Abstract
Key points
Self-management education in asthma is not an optional extra. Healthcare professionals have a responsibility to ensure that everyone with asthma has personalised advice to enable them to optimise how they self-manage their condition.
Overviews of the extensive evidence-base conclude that asthma self-management supported by regular professional review, improves asthma control, reduces exacerbations and admissions, and improves quality of life.
Self-management education should be reinforced by a written personalised asthma action plan which provides a summary of the regular management strategy, how to recognise deterioration and the action to take.
Successful implementation combines education for patients, skills training for professionals in the context of an organisation committed to both the concept and the practice of supported self-management.
Educational aims
To summarise the evidence base underpinning supported self-management for asthma
To provide clinicians with a practical approach to providing supported self-management for asthma
To suggest an appropriate strategy for implementing supported self-management
Summary
The evidence in favour of supported self-management for asthma is overwhelming. Self-management including provision of a written asthma action plan and supported by regular medical review, almost halves the risk of hospitalisation, significantly reduces emergency department attendances and unscheduled consultations, and improves markers of asthma control and quality of life. Demographic and cultural tailoring enables effective programmes to be implemented in deprived and/or ethnic communities or within schools.
A crucial component of effective asthma self-management interventions is the provision of an agreed, written personalised action plan which advises on using regular medication, recognising deterioration and appropriate action to take. Monitoring can be based on symptoms or on peak flows and should specify thresholds for action including increasing inhaled steroids, commencing oral steroids, and when (and how) to seek professional help. Plans should be personalised to reflect asthma severity and treatment regimes, avoidance of triggers, co-morbid rhinitis and the individual’s preferences.
Implementation is a challenge. Systematic review evidence suggests that it is possible to implement asthma self-management in routine care, but that to be effective this requires a whole systems approach which considers implementation from the perspective of patient education and resources, professional skills and motivation and organisation priorities and routines.
Introduction
People living with asthma have to accommodate their long-term condition within the context of their daily life. They may need to remember to use regular medication, to keep a supply of inhalers, avoid their triggers where possible, cope with the variability of asthma and the impact this has on their and their family’s lifestyle. Crucially they have to recognise when their asthma is deteriorating, and make decisions about when to adjust their medication, when to use emergency treatment and when to seek professional help.
Surveys suggests that, even in countries that have been proactive about recommending asthma self-management, three quarters of people living with asthma are managing their condition without the benefit of a written personalised asthma action plan, which could guide their self-management and help them make clinically appropriate decisions [1–4]. The UK National Review of Asthma Deaths provided a stark reminder of the importance of giving patients clear advice about what to do in an emergency [5]. Approximately half the people who died had not received any professional care during the fatal attack; many appeared not even to have tried to seek assistance and only 23% had an action plan that might have advised them when and how to seek help.
Self-management education is thus not an optional extra. All of our patients are already self-managing their own asthma (albeit sometimes inappropriately from a clinical perspective). It is the duty of all professionals involved in the care of people with asthma to ensure that all patients have personalised advice to enable them to improve and optimise their self-management.
Definition of self-management
The US Institute of Medicine defines self-management as “the tasks that individuals must undertake to live with one or more chronic conditions. These tasks include having the confidence to deal with medical management, role management and emotional management of their conditions” [6]. In the context of a variable condition, such as asthma, the core, evidence-based component is supporting patients to recognise and act on deteriorating symptoms (“medical management”), but we need to recognise that patients face challenges in accommodating asthma into their work, social and family lives and that, for some, this challenges their roles in society and/or comes at significant emotional cost.
Literature underpinning this clinical review
This clinical review is based on the evidence identified for a systematic overview of the literature on supported self-management for long-term conditions (PRISMS: Practical Systematic Review of Self-Management Support for long-term conditions) [7], which included a meta-review of systematic reviews of asthma self-management support, as well as a systematic review of implementation studies. A detailed analysis of this literature is in the PRISMS published final report [7], but this paper highlights the key messages for clinicians and health service managers providing care for people with asthma.
The evidence base for supported self-management
The evidence for supported self-management is overwhelming [7]. The British Thoracic Society/Scottish Intercollegiate Guideline Network (BTS/SIGN) asthma guideline cites 261 randomised controlled trials reported in 22 systematic reviews in support of its grade A recommendation that “all people with asthma (and/or their parents or carers) should be offered self-management education which should include a written personalised asthma action plan and be supported by regular professional review” [8]. The Global Initiative for Asthma (GINA) guideline is similarly unequivocal about the importance of “providing patients with education and skills in order to effectively manage their asthma” [9], highlighting that this should be achieved through a partnership between patients and their healthcare professional. The over-arching conclusion of these overviews of the literature is that supported asthma self-management improves asthma control, reduces exacerbations and admissions, and improves quality of life [7–9].
The evidence in adults is synthesised in a Cochrane review citing 36 randomised trials involving 6090 participants. “Optimal self-management”, defined as including provision of a written action plan for self-management of exacerbations together with self-monitoring and regular medical review, almost halved the risk of hospitalisation (risk ratio 0.58 (95% confidence interval 0.43–0.77)) [10]. Other outcomes that improved significantly with optimal self-management included emergency department attendances and unscheduled consultations, markers of asthma control and quality of life. Similar benefits were reported by meta-analyses of trials in children, which report significant reductions in unscheduled care (including hospitalisations, emergency department attendances and doctor consultations) [11], and markers of control (days of restricted activity, night disturbance and school absence) [12]. The only age-group in whom traditional action plans have consistently been shown to be ineffective are pre-school children, at least in part because of the overlap with viral-associated wheeze [13]. Innovative approaches will be needed to provide the self-management education that will support parents of wheezy toddlers.
More recent work has highlighted the importance of tailoring self-management interventions for the communities at which they are targeted. It is clear that simply “translating” a self-management programme designed for one cultural group is insufficient to allow the programme to be effective in another [7, 8]. A compelling illustration of this is a trial conducted in Birmingham, UK, in which a programme of supported self-management was provided to people with asthma from both white European and South Asian communities [14]. Resources were translated and the intervention delivered by a healthcare professional fluent in relevant languages, but no attempt was made to provide a culturally-tailored programme. Overall, the initiative reduced unscheduled care (admissions and general practitioner consultations) and oral steroid courses, but this effect was driven by substantial improvements in white European subjects. The impact on use of healthcare resources in people from the South Asian community was not significant, though the intervention was associated with an improved quality of life in Asian subjects from the low baseline (compared with white European subjects). In contrast, culturally appropriate initiatives in US inner city populations of African Americans and/or Latino populations have proved effective at reducing emergency use of healthcare resources and improving markers of control [15]. Many of these programmes have involved community-based projects, with support workers or lay befrienders and other socially and culturally tailored initiatives to support families from deprived ethnic minority populations to engage with and benefit from healthcare services. See table 1 for some evidence-based strategies for cultural tailoring of self-management interventions.
Table 1.
Strategies for cultural tailoring that have been used in effective interventions
|
Reproduced from [8] with permission from the publisher.
School-based interventions have had some success, typically not only involving children with asthma, but also raising awareness of asthma within the whole school population [16]. Interventions are heterogeneous, but often involve screening school populations for asthma, leading class lessons on asthma, providing information, technology-based learning or peer support groups.
Personalised asthma action plans
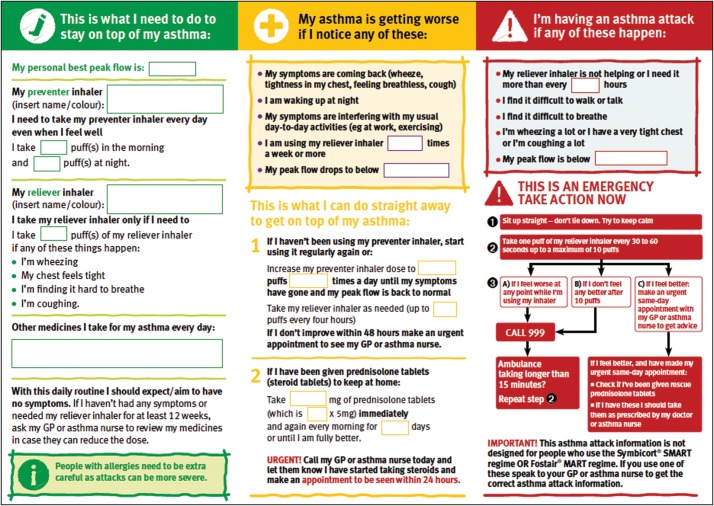
A crucial component of effective self-management interventions is the provision of an agreed, written action plan [10]. The format of the plans used in trials vary, but at their core they share a common content, which provides the patient with a summary of their regular management strategy, advice on how to monitor and recognise deterioration and recommends the action they should take. (See table 2 for a summary of the key components of an action plan) Plans should be discussed, negotiated and agreed with patients and reviewed at subsequent consultations to ensure that they remain up to date. Templates are available from many sources, often provided by national patient organisations, such as Asthma UK (see figure 1; available from www.asthma.org.uk/advice-asthma-action-plan).
Table 2.
Summary of the key components of a written personalised asthma action plan
| Component of an action plan | Result | Practical considerations |
| Format of action points | ||
| Symptom versus peak flow triggered | Similar effect | Asthma UK personalised asthma action plans include both symptom triggers and peak flow levels at which action should be taken. |
| Standard written instructions | Consistently beneficial | |
| Traffic light configuration | Not clearly better than standard instructions | |
| Number of action points | ||
| 2–3 action points | Consistently beneficial | Three commonly used action points are:Peak flow <80% best: increase inhaled steroidsPeak flow <60% best: commence oral steroids and seek medical advicePeak flow <40% best: seek urgent medical advice. |
| 4 action points | Not clearly better than 2–3 points | |
| Peak flow levels | ||
| Based on percentage personal best peak flow | Consistently beneficial | Personal best should be assessed once treatment has been optimised and peak flows are stable. Best peak flow should be updated every few years in adults, and, if a peak flow meter is being used, more frequently in growing children. |
| Based on percentage predicted peak flow | Not consistently better than usual care | |
| Treatment instructions | ||
| Individualised using inhaled and oral steroids | Consistently beneficial | Patients may safely hold an emergency supply of prednisolone tablets for use if their symptoms continue to deteriorate and/or if their peak flow falls to 60% of their best. |
| Individualised using oral steroids only | Insufficient data to evaluate | Increasing inhaled steroids is ineffective if patients are already taking moderate or high doses (≥400 µg daily) and these patients should be advised to move straight to the oral steroid step. |
| Individualised using inhaled steroids | Insufficient data to evaluate | Those on low doses (e.g. 200 µg) of inhaled steroids may be advised to increase the dose substantially (e.g. to 1200 µg daily) at the onset of deterioration. Patients who have stopped medication should be reminded to restart their inhaled steroids. |
Reproduced from [8] with permission from the publisher.
Figure 1.
Asthma action plan. An example of a asthma self-management tool. Reproduced with permission from Asthma UK. Available from www.asthma.org.uk/advice-asthma-action-plan.
Defining regular management
Adherence to maintenance asthma therapy is notoriously poor with less than half of patients taking their inhaled steroids regularly [17]. Non-adherence may be intentional (deciding not to take recommended treatment after considering the perceived necessity for/concerns about taking regular medication [18]) and/or non-intentional (e.g. misunderstanding, forgetting or being unable to afford treatment) [19]. Addressing non-adherence is a complex challenge, but an action plan, completed in discussion with the patient, may contribute to improving adherence by reducing confusion about the respective roles of different inhalers and reminding patients about when and how to use them.
Recognising deterioration
Although many action plans used in trials are based on peak flow monitoring, there is evidence that symptom-based plans are equally effective in adults [20]. Few people wish to monitor peak flows routinely, and a pragmatic approach is to include both the symptoms that should trigger action and provide peak flow thresholds so that those who wish to do so can measure their status objectively before adjusting treatment.
A recent secondary analysis of two datasets has confirmed that a fall in peak flow to 60% of personal best (not predicted) is an appropriate threshold for commencing oral steroids. This threshold predicted an exacerbation 1 day before its onset (specificity 99%; sensitivity 78%). Similarly, the combination of an increase in symptoms and fall of peak flow to 80% predicts exacerbations 5 days prior to onset (sensitivity 100%; specificity 87%) enabling inhaled steroids to be increased with the aim of restoring control [21]. Many plans, including those linked with electronic peak flow meters and digital “apps”, illustrate these thresholds with “traffic light” colour coding.
In children, symptom-based plans are more effective than peak flow based plans at reducing the need for unscheduled care, though peak flow based plans may be more effective at reducing symptom free days [22]. All other outcomes are similar with either monitoring strategy.
Advising appropriate action
Action plans should specify between two and three action points [20], with the aim of helping patients to respond to early signs of deteriorating control, commence emergency treatment at the onset of an exacerbation, and seek timely professional care. Despite evidence from pharmaceutical trials that doubling inhaled steroids is less effective than adding a long-acting β2 agonist [8], the advice to increase inhaled steroids has been included in all effective asthma action plans [20]. This apparent paradox is probably because, in contrast to trial participants, most people with asthma reduce (or stop) their maintenance treatment and this step is an essential reminder to reinstate the usual dose of preventer treatment at the first sign that control is slipping. Doubling inhaled steroids, as recommended in early action plans is probably insufficient [23], and current advice is that larger increases (e.g. quadrupling) are more effective [24]. It is important to include advice on how and when to reduce the dose of inhaled steroids to normal maintenance levels.
People already taking moderate/high doses of inhaled steroids should normally move straight to the next action point and be advised to commence oral steroids at the onset of an exacerbation. This step needs to be clearly indicated for all patients, though whether a patient chooses to hold an emergency supply of prednisolone or seek professional advice to obtain a prescription will depend on individual circumstances and take into account personal preferences. There is evidence that ownership of an action plan increases the likelihood of being prescribed oral steroids [25].
Personalisation
Asthma self-management and the supporting personalised action plan need to be tailored to the individual. From a clinical perspective a personalised action plan should:
Reflect the severity of disease. e.g. omitting the increased inhaled steroid step in someone already on high maintenance doses, facilitating prompt transfer to hospital in a patient with a history of near fatal asthma.
Be adjusted to the patient’s drug regime. e.g. whether the patient is using an add-on treatment, whether the inhaled steroids and long-acting β2 agonist are combined in a single inhaler.
Provide advice about avoidance of triggers relevant to the individual patient.
Encompass management of co-morbid allergic rhinitis if appropriate.
More broadly, it needs to be adapted to acknowledge patient preference. Some patients will be confident holding emergency steroids, others will prefer to seek professional advice before commencing emergency treatment.
Living with asthma
Whilst the management of deterioration and exacerbations, summarised in a personalised asthma action plan is central to “medical self-management” [6], qualitative studies reveal that patients perceive that plans do not reflect the breadth and nuances of living with asthma, with the risk that the action plan may be considered as irrelevant [26]. For people with severe disease, this may be because the day-to-day challenges are not addressed; for those with infrequent exacerbations advice on when to take oral steroids may be planning for an event that rarely happens; for people with occupational asthma, the priority may be the potential disruption of work roles and financial implications [27]. Discussing the wider aspects of self-management enables people to live with asthma and form the wider context for the medically focussed action plan. This “living with asthma” discussion is likely to take longer than is available in a routine consultation and may well be best provided by an asthma educator, a specialist nurse or, in some circumstances, peer support.
Supporting self-management
Professional review
Personalised asthma action plans are not static documents: they need to be regularly reviewed, revised and refined as clinical and lifestyle circumstances change [8]. Regular professional review is a core component of supported self-management with evidence of greater reductions in hospitalisations and emergency department visits in trials where the intervention includes regular review [10].
Consultation style
Self-management education requires a patient-centric style of consultation in which the patient and professional can “develop a partnership in which patients are encouraged to participate in decisions about their treatment and given the opportunity to express their expectations and concerns” [9]. A trusting relationship between the patient and their healthcare professional enables “a feeling of working together to achieve the aim of better self-management” [28].
Shared decision making has been evaluated in the context of asthma in a randomised controlled trial which compared outcomes of consultations in which the decisions about treatment were negotiated between the professional and patient compared with an approach where the clinician decided and then explained the management strategy [29]. The proportion of patients prescribed inhaled steroids was the same in both groups, but adherence to controller medication was greater after a consultation in which the decision was shared, and this effect was maintained over the 2-year trial. There were some positive effects on clinical outcomes (resource use and asthma control).
Goal setting is also attracting interest. This approach aims to help the person with asthma to identify goals meaningful to them that they can work towards by improving control of their asthma. Practical strategies that have been tried include asking the patients to prepare for their consultation by thinking about their goals. Whilst pilot studies suggest that this can work [30], there is a challenge in incorporating the approach into routine practice even for a trained professional.
Flexible access
People with long-term conditions need support from their healthcare professionals to enable them confidently to self-manage their care. In a variable condition, such as asthma, many months may go by without needing any support but, when help is wanted, access to professional advice needs to be flexible in timing and mode of delivery [31]. An acute exacerbation may need a prompt face-to-face consultation, or occasionally an immediate hospital admission. If control is good, a telephone consultation may be all that is required to check progress and review an action plan. A quick non-urgent query may be most conveniently dealt with by e-mail. Innovative use of digital solutions with, for example, cloud-based personal health records may contribute to providing convenient, flexible access to professional support.
A core component of long-term management of asthma
Supported self-management is a core component of good professional management of long-term conditions, embodied by the Chronic Care Model [32], House of Care [33] and other similar models of care. The importance of embedding self-management in good clinical care is illustrated by a systematic review which showed that the more components of the Chronic Care Model (i.e. teaching self-management skills, providing decision support, delivery system design and clinical information systems [32]) included within the service, the greater was the impact of self-management education on adherence [34].
Implementing supported self-management
Despite the strength and breadth of trial evidence for supported self-management extending back over some four decades and reflected in asthma guideline recommendations for 25 years [35], implementation in routine care remains poor [1–5]. Each healthcare setting has its own challenges. The short duration of hospital admissions may make it difficult to ensure that all patients have an action plan before they leave hospital, especially if the professionals responsible for providing self-management education are few in number or not always available. In primary care, the challenge may be more the diversity of presenting problems, so that skills and resources for an asthma consultation are competing with all the other clinical and social problems addressed in a typical family doctor clinic.
Both the UK BTS/SIGN guideline [8] and the PRISMS overview [7] considered the evidence from implementation studies. The PRISMS systematic review of experimental studies in which supported self-management was implemented in routine clinical care [7], identified 18 studies from primary, secondary, community and managed care settings serving a total estimated asthma population of 800 000 people in six countries. The review concluded that it is possible to implement asthma self-management in routine care but that to be effective, this required a whole systems approach which considered implementation from the perspective of the patient, the professional and the organisation. A 14-item taxonomy of components of effective self-management that healthcare providers could consider in developing services, has been derived from the review [7]. This includes provision of information for patients, template action plans, resources for monitoring, regular clinical review, skills training for professionals and flexible access to advice [7].
Empowering the patient
Asthma education is an essential component of self-management interventions but, in isolation, does not consistently improve clinical outcomes [7–9]. Information about asthma needs to be available in a range of formats, both paper-based or leaflets and video clips that can be found on-line. Patients may need to be guided to suitable sites offering information and resources from national patient organisations, professional societies and health services. The European Lung Foundation is a useful resource for people with lung diseases, (www.europeanlung.org) and both the BTS/SIGN and GINA have a sections on their websites with patient summaries of their guidelines. (See GINA: www.ginasthma.org/Patients and SIGN: www.sign.ac.uk/guidelines/fulltext/141/index.html).
Personalised asthma action plans vary in format and complexity. Portability has always been a consideration. Some of the earliest action plans were the size of credit cards; today there is considerable interest in “apps” that are integrated into the ubiquitous mobile phone. A recent Cochrane review of two trials of clinically designed and supported self-management apps concluded that it was unclear whether apps were better than traditional evidence-based plans, but there was no reason to think they were any less effective [36]. There are concerns, however, that the wide range of apps currently freely downloadable on to smart phones and tablets are limited in their remit and generally not fit for purpose [37].
Training the professional
Training healthcare personnel to deliver and support self-management is crucial, but insufficient as a sole intervention [7]. Even well-designed theoretically-based training for professionals, for example including generic consultation skills as well as specific knowledge about asthma self-management, may not enable the professional to implement their learning in routine practice if the organisation does not nurture and support the new skill. A trial in UK primary care failed to show a clinically meaningful improvement in clinical outcomes after providing a training workshop on self-management skills for asthma nurses [38]. The authors concluded that the pressures of routine practice, and the lack of commitment from the organisation to supporting self-management made it impossible for the nurses to develop and consolidate their skills.
Organisational priority
Effective implementation thus involves not only provision of patient education and training of professionals, but to be effective needs to be provided within an organisation that believes in and values self-management. The organisation has to invest in resources (such as information and template action plans) which are easily accessible to the clinicians as and when they are required in the course of routine practice. Self-management support must be appropriately prioritised within the organisation, and the success of implementation strategies monitored. Proactive management systems, such as including blank action plans with invitations for review, structured protocols for reviews, prompts on review templates, involvement of community pharmacists, telephone calls to provide ongoing support can all promote self-management [39].
Current practice tends to consider self-management as something delivered by one member of the team (typically an asthma nurse in the UK or an asthma educator in some other healthcare systems) [40], but for effective implementation, all members of the team need to contribute to supporting self-management. Table 3 lists a number of scenarios, adapted from the BTS/SIGN guideline [8], in which members of the team can contribute to reviewing and refining self-management.
Table 3.
Opportunities to review, refine and reinforce self-management
|
Reproduced from [8] with permission from the publisher.
Conclusion
Supported self-management improves clinical outcomes and is recommended unequivocally by asthma guidelines. A core component of effective self-management interventions is the provision of an agreed, written personalised action plan which advises on using regular medication, recognising deterioration and appropriate action to take. It is possible to implement asthma self-management in routine care but, to be effective, this requires a whole-systems approach, which considers patient education and resources, professional skills and motivational and organisational priorities and routines.
Further reading
Taylor SJC, Pinnock H, Epiphaniou E, et al. A rapid synthesis of the evidence on interventions supporting self-management for people with long-term conditions: (PRISMS – Practical Systematic Review of Self-Management Support for long-term conditions). Health Serv Deliv Res 2014; 2: DOI: 10.3310/hsdr02530
This overview of the self-management literature reviews the qualitative and quantitative evidence for supported self-management in asthma (and 13 other long-term conditions) and also synthesises the implementation literature. Supported self-management for asthma has the most robust evidence base of all the long-term conditions studied, including at the level of implementation. Practical conclusions inform strategies for clinicians and healthcare managers for integrating supported self-management into routine care.
British Thoracic Society/Scottish Intercollegiate Guideline Network. British Guideline on the Management of Asthma: 2014 update. Thorax 2014; 69: Suppl. 1, i1–i192. Available from www.sign.ac.uk.
Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention, 2014. Available from www.ginasthma.org.
These two national/global guidelines summarise the asthma self-management literature and provide evidence-based recommendations to inform standards of good practice. They both conclude that asthma self-management is an integral component of good asthma care.
Horne R. Compliance, adherence, and concordance: implications for asthma treatment. Chest 2006; 130: Suppl. 1, 65S–72S.
This clinical review considers the underlying reasons for patient non-adherence specifically in the context of asthma management and describes the role played by clinicians in promoting optimal medicine management.
Nunes V, Neilson J, O’Flynn N, et al. Medicines Adherence: involving patients in decisions about prescribed medicines and supporting adherence. London, National Collaborating Centre for Primary Care and Royal College of General Practitioners, 2009.
This UK guideline summarises the literature on adherence to medicines. It provides a practical insight into the reasons for non-adherence, and identifies approaches that clinicians can adopt to assess and improve adherence.
Educational questions
-
Supported asthma self-management:
should always include a personalised asthma action plan.
improves health outcomes.
is only suitable for patients willing and able to take responsibility for their asthma.
is appropriate for all people with asthma.
-
A personalised asthma action plan:
should include advice on doubling inhaled steroids.
may be based on peak flow or symptom monitoring.
should always be accompanied by a prescription for oral steroids.
is suitable for adults and children of all ages.
-
Implementation of supported asthma self-management:
can be delegated to an asthma nurse or asthma educator.
requires the buy-in of all professionals associated with the care of people with asthma.
needs flexible access to professional support.
involves integrating self-management within the routines of the healthcare organisation.
Suggested answers
a, b and d.
b.
b, c and d.
Footnotes
The ERS designates this educational activity for a maximum of 1 CME credit. For information on how to earn CME credits, please visit www.ers-education.org/e-learning/cme-tests
Conflict of interest H. Pinnock has received a grant from the National Institute for Health Research, Health Services and Delivery Research Programme and chairs the self-management Evidence Review Group for the British Thoracic Society/Scottish Intercollegiate Guideline Network British Asthma Guideline.
References
- 1.Wiener-Ogilvie S, Pinnock H, Huby G, et al. . Do practices comply with key recommendations of the British Asthma Guideline? If not, why not? Prim Care Respir J 2007; 16: 369–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stallberg B, Lisspers K, Hasselgren M, et al. . Asthma control in primary care in Sweden: a comparison between 2001 and 2005. Prim Care Respir J 2009; 18: 279–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sulaiman N, Aroni R, Thien F, et al. . Written Asthma Action Plans (WAAPs) in Melbourne general practices: a sequential mixed methods study. Prim Care Respir J 2011; 20: 161–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Asthma Facts: CDC’s National Asthma Control Program Grantees. Atlanta, U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, 2013. [Google Scholar]
- 5.Royal College of Physicians. Why asthma still kills: the National Review of Asthma Deaths (NRAD) Confidential Enquiry report London, RCP, 2014. [Google Scholar]
- 6.Adams K, Greiner AC, Corrigan JM, Eds. The 1st Annual Crossing the Quality Chasm Summit: A Focus on Communities. Washington, National Academic Press, 2004; p. 57. [PubMed] [Google Scholar]
- 7.Taylor SJC, Pinnock H, Epiphaniou E, et al. . A rapid synthesis of the evidence on interventions supporting self-management for people with long-term conditions: PRISMS – Practical Systematic Review of Self-Management Support for long-term conditions. Health Serv Deliv Res 2014; 2: DOI: 10.3310/hsdr02530. [PubMed] [Google Scholar]
- 8.British Thoracic Society/Scottish Intercollegiate Guideline Network. British Guideline on the Management of Asthma: 2014 update. Thorax 2014; 69: Suppl. 1, i1–i192. [PubMed] [Google Scholar]
- 9.Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention. 2014. www.ginasthma.org Date last accessed: January, 2015.
- 10.Gibson PG, Powell H, Wilson A, et al. . Self-management education and regular practitioner review for adults with asthma. Cochrane Database Syst Rev 2002; 3: CD001117. [DOI] [PubMed] [Google Scholar]
- 11.Boyd M, Lasserson TJ, McKean MC, et al. . Interventions for educating children who are at risk of asthma-related emergency department attendance. Cochrane Database Syst Rev 2009; 2:CD001290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wolf F, Guevara JP, Grum CM, et al. . Educational interventions for asthma in children. Cochrane Database Syst Rev 2002; 4: CD000326. [DOI] [PubMed] [Google Scholar]
- 13.Stevens CA, Wesseldine LJ, Couriel JM, et al. . Parental education and guided self-management of asthma and wheezing in the pre-school child: a randomised controlled trial. Thorax 2002; 57: 39–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moudgil H, Marshall T, Honeybourne D. Asthma education and quality of life in the community: a randomised controlled study to evaluate the impact on white European and Indian subcontinent ethnic groups from socioeconomically deprived areas in Birmingham, UK. Thorax 2000; 55: 177–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Press VG, Pappalardo AA, Conwell WD, et al. . Interventions to improve outcomes for minority adults with asthma: a systematic review. J Gen Intern Med 2012; 27: 1001–1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Coffman JM, Cabana MD, Yelin EH. Do school-based asthma education programs improve self-management and health outcomes? Pediatrics 2009; 124: 729–742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.van Staa TP, Cooper C, Leufkens HG, et al. . The use of inhaled corticosteroids in the United Kingdom and the Netherlands. Respir Med 2003; 97: 578–585. [DOI] [PubMed] [Google Scholar]
- 18.Horne R. Compliance, adherence, and concordance: implications for asthma treatment. Chest 2006; 130: Suppl. 1, 65S–72S. [DOI] [PubMed] [Google Scholar]
- 19.Nunes V, Neilson J, O’Flynn N, et al. . Medicines Adherence: involving patients in decisions about prescribed medicines and supporting adherence. London, National Collaborating Centre for Primary Care and Royal College of General Practitioners, 2009. [PubMed] [Google Scholar]
- 20.Gibson PG, Powell H. Written action plans for asthma: an evidence-based review of the key components. Thorax 2004; 59: 94–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Honkoop PJ, Taylor DR, Smith AD, et al. . Early detection of asthma exacerbations by using action points in self-management plans. Eur Respir J 2013; 41: 53–59. [DOI] [PubMed] [Google Scholar]
- 22.Zemek RL, Bhogal SK, Ducharme FM. Systematic review of randomized controlled trials examining written action plans in children: what is the plan? Arch Pediatr Adolesc Med 2008; 162: 157–163. [DOI] [PubMed] [Google Scholar]
- 23.Harrison TW, Oborne J, Newton S, et al. . Doubling the dose of inhaled corticosteroid to prevent asthma exacerbations: randomised controlled trial. Lancet 2004; 363: 271–275. [DOI] [PubMed] [Google Scholar]
- 24.Foresi A, Morelli MC, Catena E, et al. . Low-dose budesonide with the addition of an increased dose during exacerbations is effective in long-term asthma control. Chest 2000; 117: 440–446. [DOI] [PubMed] [Google Scholar]
- 25.Osman LM, Calder C, Godden DJ, et al. . A randomised trial of self-management planning for adult patients admitted to hospital with acute asthma. Thorax 2002; 57: 869–874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ring N, Jepson R, Hoskins G, et al. . Understanding what helps or hinders asthma action plan use: a systematic review and synthesis of the qualitative literature. Patient Educ Counsel 2011; 85: e131–e143. [DOI] [PubMed] [Google Scholar]
- 27.Gannon PJ, Weir DC, Robertson AS, et al. . Health, employment, and financial outcomes in workers with occupational asthma. Br J Ind Med 1993; 50: 491–496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pinnock H, Ehrlich E, Hoskins G, et al. . A woman with asthma: a whole systems approach to supporting self-management. NPJ Prim Care Respir Med 2014; 24: 14063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wilson SR, Strub P, Buist AS, et al. . Shared treatment decision making improves adherence and outcomes in poorly controlled asthma. Am J Respir Crit Care Med 2010; 181: 566–577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Williams B, Steven K, Sullivan F. Tacit and transitionary: an exploration of patients’ and primary care health professionals’ goals in relation to asthma. Soc Sci Med 2011; 72: 1359–1366. [DOI] [PubMed] [Google Scholar]
- 31.Kielmann T, Huby G, Powell A, et al. . From support to boundary: A qualitative study of the border between self-care and professional care. Patient Educ Counsel 2010; 79: 55–61. [DOI] [PubMed] [Google Scholar]
- 32.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA 2002; 288: 1775e9. [DOI] [PubMed] [Google Scholar]
- 33.NHS England. House of Care. www.england.nhs.uk/resources/resources-for-ccgs/out-frwrk/dom-2/house-of-care Date last accessed: February, 2015.
- 34.Moullec G, Gour-Provencal G, Bacon S, et al. . Efficacy of interventions to improve adherence to inhaled corticosteroids in adult asthmatics: Impact of using components of the chronic care model. Respir Med 2012; 106: 1211e1225. [DOI] [PubMed] [Google Scholar]
- 35.British Thoracic Society, Research Unit of the Royal College of Physicians of London, King’s Fund Centre, National Asthma Campaign. Guidelines for management of asthma in adults: I-chronic persistent asthma. BMJ 1990; 301: 651–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Marcano Belisario JS, Huckvale K, Greenfield G, et al. . Smartphone and tablet self-management apps for asthma. Cochrane Database Syst Rev 2013; 11: CD010013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Huckvale K, Car M, Morrison C, et al. . Apps for asthma self-management: a systematic assessment of content and tools. BMC Med 2012; 10: 144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cleland JA, Hall S, Price D, et al. . An exploratory, pragmatic, cluster randomised trial of practice nurse training in the use of asthma action plans. Prim Care Respir J 2007; 16: 311–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ring N, Malcolm C, Wyke S, et al. . Promoting the use of Personal Asthma Action Plans: a systematic review. Prim Care Respir J 2007; 16: 271–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Weiner-Ogilvie S, Huby G, Pinnock H, et al. . Practice organisational characteristics can impact on compliance with the BTS/SIGN asthma guideline: qualitative comparative case study in primary care. BMC Fam Pract 2008; 9: 32. [DOI] [PMC free article] [PubMed] [Google Scholar]