Abstract
Primary malignant melanoma (MM) of the lung is relatively rare, and no more than 40 cases have been reported in English literature. Here, we present a case of primary MM of the lung in a 60-year-old healthy asymptomatic male, detected following the observation of an abnormal shadow on a chest X-ray. Following computed tomography and bronchoscopy examinations, the patient underwent pneumonectomy. A diagnosis of melanoma was confirmed postoperatively following immunohistochemistry. The patient received adjuvant chemotherapy postoperatively for 6 months, and is living disease-free 18 months after the surgery without any major complaints. In conclusion, primary melanoma of the lung represents a rare pathological entity. The final diagnosis of a primary MM of the lung is based on clinical, radiological and pathological findings. Surgical resection remains the cornerstone of the treatment and postoperative adjuvant chemotherapy may offer the possibility of long-time survival for certain patients.
Keywords: primary malignant melanoma, lung, surgical resection
Introduction
Malignant melanoma (MM) is the most fatal cutaneous neoplasm, and usually arises as a result of uncontrolled growth of pigment cells called melanocytes of the skin (1). MM most commonly presents as a primary neoplasm of the skin, but it has also been identified in other sites, including the respiratory tract, esophagus, liver, gallbladder, ovaries, cervix, uterus, genitourinary tract and leptomeninges. Almost every occurrence of MM of the lung is metastatic in origin. Primary pulmonary MM accounts for just 0.01% of all primary pulmonary tumors (2). Approximately 35 cases have been described in the literature, and these are mostly case reports of primary MM of the lung. In particular, an extrapulmonary origin of the tumor should be convincingly ruled out by detailed examination of the sites where MM occurs frequently, including the skin or mucosa, before considering this diagnosis. In this article we present a case of primary MM of the lung in an elderly male, who was finally diagnosed by pathological examination.
Case report
A 60-year-old healthy asymptomatic man with an abnormal shadow on a chest X-ray was referred to Shandong Provincial Hospital Affiliated to Shandong University, China, for further investigation. The patient was an ex-smoker, having smoked 35 cigarettes per day between the age of 20 and 60. The patient had no respiratory complaints or other physical symptoms and no personal history of lung disease. The X-ray revealed an irregular opacity in his left lower lobe (Fig. 1). Computed tomography (CT) revealed a tumor located in the left lower lobe (Fig. 2). Bronchoscopy revealed an endobronchial mass obstructing the left lower lobe bronchus, and the results of the biopsy revealed non-small-cell lung carcinoma. The patient underwent thoracotomy and a semi-solid neoplasm was identified. A pneumonectomy with mediastinal lymph node dissection was carried out. Histologically the tumor was composed predominantly of epithelioid tumor cells; junctional change and mitotic activity with characteristic nesting of malignant cells beneath the bronchial epithelium was also observed, suggesting a diagnosis of MM. Immunohistochemical reactions supported this diagnosis with a positive melanoma cocktail of S-100 (Fig. 3), melanoma-associated monoclonal antibody HMB45 and α-smooth muscle actin, whereas cytokeratin, epithelial membrane antigen and calponin were negative. Dissected hilar and mediastinal lymph nodes were free of metastatic disease.
Figure 1.

X-ray revealing irregular opacity in the left lower lobe of the lung.
Figure 2.
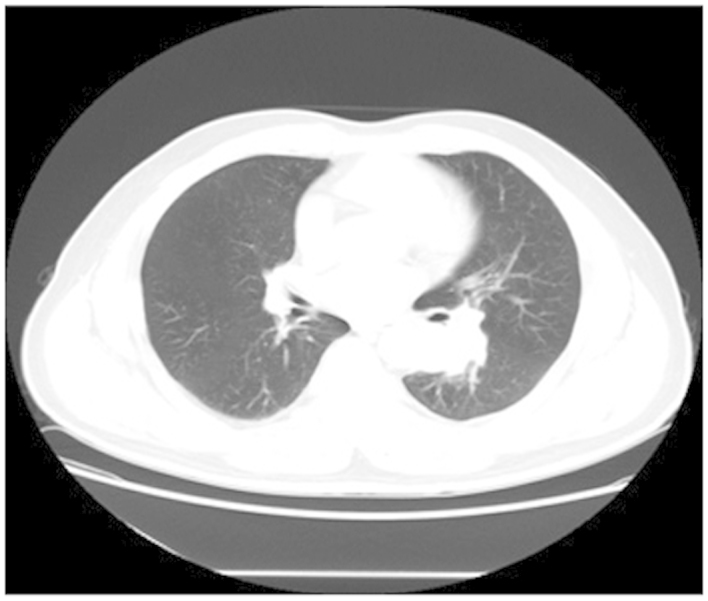
Computed tomography revealing an irregular mass located in the left lower lobe of the lung.
Figure 3.
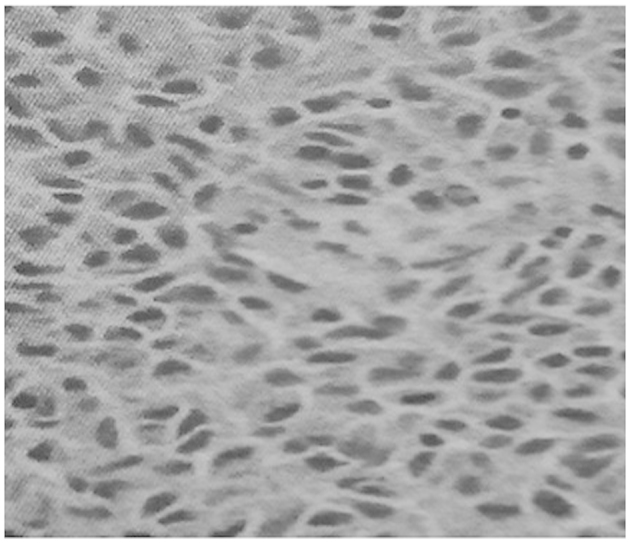
Photomicrograph demonstrating immunohistochemical staining of melanoma cells with S-100 antibody (avidin-biotin complex; magnification, x400).
Considering the possibility of pulmonary metastasis of MM, ophthalmic, skin, oral and rhinal examinations were carried out by specialists to rule out extrapulmonary disease. No additional abnormalities were observed on subsequent detailed metastatic work-up including magnetic resonance imaging of the brain, CT of the abdomen and whole-body bone scan and endoscopy (upper gastrointestinal scope, colonoscope and cystoscope). The patient received adjuvant chemotherapy postoperatively for 6 months, and is living disease-free 18 months after the surgery without any major complaints. This study was approved by the Ethics Committee of Shandong Provincial Hospital Affiliated to Shandong University (Jinan, China). Written informed consent was obtained from the patient's family.
Discussion
Primary MM of the lung is an extremely rare neoplasm that accounts for just 0.01% of all primary lung tumors. There is no precise etiology of primary MM of the lung. One possible speculation is that the tumor occurs when a certain number of epithelial cells have undergone differentiation towards melanocytes in areas of squamous metaplasia (3). No significant statistical difference in the incidence of primary MM of the lung is observed between genders. However, cigarette smoking may be a risk factor of primary MM of the lung, as cigarette smoking may cause squamous metaplasia (4).
The symptoms of MM of the lung are similar to those of bronchogenic carcinoma. It is frequently manifested with symptoms of a cough, hemoptysis, postobstructive pneumonia, lobar collapse or atelectasis. More rarely, it is identified in asymptomatic healthy patients, as in the case of our patient. Its radiological appearance is similar to that of lung cancer, manifesting as an abnormal shadow or irregular mass (5). The final diagnosis of a primary MM of the lung should be based on clinical, radiological and pathological findings. The proposed criteria for its diagnosis may be split into three groups (6–8). Clinical criteria: No previously resected pigmented skin lesion, no demonstrable melanoma in any other organ at time of surgery, solitary tumor in surgical specimen from the lung, tumor morphology comparable with that of a primary tumor. Radiological criteria: Abnormal shadow on chest X-ray, irregular mass or node on computed tomography. Pathological criteria: Invasion of the bronchial epithelium by melanoma cells, junctional changes including ‘dropping off’ or ‘nesting’ just beneath the bronchial epithelium, evident melanoma cells confirmed by immuno-histochemical staining for S-100 and HMB-45.
The optimal treatment for patients with primary MM of the lung remains to be determined. Surgical resection with an oncologically adequate margin, such as lobectomy or pneumonectomy, is usually the first choice of treatment in cases of primary MM of the lung with no distant metastasis. The role of postoperative adjuvant chemotherapy or radiotherapy is not fully known (3). Previously, various chemotherapeutic agents have been used, including dacarbazine and immunotherapy with interleukin-2 or interferon (2). Radiation therapy is often used in patients with locally or regionally advanced melanoma of the skin or for patients with unresectable distant metastases. Although it may reduce the rate of local recurrence, it does not prolong the survival rate.
The long-term survival rate of patients with primary MM of the lung is usually poor, even for patients receiving treatment of radical surgical excision. Long-term survival has been achieved in two cases in the past (10 and 11 years following lobectomy and pneumonectomy, respectively) (9,10). Further evaluation and close follow-up of the patient is advised in order to diagnose metastatic dissemination and to improve outcome.
In conclusion, primary MM of the lung represents a rare pathological entity. Careful preoperative investigation and postoperative confirmation of the diagnosis together with clinical findings may establish the diagnosis. Surgical intervention and resection of the involved lymph nodes is appropriate and offers the possibility of long-time survival for certain patients.
References
- 1.Balch CM, Soong SJ, Gershenwald JE, et al. Prognostic factors analysis of 17,600 melanoma patients: validation of the American Joint Committee on Cancer melanoma staging system. J Clin Oncol. 2001;19:3622–3634. doi: 10.1200/JCO.2001.19.16.3622. [DOI] [PubMed] [Google Scholar]
- 2.Bajetta E, Del Vecchio M, Bernard-Marty C, et al. Metastatic melanoma: chemotherapy. Semin Oncol. 2002;29:427–445. doi: 10.1053/sonc.2002.35238. [DOI] [PubMed] [Google Scholar]
- 3.Wilson RW, Moran CA. Primary melanoma of the lung: a clinicopathologic and immunohistochemical study of eight cases. Am J Surg Pathol. 1997;21:1196–1202. doi: 10.1097/00000478-199710000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Volpin E, Sauvanet A, Couvelard A, Belghiti J. Primary malignant melanoma of the esophagus: a case report and review of the literature. Dis Esophagus. 2002;15:244–249. doi: 10.1046/j.1442-2050.2002.00237.x. [DOI] [PubMed] [Google Scholar]
- 5.Cagle P, Mace ML, Judge DM, Teague RB, Wilson RK, Greenberg SD. Pulmonary melanoma. Primary vs metastatic. Chest. 1984;85:125–126. doi: 10.1378/chest.85.1.125. [DOI] [PubMed] [Google Scholar]
- 6.Allen MS, Jr, Drash EC. Primary melanoma of the lung. Cancer. 1968;21:154–159. doi: 10.1002/1097-0142(196801)21:1<154::AID-CNCR2820210123>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- 7.Bagwell SP, Flynn SD, Cox PM, Davison JA. Primary malignant melanoma of the lung. Am Rev Respir Dis. 1989;139:1543–1547. doi: 10.1164/ajrccm/139.6.1543. [DOI] [PubMed] [Google Scholar]
- 8.Alghanem AA, Mehan J, Hassan AA. Primary malignant melanoma of the lung. J Surg Oncol. 1987;34:109–112. doi: 10.1002/jso.2930340209. [DOI] [PubMed] [Google Scholar]
- 9.Reed RJ, 3rd, Kent EM. Solitary pulmonary melanomas: Two case reports. J Thorac Cardiovasc Surg. 1964;48:226–231. [PubMed] [Google Scholar]
- 10.Reid JD, Mehta VT. Melanoma of the lower respiratory tract. Cancer. 1966;19:627–631. doi: 10.1002/1097-0142(196605)19:5<627::AID-CNCR2820190505>3.0.CO;2-Y. [DOI] [PubMed] [Google Scholar]


