 40.Sudenga SL, Kempf M-C, McGwin G, Jr, Wilson CM, Hook EW, III, Shrestha S. Incidence, prevalence, and epidemiology of herpes simplex virus-2 in HIV-1-Positive and HIV-1-Negative adolescents. Sex Transm Dis. 2012;39:300–5. doi: 10.1097/OLQ.0b013e318244a90f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Madeddu G, Mameli G, Capobianco G, et al. HPV infection in HIV-positive females: the need for cervical cancer screening including HPV-DNA detection despite successful HAART. Eur Rev Med Pharmacol Sci. 2014;18:1277–85. [PubMed] [Google Scholar]
- 42.T Blackard J. HIV compartmentalization: a review on a clinically important phenomenon. Curr HIV Res. 2012;10:133–42. doi: 10.2174/157016212799937245. [DOI] [PubMed] [Google Scholar]
- 43.Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 44.Baeten JM, Kahle EM, et al. Genital HIV-1 RNA predicts risk of heterosexual HIV-1 transmission. Sci Transl Med. 2011;3:77ra29–9. doi: 10.1126/scitranslmed.3001888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lambert-Niclot S, Tubiana R, Beaudoux C, et al. Detection of HIV-1 RNA in seminal plasma samples from treated patients with undetectable HIV-1 RNA in blood plasma on a 2002–2011 survey. AIDS. 2012;26:971–5. doi: 10.1097/QAD.0b013e328352ae09. [DOI] [PubMed] [Google Scholar]
- 46.Graham SM, Holte SE, Peshu NM, et al. Initiation of antiretroviral therapy leads to a rapid decline in cervical and vaginal HIV-1 shedding. AIDS. 2007;21:501–7. doi: 10.1097/QAD.0b013e32801424bd. [DOI] [PubMed] [Google Scholar]
- 47.Sheth AN, Evans-Strickfaden T, Haaland R, et al. HIV-1 genital shedding is suppressed in the setting of high genital antiretroviral drug concentrations throughout the menstrual cycle. J Infect Dis. 2014;210:736–44. doi: 10.1093/infdis/jiu166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.UNAIDS . Treatment 2015. UNAIDS report. 2013. pp. 1–44. [Google Scholar]


