Abstract
MicroRNA-23a (miR-23a) is a potential biomarker for laryngeal cancer. Apoptotic protease activating factor 1 (APAF-1) was recently demonstrated to be a target of miR-23a. However, whether miR-23a exerts its effects via APAF-1 in laryngeal cancer, remains unknown. In the present study, miR-23a expression was detected by reverse transcription-quantitative polymerase chain reaction (RT-qPCR). APAF-1 mRNA and protein expression levels were assayed by RT-qPCR and western blotting, respectively. Binding of miR-23a to APAF-1 was monitored by a luciferase reporter assay. Gain-of-function and loss-of-function studies were performed in order to investigate the roles of miR-23a and APAF-1 in Hep2 cell proliferation and apoptosis. miR-23a and APAF-1 were found to be significantly upregulated and downregulated, respectively, in laryngeal cancer tissues, and there was a significant negative correlation between APAF-1 and miR-23a expression. The results of the luciferase reporter assay demonstrated that miR-23a bound directly to the APAF-1 mRNA 3′-untranslated region. Ectopic expression of miR-23a and knockdown of APAF-1 significantly promoted cell proliferation and colony formation, and inhibited early apoptosis in Hep2 cells. In conclusion, miR-23a acts as an oncogenic regulator in laryngeal carcinoma by directly targeting APAF-1, and may be a useful biomarker in the diagnosis and treatment of laryngeal carcinoma.
Keywords: laryngeal squamous cell carcinoma, microRNA-23a, apoptotic protease activating factor 1, proliferation, apoptosis
Introduction
Laryngeal cancer is one of the most common and lethal head and neck carcinomas, worldwide (1). More than 90% of laryngeal cancer is pathologically identified as laryngeal squamous cell carcinoma (LSCC) (2). Despite numerous advances in the diagnosis and treatment of this disease, the overall survival rate has changed little over recent decades, in part due to a lack of reliable biomarkers (3). Therefore, investigation of the molecular mechanisms underlying the development and progression of LSCC, may help to identify novel molecular targets for the treatment and diagnosis of LSCC.
MicroRNAs (miRNAs) are a novel type of biomarker, and are potential therapeutic targets for various diseases, including cancer (4). They belong to a class of small non-coding RNAs, and regulate expression of their targets through inhibition of the translation or the degradation of their corresponding mRNA targets. Approximately 30% of mRNAs are predicted to be targeted by miRNAs (5). A number of studies have demonstrated that specific miRNAs are aberrantly expressed in different types of cancer, such as leukemia, breast cancer and colorectal cancer (6–8). These miRNAs are involved in tumorigenesis, either as proto-oncogenes or as tumor suppressors, depending on their targets (9).
Several studies have shown that aberrant expression of miR-23a occurs in a variety of types of cancer, indicating that it is involved in oncogenesis. Notably, miR-23a may produce opposite effects in different types of cancer. For example, miR-23a is downregulated in oral squamous cell carcinoma (OSCC), acute promyelocytic leukemia and colon cancer (10–12). By contrast, miR-23a is overexpressed in acute lymphoblastic leukemia, glioblastoma and hepatocellular carcinoma (13–15). Li et al (16) reported that miR-23a is a candidate biomarker of laryngeal cancer, following their analysis of DNA microarrays-based microRNA expression profiles. However, the mechanisms underlying the effects of miR-23a in laryngeal cancer remain to be elucidated.
Recently, apoptotic protease activating factor-1 (APAF-1) was confirmed as a target of miR-23a (17–19). APAF-1 is frequently downregulated in a number of types of cancer, such as colorectal and lung cancer, which indicates that it participates in tumorigenesis (20–21). A previous study by our group, demonstrated that APAF-1 is downregulated in laryngeal carcinoma (22). In addition to loss of heterozygosity, it was also shown that promoter methylation decreases APAF-1 expression in human leukemia, thereby indicating a second inactivation mechanism of APAF-1 in cancer (23).
In the present study, the association between miR-23a and APAF-1 expression in LSCC was analyzed, and the binding of miR-23a to APAF-1 was assayed. The functions of miR-23a and APAF-1 in laryngeal cancer cell proliferation and apoptosis were also evaluated.
Materials and methods
Patient tissues, cell culture and nucleotide sequences
Tissue specimens, which included tumor tissues in addition to paired normal adjacent tissues from 82 patients with LSCC recruited from the Otolaryngology department of the No. 463 Hospital of PLA, were collected after patients had provided informed consent. Pathological diagnosis of the specimens was performed by a pathologist. Laryngeal cancer tissues were immediately frozen at −80°C, following removal from the patients. Hep2 human laryngeal cancer and HEK293 human embryonic kidney cell lines were obtained from the Cell Biology Institute of Shanghai, Chinese Academy of Science (Shanghai, China) and were maintained in RPMI 1640 (Gibco Life Technologies, Los Angeles, CA, USA) with 10% fetal bovine serum (Hyclone, Logan, UT, USA), 100 units/ml penicillin and 100 µg/ml streptomycin (Beyotime Institute of Biotechnology, Haimen, China) in a humidified atmosphere at 37°C with 5% CO2. All nucleotide sequences used in the study are shown in Table I. Approval for the study was received from the ethical board of China Medical University (Shenyang, China).
Table I.
Nucleotide sequences.
| Name | Sequence |
|---|---|
| miR-23a mimic | 5′-AUCACAUUGCCAGGGAUUUCC-3′ |
| miR-23a inhibitor | 5′-GGAAAUCCCUGGCAAUGUGAU-3′ |
| NC mimic | 5′-UUCUCCGAACGUGUCACGUTT-3′ |
| NC inhibitor | 5′-CAGUACUUUUGUGUAGUACAA-3′ |
| NC | 5′-GGCUACGUCCAGGAGCGCA CC-3′ |
| siAPAF-1 | 5′-GACGUCUGCAACUCAUUAATT-3′ |
| miRNA-23a (reverse transcription primer) | 5′-CTCAACTGGTGTCGTGGAGTCGGCAATTCAGTTGAGGGAAATCC-3′ |
| miRNA-23a (F) | 5′-ACACTCCAGCTGGGATCACATTGCCAGGGATTT-3′ |
| miRNA-23a (R) | 5′-TGGTGTCGTGGAGTCG-3′ |
| U6 (F) | 5′-CTCGCTTCGGCAGCACA-3′ |
| U6 (R) | 5′-AACGCTTCACGAATTTGCGT-3′ |
| APAF-1 (F) | 5′-CCTCTCATTTGCTGATGTCG-3′ |
| APAF-1 (R) | 5′-TCACTGCAGATTTTCACCAGA-3′ |
| GAPDH (F) | 5′-ATCATCAGCAATGCCTCC-3′ |
| GAPDH (R) | 5′-CATCACGCCACAGTTTCC-3′ |
NC, negative control; si, small interfering; miRNA, microRNA; APAF-1, apoptotic protease activating factor 1; F, forward; R, reverse.
Small RNAs, plasmids and gene transfection
Small RNAs including an miR-23a mimic and inhibitor, negative control miRNAs and small interfering RNA (siRNA) were obtained from GenePharma (Shanghai, China). Dual-Luciferase miRNA Target Expression Vectors (GV272-APAF-1-3′UTR and GV272-APAF-1-3′UTR-mut) were also obtained from GenePharma (Shanghai, China). Gene transfection was performed in Hep2 and/or HEK293 cells, with small RNAs and/or plasmids, at a final concentration of 50 pmol, using Lipofectamine 2000™ (Invitrogen Life Technologies Carlsbad, CA, USA) according to the manufacturer's instructions.
Reverse transcription-quantitative polymerase chain reaction (RT-qPCR)
Total RNA was extracted from the corresponding tissues and cell lines using TRIzol® (Takara Bio, Inc., Dalian, China), according to the manufacturer's instructions. miRNA was separated using an miRcute miRNA isolation kit (Tiangen, Beijing, China). Concentrations of miRNA and total RNA were measured by reading the absorbance at an optical density (OD) of 260/280 nm.
In order to detect the expression of miR-23a and APAF-1 mRNA in LSCC tissues and cell lines, RT-qPCR was conducted using the ABI 7500 Real Time PCR system (Applied Biosystems, Foster City, USA). To amplify the mature miR-23a, RT was performed using the One Step PrimeScript miRNA cDNA Synthesis kit (Takara Bio, Inc.), according to the manufacturer's instructions and qPCR was conducted using SYBR® Premix Ex Taq™ II (Takara Bio, Inc.). U6 small nuclear RNA (snRNA) was used for normalization. The thermal cycling conditions for miR-23a and U6 snRNA consisted of 95°C for 30 sec, 40 cycles of 95°C for 5 sec and 60°C for 34 sec. For the detection of APAF-1 mRNA expression, RT was performed using the cDNA Synthesis kit (Takara Bio, Inc.) according to the manufacturer's instructions and qPCR was conducted using SYBR® Premix Ex Taq™ II (Takara Bio, Inc.). GAPDH was used for normalization. The conditions for amplifying APAF-1 and GAPDH mRNA were 95°C for 30 min, 40 cycles of 95°C for 5 sec and 60°C for 34 sec. ΔCt was calculated by subtracting the Ct of U6 or GAPDH mRNA from that of the mRNA of interest. ΔΔCt was then calculated by subtracting the ΔCt of the negative control from the ΔCt of the samples. The fold change in miR-23a and APAF-1 mRNA was calculated according to the equation, 2−ΔΔCt.
Western blotting
Proteins were extracted from LSCC tissues and cell lines, using a protein extraction reagent (Beyotime, Shanghai, China) and protein concentration was measured using the BCA Protein Assay kit (Beyotime, Shanghai, China). Protein (50 µg) from each sample was separated on an 8% SDS-PAGE gel (Beyotime Institute of Biotechnology) and transferred to a PVDF membrane (Beyotime Institute of Biotechnology). The membrane was then blocked with 5% non-fat milk and incubated with rabbit monoclonal anti-APAF-1 (ab32372, 1:500 dilution; Abcam, Cambridge, USA) and mouse monoclonal anti-α-tubulin (BM1452; 1:500 dilution; Boster, Wuhan, China) for normalization followed by by incubation at 37°C for 60 min with horseradish peroxidase-conjugated antibody (1:2,000 dilution; ZhongShan, Beijing, China). The membrane was stained with ECL Plus (Beyotime Institute of Biotechnology), according to the manufacturer's instructions and exposed to a film (Fuji, Japan).
Luciferase reporter assay
HEK293 cells, seeded in 96-well plates in triplicate, were cotransfected with GV272-APAF-1-3′UTR or GV272-APAF-1-3′UTR-mut, and miRNA-23a mimic or non-relative control RNA duplex, using Lipofectamine 2000 (Invitrogen LIfe Technologies, Carlsbad, CA, USA) according to the manufacturer's instructions. The pRL-TK (Promega Corporation, Madison, WI, USA) was used for normalization. Cells were collected 24 h after transfection. Luciferase activity was measured using a dual-luciferase reporter assay kit (Promega Corporation) and recorded using a Chemiluminescence meter (Promega Corporation).
Cell proliferation assay
Hep2 cells were grown in 6-well plates to ~60% confluency and transiently transfected as described for the HEK293 cells. Following transfection, 2–3×103 Hep2 cells were seeded into 96-well plates in triplicate. Cells were then cultured for 1, 2, 3, 4 or 5 days. Absorbance at 490 nm was measured, following incubation of the cells with 100 µl of sterile MTT dye (0.5 mg/ml, Sigma, Ronkonkoma, NY, USA) for 4 h at 37°C and 150 µl DMSO for 15 min. The cell growth curve was constructed using the values at OD490 nm as ordinate axis.
Colony formation assay
At 12 h post-transfection, 3–5×103 Hep2 cells were seeded into 60-mm Petri dishes in triplicate and maintained in RPMI 1640 (GIBCO, Los Angeles, USA) with 10% fetal bovine serum. After 14 d, colonies were fixed with methanol for 30 min, stained with hematoxylin for 20 min, and visualized under a microscope (Olympus BX5, Olympus Corporation, Tokyo, Japan). Colonies was counted and calculated in relation to the values obtained from the mock and scramble-treated controls.
Apoptosis assay
Hep2 cells were grown in 6-well plates to ~60% confluence and transiently transfected with corresponding small RNAs using Lipofectamine 2000. Cells were digested and collected at 48 h post-transfection, and washed twice with PBS. Cells were then stained with Annexin V-EGFP, according to the manufacturer's instructions (KeyGEN, Nanjing, China) and apoptotic cells were quantified using flow cytometry (FACS calibur, Becton-Dickinson, Franklin Lakes, USA).
Statistical analysis
Data are presented as the mean ± standard deviation. Differences were assessed by one-way analysis of variance and Student's unpaired t-test, using SPSS 17.0 (SPSS Inc., Chicago, IL, USA). P<0.05 was considered to indicate a statistically significant difference.
Results
miR-23a and APAF-1 are involved in LSCC development
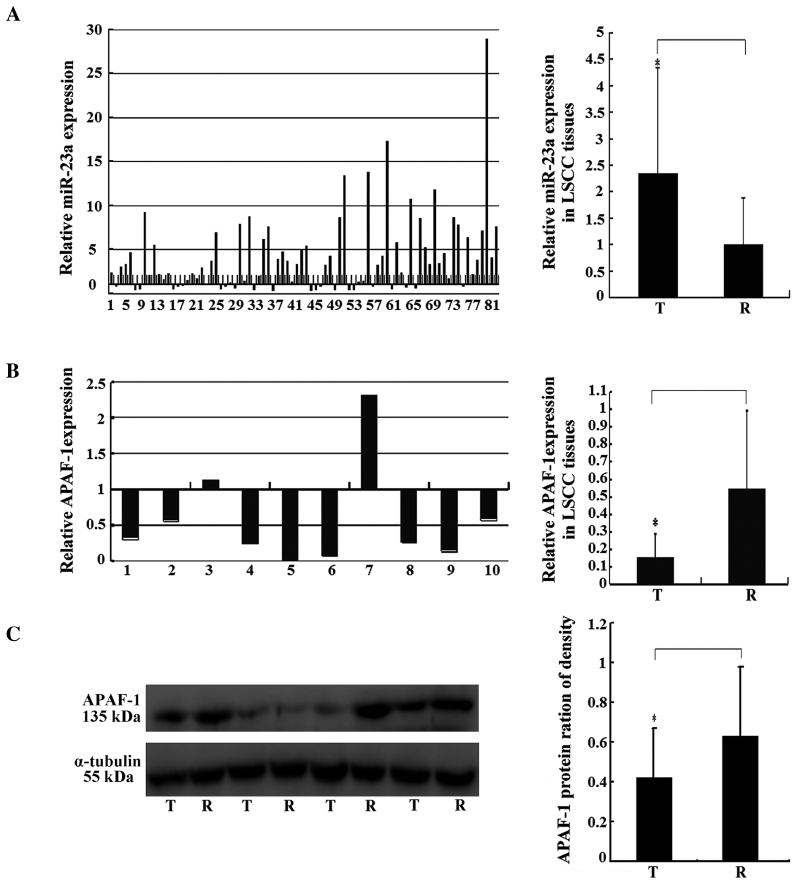
The results from the RT-qPCR assay, demonstrated that miR-23 was upregulated in 72.8% (59 of 82) cases of laryngeal cancer and the results of statistical analysis showed that miR-23a expression was significantly higher in LSCC tissues than that in adjacent normal tissues (Fig. 1), suggesting that miR-23a is involved in laryngeal oncogenesis.
Figure 1.
miR-23a and APAF-1 gene expression in LSCC. (A) miR-23a expression in 82 pairs of LSCC tissues, analyzed by RT-qPCR. The y-axis indicates the ratio of relative miR-23a expression in cancer tissues to that in paired normal adjacent tissues. The relative expression was calculated as the ratio of miR-23a to the internal control, using the equation RQ=2−ΔΔCT in each sample. The x-axis represents the number of the paired samples used in the study. (B) Relative mRNA expression levels of APAF-1 in the miRNA-23a-upregulated LSCC tissues, analyzed by RT-qPCR. The y-axis indicates the ratio of relative APAF-1 mRNA expression in cancer tissues to that in paired normal adjacent tissues. The relative expression was calculated as the ratio of APAF-1 to the internal control using the equation RQ=2−ΔΔCT in each sample. The x-axis represents the number of the paired samples used in the study. (C) Relative protein expression levels of APAF-1 in the miRNA-23a-upregulated LSCC tissues, analyzed by western blotting. α-tubulin was used as the internal control. All data are expressed as the mean ± standard deviation of three independent experiments. *P<0.05. miRNA, microRNA; APAF-1, apoptotic protease activating factor 1; LSCC, laryngeal squamous cell carcinoma; RT-qPCR, reverse transcription-quantitative polymerase chain reaction; T, tumor sample; R, paired normal adjacent sample.
In order to investigate the association between miR-23a and APAF-1 expression in LSCC, 10 pairs of LSCC tissues, in which miR-23a was upregulated, were randomly selected, and APAF-1 expression in these samples was evaluated. RT-qPCR and western blotting results showed that APAF-1 expression was significantly downregulated at the mRNA and protein levels in cancer tissues, compared with that in the normal controls (Fig. 1B and C). The results of statistical analysis, demonstrated that miR-23a expression was negatively correlated with APAF-1 expression in LSCC tissues (Table II).
Table II.
Correlation between miRNA-23a and APAF-1 expression in laryngeal cancer tissues.
| Statistical parameter | APAF-1 mRNA (n=10) | APAF-1 protein (n=10) |
|---|---|---|
| R-value | −0.697 | −0.633 |
| P-value | 0.025 | 0.049 |
APAF-1, apoptotic protease activating factor 1; miRNA, microRNA.
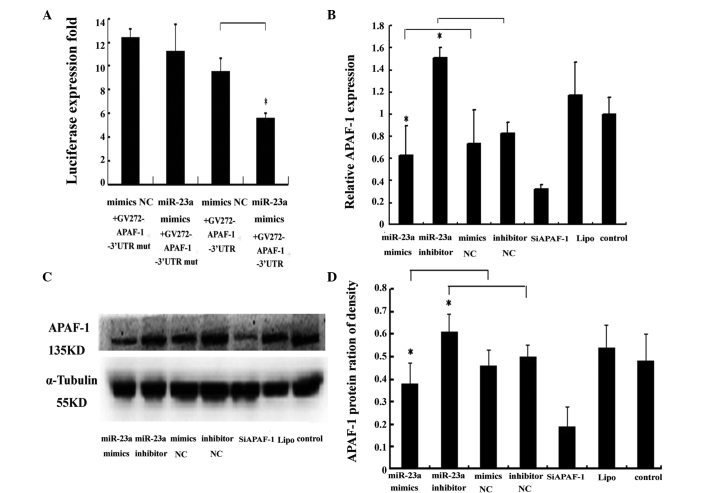
APAF-1 mRNA is a direct target of miR-23a
As illustrated in Fig. 2A, cotransfection of the APAF-1 3′ untranslated region (UTR) luciferase reporter and the miRNA-23a mimic into the HEK293 cells, resulted in a significant reduction in luciferase activity in comparison with the control groups (P<0.01). These results confirmed the hypothesis that miR-23a binds to the APAF-1 3′UTR. Western blotting and RT-qPCR results indicated that miR-23a significantly decreased APAF-1 expression at the mRNA and protein levels in Hep2 cells (Fig. 2B and C). APAF-1 expression was also significantly inhibited by APAF-1-specific siRNA, at the mRNA and protein levels in Hep2 cells (Fig. 2B and C). These results suggest that miR-23a negatively regulates APAF-1 expression, by binding the 3′UTR nucleotides of this gene in laryngeal cancer tissues.
Figure 2.
Validation of APAF-1 as a direct target of miR-23a. (A) Binding of miRNA-23a to the APAF-1 3′-UTR in HEK293 human embryonic kidney cells. The luciferase activity of HEK293 cells cotransfected with different constructs was detected. Each value of luciferase activity was calculated as the ratio of firefly to Renilla. (B) Effect of miR-23a and siAPAF-1 on APAF-1 mRNA expression in Hep2 human laryngeal cancer cells. Following transfection of the Hep-2 cells, APAF-1 mRNA expression was measured using RT-qPCR. The relative expression was calculated as the ratio of APAF-1 to the internal control, using the equation RQ=2−ΔΔCT for each sample. (C) Effect of miR-23a and siAPAF-1 on APAF-1 protein expression in Hep2 cells. Following transfection of the Hep2 cells, APAF-1 protein expression was detected by western blotting. α-tubulin was used as the internal control. Data are presented as the mean ± standard deviation of three independent experiments. *P<0.05. APAF-1, apoptotic protease activating factor 1; miRNA, microRNA; NC, normal control; UTR, untranslated region; si, small interfering; RT-qPCR, reverse transcription-quantitative polymerase chain reaction.
miR-23a and siAPAF-1 promote Hep2 cell proliferation and inhibit apoptosis
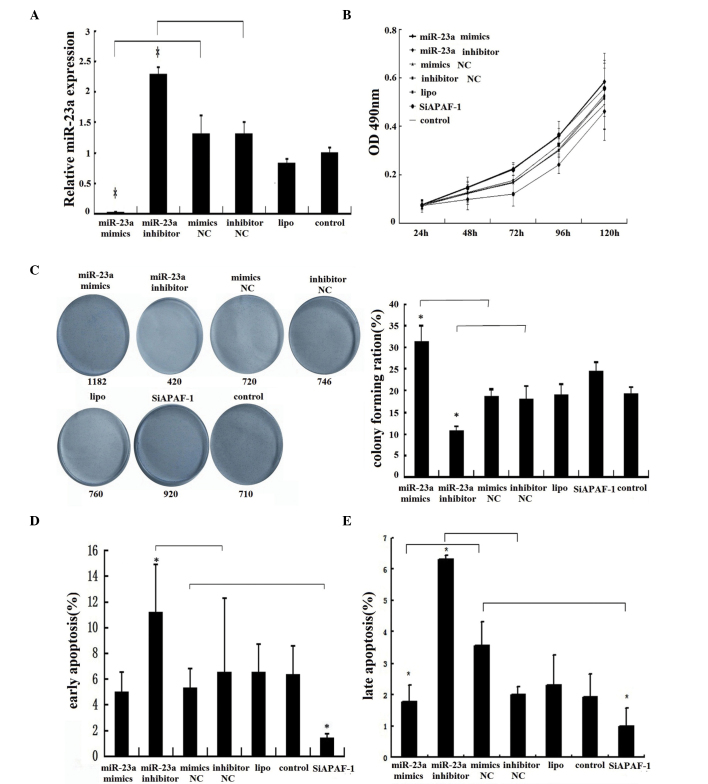
miR-23a expression was significantly higher and lower than that in the control group, in the miR-23a mimic and inhibitor groups, respectively, suggesting that transfection was successful (Fig. 3A). The MTT assay results indicated that the miR-23a mimic and inhibitor, significantly increased and decreased Hep2 cell viability, respectively, compared with the control group (Fig. 3B). In order to determine the effects of miR-23a on long-term and independent growth activity, a colony formation assay was performed. Colony formation assay results demonstrated that Hep2 cells transfected with the miR-23a-mimic or miR-23a-inhibitor exhibited significantly higher and lower colony-forming ability, respectively, compared with the controls (Fig. 3C). The flow cytometry assay results indicated that the early apoptotic rate was significantly increased in the miR 23a inhibitor group compared with the control group. However, no significant difference was observed between the miR-23a mimic group and the control group (Fig. 3D). In addition, the late apoptotic rate was significantly increased in the miR-23a inhibitor group and reduced in the miR-23a mimic group when compared with the controls, respectively (Fig. 3E). However, no significant differences in early or late apoptosis were detected in the miR-23a mimic group compared with the control group (Fig. 3D and E). It was hypothesized that there may be an abundant expression of internal miR-23a in human Hep2 cells (Fig. 3A). In a similar manner to the effect of miR-23a on Hep2 cells, knockdown of the APAF-1 gene significantly promoted cell viability (Fig. 3B) and colony formation (Fig. 3C), and inhibited early and late apoptosis in Hep2 cells (Fig. 3D and E), suggesting that miR-23a functions in Hep2 cells, at least in part via downregulation of APAF-1 expression.
Figure 3.
Regulation of miR-23a and siAPAF-1 in Hep2 human laryngeal cancer cell proliferation and apoptosis. (A) miR-23a expression levels of Hep2 cells in different groups. Following transfection of the Hep2 cells by different small RNAs, including miR-23a mimics, miR-23a inhibitor, mimics NC, inhibitor NC and siAPAF-1, the miR-23a expression was measured using RT-qPCR. (B) Effects of miR-23a and siAPAF-1 on Hep2 cell proliferation. Hep2 cells were transfected with the various small RNAs and cell proliferation was detected using an MTT assay. (C) Effects of miR-23a and siAPAF-1 on Hep2 cell colony formation. Hep2 cells were transfected with the various small RNAs and the colony-forming ability was detected using a colony formation assay. (D) and (E) Effects of miR-23a and siAPAF-1 on early and late apoptosis in the Hep2 cells. Hep2 cells were transfected with the various small RNAs and then stained by Annexin V-EGFP, according to the manufacturer's instructions. The apoptotic cells in the different groups were monitored using a flow cytometer. Data are presented as the mean ± standard deviation from three independent experiments. *P<0.05. miRNA, microRNA; siAPAF-1, small interfering RNA specific to apoptotic protease activating factor 1; RT-qPCR, reverse transcription-quantitative polymerase chain reaction; NC, normal control; lipo, Lipofectamine.
Discussion
As outlined in the introduction, miR-23a is aberrantly upregulated or downregulated in a number of types of cancer, indicating that it is involved in oncogenesis.
In the present study, miR-23a was found to be significantly overexpressed in laryngeal cancer tissues compared with normal controls, suggesting that it acts as an oncogene in the development of LSCC. In addition, APAF-1 was shown to be downregulated in LSCC tissues compared with the control tissues, and a negative correlation between miR-23a and APAF-1 expression was demonstrated in LSCC tissues. The present study also confirmed that APAF-1 is a direct target of miR-23a. Furthermore, miR-23a inhibited APAF-1 expression at the mRNA and protein levels in Hep2 cells, indicating that the degradation of APAF-1 mRNA, which may be mediated by miR-23a, contributes to the decreased expression levels of APAF-1 observed in LSCC.
As two of the ten hallmarks of cancer, sustaining proliferation and resisting cell death, are known to be important in carcinogenesis (24–25). Studies have shown that miRNAs are involved in the regulation of cancer cell proliferation and apoptosis (26–27).
The present study demonstrated that miR-23a significantly promoted Hep2 cell proliferation, while its antisense inhibitor partially reversed this effect. It was hypothesized that this enhanced proliferation may be due to an effect on cell cycle control or to the inhibition of apoptosis. However, the miR-23a inhibitor significantly increased early apoptosis in Hep2 cells, and it is suggested that low levels of apoptosis, are, in part, responsible for the high level of proliferation observed in Hep2 cells. The intrinsic apoptotic pathway is also termed the mitochondrial apoptotic pathway, and responds to intracellular signals, such as DNA damage (28). APAF-1 is a key regulator of the mitochondrial apoptotic pathway and of the central element of the multimeric apoptosome formed by procaspase 9, cytochrome c, and thus, is itself involved in the initiation and progression of cancer (29).
The study also demonstrated that silencing of APAF-1 significantly increased proliferation, and decreased early and late apoptosis in Hep2 cells. It was also shown that miR-23a significantly inhibited APAF-1 expression in Hep2 cells, suggesting that a high level of miR-23a partially represses APAF-1 expression, leading to increased early apoptosis in LSCC. In accordance with these results, miR-23a has been shown to promote glioma cell growth and to suppress cell apoptosis, by targeting APAF1 (18).
In conclusion, miR-23a is involved in the development of LSCC, acting as a pro-proliferative and antiapoptotic regulator, at least in part through direct targeting of the APAF-1 3′UTR. Whether miR-23a also regulates cancer cell proliferation via other targets, requires further investigation. Future studies by this group will also focus on the clinical application of miR-23a as a biomarker in the diagnosis and treatment of laryngeal carcinoma.
Acknowledgements
This study was supported by the National Natural Science Foundations of China (grant nos. 81172577, 81372876 and 81301767).
References
- 1.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013;63:11–30. doi: 10.3322/caac.21166. [DOI] [PubMed] [Google Scholar]
- 2.Morshed K, Polz-Dacewicz M, Szymański M, Polz D. Short-fragment PCR assay for highly sensitive broad-spectrum detection of human papillomaviruses in laryngeal squamous cell carcinoma and normal mucosa: Clinico-pathological evaluation. Eur Arch Otorhinolaryngol. 2008;265(Suppl 1):S89–S96. doi: 10.1007/s00405-007-0569-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang W, Lin P, Han C, Cai W, Zhao X, Sun B. Vasculogenic mimicry contributes to lymph node metastasis of laryngeal squamous cell carcinoma. J Exp Clin Cancer Res. 2010;29:60. doi: 10.1186/1756-9966-29-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li J, Tan S, Kooger R, Zhang C, Zhang Y. MicroRNAs as novel biological targets for detection and regulation. Chem Soc Rev. 2014;43:506–517. doi: 10.1039/C3CS60312A. [DOI] [PubMed] [Google Scholar]
- 5.Bhatt K, Mi QS, Dong Z. MicroRNAs in kidneys: Biogenesis, regulation and pathophysiological roles. Am J Physiol Renal Physiol. 2011;300:F602–F610. doi: 10.1152/ajprenal.00727.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Calin GA, Liu CG, Sevignani C, et al. MicroRNA profiling reveals distinct signatures in B cell chronic lymphocytic leukemias. Proc Natl Acad Sci USA. 2004;101:11755–11760. doi: 10.1073/pnas.0404432101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bhaumik D, Scott GK, Schokrpur S, Patil CK, Campisi J, Benz CC. Expression of microRNA-146 suppresses NF-kappaB activity with reduction of metastatic potential in breast cancer cells. Oncogene. 2008;27:5643–5647. doi: 10.1038/onc.2008.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Michael MZ, O'Connor SM, van Holst Pellekaan NG, Young GP, James RJ. Reduced accumulation of specific microRNAs in colorectal neoplasia. Mol Cancer Res. 2003;1:882–891. [PubMed] [Google Scholar]
- 9.Zhang B, Pan X, Cobb GP, Anderson TA. microRNAs as oncogenes and tumor suppressors. Dev Biol. 2007;302:1–12. doi: 10.1016/j.ydbio.2006.08.028. [DOI] [PubMed] [Google Scholar]
- 10.Kozaki K, Imoto I, Mogi S, Omura K, Inazawa J. Exploration of tumor-suppressive microRNAs silenced by DNA hypermethylation in oral cancer. Cancer Res. 2008;68:2094–2105. doi: 10.1158/0008-5472.CAN-07-5194. [DOI] [PubMed] [Google Scholar]
- 11.Saumet A, Vetter G, Bouttier M, et al. Transcriptional repression of microRNA genes by PML-RARA increases expression of key cancer proteins in acute promyelocytic leukemia. Blood. 2009;113:412–421. doi: 10.1182/blood-2008-05-158139. [DOI] [PubMed] [Google Scholar]
- 12.Xi Y, Shalgi R, Fodstad O, Pilpel Y, Ju J. Differentially regulated micro-RNAs and actively translated messenger RNA transcripts by tumor suppressor p53 in colon cancer. Clin Cancer Res. 2006;12:2014–2024. doi: 10.1158/1078-0432.CCR-05-1853. [DOI] [PubMed] [Google Scholar]
- 13.Mi S, Lu J, Sun M, et al. MicroRNA expression signatures accurately discriminate acute lymphoblastic leukemia from acute myeloid leukemia. Proc Natl Acad Sci USA. 2007;104:19971–19976. doi: 10.1073/pnas.0709313104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ciafrè SA, Galardi S, Mangiola A, et al. Extensive modulation of a set of microRNAs in primary glioblastoma. Biochem Biophys Res Commun. 2005;334:1351–1358. doi: 10.1016/j.bbrc.2005.07.030. [DOI] [PubMed] [Google Scholar]
- 15.Huang S, He X, Ding J, et al. Upregulation of miR-23a approximately 27a approximately 24 decreases transforming growth factor-beta-induced tumor-suppressive activities in human hepatocellular carcinoma cells. Int J Cancer. 2008;123:972–978. doi: 10.1002/ijc.23580. [DOI] [PubMed] [Google Scholar]
- 16.Li L, Zhang ZM, Liu Y, et al. DNA microarrays-based microRNA expression profiles derived from formalin-fixed paraffin-embedded tissue blocks of squammous cell carcinoma of larynx. Zhonghua Bing Li Xue Za Zhi. 2010;39:391–395. (In Chinese) [PubMed] [Google Scholar]
- 17.Chen Q, Xu J, Li L, et al. MicroRNA-23a/b and microRNA-27a/b suppress Apaf-1 protein and alleviate hypoxia-induced neuronal apoptosis. Cell Death Dis. 2014;5:e1132. doi: 10.1038/cddis.2014.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lian S, Shi R, Bai T, et al. Anti-miRNA-23a oligonucleotide suppresses glioma cells growth by targeting apoptotic protease activating factor-1. Curr Pharm Des. 2013;19:6382–6389. doi: 10.2174/13816128113199990509. [DOI] [PubMed] [Google Scholar]
- 19.Shang J, Yang F, Wang Y, et al. MicroRNA-23a antisense enhances 5-fluorouracil chemosensitivity through APAF-1/caspase-9 apoptotic pathway in colorectal cancer cells. J Cell Biochem. 2014;115:772–784. doi: 10.1002/jcb.24721. [DOI] [PubMed] [Google Scholar]
- 20.Huerta S, Heinzerling JH, Anguiano-Hernandez YM, et al. Modification of gene products involved in resistance to apoptosis in metastatic colon cancer cells: Roles of Fas, Apaf-1, NF kappaB, IAPs, Smac/DIABLO and AIF. J Surg Res. 2007;142:184–194. doi: 10.1016/j.jss.2006.12.551. [DOI] [PubMed] [Google Scholar]
- 21.Zang YS, Zhong YF, Fang Z, Li B, An J. MiR-155 inhibits the sensitivity of lung cancer cells to cisplatin via negative regulation of APAF-1 expression. Cancer Gene Ther. 2012;19:773–778. doi: 10.1038/cgt.2012.60. [DOI] [PubMed] [Google Scholar]
- 22.Huang DF, Fu WN, Shang C, Xu ZM, Li ZG, Sun KL. Expression and promoter methylation of Apaf-1 gene in laryngeal squamous cell carcinoma. Yi Chuan Xue Bao. 2004;31:1327–1331. (In Chinese) [PubMed] [Google Scholar]
- 23.Fu WN, Bertoni F, Kelsey SM, McElwaine SM, Cotter FE, Newland AC, Jia L. Role of DNA methylation in the suppression of Apaf-1 protein in human leukaemia. Oncogene. 2003;22:451–455. doi: 10.1038/sj.onc.1206147. [DOI] [PubMed] [Google Scholar]
- 24.Hanahan D, Weinberg RA. Hallmarks of cancer: The next generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 25.Hanahan D, Weinberg RA. The hallmarks of cancer. Cell. 2000;100:57–70. doi: 10.1016/S0092-8674(00)81683-9. [DOI] [PubMed] [Google Scholar]
- 26.Nakano H, Yamada Y, Miyazawa T, Yoshida T. Gain-of-function microRNA screens identify miR-193a regulating proliferation and apoptosis in epithelial ovarian cancer cells. Int J Oncol. 2013;42:1875–1882. doi: 10.3892/ijo.2013.1896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Christensen LL, Holm A, Rantala J, et al. Functional screening identifies miRNAs influencing apoptosis and proliferation in colorectal cancer. PLoS One. 2014;9:e96767. doi: 10.1371/journal.pone.0096767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Taylor RC, Cullen SP, Martin SJ. Apoptosis: controlled demolition at the cellular level. Nat Rev Mol Cell Biol. 2008;9:231–241. doi: 10.1038/nrm2312. [DOI] [PubMed] [Google Scholar]
- 29.Campioni M, Santini D, Tonini G, Murace R, Dragonetti E, Spugnini EP, Baldi A. Role of Apaf-1, a key regulator of apoptosis, in melanoma progression and chemoresistance. Exp Dermatol. 2005;14:811–818. doi: 10.1111/j.1600-0625.2005.00360.x. [DOI] [PubMed] [Google Scholar]