Abstract
External-beam radiotherapy (EBRT) combined with androgen deprivation therapy (ADT) is known to provide improved survival outcomes compared with EBRT alone in the treatment of prostate cancer; however, the use of ADT has been reported to be associated with adverse events. Accordingly, the aim of the present study was to clarify the adequate duration of ADT when combined with EBRT to treat patients with high-risk localized prostate cancer, with consideration of survival outcomes and toxicity. Between 2001 and 2011, 173 patients with high-risk localized prostate cancer received ADT combined with EBRT, at a median dose of 69.6 Gy. Of these, 54 (31%) underwent short-term ADT (<36 months) and 119 (69%) underwent long-term ADT (≥36 months). During the median follow-up period of 54 months, the five-year progression-free survival rate of patients receiving short-term ADT (72.9%) was significantly lower than that of patients receiving long-term ADT (92.8%) (P<0.01). Furthermore, the incidence of cardiovascular toxicity at grade II or above was significantly higher amongst patients treated with short-term ADT compared with patients treated with long-term ADT (P<0.01). Thus, the present study determined that ADT for ≥36 months combined with EBRT significantly improved the progression-free survival of patients with high-risk localized prostate cancer and exhibited an acceptable toxicity profile.
Keywords: androgen deprivation therapy, prostate cancer, external-beam radiotherapy
Introduction
Since screening tests for prostate cancer using prostate-specific antigen (PSA) were introduced, the proportion of patients exhibiting locally advanced disease at diagnosis has decreased in Japan (1). Accordingly, the number of patients undergoing external-beam radiotherapy (EBRT) as curative treatment has increased (2). Despite this, the mortality rate associated with prostate cancer has continuously increased over the past few decades (3); therefore, to address this, radiotherapy combined with androgen deprivation therapy (ADT) has been evaluated for the treatment prostate cancer.
Various studies have demonstrated that EBRT combined with ADT provides improved biochemical progression-free and overall survival compared with EBRT alone (4–6). However, the use of ADT has been reported to be a risk factor for cardiovascular mortality (7) and deterioration in the quality of life (8). Furthermore, Bolla et al (9) recently reported that EBRT combined with six months of ADT resulted in shorter overall survival times than EBRT combined with 36 months of ADT; however, it remains unclear whether EBRT combined with an ADT duration of ≥36 months provides any benefit for patients with prostate cancer. Thus, the present study was performed to investigate survival rate and the incidence of adverse events in high-risk localized prostate cancer patients treated with EBRT combined with ADT administered over a short (<36 months) or long (≥36 months) period.
Patients and methods
Patients
The present study retrospectively identified 173 patients with high-risk localized prostate cancer who were treated using definitive EBRT between January 2001 and August 2011 at the Hachioji Center of the Tokyo Medical University Hospital (Tokyo, Japan). Written informed consent was obtained for all patients prior to EBRT treatment. High-risk disease was diagnosed on the basis of the presence of at least one of the following factors, according to the classification utilized by Kuban et al (10): A stage T3-4 tumor, a tumor with a Gleason score of ≥8 or a serum PSA level of >20 ng/ml. Additionally, the disease stage was determined according to the sixth edition of the tumor-node-metastasis classification system of the International Union Against Cancer 2002 (11).
Treatment strategy
Patients were divided into two groups according to the duration of ADT, with one receiving a short-term course of ADT (<36 months; n=54) and the other a long-term course of ADT (≥36 months; n=119).
EBRT treatment preparation and the actual procedure were performed with the patient in a supine position and with a full bladder. For treatment preparation, all patients underwent pelvic computed tomography at a 2.5-mm slice thickness. Typically, the EBRT treatment included prostate and pelvic lymph node irradiation using anteroposterior opposite ports or a box technique at a dose of 40 Gy. An additional dose of 30 Gy was administrated to the prostate and the proximal portion of the seminal vesicle using the lateral and anterior ports. Subsequently, all patients were treated with photons of 10 MV and 1.8 or 2.0 Gy, once a day, five days a week.
Follow-up procedure
After the completion of EBRT, clinical assessments, laboratory tests for toxicity and PSA measurements were performed every three months for five years and every six months thereafter. Biochemical progression was defined as a rise in PSA levels of 2 ng/ml above the PSA nadir according to the American Society for Therapeutic Radiation and Oncology consensus guidelines (12); progression-free survival was defined as the time from commencing EBRT to the time of biochemical progression, clinical progression or mortality from any cause; and overall survival was defined as the time from commencing EBRT to the time of mortality from any cause.
Statistical analysis
The survival rate was calculated using the Kaplan-Meier method, the difference in survival was assessed by performing the log-rank test, and hazard ratio and confidence intervals were estimated using Cox's proportional hazards model. Furthermore, statistical analysis was performed using Stata statistical software (version 12; StataCorp, College Station, TX, USA) and the Common Terminology Criteria for Adverse Events (version 3.0) (13) was used to assess toxicities. P<0.05 was considered to indicate a statistically significant difference.
Results
Patients
The characteristics of the 173 patients with histologically-proven adenocarcinoma included in the current analysis are summarized in Table I. The median age of the patients was 74 years (range, 56–87 years) and all patients had an Eastern Cooperative Oncology Group performance status of 0 or 1 (14). Furthermore, 66% of tumors were classified as T3 or T4 and 60% of tumors were assigned a Gleason score of ≥8 (15). The median pretreatment PSA level was 24 ng/ml (range, 0.2–400 ng/ml) and the median follow-up duration of the patients was 53 months (range, 8–143 months).
Table I.
Patient and disease characteristics.
| Duration of ADT, months | |||
|---|---|---|---|
| Parameter | <36 (n=54) | ≥36 (n=119) | P-value |
| Age, years | |||
| Median (range) | 74 (83–58) | 74 (87–56) | 0.73 |
| T stage, n (%) | |||
| T1 | 12 (22) | 18 (15) | |
| T2 | 9 (17) | 20 (17) | |
| T3 | 31 (57) | 74 (62) | |
| T4 | 2 (4) | 7 (6) | 0.67 |
| Gleason score, n (%) | |||
| ≤6 | 6 (11) | 11 (9) | |
| 7 | 14 (26) | 38 (32) | |
| ≥8 | 34 (63) | 70 (59) | 0.71 |
| PSA levela, n (%) | |||
| <10.0 | 15 (28) | 20 (17) | |
| 10.0–20.0 | 7 (13) | 27 (23) | |
| ≥20.0 | 32 (59) | 72 (60) | 0.14 |
| Irradiated site, n (%) | |||
| Prostate only | 3 (6) | 14 (12) | |
| Pelvic lymph node and prostate | 51 (94) | 105 (88) | 0.28 |
PSA is represented as ng/ml. ADT, androgen deprivation therapy; PSA, prostate-specific antigen.
Treatment
In total, five patients (3%) underwent orchiectomy and 151 patients (87%) were treated with a luteinizing hormone-releasing hormone (LH-RH) agonist (3.75 mg subcutaneously per month) and bicalutamide (80 mg/day) immediately after histological confirmation of prostate cancer. A total of 14 (8%) and three (2%) patients received only LH-RH or bicalutamide, respectively. The median duration of ADT was 47 months (range, 3–144 months); 54 patients (31%) received a short-term course of ADT (<36 months; median, 24.5 months) and the remaining 119 patients (69%) received a long long-term course (≥36 months; median, 58 months). Furthermore, neoadjuvant ADT was administered to 71 patients (41%) for a median duration of four months.
All patients underwent definitive EBRT, however, 17 patients (10%) underwent prostate irradiation only. The total median dose received was 69.6 Gy (range, 65.6–74 Gy) and the median duration of EBRT was 53 days (range, 45–66 days).
Survival outcomes
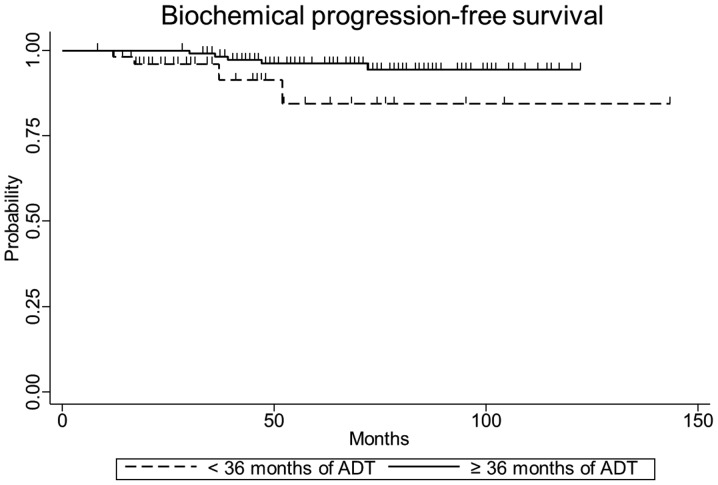
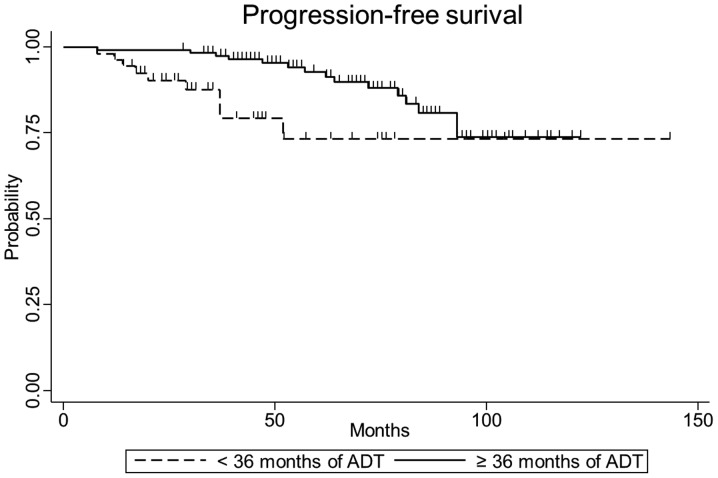
The five-year biochemical progression-free, clinical progression-free and overall survival rates were 84.0% [95% confidence interval (CI), 58.0–94.6], 72.9% (95% CI, 50.9–86.2) and 86.8% (95% CI, 70.0–94.6), respectively, for patients in the short-term ADT group, and 96.2% (95% CI, 90.2–98.6), 92.8% (95% CI, 85.3–96.6) and 94.4% (95% CI, 86.9–97.7), respectively, for patients in the long-term ADT group. The differences in five-year biochemical (P=0.04) and clinical progression-free survival (P<0.01) were statistically significant between the short- and long-term treatment groups, however, the difference in overall survival (P=0.16) was not. The biochemical and clinical progression-free survival curves according to the duration of ADT are indicated in Figs. 1 and 2. Only the duration of ADT was identified as a significant prognostic factor for progression-free survival in high-risk localized prostate cancer, according to multivariate analysis (hazard ratio, 0.30; 95% CI, 0.12–0.75; P=0.01; Table II).
Figure 1.
Kaplan-Meier analysis indicating a significant difference in biochemical progression-free survival depending on the duration of ADT (P=0.04). The five-year biochemical progression-free survival rates in patients treated with <36 or ≥36 months of ADT were 84.0% [95% confidence interval (CI), 58.0–94.6] and 96.2% (95% CI, 90.2–98.6), respectively. ADT, androgen deprivation therapy.
Figure 2.
Kaplan-Meier analysis indicating a significant difference in progression-free survival (P<0.01) depending on the duration of ADT. The five-year progression-free survival rates after <36 or ≥36 months of ADT were 72.9% [95% confidence interval (CI), 50.9–86.2] and 92.8% (95% CI, 85.3–96.6), respectively. ADT, adrogen deprivation therapy.
Table II.
Prognostic factors for progression-free survival.
| Prognostic factor | Hazard ratio | 95% confidence interval | P-value |
|---|---|---|---|
| Age, <75 vs. ≥75 years | 0.82 | 0.35–1.93 | 0.64 |
| T stage, T1,2 vs. T3,4 | 1.63 | 0.63–4.23 | 0.32 |
| Gleason score, <8 vs. ≥8 | 0.95 | 0.10–2.23 | 0.90 |
| PSA, <20 vs. ≥20 ng/ml | 1.37 | 0.55–3.41 | 0.50 |
| Duration of ADT, <36 vs. ≥36 months | 0.30 | 0.12–0.75 | 0.01 |
| Irradiated volume, PO vs. WP | 0.57 | 0.17–1.87 | 0.35 |
PSA, prostate-specific antigen; ADT, androgen deprivation therapy; PO, prostate only; WP, pelvic lymph node and prostate.
Toxicity
With regard to the treatment-associated toxicities of grade II or above, diarrhea was significantly more common amongst patients treated with long-term ADT than among patients who underwent short-term ADT (P=0.02; Table III). By contrast, cardiovascular toxicity was significantly more common amongst patients treated with short-term ADT compared with those treated with long-term ADT (P<0.01; Table III).
Table III.
Number of toxicities grade II or above in groups treated with ADT for <36 (n=54) or ≥36 (n=119) months.
| Duration of ADT, months | |||
|---|---|---|---|
| Toxicity | <36, n (%) | ≥36, n (%) | P-value |
| Gastrointestinal | |||
| Diarrhea | 2 (4) | 19 (16) | 0.02 |
| Rectal bleeding | 1 (2) | 0 (0) | 0.31 |
| Genitourinary | 8 (15) | 26 (22) | 0.42 |
| Cardiovascular | 5 (9) | 0 (0) | <0.01 |
ADT, adrogen deprivation therapy.
Discussion
In the present retrospective study, it was identified that high-risk prostate cancer patients treated with EBRT in combination with ADT for ≥36 months demonstrated improved progression-free survival rates compared with patients treated with EBRT in combination with ADT for <36 months. Over the median 53-month follow-up period, overall survival was not significantly different between the two groups, although a number of patients undergoing short-term ADT exhibited cardiovascular toxicity.
For high-risk prostate cancer, three previously conducted clinical trials have compared the outcomes of patients treated with long-term ADT alone and those treated with long-term ADT in combination with EBRT (16–18). These trials demonstrated improved biochemical progression-free (16) and overall (17,18) survival amongst patients who underwent combined long-term ADT and EBRT; however, the patient cohorts in these studies were inherently heterogeneous and different clinical stages were included. For example, the Scandinavian Prostate Cancer Group Study-7 and Swedish Association for Urological Oncology-3 (SPCG-7/SAUO-3) trial included a higher proportion of patients with favorable characteristics (18). By contrast, trials conducted in France (16), as well as in Canada and the UK [conducted by the National Cancer Institute of Canada Clinical Trial Group (PR.3) and the Medical Research Council (PR07; NCIC/MRC)] (17) enrolled patients with clinical stage T3 or T4 tumors, and >60% of patients had a PSA level of >20 mg. Similarly, ~70% of patients in the present study had a T3 or T4 stage tumor and 60% of patients had a PSA level of ≥20 mg. Overall, the patient characteristics in the current study were similar to those in the two aforementioned trials, and five-year progression-free survival was comparable between the current study and the NCIC/MRC trial. However, the outcome of the patients in the French study was apparently inferior to those in the present study and NCIC/MRC trials, despite the use of similar radiation doses and the administration of LH-RH.
With regard to the Gleason score, tumors in the present study were assigned a higher Gleason score compared with the SPCG-7/SAUO-3 and NCIC/MRC trials. However, Albertsen et al (19) reported that pathologists have recently tended to assign higher Gleason scores, with tumors diagnosed between 2002 and 2004 being assigned higher scores than those diagnosed between 1990 and 1992. As a result, prostate cancer mortality rates for these patients artificially improved from 2.08 to 1.50 mortalities per 100 individuals when the Gleason score was standardized (19). Therefore, greater care may be required when comparing current data to that reported in previous studies.
In addition to the combination of ADT followed by EBRT, the administration of EBRT followed by ADT has been demonstrated to provide improved clinical outcomes compared with EBRT alone (4–6). However, these results were reported in trials that enrolled patients with more favorable prostate cancer risk factors compared with other trials of combined ADT and EBRT. Furthermore, the duration of ADT varied, lasting for four (6), six (5) and 36 (4) months. Whilst these studies demonstrated that EBRT plus long-term androgen suppression may improve the survival of prostate cancer patients, no evidence was provided with regard to the optimal duration of androgen suppression.
The Radiation Therapy Oncology Group (RTOG) 92–02 (20) and European Organization for Research and Treatment of Cancer (EORTC) 22961 (9) trials addressed the issue of the optimal duration of ADT. The RTOG 92–02 trial compared disease-free and overall survival times between patients treated with ADT for 4 or 24 months. The latter resulted in significantly longer disease-free survival times, but not overall survival times. However, a statistically significant difference in overall survival time was observed in a subset analysis of patients with tumors of Gleason scores of 8–10. The EORTC 22961 trial investigated whether six months of ADT was as efficacious as 36 months of ADT with respect to overall survival (9). The results indicated that survival associated with six months of ADT combined with EBRT was inferior to survival with 36 months of ADT combined with EBRT. These results are consistent with the findings of the present study and indicate that long-term ADT is an appropriate treatment strategy, particularly for high-risk prostate cancer patients.
Treatment with ADT should be adopted with caution, as it may induce a number of morbidities, including myocardial infarction (7). For example, five patients in the short-term ADT group of the present study experienced exacerbated cardiovascular disease; however, retrospective data of >5,000 patients has demonstrated that ADT was not associated with induced cardiovascular disease if patients had no existing comorbidities (21). D'Amico et al (7) reported that the duration of ADT was not associated with myocardial infarction, but that it was associated with older age, indicating that ADT may be used with caution for the treatment of older patients or those exhibiting cardiovascular disease, regardless of ADT duration.
Based on a previous study conducted at the Fox Chase Cancer Center, Feigenberg et al (8) reported that the use of long-term ADT increased the incidence of late gastrointestinal and genitourinary morbidity of grade II or over. Furthermore, the RTOG 92–02 trial indicated that long-term ADT marginally increased the rate of late toxicities (20). With respect to increased toxicities in patients treated with long-term ADT, the present findings were consistent with these previous studies.
In the current study, irradiation to the pelvic node was the most frequent type of EBRT (90% of patients), followed by irradiation to the prostate only; however, multivariate analysis revealed that long-term ADT was the only significant prognostic factor for the progression-free survival of high-risk prostate cancer patients. Numerous trial protocols for high-risk prostate cancer patients have specified the irradiation of pelvic lymph nodes at a dose of 45 or 50 Gy (4,5,9,17,18,20), however, the RTOG 94–13 trial did not report improved disease outcomes upon using pelvic lymph node and prostate irradiation compared with irradiation of the prostate alone (22). Thus, pelvic lymph node irradiation was not determined to provide any clinical benefit.
In conclusion, in the present study, EBRT combined with ≥36 months of ADT for patients with high-risk localized prostate cancer resulted in prolonged biochemical and progression-free survival compared to EBRT combined with a shorter duration of ADT, and exhibited an acceptable toxicity profile.
References
- 1.Watanabe H. Mass screening program for prostatic cancer in Japan. Int J Clin Oncol. 2001;6:66–73. doi: 10.1007/pl00023927. [DOI] [PubMed] [Google Scholar]
- 2.Ogawa K, Nakamura K, Onishi H, et al. Japanese Patterns of Care Study Working Subgroup of Prostate Cancer: Radical external beam radiotherapy for prostate cancer in Japan: results of the 1999–2001 patterns of care process survey. Jpn J Clin Oncol. 2006;36:40–45. doi: 10.1093/jjco/hyi216. [DOI] [PubMed] [Google Scholar]
- 3.Marugame T, Mizuno S. Comparison of prostate cancer mortality in five countries: France, Italy, Japan, UK and USA from the WHO mortality database (1960–2000) Jpn J Clin Oncol. 2005;35:690–691. doi: 10.1093/jjco/hyi185. [DOI] [PubMed] [Google Scholar]
- 4.Bolla M, Van Tienhoven G, Warde P, et al. External irradiation with or without long-term androgen suppression for prostate cancer with high metastatic risk: 10-year results of an EORTC randomised study. Lancet Oncol. 2010;11:1066–1073. doi: 10.1016/S1470-2045(10)70223-0. [DOI] [PubMed] [Google Scholar]
- 5.D'Amico AV, Chen MH, Renshaw AA, Loffredo M, Kantoff PW. Androgen suppression and radiation vs. radiation alone for prostate cancer: a randomized trial. JAMA. 2008;299:289–295. doi: 10.1001/jama.299.3.289. [DOI] [PubMed] [Google Scholar]
- 6.Jones CU, Hunt D, McGowan DG, et al. Radiotherapy and short-term androgen deprivation for localized prostate cancer. N Engl J Med. 2011;365:107–118. doi: 10.1056/NEJMoa1012348. [DOI] [PubMed] [Google Scholar]
- 7.D'Amico AV, Denham JW, Crook J, et al. Influence of androgen suppression therapy for prostate cancer on the frequency and timing of fatal myocardial infarctions. J Clin Oncol. 2007;25:2420–2425. doi: 10.1200/JCO.2006.09.3369. [DOI] [PubMed] [Google Scholar]
- 8.Feigenberg SJ, Hanlon AL, Horwitz EM, Uzzo RG, Eisenberg D, Pollack A. Long-term androgen deprivation increases Grade 2 and higher late morbidity in prostate cancer patients treated with three-dimensional conformal radiation therapy. Int J Radiat Oncol Biol Phys. 2005;62:397–405. doi: 10.1016/j.ijrobp.2004.10.021. [DOI] [PubMed] [Google Scholar]
- 9.Bolla M, de Reijke TM, Van Tienhoven G, et al. EORTC Radiation Oncology Group and Genito-Urinary Tract Cancer Group: Duration of androgen suppression in the treatment of prostate cancer. N Engl J Med. 2009;360:2516–2527. doi: 10.1056/NEJMoa0810095. [DOI] [PubMed] [Google Scholar]
- 10.Kuban DA, Thames HD, Levy LB, et al. Long-term multi-institutional analysis of stage T1-T2 prostate cancer treated with radiotherapy in the PSA era. Int J Radiat Oncol Biol Phys. 2003;57:915–928. doi: 10.1016/S0360-3016(03)00632-1. [DOI] [PubMed] [Google Scholar]
- 11.Sobin LH, Wittekind CH, editors. International Union Against Cancer (UICC) TNM Classification of Malignant Tumors. 6th. Wiley; New York, NY: 2002. [Google Scholar]
- 12.Roach M, III, Hanks G, Thames H, Jr, et al. Defining biochemical failure following radiotherapy with or without hormonal therapy in men with clinically localized prostate cancer: recommendations of the RTOG-ASTRO Phoenix Consensus Conference. Int J Radiat Oncol Biol Phys. 2006;65:965–974. doi: 10.1016/j.ijrobp.2006.04.029. [DOI] [PubMed] [Google Scholar]
- 13.Trotti A, Colevas AD, Setser A, et al. CTCAE v3.0: development of a comprehensive grading system for the adverse effects of cancer treatment. Semin Radiat Oncol. 2003;13:176–181. doi: 10.1016/S1053-4296(03)00031-6. [DOI] [PubMed] [Google Scholar]
- 14.Oken MM, Creech RH, Tormey DC, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5:649–655. doi: 10.1097/00000421-198212000-00014. [DOI] [PubMed] [Google Scholar]
- 15.Epstein JI, Allsbrook WC, Jr, Amin MB, Egevad LL. ISUP Grading Committee: The 2005 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostatic Carcinoma. Am J Surg Pathol. 2005;29:1228–1242. doi: 10.1097/01.pas.0000173646.99337.b1. [DOI] [PubMed] [Google Scholar]
- 16.Mottet N, Peneau M, Mazeron JJ, Molinie V, Richaud P. Addition of radiotherapy to long-term androgen deprivation in locally advanced prostate cancer: an open randomised phase 3 trial. Eur Urol. 2012;62:213–219. doi: 10.1016/j.eururo.2012.03.053. [DOI] [PubMed] [Google Scholar]
- 17.Warde P, Mason M, Ding K, et al. NCIC CTG PR.3/MRC UK PR07 Investigators: Combined androgen deprivation therapy and radiation therapy for locally advanced prostate cancer: a randomised, phase 3 trial. Lancet. 2011;378:2104–2111. doi: 10.1016/S0140-6736(11)61095-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Widmark A, Klepp O, Solberg A, et al. Scandinavian Prostate Cancer Group Study 7; Swedish Association for Urological Oncology 3: Endocrine treatment, with or without radiotherapy, in locally advanced prostate cancer (SPCG-7/SFUO-3): an open randomised phase III trial. Lancet. 2009;373:301–308. doi: 10.1016/S0140-6736(08)61815-2. [DOI] [PubMed] [Google Scholar]
- 19.Albertsen PC, Hanley JA, Barrows GH, et al. Prostate cancer and the Will Rogers phenomenon. J Natl Cancer Inst. 2005;97:1248–1253. doi: 10.1093/jnci/dji248. [DOI] [PubMed] [Google Scholar]
- 20.Horwitz EM, Bae K, Hanks GE, et al. Ten-year follow-up of radiation therapy oncology group protocol 92–02: a phase III trial of the duration of elective androgen deprivation in locally advanced prostate cancer. J Clin Oncol. 2008;26:2497–2504. doi: 10.1200/JCO.2007.14.9021. [DOI] [PubMed] [Google Scholar]
- 21.Nanda A, Chen MH, Braccioforte MH, Moran BJ, D'Amico AV. Hormonal therapy use for prostate cancer and mortality in men with coronary artery disease-induced congestive heart failure or myocardial infarction. JAMA. 2009;302:866–873. doi: 10.1001/jama.2009.1137. [DOI] [PubMed] [Google Scholar]
- 22.Lawton CA, DeSilvio M, Roach M, III, et al. An update of the phase III trial comparing whole pelvic to prostate only radiotherapy and neoadjuvant to adjuvant total androgen suppression: updated analysis of RTOG 94–13, with emphasis on unexpected hormone/radiation interactions. Int J Radiat Oncol Biol Phys. 2007;69:646–655. doi: 10.1016/j.ijrobp.2007.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]