Abstract
Background
Obesity is becoming a worldwide public health problem and it is expected to worsen as its prevalence is increasing in children and adolescents. This report examined the distribution of major cardiovascular disease (CVD) risk factors and the effect of lifestyle changes on coronary heart disease (CHD) risk prediction in a high risk obese African Americans.
Methods
We examined the baseline distribution of CVD risk factors in 515 obese African Americans, with mean BMI of 42.9 ± 6.8 kg/m2, and prospectively the effect of a 6-month low-salt, low-fat diet and aerobic-exercise intervention program on risk reduction.
Results
Prevalence of hypertension, dyslipidemia, and diabetes mellitus were 57%, 27% and 24% respectively. Metabolic syndrome was present in 36% and 39% met two features of the syndrome. The 10-year risk prediction for developing CHD ranged from 4% to 17% for women and 6% to 29% for men. After 6 months of life-style changes, many of the risk factors improved, and the CHD risk scores decreased from 6% to 4% in the women and 16% to 13% in the men.
Conclusion
The high prevalence and increasing incidence of obesity and associated cardiovascular risk emphasizes the need to focus on obesity reduction in this high risk population.
Keywords: Blood Pressure, African American, Cardiovascular Diseases, Metabolic Syndrome, Obesity
Introduction
Obesity is excess body weight or excess body fat defined as body mass index1 (BMI) ≥ 30 kg/m2. In the United States, it is estimated that 35.5% of adult men and 35.8% of adult women are obese. The prevalence is disproportionately high in African Americans with age-adjusted rate of 49.5% compared to 39.1% in Hispanics and 34.3% in Caucasians.1 Within the African American population, the rates are 38.8% in men and 58.6% in women.1 In recent years, there has been a rise in obesity-related cardiovascular disease (CVD) morbidity and mortality2,3 and the increased prevalence of obesity in adolescents4 is not a sign of hopeful future. Obesity has been linked to major CVD risk factors including hypertension, diabetes mellitus, and dyslipidemia.2–11 A report by Fontaine et al12 indicated marked reduction in life expectancy due to obesity; the years-of-life lost for the young adult obese African American man was estimated to be 20 years compared to 13 years for obese Caucasians. Another study,13 which reported the impact of obesity on health-related quality of life, noted increased impairment with increasing BMI.6,7,14,15 A report by Randall et al16 suggests that a threshold BMI for maximal appearance of CVD risk factors seems to be between 30 kg/m2 to 35 kg/m2, after adjusting for age and sex. This finding implies preventive measures need to be implemented before reaching the threshold BMI.
Coexistence of obesity-related CVD risk factors including hypertension, diabetes, and dyslipidemia is termed metabolic syndrome (MetS),4,11–19 Metabolic syndrome is a precursor for atherosclerosis, including premature coronary artery disease, CV mortality and affects about 25–35% of the US adults.17–20 Among African Americans, MetS has been linked to increased insulin levels (resistance), elevated blood pressure (BP), dyslipidemia and endothelial dysfunction.17–19 Cherqaoui et al21 noted that, even in the so-called obese but metabolically healthy, the state of the phenotype appears to be only transient. The findings in the study suggest that gaining excess weight is associated with CV risk that may accumulate over time, even before metabolic and cardiovascular signs become apparent in routine tests.
Heart disease is the leading cause of death in all Americans,22,23 however, the CVD morbidity and mortality rate is disproportionally high among African Americans. From 2006 to 2010, the age-adjusted prevalence of coronary heart disease (CHD) declined from 6.4% to 5.8% for Whites, and 6.9% to 6.1% for Hispanics. However, among Blacks, the prevalence increased, though marginally23 from 6.4% to 6.5%. It is believed that genetic, environmental, and lifestyle factors, may be responsible for the high prevalence of obesity, and access to healthcare are the major contributors to the negative outcomes seen in African Americans.24
Several studies support the prognostic significance of 24-hour ambulatory blood pressure, AMBP, monitoring.24–32 Although a nocturnal fall in BP (dipping), is believed to be beneficial, African Americans have been noted to have little or no dipping.24,26 Individuals with a lack of a significant dipping in BP have been linked to higher incidence of cardiovascular complications and more serious target organ damage than those with a significant dipping.28–32 It would be interesting to see how this phenomenon is affected by obesity reduction.
Pulse pressure (PP), a marker of arterial stiffness, is another predictor of CV conditions including carotid atherosclerosis,33,34 left ventricular mass,35 white matter lesions,36 and LVH.37 While an association between increased BMI and elevated BP has been established,38–40 limited data exist that examined the relationship between BMI and PP. Randall et al41 and Kwagyan et al42 showed a stronger significant correlation between PP and BMI than between SBP and BMI. The foregoing review highlights the negative impact of excess body weight on cardiovascular health in obese individuals.
The main purpose of this study was to examine the effect of low-salt, low-calorie diet and aerobic-exercise program on obesity reduction, its impact on major CVD risk factors and CHD risk prediction.
Methods
We studied 515 obese African Americans who were enrolled in a diet-exercise program for weight reduction conducted between August 1998 and October 2000. Details of the diet-exercise program has been previously published.43 In summary, participants with known metabolic and hormonal diseases that cause obesity, and clinical conditions that would not allow moderate to vigorous exercise were excluded. Also excluded were patients with known coronary artery disease, or coronary disease provoked by diagnostic exercise treadmill tests, a history or symptoms of heart failure, or electrocardiographic evidence of arrhythmia. BP was obtained with appropriate sized cuff mercury sphygmomanometer. Blood samples were obtained after fasting for at least 8 hours, and lipid profiles and serum chemistries, including, total cholesterol (TC), triglycerides (TG), low density lipoprotein (LDL), and high density lipoprotein (HDL) and blood sugar (BS) were measured. Hypertension was defined as BP ≥140/90 or on antihypertensive medications. Dyslipidemia was defined as TC ≥200 mg/dL, LDL ≥130 mg/dL, TC /HDL ratio ≥ 4.5 or on treatment. Diabetes mellitus was defined by blood glucose ≥126 mg/dL, or on treatment.
Classification of Metabolic Syndrome
We classified MetS according to NCEP-ATP III43 criteria when at least three of the following features were present: abdominal obesity, characterized by waist circumference >102 cm in men and >88 cm in women; HDL <40 mg/dL in men or <50 mg/dL in women; TG ≥150 mg/dL; BP ≥130/85 mmHg; BS ≥110 mg/dL.
In addition, the arm circumference of each participant was measured and fitted with the appropriate size BP cuff, which was connected to an AMBP monitor unit. The systems were programmed to obtain a BP and heart rate (HR) reading every hour for 24 hours. Pulse pressure for each subject was calculated as the difference between the average 24-hour SBP and DBP. Daytime BP was defined as the average reading from 6AM-10PM, and night-time from 10PM-6AM. Nocturnal BP dippers were defined as those who exhibit a reduction in average BP by at least 10% from daytime to nighttime.
Statistical Analysis and Results
Of the 515 individuals studied, 80% were females. The average age ± SD was 48.3 ± 9.9 years and BMI 42.9 ± 6.8 kg/m2. Table 1 presents the demographic and clinical characteristics. As previously reported, the prevalence rates were 27% for dyslipidemia, 56.9% hypertension and 24.1% DM. The participants were classified into different degrees of obesity as follows: BMI of 30–34.9 kg/m2, BMI of 35–39.9 kg/m2, BMI of 40–44.9 kg/m2, BMI of 45– 49.9 kg/m2, BMI of ≥ 50 kg/m2. The prevalence of CVD risk factors was examined by calculating the proportion of individuals with the condition, expressed as percentages, and Cochran-Armitage test was used to examine trends in prevalence across BMI categories. Table 2 presents the prevalence of the CVD risk factors across the different BMI categories. After adjusting for age and sex, there were no significant differences in the prevalence rates of these risk factors according to increasing BMI, suggesting a threshold of between 30 kg/m2 to 34.99 kg/m2 for maximal appearance of these risk factors.16 Table 3 shows the distribution of MetS features across BMI categories. Ninetynine percent met MetS criteria for waist circumference, 40% met the criteria for BP, and 37% for HDL. Thirty-nine percent had exactly two features of the metabolic syndrome and 36% were diagnosed with it. The proportion of participants who met MetS criteria for HDL as well as those diagnosed with it increases significantly across BMI categories. In particular, a logistic regression analysis showed a 5kg/m2 rise in BMI increased the risk of MetS by 44%. Nocturnal BP dippers, defined as those who exhibit a reduction in average BP by at least 10% from daytime to nighttime were 17%, 54% and 40% for systolic, diastolic and mean arterial BP, respectively for this group. In multiple regression analysis, PP, a surrogate of arterial vascular properties and predictor of CVD, was positively correlated with increasing BMI (P<.01).
Table 1.
Clinical and demographic characteristics of study participants, N=515
| Age, years | 46 ± 13 [range:17–75] |
| Female | 437 (84.8) |
| Body mass index, kg/m2 | 42.8 ± 8.7 |
| Dyslipidemiaa | 139 (27.0) |
| Hypertensionb | 293 (56.9) |
| Diabetes mellitusc | 124 (24.1) |
Data are mean ± SD or n (%)
TC >200 mg/dL, or LDL >130 mg/dL, or on treatment.
BP ≥140/90 mm Hg or on treatment.
Fasting blood glucose > 125 mg/dL or on treatment.
Table 2.
Prevalence rates of CVD risk factors of hypertension, dyslipidemia and diabetes mellitus across BMI categories
| BMI Category | ||||||
|---|---|---|---|---|---|---|
| Risk Factors | 30–34.9, n=86 |
35–39.9, n=125 |
40–44.9, n=110 |
45–49.9, n=92 |
≥50, n=105 |
Total, N=515 |
| None | 26 | 22 | 29 | 29 | 27 | 26 |
| Dyslipidemiaa | 26 | 34 | 29 | 26 | 19 | 27 |
| Hypertensionb | 63 | 62 | 53 | 48 | 63 | 57 |
| Diabetes mellitusc | 20 | 29 | 22 | 20 | 30 | 24 |
Data are %.
TC >200 mg/dL, or LDL >130 mg/dL, or on treatment.
BP ≥140/90 mm Hg or on treatment.
Fasting blood glucose >125 mg/dL or on treatment
Table 3.
Prevalence rates of metabolic syndrome and its features across BMI category
| BMI (kg/m2) | n | Metabolic Syndrome Features | Metabolic Syndrome Diagnosisf |
||||
|---|---|---|---|---|---|---|---|
| Waist Circumferencea | Blood Pressureb | Blood Sugarc | Triglyceridesd | Hyperlipidemiaef | |||
| 30–34.99 | 52 | 98 | 40 | 21 | 29 | 21 | 29 |
| 35–39.99 | 128 | 100 | 32 | 24 | 24 | 29 | 29 |
| 40–44.99 | 150 | 100 | 37 | 18 | 10 | 38 | 31 |
| 45–49.99 | 113 | 100 | 47 | 13 | 30 | 39 | 40 |
| ≥50 | 78 | 78 | 47 | 26 | 16 | 63 | 58 |
| Total | 515 | 99 | 40 | 20 | 20 | 67 | 36 |
Data are %.
Metabolic syndrome defined by NCEP ATP III guidelines as presence of 3 of the following features:
Waist circumference >102cm (men), >88cm (women).
Blood pressure ≥130/85mm Hg.
Fasting serum blood sugar >110mm/dL.
Serum triglycerides ≥150 mg/dL.
High density lipoprotein <40mg/dL (men), <50mg/dL (women).
Significant trend across BMI categories.
Intervention Results
At baseline, the 10-year risk prediction44–46 for developing CHD, in these obese individuals, ranged from 4% to 17% for women and 6% to 29% for men. We examined the effect of a 6-month diet-exercise program on CVD risk outcomes in 129 obese African Americans. The changes in anthropometric, hemodynamic and lipid measures after 6 months diet and exercise intervention are presented in Table 4. Results show an 11% decrease in BMI, an 8% decrease in LDL, and a 10% increase in HDL. The LDL/HDL ratio decreased from 2.3 to 2.1, while the total cholesterol/HDL ratio decreased from 4.4 to 3.4. The 10-year CHD risk prediction decreased on average from 6% to 4% in the women and 16% to 13% in the men. The results highlight the importance of continuous and persistence adherence to life-style changes to risk reduction and cardiovascular health.
Table 4.
Changes in anthropometric, hemodynamic and lipid profiles at baseline and ± months, N=129
| Baseline | 6 Month | % change | P | |
|---|---|---|---|---|
| Variable | ||||
| BMI, kg/m2 | 42.5 ± 1.8 | 37.9 ± 1.5 | −10.8 | <.01 |
| Waist circumference, cm | 118.4 ± 4.2 | 110.8 ± 3.7 | −6.4 | .02 |
| Systolic BP, mm Hg | 131.9 ± 2.2 | 124.2 ± 1.9 | −5.8 | .02 |
| Diastolic BP, mm Hg | 79.8 ± 1.6 | 76.2 ± 1.3 | −3.6 | .05 |
| Pulse pressure, mm Hg | 52.3 ± 1.4 | 48.0 ± 1.2 | −8.2 | <.01 |
| Heart rate, bpm | 82.7 ± 1.9 | 76.6 ± 2.1 | −7.4 | <.01 |
| Glucose, mg/dL | 111.0 ± 8.0 | 101.4 ± 11.6 | −5.7 | .24 |
| Total cholesterol, mg/dL | 224.2 ± 8.6 | 212.6 ± 8.6 | −5.2 | .10 |
| Low density lipoprotein, mg/dL | 137.7 ± 7.8 | 126.8 ± 6.3 | −7.9 | .01 |
| High density lipoprotein, mg/dL | 56.4 ± 2.3 | 61.8 ± 3.2 | +9.6 | <.01 |
| 10-Year CHD risk prediction | ||||
| Women | 6 | 4 | −33.3 | <.01 |
| Men | 16 | 13 | −18.5 | <.01 |
Data are mean ± SD or %.
Conclusion
In cardiovascular research, the paramount objective should be to identify and attempt to prevent or reduce the onset of risk factors that are predictors of CVD morbidity and mortality. The high prevalence of CVD risk factors including MetS in the studied obese persons concurs with other studies.47,48 Central obesity, a marker of insulin resistance, was present in almost all of the study participants. In effect, therefore, these obese individuals already had “one strike” against them in the process of diagnosing MetS. Diagnosis of MetS allows for early recognition of an increased risk of CVD. Whether central obesity per se is a direct cause of risk factors or a reflection of an underlying metabolic abnormality of a more fundamental type is not certain, but the association with cardiovascular risk factors has been documented.49,50
A lack of a significant nocturnal fall in BP has been linked to more serious target organ damage and higher incidence of cardiovascular complications28–32 than with a nocturnal fall. The higher percentage is alarming in this population. The underlying mechanism for dipping is complex and is determined in part by changes in sympathetic nervous system activity. Though not apparent from this study, the autonomic nervous system regulations of hemodynamic variables, which determine the systolic cardiovascular function and BP, are minimally affected during sleep, while their effect on DBP occurring in the passive phase of the cardiac cycle is diminished and likely resulting in the greater rate of dipping in DBP than SBP. The high rate of nondipping in this obese population reinforces the need to reduce BMI and improve hemodynamic and lipid profiles and reduce the potential risk for target organ damage.
Evidence suggests that PP may be a better correlate for cardiovascular morbidity and mortality than either SBP or DBP alone.51,52 Balkestein et al53 reported in a study of healthy obese men, that an increase in BMI was associated with a decrease in large arterial distensibility. The inverse relation between PP and arterial compliance has been established in man and animals,54–56 suggesting an increase in PP to be accompanied by progressive vessel wall damage and atherogenesis.57,58 The present study shows that obesity and MetS adversely affect the arterial vascular properties, as reflected by a higher PP.
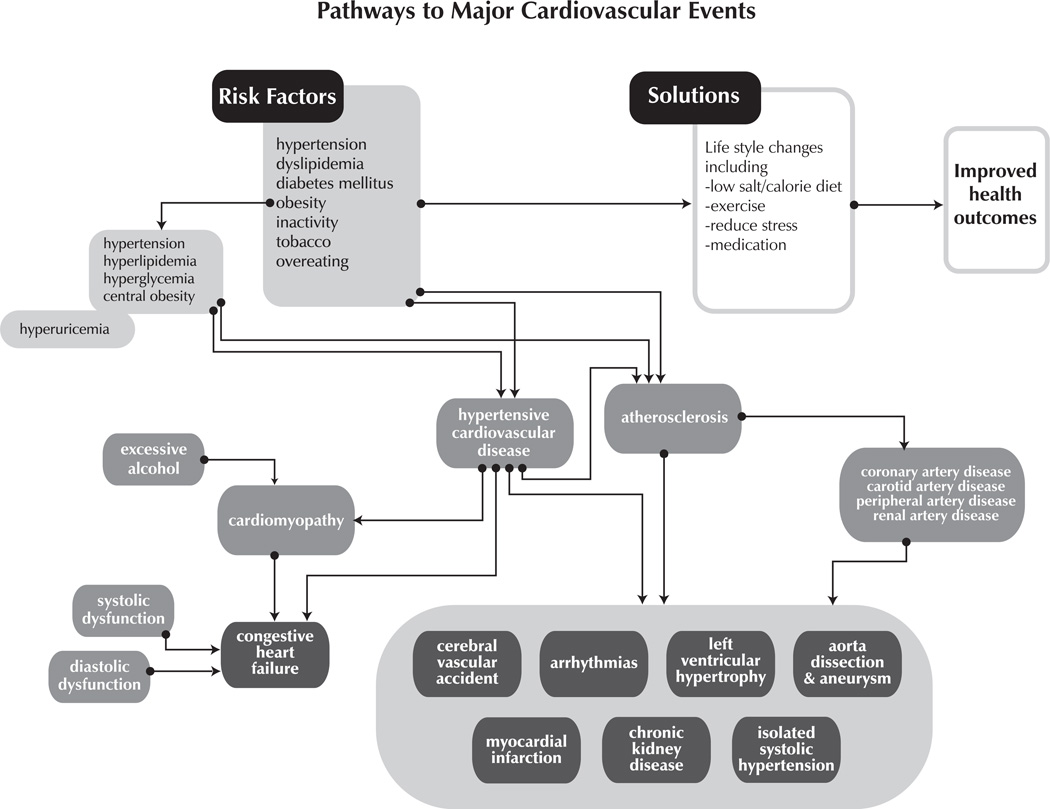
A key element of prevention is to recognize individuals most likely to have cardiovascular events and identify intervention strategie for reduction of risk factors. The high prevalence and increasing incidence of obesity and associated risk factors emphasize the need to focus on obesity reduction. Figure 1, provides a conceptual pathway for the development of various CV outcomes including myocardial infarction, congestive heart failure, left ventricular hypertrophy and stroke. The pathway suggests the autonomous influence of obesity in the development of CV outcomes. The first strategy involves weight reduction and increased physical activity, both of which can improve all components of the CHD risk profile. Our own studies41–43 and others have shown that this can be achieved through a successful diet and exercise program and likely at less cost in the long-term than through pharmacological means. Education is of the utmost importance in ensuring success with the diet-exercise program.59 Understanding why they are overweight/obese and more importantly why they need to take it off is the reason many participants adhered to the program.43
Fig 1.
Risk factors affecting the developmental pathway to major cardiovascular disease events
In conclusion, it cannot be emphasized enough that, in such unprecedented high rates of obesity and associated conditions, earlier intervention through lifestyle modification to stop this epidemic will be of great benefit to society.
Acknowledgments
This manuscript was supported in part with federal funds from NIH/NCATS grant number UL1TR000101, NIH/NIMHHD grant number G12 MD007597 and NIH/ NHLBI grant number U01-HL03679.
Footnotes
Author Contributions
Design concept of study: Kwagyan, Randall
Acquisition of data: Ketete, Bettencourt, Maqbool, Xu
Data analysis and interpretation: Kwagyan, Retta, Ketete, Bettencourt, Maqbool, Xu, Randall
Manuscript draft: Kwagyan, Retta, Randall
Statistical expertise: Kwagyan
Acquisition of funding: Randall
Administrative: Retta, Ketete, Bettencourt, Maqbool, Xu, Randall
Supervision: Randall
References
- 1.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307(5):491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 2.Yang Q, Cogswell ME, Flanders WD, et al. Trends in cardiovascular health metrics and associations with all-cause and CVD mortality among US adults. JAMA. 2012;307(12):1273–1283. doi: 10.1001/jama.2012.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. Obesity: Preventing And Managing The Global Epidemic. Geneva: Report of a WHO consultation on obesity; 1998. [PubMed] [Google Scholar]
- 4.Weiss R, Dziura J, Burgert TS, et al. Obesity and the metabolic syndrome in children and adolescents. N Engl J Med. 2004;350(23):2362–2374. doi: 10.1056/NEJMoa031049. [DOI] [PubMed] [Google Scholar]
- 5.Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults. The Evidence Report. NHLB: NIH Pub No; 1998. National Institutes of Health, National Heart, Lung, and Blood Institute; pp. 98–4083. [PubMed] [Google Scholar]
- 6.Pi-Sunyer FX. Health implication on obesity. Am J Clin Nutr. 1991;53(6):1595s–1603s. doi: 10.1093/ajcn/53.6.1595S. [DOI] [PubMed] [Google Scholar]
- 7.Denke MA, Sempos CT, Grundy SM. Excess body weight. An under recognized contributor to high blood cholesterol levels in White American men. Arch Intern Med. 1993;153:1093–1103. doi: 10.1001/archinte.153.9.1093. [DOI] [PubMed] [Google Scholar]
- 8.Kucamarski RJ, Flegal KM, Campbell SM, Johnson CL. Increasing prevalence of overweight among US adults, the NHANES 1960–1991. JAMA. 1994;272:205–211. doi: 10.1001/jama.272.3.205. [DOI] [PubMed] [Google Scholar]
- 9.Burt VL, Whelton P, Roccella EJ, et al. Prevalence of hypertension in the U.S. adult population: results from NHANES III, 1988–1991. Hypertension. 1995;25:305–313. doi: 10.1161/01.hyp.25.3.305. [DOI] [PubMed] [Google Scholar]
- 10.Colditz GA, Willett WC, Rotnitzky A, Manson JE. Weight gain as a risk factor for clinical diabetes mellitus in women. Ann Intern Med. 1995;122:481–486. doi: 10.7326/0003-4819-122-7-199504010-00001. [DOI] [PubMed] [Google Scholar]
- 11.Ford ES, Williamson DF, Liu S. Weight change and diabetes incidence: findings from a national cohort of US adults. Am J Epidemiol. 1997;146:214–222. doi: 10.1093/oxfordjournals.aje.a009256. [DOI] [PubMed] [Google Scholar]
- 12.Fontaine KR, Redden DT, Wang C, Westfall AO, Allison DB. Years of life lost due to obesity. JAMA. 2003;289:187–193. doi: 10.1001/jama.289.2.187. [DOI] [PubMed] [Google Scholar]
- 13.Fontaine KR, Cheskin LJ, Barofsky I. Health related quality of life in obese persons seeking treatment. J Fam Pract. 1996;43:265–279. [PubMed] [Google Scholar]
- 14.He Q, Ding ZF, Fong DY, Kalberg J. Blood pressure is associated with body mass index in both normal and obese children. Hypertension. 2000;36:165–170. doi: 10.1161/01.hyp.36.2.165. [DOI] [PubMed] [Google Scholar]
- 15.Masuo K, Mikami H, Ogahara T, Tuck ML. Weight gain-induced blood pressure elevation. Hypertension. 2000;35:1135–1140. doi: 10.1161/01.hyp.35.5.1135. [DOI] [PubMed] [Google Scholar]
- 16.Randall OS, Retta TM, Kwagyan J, et al. Obese African Americans: the prevalence of dyslipidemia, hypertension, and diabetes mellitus. Ethn Dis. 2004;14(3):384–388. [PubMed] [Google Scholar]
- 17.Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults. JAMA. 2002;287:356–359. doi: 10.1001/jama.287.3.356. [DOI] [PubMed] [Google Scholar]
- 18.Cook S, Weitzman M, Auinger P, Nguyen M, Dietz WH. Prevalence of a metabolic syndrome phenotype in adolescents: findings from the NHANES III, 1988–1994. Arch Pediatr Adolesc Med. 2003;157(8):821. doi: 10.1001/archpedi.157.8.821. [DOI] [PubMed] [Google Scholar]
- 19.Ford ES. Prevalence of the metabolic syndrome defined by the International Diabetes Federation among adults in the US. Diabetes Care. 2005;28(11):2745–2749. doi: 10.2337/diacare.28.11.2745. [DOI] [PubMed] [Google Scholar]
- 20.Haffner S, Heinrich T. Epidemic obesity and the metabolic syndrome. Circulation. 2003:1541–1545. doi: 10.1161/01.CIR.0000088845.17586.EC. [DOI] [PubMed] [Google Scholar]
- 21.Cherqaoui R, Kassim TA, Kwagyan J, et al. The metabolically healthy but obese phenotype in African Americans. J Clin Hypertens (Greenwich) 2012;14(2):92–96. doi: 10.1111/j.1751-7176.2011.00565.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cook S, Weitzman M, Auinger P, Nguyen M, Dietz WH. Prevalence of a metabolic syndrome phenotype in adolescents: findings from NHANES III, 1988–1994. Arch Pediatr Adolesc Med. 2003;157:821–827. doi: 10.1001/archpedi.157.8.821. [DOI] [PubMed] [Google Scholar]
- 23.Sidney S, Rosamond WD, Howard VJ, Luepker RV. The “Heart Disease and Stroke Statistics—2013 Update” and the Need for a National Cardiovascular Surveillance System. Circulation. 2013;127(1):21–23. doi: 10.1161/CIRCULATIONAHA.112.155911. [DOI] [PubMed] [Google Scholar]
- 24.CDC Weekly. Prevalence of coronary heart disease - United States 2006–2010. [Accessed February 4, 2014];2011 Oct;60(40):1377–1381. cdc.gov/mmwr/preview/mmwrhtml/mm6040a1.htm. [PubMed] [Google Scholar]
- 25.Verdecchia P, Porcellati C, Schillaci G, et al. Ambulatory blood pressure. An independent predictor of prognosis in essential hypertension. Hypertension. 1994;34:793–801. doi: 10.1161/01.hyp.24.6.793. [DOI] [PubMed] [Google Scholar]
- 26.Verdecchia P, Schillaci G, Borgioni C. Ambulatory pulse pressure: a potent predictor of total cardiovascular risk in hypertension. Hypertension. 1998;32:983–988. doi: 10.1161/01.hyp.32.6.983. [DOI] [PubMed] [Google Scholar]
- 27.Verdecchia P, Schillaci G, Reboldi G, et al. Different prognostic impact of 24-hour mean blood pressure and pulse pressure on stroke and coronary artery disease in essential hypertension. Circulation. 2001;103:2579–2584. doi: 10.1161/01.cir.103.21.2579. [DOI] [PubMed] [Google Scholar]
- 28.Devereax RB, Pickering TG. Relationship between the level, pattern and variability of ambulatory blood pressure and target organ damage in hypertension. J Hypertens Suppl. 1991;9(8):S34–S38. [PubMed] [Google Scholar]
- 29.Parati G, Pomidossi G, Albini F, Malaspina D, Mancia G. Relationship of 24-hour blood pressure mean and variability to severity of target organ damage. J Hypertens. 1987;5(1):93–98. doi: 10.1097/00004872-198702000-00013. [DOI] [PubMed] [Google Scholar]
- 30.Redon J, Campos C, Narciso ML, Rodicio JL, et al. Prognostic value of ambulatory blood pressure monitoring in refractory hypertension. Hypertension. 1998;31:712–718. doi: 10.1161/01.hyp.31.2.712. [DOI] [PubMed] [Google Scholar]
- 31.Mancia G, Parati G. Ambulatory blood pressure monitoring and organ damage. Hypertension. 2000;36:894–900. doi: 10.1161/01.hyp.36.5.894. [DOI] [PubMed] [Google Scholar]
- 32.Mancia G, Zanchetti A, Agabiti-Rosei E, et al. Ambulatory blood pressure is superior to clinic blood pressure in predicting treatment-induced regression of left ventricular hypertrophy. Circulation. 1997;95:1464–1470. doi: 10.1161/01.cir.95.6.1464. [DOI] [PubMed] [Google Scholar]
- 33.Staessen JA, Thijs L, Fagard R. Predicting cardiovascular risk using conventional versus ambulatory blood pressures in older patients with systolic hypertension. JAMA. 1999;282:539–546. doi: 10.1001/jama.282.6.539. [DOI] [PubMed] [Google Scholar]
- 34.Franklin SS, Sutton-Tyrell K, Belle S, et al. The importance of pulsatile components of hypertension in predicting carotid stenosis in older adults. J Hypertens. 1997;15:1143–1150. doi: 10.1097/00004872-199715100-00012. [DOI] [PubMed] [Google Scholar]
- 35.Suurkula M, Agewall S, Fagerberg B, et al. Ultrasound evaluation of atherosclerotic manifestations in the carotid artery in high-risk hypertension patients. Arterioscler Thromb. 1994;14:1297–1304. doi: 10.1161/01.atv.14.8.1297. [DOI] [PubMed] [Google Scholar]
- 36.Pannier B, Brunel P, El Aroussy W. Pulse pressure and echocardiographic findings in essential hypertension. J Hypertension. 1989;7:127–132. [PubMed] [Google Scholar]
- 37.Randall O, Kwagyan J, Retta T, et al. Effect of intensive blood pressure control on cardiovascular remodeling in hypertensive patients with nephrosclerosis. Int J Nephrol. 2013;2013:120167. doi: 10.1155/2013/120167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Liao D, Cooper L, Toole J. The prevalence and severity of white lesions, their relationship with age, ethnicity, gender and cardiovascular disease risk factors: ARIC Study. Neuroepidemiology. 1997;16(3):149–162. doi: 10.1159/000368814. [DOI] [PubMed] [Google Scholar]
- 39.Masuo K, Mikami H, Ogahara T, Tuck ML. Weight gain-induced blood pressure elevation. Hypertension. 2000;35:1135–1140. doi: 10.1161/01.hyp.35.5.1135. [DOI] [PubMed] [Google Scholar]
- 40.Ferrannini E. The hemodynamics of obesity: a theoretical analysis. J Hypertens. 1992;10:1417–1423. doi: 10.1097/00004872-199211000-00015. [DOI] [PubMed] [Google Scholar]
- 41.Martins D, Tareen N, Pan D, Norris K. The relationship between body mass index and pulse pressure in older adults with isolated systolic hypertension. Am J Hypertens. 2002;15:538–543. doi: 10.1016/s0895-7061(02)02269-0. [DOI] [PubMed] [Google Scholar]
- 42.Randall OS, Kwagyan J, Huang Z, Xu S, Ketete M, Maqbool AR. Effect of diet and exercise on pulse pressure and cardiac function in morbid obesity: analysis of 24 hour ambulatory blood pressure. J Clin Hyperten (Greenwich) 2005;7(8):455–463. doi: 10.1111/j.1524-6175.2005.04491.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kwagyan J, Tabe CE, Xu S, Maqbool AR, Gordeuk VR, Randall OS. The impact of body mass index on pulse pressure in obesity. J Hypertension. 2005;23(3):619–624. doi: 10.1097/01.hjh.0000160220.71350.5f. [DOI] [PubMed] [Google Scholar]
- 44.Randall OS, Feseha HB, Illoh K, et al. Response of lipoprotein(a) levels to therapeutic life-style change in obese African-Americans. Atherosclerosis. 2004;172:155–160. doi: 10.1016/j.atherosclerosis.2003.09.017. [DOI] [PubMed] [Google Scholar]
- 45.National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation and Treatment of High Cholesterol in Adults final report. Circulation. 2002;288:1491–1498. [PubMed] [Google Scholar]
- 46.Dawber TR, et al. Epidemiological approaches to heart disease: the Framingham Study. Am J Public Health. 1951;41:279–286. doi: 10.2105/ajph.41.3.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kannel WB, et al. An investigation of coronary heart disease in families: the Framingham Offspring Study. Am J Epidemiol. 1979;110:281–290. doi: 10.1093/oxfordjournals.aje.a112813. [DOI] [PubMed] [Google Scholar]
- 48.Must A, Spadano J, Coakley EH, Field AE, Colditz WH. The disease burden associated with overweight and obesity. JAMA. 1999;282(16):1523–1529. doi: 10.1001/jama.282.16.1523. [DOI] [PubMed] [Google Scholar]
- 49.National Task Force on the Prevention and Treatment of Obesity. Overweight, obesity and health risk. Arch Intern Med. 2000;160:898–904. doi: 10.1001/archinte.160.7.898. [DOI] [PubMed] [Google Scholar]
- 50.Larson B, Svardsudd K, Welin L, et al. Abdominal adipose tissue distribution, obesity and risk of cardiovascular disease and death: 13-year follow-up of participants in the study of men born in 1913. Br Med J (Clin Res Ed) 1984;288:1401–1404. doi: 10.1136/bmj.288.6428.1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Vega GL. Obesity, the metabolic syndrome, and cardiovascular disease. Am Heart J. 2001;142:1108–1116. doi: 10.1067/mhj.2001.119790. [DOI] [PubMed] [Google Scholar]
- 52.Haider AW, Larson MG, Franklin SS, et al. Systolic blood pressure, diastolic blood pressure, and pulse pressure as predictors of risk for congestive heart failure in the Framingham Heart Study. Ann Intern Med. 2003;138:10–16. doi: 10.7326/0003-4819-138-1-200301070-00006. [DOI] [PubMed] [Google Scholar]
- 53.Benetos A, Rudichi A, Safar M, et al. Pulse pressure and cardiovascular mortality in normotensive and hypertensive subjects. Hypertension. 1998;32:560–564. doi: 10.1161/01.hyp.32.3.560. [DOI] [PubMed] [Google Scholar]
- 54.Balkestein EJ, Van Aggel-Leijssen DP, Baak MA, et al. The effect of weight loss with or without exercise training on large artery compl iance in healthy obese men. J Hypertens. 1999;17:1831–1835. doi: 10.1097/00004872-199917121-00008. [DOI] [PubMed] [Google Scholar]
- 55.Burton AC. Physiology and Biophysics of the Circulation. Vol. 161 Chicago, IL: Year Book Medical Publishers; 1965. [Google Scholar]
- 56.Randall OS, van den Bos GC, Westerhoff N. Systemic compliance: does it play a role in the genesis of essential hypertension? Cardiovasc Res. 1984;18:455–462. doi: 10.1093/cvr/18.8.455. [DOI] [PubMed] [Google Scholar]
- 57.Ferguson JJ, Randall OS. Hemodynamic correlates of arterial compliance. Cathet Cardiovasc Diagn. 1986;12:376–380. doi: 10.1002/ccd.1810120604. [DOI] [PubMed] [Google Scholar]
- 58.Chen YT, Vaccarino V, Williams CS, Buttler J, Berkman LF, Krumholz HM. Risk factors for heart failure in the elderly: a prospective community-based study. Am J Med. 1999:605–612. doi: 10.1016/s0002-9343(99)00126-6. [DOI] [PubMed] [Google Scholar]
- 59.Randall OS, Randall D. Menu for Life: African Americas Get Healthy, Eat Well, Loss Weight and Live Beautifully. New York, NY: Random House Inc; 2003. p. 22. [Google Scholar]