Abstract
The primary purpose of this case report is to outline the diagnosis, intervention and clinical outcome of a patient presenting with occipital neuralgia. Upon initial presentation, the patient described a four-year history of stabbing neck pain and headaches. After providing informed consent, the patient underwent a total of four dry needling (DN) sessions over a two-week duration. During each of the treatment sessions, needles were inserted into the trapezii and suboccipital muscles. Post-intervention, the patient reported a 32-point change in her neck disability index score along with a 28-point change in her headache disability index score. Thus, it appears that subsequent four sessions of DN over two weeks, our patient experienced meaningful improvement in her neck pain and headaches. To the best of our knowledge, this is the first case report describing DN to successfully improve clinical outcomes in a patient diagnosed with occipital neuralgia.
Keywords: dry needling, intramuscular stimulation, occipital neuralgia, headache, neck pain, chiropractic
Abstract
L’objectif principal de cet exposé de cas est de souligner le diagnostic, l’intervention et le résultat clinique d’un patient souffrant de névralgie cervico-occipitale. Lors de la présentation initiale, la patiente a décrit des antécédents de douleur aiguë dans le cou et de céphalées pendant quatre ans. Après avoir fourni le consentement éclairé, la patiente a subi un total de quatre séances de piqûres sèches sur une période de deux semaines. Au cours de chaque séance de traitement, des aiguilles lui ont été insérées dans le trapèze et les muscles sousoccipitaux. Après l’intervention, la patiente a signalé un changement de 32 points à l’index d’incapacité cervicale avec un changement de 28 points à l’index d’incapacité liée aux céphalées. Par conséquent, il semble qu’à la suite des quatre séances de piqûres sèches réparties sur deux semaines, notre patiente a connu une amélioration remarquable concernant ses douleurs cervicales et ses céphalées. À notre connaissance, il s’agit du premier exposé de cas décrivant des piqûres sèches qui améliorent avec succès les résultats cliniques chez un patient ayant reçu un diagnostic de névralgie cervico-occipitale.
Keywords: piqûres sèches, stimulation intramusculaire, névralgie cervico-occipitale, céphalée, douleur cervicale, chiropratique
Introduction
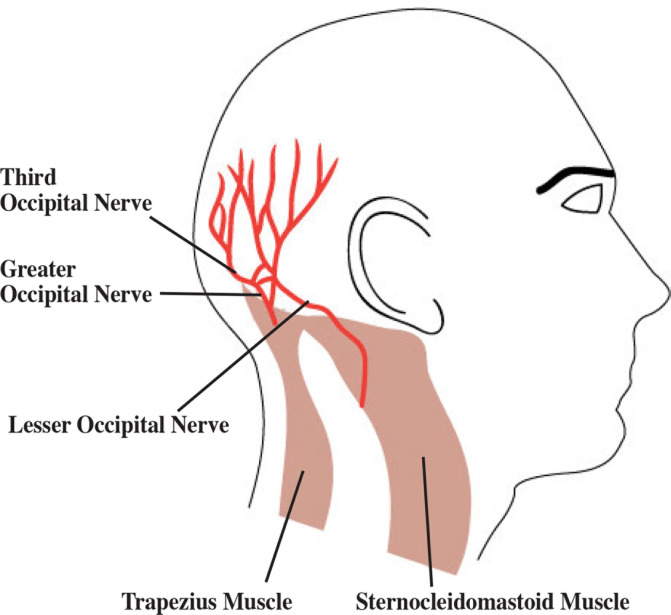
Occipital neuralgia is defined according to guidelines provided by the International Headache Society (IHS). Briefly, the IHS diagnostic criteria include sharp, paroxysmal, severe pain in the occipital region along with associated tenderness and sensory disturbances.1 Occipital neuralgia may be the result of pathology in the greater, lesser or third occipital nerves (Figure 1).2 Previous evidence indicates that occipital neuralgia affects the greater occipital nerve in 90% of cases, lesser occipital nerve in 10% of cases, and both occipital nerves in 9% of cases.3 However, the specific incidence and prevalence rates for occipital neuralgia remain unknown along with an elusive pathophysiology including the precise etiology.2,4 Differential diagnoses for occipital neuralgia include cervicogenic, migraine, cluster and tension-type headaches. Treatment for occipital neuralgia may comprise interventions such as pharmacology, conservative care, interventional therapies and/or surgery.2,5–8
Figure 1:
Distribution of the greater, lesser, and third occipital nerves.
Adapted from: Kemp III WJ, Tubbs RS, Cohen-Gadol AA. The innervation of the scalp: a comprehensive review including anatomy, pathology, and neurosurgical correlates. Surg Neurol Int. 2011;2:178.49
Dry needling (DN) or intramuscular stimulation is defined as a therapeutic procedure that involves inserting a dry needle, without medication, into a myofascial trigger point with the goal of inactivating a trigger point and mitigating pain.9,10 In 1979, Karel Lewit became one of the first persons to distinguish between the effects of inserting a dry needle into a myofascial trigger point and injection of a medicinal substance into a myofascial trigger point.11 Since that publication, there has been accumulating evidence supporting the use of DN in the management of myofascial pain along with basic science research attempting to establish therapeutic mechanisms.12–14
The primary purpose of this case report is to outline the diagnosis, intervention and clinical outcome of a 26-year-old female with occipital neuralgia. As part of this discussion, our article includes information outlining the anatomy, pathophysiology, clinical presentation, differential diagnosis and management of occipital neuralgia. In addition, this paper briefly reviews evidence supporting the use of DN in managing myofascial pain.
Case Report
Upon arrival, a 26-year-old female described a four-year history of neck pain and headaches. The patient related the onset of these symptoms secondary to a traumatic event four years prior to presentation. While walking a dog in damp conditions, she reported falling backwards and striking her head on the ground with a transient loss of consciousness. The day after striking her head, she proceeded to the hospital complaining of right-sided neck pain and headache in the occipital region. After an examination including x-rays, the patient described a diagnosis of “concussion” from the hospital physician. Also, she described “swelling” in her anterior neck region for approximately four weeks post-trauma, but the swelling abated with time and use of over-the-counter medications. However, her neck pain and headache continued beyond dissipation of the edema, transitioning to a persistent condition.
During the initial consultation, the patient described her right-sided neck pain and occipital headache as “knife-like” and stabbing. When asked to point to the painful region, she touched the right occipital region between the midline and the sternocleidomastoid muscle. Also, she recounted that the pain occasionally radiates into her right fronto-orbital region. She described a paroxysmal pattern to the stabbing pain, without ever experiencing complete resolution of symptoms. She indicated experiencing a severe headache in her right occipital region approximately one to two times a month with each occurrence lasting for about one week, including two to three days of high intensity pain with each episode. She denied vomiting, aura, prodrome or neurological indicators such nystagmus, numbness, nausea, dizziness, dysarthria, dysphagia, diplopia, drop attacks and ataxia. The patient rated the average daily pain as 2/10 on a verbal pain rating scale, with exacerbations or paroxysms rated as 9/10. She denied any triggers or aggravating factors related to the paroxysms, but these changes in pain seem random or unpredictable. However, the patient described several factors that afford pain relief, albeit temporary.
Factors that yielded provisional and limited relief of pain included spinal manipulation, transcutaneous electrical nerve stimulation (TENS), physical therapy, needling, and an orthodontic appliance. Previous physical therapy interventions included neck strengthening and relaxation exercises, while the orthodontist provided an oral appliance to reduce nocturnal “clenching” of the jaw. In addition, her family physician prescribed Maxalt (sublingual and oral) for treatment of headaches with a variable clinical response including limited relief or no effect. Finally, she recounted that “rubbing” or pressing the right temporal region above her eye reduces the severe pain associated with headaches, but this stimulation creates lacrimation and nausea. However, none of the remedies or interventions described above brought complete or lasting resolution of her pain.
She conveyed no previous specific diagnoses for her neck pain and headache. However, her past medical history included diagnoses related to low back pain, anxiety/depression, attention deficit disorder (ADD), acne, and pre-diabetic. She reported ongoing use of medications for managing her anxiety/depression (Cymbalta), ADD (Adderall), acne (Spironolactone), and pre-diabetes (Metformin). Her past medical history also included knee reconstruction approximately ten years prior. Her social and occupational history included limited alcohol (one unit per week) and caffeine (two drinks per day) consumption along with moderate exercise (three to four days per week for 30–45 minutes per session). The patient denied tobacco use or any other diagnoses.
Examination procedures included neurological screening/testing, range of motion/mobility, palpation, and orthopedic testing. Neurological testing included cranial nerve function along with muscle/strength testing, deep tendon reflexes, and sensation. Based upon examination, cranial nerve and upper quarter neurological function appeared within normal limits. Cervical spine active range of motion (AROM) consisted of three trials of motion in each direction measured with a single inclinometer. Based upon normative comparison values15, the patient’s AROM emerged WNL, except for limited extension (Table 1). Also, the patient denied painful sensations during performance of cervical AROM.
Table 1:
Pre-intervention Cervical Spine Active Range of Motion
| Trial | RR (°) | LR (°) | RLF (°) | LLF (°) | F (°) | E (°) |
|---|---|---|---|---|---|---|
| 1 | 78 | 74 | 38 | 42 | 60 | 40 |
| 2 | 82 | 78 | 44 | 42 | 54 | 39 |
| 3 | 76 | 78 | 45 | 51 | 59 | 41 |
| Mean±SD | 78.7±3.1 | 76.7±2.3 | 42.3±3.8 | 45.0±5.2 | 57.7±3.2 | 40.0±1.0 |
RR = right rotation; LR = left rotation; RLF = right lateral flexion;
LLF = left lateral flexion; F = flexion; E = extension; SD = standard deviation
Palpation of the cervical spine revealed elevated muscle tone in bilateral upper trapezii muscles. Using a soft tissue tenderness grading scheme16, palpation uncovered grade I tenderness in bilateral levator scapula muscles along the superomedial border of the scapula, bilateral interscapular muscles (rhomboids, middle trapezii, lower trapezii), and right posterior cuff muscles (teres minor, teres major). In addition, palpation elicited grade II tenderness in the right upper trapezius and occipital regions. For an additional description of this soft tissue tenderness grading scheme, please see Hubbard and Berkoff.16 Palpation revealed myofascial trigger points in bilateral upper trapezii muscles along with the right suboccipital muscles.
Orthopedic testing consisted of regional examination related to the complaint of cervical spine pain. The upper limb tension test A (ULTTA) and shoulder depression tests revealed negative results bilaterally.17,18 However, the cervical compression test elicited localized right-sided neck pain in the upper cervical region; left cervical compression produced negative results.17,18 Also, Spurling’s tests yielded localized right-sided pain in the upper cervical region and localized left-sided pain in the mid-cervical region.17,18 Cervical distraction test reduced the right-sided pain in the upper cervical region.17,18
Other outcomes measures for this case report included the neck disability index (NDI), and headache disability index (HDI). The patient completed each of these questionnaires on two occasions: pre-intervention at baseline and post-intervention at three week follow-up. Table 2 lists the NDI, and HDI scores pre and post-intervention.
Table 2:
Pre-intervention and Post-intervention Neck Disability Index (NDI), and Headache Disability Index (HDI) Scores
| Outcome Measure | Pre-Intervention | Post-Intervention |
|---|---|---|
| NDI | 42/100 | 10/100 |
| HDI | 62/100 | 34/100 |
The patient presentation and examination findings suggested a probable diagnosis of occipital neuralgia. Differential diagnoses included cervicogenic headache, migraine headache, and tension-type headache. After the patient read and signed the appropriate informed consent forms, the clinician initiated an intervention consisting of dry needling (DN). The patient underwent a total of four DN sessions over a two-week duration.
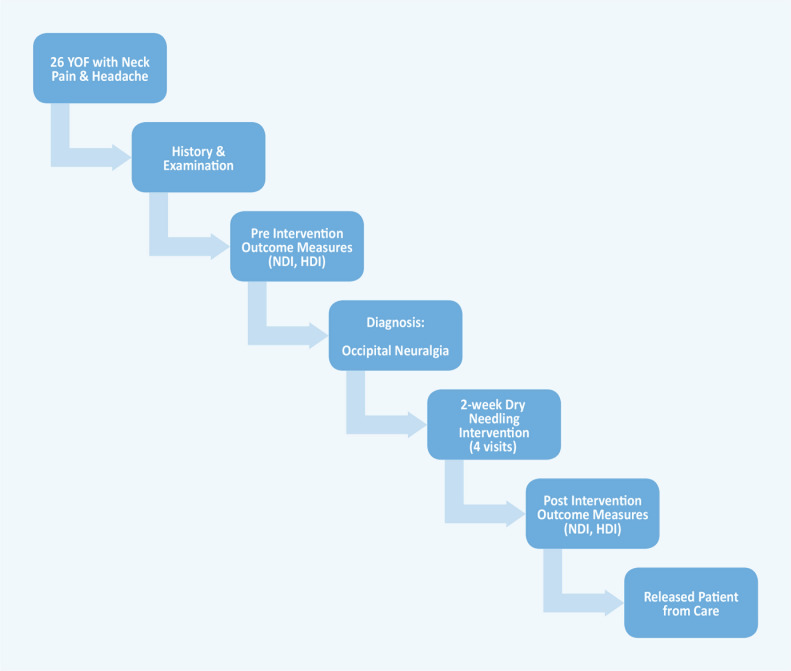
The first treatment session involved placing needles into myofascial trigger points located in bilateral upper trapezii muscles (see video demonstration) and bilateral cervical multifidi muscles between the C5-T1 regions. Following the first DN session, the patient reported “stiffness” in the right upper trapezius muscle that lasted approximately one hour. Also, she rated her right-sided neck pain and headache as 1/10 using the verbal pain rating scale. Orthopedic testing reproduced her neck pain and palpation elicited grade I tenderness in bilateral upper trapezii muscles and interscapular muscles, along with the right posterior cuff and suboccipital muscles. The second treatment session consisted of DN myofascial trigger points in the same anatomical regions as the first visit. A week later during the third visit, the patient reported sleeping on a “different pillow” which seemed to aggravate her condition. The patient stated that she seemed “on the verge” of an exacerbation in symptoms. During this third treatment session, needles were inserted into one additional anatomical region. On this occasion, needles were placed into bilateral upper trapezii muscles, bilateral cervical multifidi muscles, and the proximal attachment of bilateral suboccipital muscles along the nuchal line. Two days later, upon presentation for the fourth visit, the patient reported complete resolution of her neck pain and headache. Also, she felt that the last DN session had “aborted” her imminent exacerbation. Orthopedic testing demonstrated negative tests bilaterally for cervical compression and Spurling’s. Again, needles were placed into myofascial trigger points in bilateral upper trapezii, cervical multifidi and suboccipital muscles. During each of the four treatment sessions, insertion of needles into the described muscles elicited palpable and/or visible local twitch responses (LTRs). Three weeks following the final treatment session, the patient completed the post-intervention neck disability index, and headache disability index questionnaires. Finally, as a result of her favorable clinical outcome, the patient was discharged from care (Figure 2).
Figure 2:
Patient flow diagram outlining course of care and collection of outcome measures.
Discussion
A. Occipital Neuralgia
Anatomy
As previously discussed, occipital neuralgia may involve the greater occipital nerve, lesser occipital nerve, third occipital nerve or a combination of these neural structures (Figure 1).1–3 The greater occipital nerve derives from the medial branch of dorsal ramus of C2 while the lesser occipital nerve arises from branches of C2 and C3 in the cervical plexus.19 Lastly, the third occipital nerve originates from the medial branch of C3.19 Sensory innervation of greater occipital nerve consists of the cutaneous region on the posterior scalp between the external occipital protuberance and the vertex.19 The lesser occipital nerve provides cutaneous innervation to the lateral region of the scalp posterior to the ear whereas the third occipital nerve innervates the upper cervical spine and inferior occipital regions.19
Pathophysiology
Presently, the precise etiology of occipital neuralgia remains unclear with most cases presenting as idiopathic. However, proposed mechanisms of onset for occipital neuralgia include trauma, muscular entrapment, structural lesions or secondary diseases such as multiple sclerosis and myelitis.20–24 Based upon the potential presence of structural or organic etiologies associated with occipital neuralgia, neuroimaging modalities such as magnetic resonance imaging (MRI) may be indicated to rule out serious pathology.2
Clinical Presentation
The clinical presentation for occipital neuralgia has been described by the International Headache Society (IHS) including specific diagnostic criteria (Table 3). Also, according to the IHS, the pain associated with occipital neuralgia may extend to the fronto-orbital area via trigeminocervical interneuronal networks in the trigeminal spinal nuclei.1 In addition to the IHS criteria, patients may demonstrate a positive Tinel’s sign with repeated tapping over the occipital condyle producing numbness and/or tingling.2
Table 3:
IHS Diagnostic Criteria for Occipital Neuralgia1
Reproduced from: International Classification of Headache Disorders, 3rd edition. Cephalalgia: An International J Headache. 2013;33(9):629–808. With permission: SAGE Publications.
| A. | Unilateral or bilateral pain fulfilling criteria B–E |
| B. | Pain is located in the distribution of the greater, lesser and/or third occipital nerves |
| C. | Pain has two of the following three characteristics:
|
| D. | Pain is associated with both of the following:
|
| E. | Pain is eased temporarily by local anaesthetic block of the affected nerve |
| F. | Not better accounted for by another ICHD-3 diagnosis. |
Differential Diagnosis
As previously stated, differential diagnoses for occipital neuralgia include cervicogenic, migraine, cluster and tension-type headaches. These headache disorders closely resemble the clinical presentation associated with occipital neuralgia, particularly cervicogenic headache. For example, both occipital neuralgia and cervicogenic headache may present with pain the upper cervical and occipital regions. However, the pain associated with cervicogenic headache is often described as dull, while the pain description for occipital neuralgia is usually expressed as sharp, stabbing or shooting.2 In light of the IHS diagnostic criteria for cervicogenic headache (Table 4), it becomes apparent that the clinical presentations for cervicogenic headache and occipital neuralgia overlap, thus creating a diagnostic challenge.1 The diagnostic hallmarks of migraine headache (with or without aura) include unilateral location with pulsating quality of moderate or severe pain intensity and aggravated by or causing avoidance of routine physical activity, while cluster headaches present as brief, severe, unilateral headaches with associated lacrimation, rhinorrhea, facial sweating along with myosis and/or ptosis.1 The clinical presentation for tension-type headache includes bilateral location with a pressing or tightening (non-pulsating) quality of mild or moderate intensity.1 Thus, mindful clinical evaluation is needed to ensure the correct diagnosis for a particular headache presentation.
Table 4:
IHS Diagnostic Criteria for Cervicogenic Headache1
Reproduced from: International Classification of Headache Disorders, 3rd edition. Cephalalgia: An International J Headache. 2013;33(9):629–808. With permission: SAGE Publications.
| A. | Any headache fulfilling criterion C |
| B. | Clinical, laboratory and/or imaging evidence of a disorder or lesion within the cervical spine or soft tissues of the neck, known to be able to cause headache |
| C. | Evidence of causation demonstrated by at least two of the following:
|
| D. | Not better accounted for by another ICHD-3 diagnosis. |
Management
As outlined earlier, management considerations for occipital neuralgia may include pharmacology, conservative care, interventional therapies and/or surgery. With regards to pharmacological approaches, previous literature describes using non-steroidal anti-inflammatory drugs (NSAIDs), muscle relaxers, tricyclic antidepressants, and antiepileptics to manage occipital neuralgia.2,7 Conservative or non-pharmacological interventions targeting abnormal muscle tone involve rest, cryotherapy or thermotherapy, soft-tissue massage, and physical therapy.7
Interventional therapies (ITs) for managing occipital neuralgia consist of injections, pulsed radiofrequency ablation, and occipital neurostimulation.2,6,7,25 Briefly expanding on these ITs, injection or infiltration of the greater occipital nerve or lesser occipital nerve with anaesthetic (i.e., lidocaine) is considered diagnostic for occipital neuralgia, but also therapeutic by providing transient pain relief.20,25 In addition, botulinum toxin type A is another infiltrate that has been reported as beneficial for managing occipital neuralgia.26 According to Dougherty, pulsed radiofrequency (PRF) exposes afferent nerve endings to intermittent short duration, high-voltage radiofrequency signals creating a low-intensity electrical field around sensory nerves, thus modulating pain via ablation or degeneration.2 Lastly, occipital neurostimulation involves implantation of electrodes in the occipital region that produce paresthesia with resultant pain modulation in the distribution of the occipital nerves.27
Previous research indicates surgical excision of the greater occipital nerve may provide pain relief for occipital neuralgia.5 However, this surgical procedure should only be considered as a last resort in response to unsuccessful attempts to resolve pain via other interventions.5
B. Dry Needling
As previously mentioned, dry needling (DN) or intramuscular stimulation is defined as a therapeutic procedure that involves inserting a dry needle, without medication, into a myofascial trigger point with the goal of inactivating a trigger point and mitigating pain.9,10 By comparison, a fundamental premise of acupuncture is controlling and regulating energy flow and balance via needling of defined points.9 Also, acupuncture is founded on Eastern concepts, while DN is based on neurophysiological and biomechanical principles.9,28 However, according to scientific literature, acupuncture and DN employ the same therapeutic tool, namely a solid filament needle. For a more detailed discussion of DN and acupuncture, please review an article written by Dommerholt.9
By definition, a myofascial trigger point is described as a hyperirritable point in a taut band of skeletal muscle fibers with resultant local ischemia and hypoxia along with peripheral and central sensitization.12 A theoretical construct outlining the outcomes of DN proposes that needling of myofascial trigger points induces physiological effects that modulate muscle tension, local ischemia and hypoxia, along with peripheral and central sensitization.12
Previous literature describes that DN of myofascial trigger points elicits a local twitch response (LTR) thus changing muscle length and tension through regulation of spontaneous electrical activity.29,30 By definition, a LTR is a localized contraction within a muscle produced by an involuntary spinal reflex as a result of being stretched, injected or dry needled.12 Also, previous research suggests that eliciting a LTR improves the clinical outcomes associated with DN.31 In addition to changing muscle length and tension, DN may stimulate a change in blood flow within the ischemic and hypoxic tissues of a myofascial trigger point.32 Lastly, research indicates that DN may modulate pain through peripheral and central pathways including segmental inhibition and biochemical cascades such as endogenous opioids, and serotonergic and adrenergic mediators.33–37
A recent systematic review and meta-analysis recommended DN for patients with upper-quarter myofascial pain syndrome, compared to sham or placebo, for reducing pain immediately following treatment and at four weeks post-intervention.38 According to Vulfsons et al, DN performed by a competent clinician may be considered a safe intervention.13 However, mild adverse events have been reported including localized muscle soreness and hemorrhaging, or more seriously, spinal epidural hematoma.39,40 Evidence suggests that the incidence of severe adverse events associated with needling is very rare.41 Moreover, caution is advised while DN around potentially vulnerable anatomical structures such as those within the cervical and thorax regions.13
In the context of this case report, the patient presentation closely matched the International Headache Society (IHS) criteria for occipital neuralgia including unilateral, severe, stabbing, paroxysmal pain in the greater occipital nerve region with associated tenderness and myofascial trigger points. The patient presentation did not meet the IHS criteria of temporary pain relief provided by local anaesthetic block of the affected nerve. However, following the four sessions of myofascial trigger point dry needling in our case report, the patient reported a 32-point change on a 100-point scale in her neck disability index score along with a 28-point change on a 100-point scale in her headache disability index score. According to recent literature, the minimum detectable change (MDC) for the neck disability index is approximately 10/100 for uncomplicated neck pain and 20/100 for cervical radiculopathy.42,43 Also, the described clinically important difference (CID) for the neck disability index varies amongst reports ranging from 10/100 to 38/100.43 In order to ascribe the effects of clinical improvement to an intervention, a patient must report a 29-point change in headache disability index scores from pre to post-intervention.44 Thus, it appears that following four sessions of DN over two weeks, our patient experienced meaningful improvement in her neck pain and headaches.
Previous literature supports the theory that the therapeutic mechanism of pain relief following anaesthetic injection of myofascial trigger points might be the associated neuromechanical stimulation of the needle itself.9,11,14,31 For example, a recent study compared the effects of dry needling, lidocaine injections and botulinum toxin type A injections into myofascial trigger points of patients presenting with myofascial pain syndrome.45 Using a syringe (not an acupuncture needle) for each of the three needling interventions, the researchers reported clinical outcomes such as pain pressure threshold and pain scores significantly improved in all three groups. When contrasting injection therapy with DN of myofascial trigger points, numerous investigators have proposed that “dry needling of the myofascial trigger point provides as much pain relief as injection of lidocaine but causes more post-injection soreness”.46 Thus, using DN to manage the myofascial trigger points associated with occipital neuralgia may have implicitly met the IHS criteria of pain relief following anaesthetic block of the affected nerve.
Previous case reports using acupuncture to manage occipital neuralgia have described favorable clinical outcomes.8,47,48 However, to the best of our knowledge, this is the first case report describing dry needling to successfully improve clinical outcomes in a patient diagnosed with occipital neuralgia.
Limitations
As this paper describes a single case report involving occipital neuralgia and dry needling, there may be possible limitations. Although diagnosed with occipital neuralgia based upon the IHS criteria, the patient may have exhibited an alternative diagnosis or a more complex diagnosis with associated co-morbidities. Also, the clinical presentation might have mimicked another closely related condition such cervicogenic headache. Also, it is not plausible to establish a causal relationship between DN and occipital neuralgia based upon a single case report. However, the information from this case report may stimulate critical thinking and appraisal leading to a more sophisticated experimental design examining the effects of DN in patients presenting with occipital neuralgia.
Footnotes
Consent
The patient provided written informed consent acknowledging permission for publication of this case report. A copy of the written consent is accessible for review from the Editor of this journal.
Authors’ Contributions
BB provided patient care along with conducting the literature review and composing the manuscript. CK also assisted with the literature review and manuscript preparation. Both author’s read and approved the final manuscript.
Declaration: The authors have no conflicts of interest to declare regarding this paper or the material described therein.
Consent: The patient provided written informed consent acknowledging permission for publication of this case report.
References
- 1.The International Classification of Headache Disorders. 3rd edition. 9. Vol. 33. Cephalalgia: An International J Headache; 2013. pp. 629–808. (beta version). [DOI] [PubMed] [Google Scholar]
- 2.Dougherty C. Occipital neuralgia. Current Pain and Headache Reports. 2014;18(5):411. doi: 10.1007/s11916-014-0411-x. [DOI] [PubMed] [Google Scholar]
- 3.Hammond SR, Danta G. Occipital Neuralgia. Clinical and Experimental Neurology. 1978;15:258–70. [PubMed] [Google Scholar]
- 4.Sahai-Srivastava S, Zheng L. Occipital neuralgia with and without migraine: difference in pain characteristics and risk factors. Headache. 2011;51(1):124–8. doi: 10.1111/j.1526-4610.2010.01788.x. [DOI] [PubMed] [Google Scholar]
- 5.Ducic I, Felder JM, 3rd, Khan N, Youn S. Greater occipital nerve excision for occipital neuralgia refractory to nerve decompression. Annals Plastic Surg. 2014;72(2):184–7. doi: 10.1097/SAP.0b013e3182898736. [DOI] [PubMed] [Google Scholar]
- 6.Hamer JF, Purath TA. Response of cervicogenic headaches and occipital neuralgia to radiofrequency ablation of the C2 dorsal root ganglion and/or third occipital nerve. Headache. 2014;54(3):500–10. doi: 10.1111/head.12295. [DOI] [PubMed] [Google Scholar]
- 7.Vanelderen P, Lataster A, Levy R, Mekhail N, van Kleef M, Van Zundert J. 8. Occipital neuralgia. Pain Practice: Official Journal of World Institute of Pain. 2010;10(2):137–44. doi: 10.1111/j.1533-2500.2009.00355.x. [DOI] [PubMed] [Google Scholar]
- 8.Pan C, Tan G. Forty-two cases of greater occipital neuralgia treated by acupuncture plus acupoint-injection. J Traditional Chinese Medicine = Chung i tsa chih ying wen pan /sponsored by All-China Association of Traditional Chinese Medicine, Academy of Traditional Chinese Medicine. 2008;28(3):175–7. doi: 10.1016/s0254-6272(08)60040-0. [DOI] [PubMed] [Google Scholar]
- 9.Dommerholt J, Mayoral del Moral O, Gröbli C. Trigger point dry needling. J Manual & Manipulative Ther. 2006;14(4):70E–87E. doi: 10.1080/10669817.2019.1568699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.American Physical Therapy Association Department of Practice and State Government Affairs. Physical Therapists and the Performance of Dry Needling: An Educational Resource Paper. APTA; 2012. [Google Scholar]
- 11.Lewit K. The needle effect in the relief of myofascial pain. Pain. 1979;6(1):83–90. doi: 10.1016/0304-3959(79)90142-8. [DOI] [PubMed] [Google Scholar]
- 12.Cagnie B, Dewitte V, Barbe T, Timmermans F, Delrue N, Meeus M. Physiologic effects of dry needling. Current Pain and Headache Reports. 2013;17(8):348. doi: 10.1007/s11916-013-0348-5. [DOI] [PubMed] [Google Scholar]
- 13.Vulfsons S, Ratmansky M, Kalichman L. Trigger point needling: techniques and outcome. Current Pain and Headache Reports. 2012;16(5):407–12. doi: 10.1007/s11916-012-0279-6. [DOI] [PubMed] [Google Scholar]
- 14.Kalichman L, Vulfsons S. Dry needling in the management of musculoskeletal pain. J Am Board of Family Med: JABFM. 2010;23(5):640–6. doi: 10.3122/jabfm.2010.05.090296. [DOI] [PubMed] [Google Scholar]
- 15.Reese NB, Bandy WD. Joint range of motion and muscle length testing. Elsevier Health Sciences; 2013. [Google Scholar]
- 16.Hubbard DR, Berkoff GM. Myofascial trigger points show spontaneous needle EMG activity. Spine. 1993;18(13):1803–7. doi: 10.1097/00007632-199310000-00015. [DOI] [PubMed] [Google Scholar]
- 17.Hoens A. Orthopaedic Clinical Examination: An evidence-based approach for physical therapists. Physiotherapy Canada. 2008;60(2):198. [Google Scholar]
- 18.Cleland J. Orthopaedic clinical examination: an evidence-based approach for physical therapists. WB Saunders Co; 2005. [Google Scholar]
- 19.Standring S. Gray’s anatomy. The anatomical basis of clinical practice. 2008. p. 39.
- 20.Walker J, Howell S. Ultrasound guided greater occipital nerve blocks for post-traumatic occipital neuralgia. West Virginia Med J. 2014;110(2):12–3. [PubMed] [Google Scholar]
- 21.Son BC, Kim DR, Lee SW. Intractable occipital neuralgia caused by an entrapment in the semispinalis capitis. J Korean Neurosurgical Society. 2013;54(3):268–71. doi: 10.3340/jkns.2013.54.3.268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.White JB, Atkinson PP, Cloft HJ, Atkinson JL. Vascular compression as a potential cause of occipital neuralgia: a case report. Cephalalgia: An International J Headache. 2008;28(1):78–82. doi: 10.1111/j.1468-2982.2007.01427.x. [DOI] [PubMed] [Google Scholar]
- 23.De Santi L, Annunziata P. Symptomatic cranial neuralgias in multiple sclerosis: clinical features and treatment. Clinical Neurology Neurosurg. 2012;114(2):101–7. doi: 10.1016/j.clineuro.2011.10.044. [DOI] [PubMed] [Google Scholar]
- 24.Goicochea MT, Romero C, Leston JA. Occipital neuralgia with cervical myelitis. Cephalalgia: An International J Headache. 2008;28(5):567–8. doi: 10.1111/j.1468-2982.2008.01543.x. [DOI] [PubMed] [Google Scholar]
- 25.Gadient PM, Smith JH. The neuralgias: diagnosis and management. Current Neurology and Neuroscience Reports. 2014;14(7):459. doi: 10.1007/s11910-014-0459-3. [DOI] [PubMed] [Google Scholar]
- 26.Kapural L, Stillman M, Kapural M, McIntyre P, Guirgius M, Mekhail N. Botulinum toxin occipital nerve block for the treatment of severe occipital neuralgia: a case series. Pain Practice: Official J World Institute Pain. 2007;7(4):337–40. doi: 10.1111/j.1533-2500.2007.00150.x. [DOI] [PubMed] [Google Scholar]
- 27.Paemeleire K, Bartsch T. Occipital nerve stimulation for headache disorders. Neurotherapeutics: J Am Society for Experimental NeuroTherapeutics. 2010;7(2):213–9. doi: 10.1016/j.nurt.2010.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dommerholt J. Dry needling - peripheral and central considerations. J Manual & Manipulative Ther. 2011;19(4):223–7. doi: 10.1179/106698111X13129729552065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen JT, Chung KC, Hou CR, Kuan TS, Chen SM, Hong CZ. Inhibitory effect of dry needling on the spontaneous electrical activity recorded from myofascial trigger spots of rabbit skeletal muscle. Am J Phys Med Rehabil / Assoc Academic Physiatrists. 2001;80(10):729–35. doi: 10.1097/00002060-200110000-00004. [DOI] [PubMed] [Google Scholar]
- 30.Hsieh YL, Chou LW, Joe YS, Hong CZ. Spinal cord mechanism involving the remote effects of dry needling on the irritability of myofascial trigger spots in rabbit skeletal muscle. Arch Phys Med Rehabil. 2011;92(7):1098–105. doi: 10.1016/j.apmr.2010.11.018. [DOI] [PubMed] [Google Scholar]
- 31.Hong CZ. Lidocaine injection versus dry needling to myofascial trigger point. The importance of the local twitch response. Am J Phys Med Rehabil / Assoc Academic Physiatrists. 1994;73(4):256–63. doi: 10.1097/00002060-199407000-00006. [DOI] [PubMed] [Google Scholar]
- 32.Cagnie B, Barbe T, De Ridder E, Van Oosterwijck J, Cools A, Danneels L. The influence of dry needling of the trapezius muscle on muscle blood flow and oxygenation. J Manip Physiol Thera. 2012;35(9):685–91. doi: 10.1016/j.jmpt.2012.10.005. [DOI] [PubMed] [Google Scholar]
- 33.Hsieh YL, Yang SA, Yang CC, Chou LW. Dry needling at myofascial trigger spots of rabbit skeletal muscles modulates the biochemicals associated with pain, inflammation, and hypoxia. Evidence-based Complementary and Alternative Medicine: Ecam. 2012;2012:342165. doi: 10.1155/2012/342165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Srbely JZ, Dickey JP, Lee D, Lowerison M. Dry needle stimulation of myofascial trigger points evokes segmental anti-nociceptive effects. J Rehab Med. 2010;42(5):463–8. doi: 10.2340/16501977-0535. [DOI] [PubMed] [Google Scholar]
- 35.Niddam DM, Chan RC, Lee SH, Yeh TC, Hsieh JC. Central modulation of pain evoked from myofascial trigger point. Clin J Pain. 2007;23(5):440–8. doi: 10.1097/AJP.0b013e318058accb. [DOI] [PubMed] [Google Scholar]
- 36.Shah JP, Phillips TM, Danoff JV, Gerber LH. An in vivo microanalytical technique for measuring the local biochemical milieu of human skeletal muscle. J Applied Physiology (Bethesda, Md: 1985) 2005;99(5):1977–84. doi: 10.1152/japplphysiol.00419.2005. [DOI] [PubMed] [Google Scholar]
- 37.Shah JP, Gilliams EA. Uncovering the biochemical milieu of myofascial trigger points using in vivo microdialysis: an application of muscle pain concepts to myofascial pain syndrome. J Bodywork Movement Ther. 2008;12(4):371–84. doi: 10.1016/j.jbmt.2008.06.006. [DOI] [PubMed] [Google Scholar]
- 38.Kietrys DM, Palombaro KM, Azzaretto E, et al. Effectiveness of dry needling for upper-quarter myofascial pain: a systematic review and meta-analysis. J Ortho Sports Phys Ther. 2013;43(9):620–34. doi: 10.2519/jospt.2013.4668. [DOI] [PubMed] [Google Scholar]
- 39.Ga H, Choi JH, Park CH, Yoon HJ. Dry needling of trigger points with and without paraspinal needling in myofascial pain syndromes in elderly patients. J Alternative and Complementary Medicine (New York, NY) 2007;13(6):617–24. doi: 10.1089/acm.2006.6371. [DOI] [PubMed] [Google Scholar]
- 40.Lee JH, Lee H, Jo DJ. An acute cervical epidural hematoma as a complication of dry needling. Spine. 2011;36(13):E891–3. doi: 10.1097/BRS.0b013e3181fc1e38. [DOI] [PubMed] [Google Scholar]
- 41.Yamashita H, Tsukayama H, Tanno Y, Nishijo K. Adverse events in acupuncture and moxibustion treatment: a six-year survey at a national clinic in Japan. J Alternative and Complementary Medicine (New York, NY) 1999;5(3):229–36. doi: 10.1089/acm.1999.5.229. [DOI] [PubMed] [Google Scholar]
- 42.Cleland JA, Childs JD, Whitman JM. Psychometric properties of the Neck Disability Index and Numeric Pain Rating Scale in patients with mechanical neck pain. Arch Phys Med Rehabil. 2008;89(1):69–74. doi: 10.1016/j.apmr.2007.08.126. [DOI] [PubMed] [Google Scholar]
- 43.MacDermid JC, Walton DM, Avery S, et al. Measurement properties of the neck disability index: a systematic review. J Ortho Sports Phys Ther. 2009;39(5):400–17. doi: 10.2519/jospt.2009.2930. [DOI] [PubMed] [Google Scholar]
- 44.Jacobson GP, Ramadan NM, Aggarwal SK, Newman CW. The Henry Ford Hospital Headache Disability Inventory (HDI) Neurology. 1994;44(5):837–42. doi: 10.1212/wnl.44.5.837. [DOI] [PubMed] [Google Scholar]
- 45.Kamanli A, Kaya A, Ardicoglu O, Ozgocmen S, Zengin FO, Bayik Y. Comparison of lidocaine injection, botulinum toxin injection, and dry needling to trigger points in myofascial pain syndrome. Rheumatology International. 2005;25(8):604–11. doi: 10.1007/s00296-004-0485-6. [DOI] [PubMed] [Google Scholar]
- 46.Borg-Stein J. Treatment of fibromyalgia, myofascial pain, and related disorders. Phys Med Rehabil Clinics of North America. 2006;17(2):491–510. doi: 10.1016/j.pmr.2005.12.003. [DOI] [PubMed] [Google Scholar]
- 47.Wang H, Chen H, Jiang H. Experience in acupuncture treatment of occipital neuralgia. J Traditional Chinese Medicine = Chung i tsa chih ying wen pan / sponsored by All-China Association of Traditional Chinese Medicine, Academy of Traditional Chinese Medicine. 2002;22(3):183. [PubMed] [Google Scholar]
- 48.Xie Z. 51 cases of occipital neuralgia treated with acupuncture. J Traditional Chinese Medicine = Chung i tsa chih ying wen pan / sponsored by All-China Association of Traditional Chinese Medicine, Academy of Traditional Chinese Medicine. 1992;12(3):180–1. [PubMed] [Google Scholar]
- 49.Kemp WJ, 3rd, Tubbs RS, Cohen-Gadol AA. The innervation of the scalp: A comprehensive review including anatomy, pathology, and neurosurgical correlates. Surgical Neurology International. 2011;2:178. doi: 10.4103/2152-7806.90699. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.