Educational aims
To highlight the risk of domestic fires in the home use of oxygen
To recommend measures to reduce the risk
Introduction
Oxygen can be both a saviour and a killer. As one of the elements of the fire triangle (heat, fuel and oxygen), it has the potential to kill and injure very easily. However, as a treatment for respiratory and cardiac failure, it is a successful lifesaver [1–3]. The risks of home oxygen services (HOS), their usage and house fires are intuitively obvious [4], but are those risks actually more than just tobacco smoking? Does the problem of duty of care extend beyond the patient being treated? This article aims to highlight the key issues of home oxygen, safety and fires in the home.
The enrichment of normal room air with oxygen increases the energy, heat release and severity of any fire. What can normally be a fairly nonflammable substance can, in the presence of oxygen, burn with vigour and produce noxious fumes very rapidly.
Risks of home oxygen
The greatest risk for oxygen users is tobacco smoking when using oxygen. Of course, it is not just tobacco smoking [5, 6] that is a risk to home oxygen patients (fig. 1), as any naked flame can be a serious hazard. Indeed, the hazards of home oxygen fires are not always obvious and reports of fires and near misses include a wide range of common (and not so common) activities (table 1) [7–10].
Figure 1.
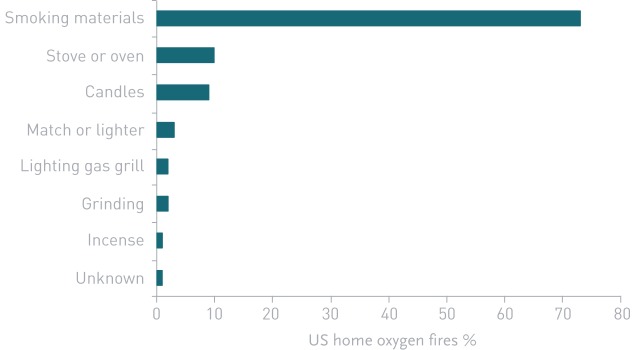
Causes of home oxygen fires the USA, 2003–2006. Data from the US National Electronic Injury Surveillance System.
Table 1.
Hazards for home oxygen usage
| Hazard | Specific risks |
| Tobacco smoking | Burning substances, naked flames (matches, lighters, etc.) |
| Cooking | Naked gas flames, barbecues (gas or charcoal) |
| Candles | Birthday cakes, scented candles, decorative candles, lanterns |
| Household heating | Gas fires, coal fires, log burners, oil fired heaters, etc. |
| Outdoor | Bonfires, fireworks, gas patio heaters |
| Flammable materials | Cleaning fluids, paint thinners, petroleum spirit (e.g. for lawn mowers, strimmers and saws), petroleum-based creams or aerosols, alcohols, acetone, some nail-varnish removers, oils, greases or lotions, etc. |
| Sparks | Grinders, children's toys, some electric shavers |
| Other | High-frequency, short-wave and laser equipment; hair dryers; arcing, “electronic cigarettes” |
The outcomes of fires involving home oxygen can be categorised into different scales of damage and risk:
Minor damage to fixtures and fittings.
Major damage to property (requiring rehousing, etc.) and/or minor injury.
Injury requiring medical treatment.
Injury requiring hospitalisation.
Fatality.
The last three categories are more likely to be reported because legislation and reporting systems are usually put in place by oxygen providers, but the size of the home oxygen/house fires and smoking problem is largely under-estimated because smoking patients rarely report minor incidents because they feel they will be blamed for the incident. Often, visiting healthcare staff or oxygen supply personnel will record indications of smoking damage to property and even burns to the patient. Fires burn hotter and faster in oxygen-enriched atmospheres so usually nonflammable things can ignite at lower temperatures. The materials that oxygen cannulae are made from, for example, can become highly flammable and cause serious injury irrespective of the poisonous fumes they give off when burning. Similarly, clothing, bedding and an array of household materials can suddenly become a risk to combustion in the presence of oxygen-enriched air. This is also true for “electronic cigarettes”, which the European Industrial Gases Association has declared to be unsafe to use with home oxygen.
Estimates of home oxygen users who continue to smoke range from 14% to 51% [11], which presents as a significant safety issue given the number of patients across Europe on home oxygen therapy. However, there are few European data available to capture the size of the problem of what additional measures should be provided and what additional precautions might be useful (e.g. smoke alarms or fire extinguishers). Although the World Health Organization collects total fire death statistics (table 2), these are not broken down into home fires or fires in homes where oxygen is being used. Indeed, data on how many patients in Europe are on home oxygen are difficult to obtain, although the financial market statistics for medical oxygen are available for commercial interests.
Table 2.
Death rates from all fires across Europe
| Country | Deaths per 100 000 population (2008–2010) |
| Switzerland | 0.34 |
| Italy | 0.45 |
| Netherlands | 0.46 |
| Austria | 0.47 |
| Slovenia | 0.49 |
| Spain | 0.52 |
| Portugal | 0.57 |
| Germany | 0.60 |
| UK | 0.75 |
| France | 0.96 |
| Greece | 1.05 |
| Norway | 1.14 |
| Ireland | 1.17 |
| Belgium | 1.21 |
| Czech Republic | 1.35 |
| Denmark | 1.36 |
| Sweden | 1.49 |
| Poland | 1.52 |
| Hungary | 1.53 |
| Romania | 1.76 |
| Finland | 2.03 |
Data from the World Health Organization.
Some European countries do have data on how many fires occur with home oxygen but there is inadequate coordination to publish this information centrally. This inconsistency in records occurs despite a European Union Medical Device Directive requiring the reporting of incidents to national vigilance authorities, but based upon the experience of the German Vigilance Authority, it is very likely that such incidents are grossly under-reported. Fortunately, there are some reliable data from the USA as well as the UK because of the NHS Service Specification for Home Oxygen (4.4.1.8) [12] that requires the central reporting of all adverse incidents.
The experience in the USA
An analysis of deaths in four US states as a direct result of home oxygen fires caused by smoking was undertaken by Wendling et al. [13] in 2008. This analysis drew from a variety of data sources, and covered home oxygen fires in Maine, Massachusetts, New Hampshire and Oklahoma (the Maine Group). Over an 8-year period (2000–2007), Wendling et al. [13] identified 38 deaths attributable to home oxygen fires caused by smoking. The Maine Group represents a population of 13 million (4.3% of the US total population in 2010), so extrapolation of the data gives a crude estimate for the whole of the USA.
Further US data that are available online from the Consumer Product Safety Commission's National Electronic Injury Surveillance System (2003–2006) shows that home medical oxygen was involved in an average of 1190 thermal burns seen annually in US emergency rooms. Uniquely, in the USA, details of home fires involving oxygen are recorded annually.
Amongst the most helpful information, because it is recorded centrally and published annually, are data from version 5.0 of the US Fire Administration's National Fire Incident Reporting System, which indicate that, in 2002–2005, US fire departments responded to an estimated average of 182 home fires per year in which home oxygen equipment was directly involved in the fire itself. 46 people died in these fires per year and smoking was by far the leading factor in these incidents (see also fig. 1). Several studies suggest that the number of burn injuries associated with home use of medical oxygen has been increasing over time.
Strict requirements regulate the use and storage of medical oxygen in healthcare facilities, yet few regulations apply in the home environment. Finding the balance between preserving the patient's privacy and protecting safety is a multidisciplinary challenge.
The experience in the UK
Lindford et al. [10] published a review that identified and compared all reported cases of burns in home oxygen users in the UK. Patient demographics, oxygen delivery type, injury severity, tobacco smoking and patient outcome were all recorded. They found four major series [5, 14–16] and, from these, they reported that in 86 cases of home oxygen burns:
The mean age of the patients was 65 years.
The most common diagnosis was chronic obstructive pulmonary disease (COPD).
63% were smokers, 13% were nonsmokers and 24% were unspecified.
The average burn size was 8.1% of total body surface area, with seven patients sustaining full-thickness burns and two requiring skin grafts.
24% patients suffered an inhalational injury.
The length of hospital stay averaged 4.6 days.
Nine (10.5%) patients died.
From this, it is clear that those at greatest risk of injury are the elderly who smoke and use HOS. Further statistics indicate that the elderly are twice as likely to die in a home fire than younger people [17].
Another study of burns patients who had been smoking and using home oxygen at the time of their injury collected retrospective epidemiological data on patients treated in 1999–2008 [18]. 17 COPD patients sustained injuries secondary to smoking on HOS over the 9-year period; 11.8% (two out of 17) sustained inhalation injury requiring intubation and 23.5% (four out of 17) required wound debridement and skin grafting. Mean hospital stay was greater (42.8±12.5 versus 10.3±5.4 days) in the intensive care unit and 32.5±11.0 days in the ward. On discharge from hospital, most produced an excessive burden on the local healthcare facilities (47.1% in extended care facilities, 11.8% died during their hospitalisation and there was a 35.3% reduction in patients able to return home and/or live independently). These patients were older, had higher rates of inhalation injury and had much longer lengths of hospitalisation, despite smaller burns injuries than routine burns patients. They concluded that prevention of such injuries would improve the safety of the patient and those around them as well as healthcare resource allocation. This finding that elderly COPD patients who smoke while on oxygen are at greatest risk of death from a home fire is a fact of which many home oxygen services are only too well aware.
There are unique UK data from one oxygen provider (Air Products, Allentown, PA, USA) that show detail of the scale of oxygen fire incidents. Details of the analysis of serious events of adverse nature (SEANs) reports between 2010 and 2012 on investigated SEANs related to fire and smoking events in several regions of the UK are given in table 3. These represent 62 (44%) out of 140 incidents reported at levels 3–5, in which patients sustained injuries requiring medical treatment (level 3) or hospitalisation (level 4) or fatalities (level 5). These regional variations (0.08–0.20%) in the number of fires/patients on oxygen cannot be easily explained despite reasonable standardisation of service delivery. However, the overall average is the first published national average figure (0.12%) for fire/oxygen events in UK home oxygen patients.
Table 3.
Analysis of UK home oxygen service serious events of adverse nature (SEANs) by region, 2010–2012
| Region | Level 3–5 SEAN | Patients | Patients per SEAN | Fires per patient % |
| Yorkshire and Humber | 18 | 9000 | 500 | 0.20 |
| West Midlands | 13 | 9500 | 725 | 0.13 |
| North London | 7 | 6500 | 925 | 0.11 |
| North West | 12 | 13 000 | 1075 | 0.09 |
| Wales | 6 | 7000 | 1150 | 0.09 |
| East Midlands | 6 | 8000 | 1325 | 0.08 |
| All regions | 62 | 53 000 | 1170 | 0.12 |
Annualised data: one level 3–5 SEAN per 1060 patients per annum (Air Products, Allentown, PA, USA).
To put this in perspective, annually, there are usually about 30 000 house fires in the UK (population 55 million), giving an incidence of 0.06% fires per citizen. This puts the incidence of home fires with oxygen (level 3–5) as twice that of the general population.
Further analysis of the severity of the adverse events (table 4) shows that tobacco smoking was strongly associated with house fires with home oxygen.
Table 4.
Analysis of UK home oxygen service serious events of adverse nature (SEANs) by severity
| SEAN level | Smoking | Fire | Total |
| Level 5: fatal | 2 (50%) | 2 (50%) | 4 |
| Level 4: hospitalisation | 6 (46%) | 7 (54%) | 13 |
| Level 3: medical attention | 35 (78%) | 10(22%) | 45 |
Data are from October 1, 2009 to November 8, 2010 (Air Products, Allentown, PA, USA).
Causes of SEANs unrelated to smoking (table 5) are linked to gas cookers, candles and matches, but generally lead to less severe adverse events. Clearly, the addition of oxygen in the home where fires can happen anyway increases the risks of both the development and severity of house fires.
Table 5.
Analysis of nonsmoking fires
| Advised cause | SEAN level | |||
| Level 3 | Level 4 | Level 5 | Total | |
| Gas cooker | 3 | 1 | 4 | |
| Candles | 4 | 4 | ||
| Lighters and matches | 2 | 2 | ||
| Electric fire | 1 | 1 | ||
| House fires | 2 | 2 | ||
| Unknown cause | 1 | 5 | 6 | |
Data are from October 1, 2009 to November 8, 2010 (Air Products, Allentown, PA, USA).
SEAN: serious events of adverse nature.
It could be argued that a single oxygen provider may operate different levels of safety when delivering HOS and that these data therefore give a false impression of the overall risks. Table 6 shows data collected over the same period for the three UK HOS providers. There appear to be different levels of reporting of incidents or there are different numbers of incidents occurring across the whole of the UK. Further research is required in these areas. As a part of the UK HOS contract, providers have to report all fire-related incidents with home oxygen to the UK Department of Health. Further analysis of those data should produce clear safety messages and actions to improve prevention.
Table 6.
National data on UK home oxygen service serious events of adverse nature (SEANs)
| SEAN level | |||
| Level 3 | Level 4 | Level 5 | |
| Air Products | 29 | 6 | 4 |
| Air Liquide | 6 | 3 | 1 |
| BOC | 1 | 0 | 1 |
| Total | 36 | 9 | 6 |
| O2 fires | 70.5% | 17.6% | 11.8% |
Data are from October 2009 to July 2010.
There are insufficient European data to compare adverse events with home oxygen fires between countries, but comparison with the abundant USA data shows the UK to have about half the death rate due to fires with home oxygen (table 7). One possible explanation for this difference is that in the UK, “fire-breaks” (see later) are mandatory, whereas in the USA they are optional. Of course, there may be other explanations, such as that many US homes are built of wood rather than brick, and there may be different levels of smoke detector usage or policy on issuing home oxygen to smokers. Nevertheless, as International Organization for Standardization (ISO) standards for home oxygen become stricter worldwide and the USA adopts fire-breaks, then it will be interesting to see if the death rates fall in home oxygen users in the USA.
Table 7.
Comparison of US and UK deaths from home fires with oxygen
| Maine Group | England and Wales | |
| Population, millions | 13.14 | 55.2 |
| % national population | 4.3% | 100% |
| Oxygen users# | 76 792 | 90 000¶ |
| Average deaths per year | 4.75 | 3.2 |
| Deaths per year per 10 million population | 3.6 | 0.58 |
| Deaths per year per 10 000 O2 users | 0.62 | 0.36 |
#: 0.58% of the US population; ¶: known data.
Legal issues
The whole issue of tobacco smoking and home oxygen is full of controversy with ethical arguments of discrimination against smokers who, after all, may have an addiction, and who cannot therefore have treatments withheld. However, recent cases in the UK involving legal opinion have found that healthcare practitioners have a duty of care not just for the patient but also for protecting relatives, neighbours and carers who live in and around homes with an oxygen patient who smokes. This is even more important in elderly care homes where confused patients who smoke and are on oxygen may endanger the lives of often many residents.
Recommendations for prevention
So having described the risk of home fires with oxygen, what actions can be taken to reduce the incidence of injury and death? There are a variety of preventive steps that can reduce the severity of injury or avoidance of death from these fires.
Smoking cessation
Smoking cessation in people who use home oxygen is by far the best way to reduce deaths from house fires in this patient group (and those who live around them). Healthcare staff should do all they can to help stop smokers before they commence home oxygen.
Fire-breaks
The ISO standard for oxygen concentrators, ISO 8359 amendment, now requires that safety devices be added to all oxygen concentrators and accessories to reduce the acceleration of fires. This has been approved by many countries and, therefore, affects manufacturers that do business worldwide. The amendment requires two safety devices:
A fire-break, such as a metal fitting or metal plate, at the outlet of the oxygen concentrator.
A “flow stop” device in the tubing.
Implementation of this across Europe can only reduce the deaths and serious injuries caused by these fires.
Dramatic videos of the “cannula fuse” [19] demonstrate the speed of the flame and the large amount of toxic black smoke emitted from less than a metre of polyvinyl chloride cannula tubing. The fire-break stops the flame immediately at the point in the tubing where it is installed. Ironically, the higher the flow of oxygen used the slower the cannula burns, but the more intense the fire becomes. With pulsed oxygen, the risk of this cannula effect is reduced.
However, some critics (e.g. AirSep Corp., Buffalo, NY, USA) point out that there are limitations to fire-breaks (see website). They do not reduce the occurrence of fires or awaken individuals when they occur (especially patients falling asleep in bed while smoking). They do not extinguish the fires because the flames often initiate secondary fires of combustible items such as clothing, bedding, carpeting, curtains or furniture. A fire can also jump sections of coiled tubing and bypass the fire-break, and they are useless if inserted the wrong way by patients. Sometimes, they need to be removed during pulse-flow delivery because they offer a resistance to flow.
Risk assessments in the home
The UK National Framework Agreement for Home Oxygen Services (December 2000, transitioned to NHS England 2013) [12] outlines the contractual obligations of HOS companies in England, Wales and Scotland. All contracted suppliers are obliged to carry out a home risk assessment prior to oxygen installation.
This includes a field-based risk assessment to identify potential fire-related risks in the patient's home, and should include:
An assessment of the presence of an operational smoke detector or alarm (if no smoke detector or fire alarm is present, the supplier must inform the local fire authorities together with any specific fire risks that have been identified).
The assessment should take into account the risk to relatives, neighbours and carers who live in and around homes with an oxygen patient who smokes.
A check to see if the concentrator and any cylinders are positioned with sufficient ventilation and at a safe distance from any naked flame, cooking or heating appliance.
The oxygen contractor should inform the assessment service of any safety issues concerning the patient and the oxygen equipment and its use.
These are the UK recommendations; however, what can respiratory clinicians in Europe do to make oxygen in the home safer and reduce the number of deaths and injuries from oxygen-related home fires?
Actions by healthcare teams for prevention of burns and fatalities in home fires with HOS
Smoking cessation for oxygen users is essential.
The implementation of fire-breaks, not just for oxygen concentrators but for all cylinder and liquid oxygen.
Educating patients and carers of the dangers of home oxygen and fires (especially smoking).
Ultimately, advising legal withdrawal of oxygen where it is a risk to others as well as the patient.
Where necessary, the fire and rescue service or a community fire safety officer should visit to discuss fire safety, smoke alarms and safe exit routes in the event of a fire.
What can industry and professional bodies do to help at national and international levels?
Use of less combustible material for cannula tubing and a more efficient oxygen delivery system may reduce the incidence of such burns.
Clearly labelling oxygen cylinders with large stickers emphasising the danger of smoking in the presence of oxygen.
Collect and publish national and European wide statistics on home fires with HOS. Such data should be routinely provided to oxygen assessment services.
What can the patient do to reduce the risk of injury or death from fires?
Patients should take a few additional measures and precautions such as installing working (and routinely checked) smoke alarms, perhaps possessing a fire extinguisher and working out a simple plan of what they should do in the event of a fire (turn off the oxygen supply, use a pre-planned escape route, ensure doors windows can be accessed safely, etc.).
In some countries, it is usual to notify fire services that you have oxygen at home. Sometimes (but rarely) it may be necessary to contact insurance companies. These steps vary from country to country. It may also be useful for patients and carers to know some simple, first-aid advice about what should be done with minor burns.
Conclusion
Supplemental oxygen is potentially a serious risk to fire safety in the home. Approximately 0.12% of patients on oxygen have a serious adverse event involving fire while on home oxygen in the UK. They have twice the risk of a serious fire in the home compared with the general population, but this average figure is variable and the risk may be much greater than this. The figures for other European countries are unknown, but given the variation in the incidence of all deaths from fire generally in Europe, there is a large potential health and mortality problem. It is the responsibility of healthcare professionals to warn and advise patients about the risks of naked flames, smoking and home oxygen. However, smoking cessation is probably the best method of reducing deaths from home fires with oxygen, followed by adequate risk assessment of patients and others living nearby before oxygen is put in the home. Educating patients and carers of the risk must be a high priority to save life and injury.
Acknowledgement
I am grateful to Ben Johnson of BPR Medical (Mansfield, UK) for information and data regarding home oxygen use and fires in the home. I receive no benefit from this company.
Footnotes
This article has been reproduced from the ERS Buyers' Guide 2014/2015: 61–69
Conflict of interest B.G. Cooper was a member of the Air Products Clinical Governance Committee from 2007 to 2012, receiving minimal travel re-imbursement and no personal or departmental benefits.
References
- 1.Barach AL. The therapeutic use of oxygen. JAMA 1922; 79: 693–638. [Google Scholar]
- 2.Nocturnal Oxygen Therapy Trial Group. Continuous or nocturnal oxygen therapy in hypoxaemic chronic obstructive lung disease: a clinical trial. Ann Intern Med 1980; 93: 391–398. [DOI] [PubMed] [Google Scholar]
- 3.Medical Research Working Party. Long-term domiciliary oxygen therapy in chronic hypoxic cor pulmonale complicating chronic bronchitis and emphysema. Lancet 1981; 1: 681–686. [PubMed] [Google Scholar]
- 4.Maxwell DL, McGlashan JA, Andrews S, et al. . Hazards of domiciliary oxygen therapy. Respir Med 1993; 87: 225–226. [DOI] [PubMed] [Google Scholar]
- 5.Muehlberger T, Smith MA, Wong L. Domiciliary oxygen and smoking: an explosive combination. Burns 1998; 24: 658–660. [DOI] [PubMed] [Google Scholar]
- 6.Burns HL, Ralston D, Muller M, et al. . Cooking and oxygen. An explosive recipe. Aust Fam Physician 2001; 30: 138–140. [PubMed] [Google Scholar]
- 7.Laubscher B. Home oxygen therapy: beware of birthday cakes. Arch Dis Child 2003; 88: 1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McCauley CS, Boller LR. The hazards of home oxygen therapy. N Engl J Med 1987; 316: 107. [DOI] [PubMed] [Google Scholar]
- 9.Stobie TD, Finucane P. Going up in smoke. Med J Aust 1995; 163: 656. [DOI] [PubMed] [Google Scholar]
- 10.Lindford AJ, Tehrani H, Sassoon EM, et al. . Home oxygen therapy and cigarette smoking: a dangerous practice. Ann Burns Fire Disasters 2006; 19: 99–100. [PMC free article] [PubMed] [Google Scholar]
- 11.Shiner RJ, Zaretsky U, Mirali M, et al. . Evaluation of domiciliary long-term oxygen therapy with oxygen concentrators. Israel J Med Sci 1997; 33: 23–29. [PubMed] [Google Scholar]
- 12.Dept of Health. NHS Primary Care Commissioning. www.pcc.nhs.uk/home-oxygen-service
- 13.Wendling T, Pelletier A. Fatal fires associated with smoking during long-term oxygen therapy – Maine, Massachusetts, New Hampshire and Oklahoma 2000–2007. MMWR Morb Mortal Wkly Rep 2008; 57: 852–854. [PubMed] [Google Scholar]
- 14.Robb BW, Hungness ES, Hershko DD, et al. . Home oxygen therapy: 14 adjunct or risk factor? J Burn Care Rehabil 2003; 24: 403–406. [DOI] [PubMed] [Google Scholar]
- 15.Chang TT, Lipinski CA, Sherman HF. A hazard of home oxygen therapy. J Burn Care Rehabil 2001; 22: 71–74. [DOI] [PubMed] [Google Scholar]
- 16.Barillo DJ, Coffey EC, Shirani KZ, et al. . Burns caused by medical therapy. J Burn Care Rehabil 2001; 21: 269–273. [DOI] [PubMed] [Google Scholar]
- 17.US Fire Administration, National Fire Data Center. Fire risk: topical fire research series, volume 4 – issue 7. www.usfa.fema.gov/downloads/pdf/statistics/v4i7.pdf [Google Scholar]
- 18.Murabit A, Tredget EE. Review of burn injuries secondary to home oxygen. J Burn Care Res 2012; 33: 212–217. [DOI] [PubMed] [Google Scholar]
- 19.BBC News Nottingham. BPR Medical wins award for oxygen fire valve. www.bbc.co.uk/news/uk-england-nottinghamshire-20021447 Date last updated: October 22, 2012.


