Abstract
Background:
There is limited research related to spinal manipulation of uncomplicated thoracic spine pain and even less when pain is associated with comorbid conditions such as rheumatoid arthritis. In the absence of trial evidence, clinical experience and appropriate selection of the type of intervention is important to informing the appropriate management of these cases.
Case presentation:
We present a case of a patient with long standing rheumatoid arthritis who presented with acute thoracic pain. The patient was diagnosed with costovertebral joint dysfunction and a myofascial strain of the surrounding musculature. The patient was unresponsive to treatment involving a generalized manipulative technique; however, improved following the administration of a specific applied manipulation with modified forces. The patient was deemed recovered and discharged with ergonomic and home care recommendations.
Discussion:
This case demonstrates a clinical situation where there is a paucity of research to guide management, thus clinicians must rely on experience and patient preferences in the selection of an appropriate and safe therapeutic intervention. The case highlights the need to contextualize the apparent contraindication of manipulation in patients with rheumatoid arthritis and calls for further research. Finally the paper advances evidence based decision making that balances the available research, clinical experience, as well as patient preferences.
Keywords: Rheumatoid arthritis, manipulation, mobilization, chiropractic
Abstract
Historique :
Il existe peu d’études sur la manipulation vertébrale de douleur de la colonne dorsale sans complication, et encore moins lorsque la douleur est associée à des conditions comorbides comme la polyarthrite rhumatoïde. En l’absence de résultats d’essais cliniques, l’expérience clinique et le choix approprié du type d’intervention sont importants pour trouver la gestion appropriée de ces cas.
Présentation de cas :
Nous présentons le cas d’un patient souffrant de polyarthrite rhumatoïde de longue date avec une douleur thoracique aiguë. Le patient a reçu un diagnostic de dysfonctionnement de l’articulation costo-vertébrale et une tension myofasciale de la masse musculaire qui l’enveloppe. Le patient ne répondait pas au traitement comprenant une technique de manipulation généralisée; cependant, il a démontré une amélioration à la suite de l’administration d’une manipulation spécifique avec des forces modifiées. Le patient a été jugé rétabli et a obtenu son congé avec des recommandations de soins ergonomiques et à domicile.
Discussion :
Ce cas illustre une situation clinique où il y a n’y a pas assez d’études permettant d’orienter la gestion; par conséquent, les cliniciens doivent s’appuyer sur l’expérience et les préférences du patient pour choisir une intervention de traitement appropriée et sécuritaire. Ce cas souligne le besoin de contextualiser la contre-indication apparente de la manipulation chez les patients avec de l’arthrite rhumatoïde et le besoin de recherche supplémentaire. Finalement, l’étude préconise un processus décisionnel fondé sur des preuves qui équilibrent les études consultables, l’expérience en clinique et les préférences du patient.
Keywords: arthrite rhumatoïde, manipulation, mobilisation, chiropratique
Background
Rheumatoid arthritis (RA) is a seronegative spondyloarthropathy that usually presents in females between the ages of 45 and 65.1 The disease can lead to disability and significantly diminish quality of life by affecting a patient’s physical, emotional and social functioning.2,3 Treatment commonly involves a pharmacologic approach, including such drugs as non-steroidal anti-inflammatories (NSAIDS), anti-tumor necrosis factors, disease modifying anti-rheumatics and/or corticosteroids.4 Non-pharmacologic management includes a vast array of interventions including manual therapies; however, there is limited scientific evidence to inform their use.
This case report demonstrates the utilization of spinal manipulative therapy (SMT) otherwise referred to as high velocity, low amplitude (HVLA) manipulation in the treatment of thoracic spine pain in a patient with RA. It also discusses the need for further research on the use and benefit of manual therapies, in particular manipulation, in the management of patients with RA.
Case presentation
History
A 66 year old female presented with a new complaint of left-sided mid-thoracic pain that radiated anteriorly to her lower chest and upper abdomen. The onset was attributed to lifting a 2kg bag of baking flour from the floor onto a 91 centimetre high counter. The pain was reported to be a constant dull ache, which became intensely sharp upon aggravation. Aggravating factors included extension and rotation movements of the spine, holding objects with her left arm outstretched, and coughing. Relieving factors included resting and taking over-the-counter pain medications along with an NSAID (i.e. naproxen). Associated symptoms included abdominal discomfort and nausea which she attributed to the commencement of her taking the medications.
She reported a history of neck, back and extremity joint pains which she associated to her rheumatoid arthritis (RA) (diagnosed at 18 years of age). Her RA was being managed pharmacologically with methotrexate but previously included gold injections, choloroquine and prednisone; however, she reported increasing intolerance to the medication. Other relieving factors for her pains included chiropractic treatments which consisted of spinal manipulation and mobilization, physical therapy modalities and soft tissue therapies. She had surgical excision of nodules in her feet and hands about 15 and 3 years ago, respectively. Aside from being hypertensive, she reported no other health problems.
Examination
On examination, she was able to ambulate and assume sitting positions without guarding. Blood pressure was 130/80. She had bilateral ulnar deviation with multiple Heberden’s and Bouchard’s nodes in the distal and proximal interphalangeal joints, respectively. The tender joint count was 20 and swollen joint count was 7. The active ranges of motion of her thoracic spine were mildly limited (20–25%) by pain in all directions. Deep breathing and coughing localized the sharp pain to the area of complaint. Global lateral and anteroposterior compression of the entire rib cage did not reproduce any local or radiating discomfort. Palpation of her thoracic spine revealed tenderness with restricted joint movement from T5–T7, as well as the left 6 and 7 costovertebral joints. The left intercostal space between rib 6 and 7 and the paraspinal musculature (rhomboids major, spinalis thoracis, longissimus thoracis, iliocostalis thoracis, multifidus thoracis) from T4 to the iliac crest were tender to palpation with increased myofascial tension, especially on the left.
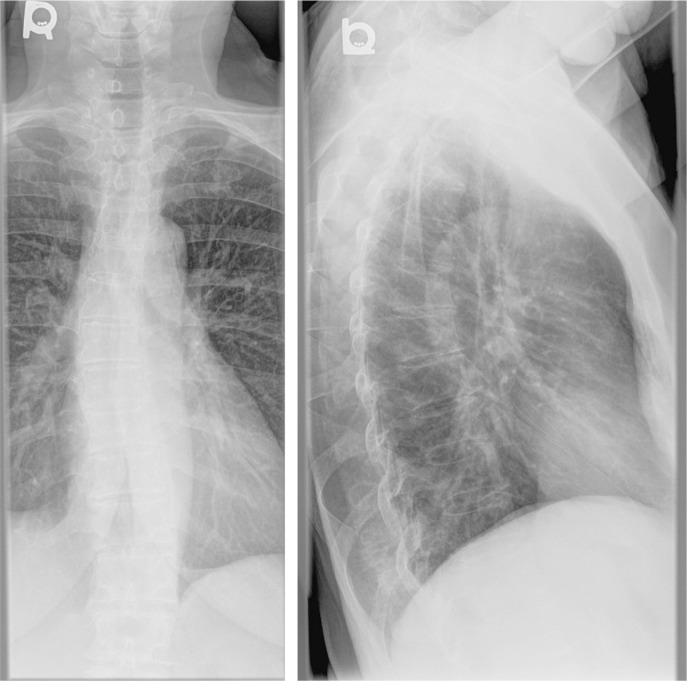
Radiographic studies indicated moderate osteopenia, mild degenerative disc disease from T4–T9, mild uncovertebral arthrosis at C5–C6 and a mild s-shaped thoracolumbar curve (<15 ° Cobb angle) (See Figure 1).
Figure 1A and 1B:
Anterior-posterior (A) and lateral thoracic (B) spine radiographs.
Management
The patient was diagnosed with acute costovertebral joint dysfunction of the 6th and 7th ribs with associated myofascial strain. Differential diagnoses included reactive synovitis, a rib fracture, a sprain/strain, or gastritis. Due to the concerns of an underlying active RA and abdominal pain, she was requested to see her physician for co-management.
She received 4 treatments over the next 7 days. The first 2 treatments were provided by an associate chiropractor who performed soft tissue therapy and interferential current to control her pain, along with SMT in a postero-anterior direction to the mid thoracic spine. The patient was placed in a prone position while the chiropractor performed a prone, cross bilateral manipulation with thenar contact to double transverse processes of the thoracic spine. This procedure is described as a soft thenar contact over the area of the transverse process and application of a high velocity low amplitude body drop procedure as described by Byfield.5 The patient was advised to continue her daily walking and to rest intermittently as needed. She was also instructed to use cryotherapy for general pain control. After the second visit, the patient reported minimal and temporary relief. Furthermore, she reported that the cryotherapy aggravated her coughing symptoms and hence her mid-thoracic pain.
On the third visit, the plan of management was reviewed due to the minimal response to therapy. The diagnosis of costovertebral dysfunction was revisited and the next two treatments were delivered by her primary chiropractor who focused the manipulation to the hypomobile costovertebral joints. The manipulative technique was modified to a supine, single spinous supine thoracic manipulation utilising a soft thenar contact inferior to the restricted spinal segments of T5–T7 about the area of the costovertebral joints of the 6th and 7th ribs as described Byfield.5 With the patient supine and her arms folded across her chest, a minimal short lever, body drop procedure was used while modulating the depth (low amplitude) and speed (low velocity) of the thrust to the patient’s tolerance (See Figure 2). This procedure was most comfortable to the patient, resulting in an audible joint cavitation with significant immediate pain relief. She was instructed to avoid lifting but assume her normal activities of daily living.
Figure 2:
Thenar eminence contact position for anterior thoracic spinal manipulation
She returned two days later reporting that the same original sharp pain in her thoracic spine had returned after having a “rough night” that she attributed to all-day gardening a day earlier. As in the third visit, treatment was directed to the costovertebral joint using SMT as per the third visit and the surrounding musculature with myofascial release therapy. Once again, she had immediate relief which was sustained over time. Her abdominal pain subsided upon her cessation of her taking naproxen. The patient was discharged with ergonomic advice and exercises, and managed collaboratively as necessary. There were no reported changes to her medications subsequent to her visiting her family physician.
Discussion
This case illustrates how management of thoracic pain may be complicated in a patient with co-existent underlying conditions. Clinicians are often faced with this dilemma as the typical plan of management or interventions utilized need to be evaluated with an emphasis on the potential changes to risks and benefits which may be altered based on the individual characteristics of each patient. The patient in this case had a history of RA and presented with what was considered to be a recurrent episode of acute mechanical thoracic pain.
Literature suggests a limited role for manipulative therapy in managing the inflammatory component of RA6, yet it may provide symptomatic pain relief of mechanical origin caused by abnormal compensatory kinematics (of non-inflammatory origin). Shaikh suggests that clinicians differentiate inflammatory back pain from mechanical back pain during the clinical history.7 Inflammatory back pain typically presents as morning stiffness greater than 30 minutes, relief of pain with exercise but not rest, pain may be present at night which wakes the individual, and alternating buttock pain.7 However, the available scientific evidence is limited in guiding clinicians in differentiating between inflammatory and non-inflammatory pain when they may both be present and furthermore in the management of these cases.
The general consensus is that management of patients with RA includes a multidisciplinary approach incorporating both pharmacologic and non-pharmacologic interventions.8,9 In regard to non-pharmacologic interventions, dynamic exercises have been shown to be beneficial in improving aerobic capacity and muscle strength without detrimental effects on disease activity.10 Education has been shown to increase self efficacy, knowledge of disease management and decrease morning stiffness.11 Physical therapy modalities (e.g. interferential current) have been reported to potentially facilitate pain modulation but their effectiveness is inconclusive.12 While orthoses and assistive devices have been shown to decrease the swelling and pain of RA, they may limit dexterity and function when performing activities of daily living.13
As for manual therapy, recent guidelines recommend mobilizations but the level of evidence is that of expert opinion.14 Mobilizations involve positioning a joint at its restrictive barrier (i.e. end of passive range of motion) and then the practitioner uses a series of gentle, repetitive movements towards and through the restriction.15 Manipulation, commonly referred to as “an adjustment” by chiropractors, is another form of manual therapy which involves a joint positioned at its restrictive barrier and then the practitioner applies a quick, short impulse (HVLA) thrust.16 Both procedures are typically directed at hypomobile joints.
Hypomobile vertebral segments have been thought to result from “adhesions” within the zygapophysial joints.17 This hypomobility or aberrant joint motion is thought to be amenable to manipulation.18 Cramer et al. have suggested that spinal manipulation increases the gapping of vertebral joints compared to controls, presumably facilitating the breaking of these adhesions and improving joint kinematics.19 Considering the potential for alterations in joint kinematics and subsequent pain generation from compensatory mechanisms, as well as the inherent joint changes in rheumatologic patients, manipulative therapy may be a viable therapeutic option.
Alternatively, others have suggested a more neurophysiological theoretical framework to explain how spinal manipulation may modulate pain and movement. These include spinal reflex excitability20, decreased electromyographic activity of paraspinal muscles21,22, motor-neuron excitability23, strength modulation24,25, reflex inhibition of pain by stimulation of joint mechanoreceptors26, activation of endogenous opioids27, altering chemical mediators28, and activating segmental inhibitory pathways or descending pain inhibitory systems29,30. Hence manipulation may have mechanistic and neurophysiologic effects that should be considered when justifying its use.
Empirically, the use of manipulation is limited to non-inflammatory regions, and joints susceptible to inflammatory pathology are avoided. The World Health Organization reported that joint manipulation in patients with RA is an absolute contraindication in anatomical regions of involvement.31 For example, cervical spine manipulation in patients with RA is considered an absolute contraindication due to instability of the atlanto-axial joint and predisposition to transverse ligament rupture.32 It appears the utilization of the term “absolute” in patients with RA may have been generalized to all joints rather than being restricted to joints where risks associated with manipulation outweighs the potential benefits.
The thoracic spine has not been researched as much as the cervical and lumbar spine when considering manipulative therapy.15 The case described was that of a patient with RA and co-existent thoracic pain. Manipulation to the thoracic spine appears to be effective at restoring joint mechanics and the recovery of thoracic range of motion immediately after treatment.18 Treatment of this region also requires a more cautious approach due to the presence of numerous joints, the thoracic cage, autonomic ganglia, and the passage of the neurovascular bundle in the thoracic outlet.33 Thus training and experience may be important in modulating the selected manipulative procedure.34
Bergmann35 reported that manipulation requires a controlled delivery of the HVLA thrust that is developed with extensive training to perfect the psychomotor skills. Such training develops the palpatory sense and control to enable delivery of a thrust of appropriate depth and force and that has been postulated to be more effective compared to those with less training.34
Additionally, timing of delivery of therapeutic interventions such as manipulation needs to be considered in patients with RA. The unpredictable pattern of changing symptoms in rheumatologic patients can differ day to day.4 Thus, the patient’s symptoms need to be evaluated on each visit to ensure that the appropriate management options are being provided.
During episodes of acute pain, clinicians are faced with the challenge of sifting through the many grey areas of evidence which also includes clinical experience and patient values.36 Patient preferences are a component of patient value that should be integrated into clinical decision-making.37 In this case, the patient presented with RA and a history of adverse reactions to medications. She also reported a preference for alternative therapies for pain relief especially in light of prior benefit. In situations where a patient is seeking care for a therapy with limited evidence, clinical expertise becomes invaluable. In consideration of the patient’s pre-existing condition and the rationale for conservative care, clinical experience guided the selection of an appropriate procedure and the applied force and location of intervention were modified to the patient’s tolerance and preference.
Finally, co-management of the patient’s pain was achieved with appropriate communication with the patients’ family physician and rheumatologist to address the multiple factors that were contributing to the patient’s symptoms.
Summary
The authors acknowledge the limitation of case reports in the evidence hierarchy. However to our knowledge, this is the first report of a rheumatoid patient receiving manipulation in the management of her acute symptomatic thoracic spine pain. The patient reported to have experienced significant and immediate pain relief from the procedure performed in the 3rd and 4th visit. Manipulative therapy was limited to pain relief, while the patient also received ergonomic education and active exercises. This case report is meant to stimulate increased research in this field, question the generalization of contraindications without adequate evidence, and provide a basis for further investigation.
Figure 3:
Anterior thoracic spinal manipulative procedure
References
- 1.Stenstrom CH, Minor MA. Evidence for the benefit of aerobic and strengthening exercise in rheumatoid arthritis. Arthritis Rheum. 2003;49:428–434. doi: 10.1002/art.11051. [DOI] [PubMed] [Google Scholar]
- 2.Scott DL, Smith C, Kingsley G. What are the consequences of early rheumatoid arthritis for the individual? Best Pract Res Clin Rheumatol. 2005;19:117–136. doi: 10.1016/j.berh.2004.08.007. [DOI] [PubMed] [Google Scholar]
- 3.Combe B. Early rheumatoid arthritis: strategies for prevention and management. Best Pract Res Clin Rheumatol. 2007;21:27–42. doi: 10.1016/j.berh.2006.08.011. [DOI] [PubMed] [Google Scholar]
- 4.Home D, Carr M. Rheumatoid arthritis: the role of early intervention and self-management. Br J Community Nursing. 2009;14:432–436. doi: 10.12968/bjcn.2009.14.10.44495. [DOI] [PubMed] [Google Scholar]
- 5.Byfield D. Thoracic Spine Adjustive and Manipulative Techniques. In: Elsevier Byfield D., editor. Technique Skills in Chiropractic. Churchill Livingstone; 2012. pp. 241–278. [Google Scholar]
- 6.Droz-Georget JH. Aspects of Manipulative Therapy. Lincoln Institute of Heath Sciences; 1980. High velocity thrust and pathophysiology of segmental dysfunction; pp. 81–87. [Google Scholar]
- 7.Shaikh SA. Ankylosing spondylitis: recent breakthroughs in diagnosis and treatment. J Can Chiropr Assoc. 2007;51:249–260. [PMC free article] [PubMed] [Google Scholar]
- 8.Luqmani R, Hennell S, Estrach C, Birrell F, Bosworth A, Davenport G, Fokke C, Goodson N, Jeffreson P, Lamb E, et al. Br Soc Rheum and Br Health Professionals in Rheumatology guideline for the management of rheumatoid arthritis (the first two years) Rheumatology (Oxford) 2006;45:1167–1169. doi: 10.1093/rheumatology/kel215a. [DOI] [PubMed] [Google Scholar]
- 9.Hennell S, Luqmani R. Developing multidisciplinary guidelines for the management of early rheumatoid arthritis. Musculoskeletal Care. 2008;6:97–107. doi: 10.1002/msc.117. [DOI] [PubMed] [Google Scholar]
- 10.Gaudin P, Leguen-Guegan S, Allenet B, Baillet A, Grange L, Juvin R. Is dynamic exercise beneficial in patients with rheumatoid arthritis? Joint Bone Spine. 2008;75:11–17. doi: 10.1016/j.jbspin.2007.04.015. [DOI] [PubMed] [Google Scholar]
- 11.Lineker SC, Bell MJ, Wilkins AL, Badley EM. Improvements following short term home based physical therapy are maintained at one year in people with moderate to severe rheumatoid arthritis. J Rheumatol. 2001;28:165–168. [PubMed] [Google Scholar]
- 12.Brosseau L, Judd MG, Marchand S, Robinson VA, Tugwell P, Wells G, Yonge K. Transcutaneous electrical nerve stimulation (TENS) for the treatment of rheumatoid arthritis in the hand. Cochrane Database Syst Rev. 2003:CD004377. doi: 10.1002/14651858.CD004377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Egan M, Brosseau L, Farmer M, Ouimet MA, Rees S, Wells G, Tugwell P. Splints/orthoses in the treatment of rheumatoid arthritis. Cochrane Database Syst Rev. 2003:CD004018. doi: 10.1002/14651858.CD004018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Forestier R, André-Vert J, Guillez P, Coudeyre E, Lefevre-Colau MM, Combe B, Mayoux-Benhamou MA. Non-drug treatment (excluding surgery) in rheumatoid arthritis: clinical practice guidelines. Joint Bone Spine: Revue Du Rhumatisme. 2009;76:691–698. doi: 10.1016/j.jbspin.2009.01.017. [DOI] [PubMed] [Google Scholar]
- 15.Atchison JW. Manipulation efficacy: upper body. J Back Musculo Rehabil. 2000;15:3–15. doi: 10.3233/bmr-2000-15102. [DOI] [PubMed] [Google Scholar]
- 16.Bergmann TF. High-velocity Low-amplitude Manipulative Techniques. In: Haldeman S, Dagenais S, Budgell B, Grunnet-Nilsson N, Hooper PD, Meeker WC, et al., editors. Principles and Practice of Chiropractic. 3rd edition. McGraw-Hill; 2005. pp. 755–766. [Google Scholar]
- 17.Mooney V, Robertson J. The facet syndrome. Clin Orthop Relat Res. 1976 Mar-Apr;(115):149–156. [PubMed] [Google Scholar]
- 18.Haas M, Panzer D, Peterson D, Raphael R. Short-term responsiveness of manual thoracic end-play assessment to spinal manipulation: a randomized controlled trial of construct validity. J Manipulative Physiol Ther. 1995;18:582–589. [PubMed] [Google Scholar]
- 19.Cramer GD, Tuck NR, Jr, Knudsen JT, Fonda SD, Schliesser JS, Fournier JT, Patel P. Effects of side-posture positioning and side-posture adjusting on the lumbar zygapophysial joints as evaluated by magnetic resonance imaging: a before and after study with randomization. J Manipulative Physiol Ther. 2000;23:380–394. doi: 10.1067/mmt.2000.108145. [DOI] [PubMed] [Google Scholar]
- 20.Dishman JD, Burke J. Spinal reflex excitability changes after cervical and lumbar spinal manipulation: a comparative study. Spine J. 2003;3:204–212. doi: 10.1016/s1529-9430(02)00587-9. [DOI] [PubMed] [Google Scholar]
- 21.DeVocht JW, Pickar JG, Wilder DG. Spinal manipulation alters electromyographic activity of paraspinal muscles: a descriptive study. J Manipulative Physiol Ther. 2005;28:465–471. doi: 10.1016/j.jmpt.2005.07.002. [DOI] [PubMed] [Google Scholar]
- 22.Lehman G. Kinesiological research: the use of surface electromyography for assessing the effects of spinal manipulation. J Electromyogr Kinesiol. 2012;22:692–696. doi: 10.1016/j.jelekin.2012.02.010. [DOI] [PubMed] [Google Scholar]
- 23.Pickar JG. Neurophysiological effects of spinal manipulation. Spine J. 2002;2:357–371. doi: 10.1016/s1529-9430(02)00400-x. [DOI] [PubMed] [Google Scholar]
- 24.Botelho MB, Andrade BB. Effect of cervical spine manipulative therapy on judo athletes’ grip strength. J Manipulative Physiol Ther. 2012;35:38–44. doi: 10.1016/j.jmpt.2011.09.005. [DOI] [PubMed] [Google Scholar]
- 25.Grindstaff TL, Hertel J, Beazell JR, Magrum EM, Ingersoll CD. Effects of lumbopelvic joint manipulation on quadriceps activation and strength in healthy individuals. Man Ther. 2009;14:415–420. doi: 10.1016/j.math.2008.06.005. [DOI] [PubMed] [Google Scholar]
- 26.Pickar JG. An in vivo preparation for investigating neural responses to controlled loading of a lumbar vertebra in the anesthetized cat. J Neurosci Methods. 1999;89:87–96. doi: 10.1016/s0165-0270(99)00060-6. [DOI] [PubMed] [Google Scholar]
- 27.Vernon HT, Dhami MS, Howley TP, Annett R. Spinal manipulation and beta-endorphin: a controlled study of the effect of a spinal manipulation on plasma beta-endorphin levels in normal males. J Manipulative Physiol Ther. 1986;9:115–123. [PubMed] [Google Scholar]
- 28.Sambajon VV, Cillo JE, Jr, Gassner RJ, Buckley MJ. The effects of mechanical strain on synovial fibroblasts. J Oral Maxillofac Surg. 2003;61:707–712. doi: 10.1053/joms.2003.50141. [DOI] [PubMed] [Google Scholar]
- 29.Haldeman S. Pain physiology as a neurological model for manipulation. Manual Medicine. 1981;19:5–11. [Google Scholar]
- 30.Wall PD. The dorsal horn. In: Wall PD, Malzack R, editors. Textbook of pain. 2nd edition. 2006. [Google Scholar]
- 31.Sweaney JA. WHO giudelines on basic training and safety in chiropractic. Geneva: 2005. [Google Scholar]
- 32.Dvorak J, Dvorak V, Gilliar W, Schneider W, Spring H, Tritschler T. Musculoskeletal Manual Medicine. Stuttgart: Thieme Publishing; 2008. [Google Scholar]
- 33.Vanti C, Ferrari S, Morsillo F, Tosarelli D, Pillastrini P. Manual therapy for non-specific thoracic pain in adults: Review of the literature. J Back Musculo Rehabil. 2008:43–152. [Google Scholar]
- 34.Triano JJ, Bougie J, Rogers C, Scaringe J, Sorrels K, Skogsbergh D, Mior S. Procedural skills in spinal manipulation: do prerequisites matter? Spine J. 2004;4:557–563. doi: 10.1016/j.spinee.2004.01.017. [DOI] [PubMed] [Google Scholar]
- 35.Principles and Practice of Chiropractic. McGraw-Hill; 2005. [Google Scholar]
- 36.Sackett DL, Rosenberg WM, Gray JA, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn’t. BMJ. 1996;312:71–72. doi: 10.1136/bmj.312.7023.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kelly AM. Evidence-based practice: an introduction and overview. Semin Roentgenol. 2009;44:131–139. doi: 10.1053/j.ro.2009.03.010. [DOI] [PubMed] [Google Scholar]