Abstract
Objective
To statistically analyze the results obtained from biomechanical tests on fixation of femoral neck fractures of Pauwels III type, in synthetic bone, using the dynamic hip system with an anti-rotation screw, versus a control group.
Methods
Ten synthetic bones from a Brazilian manufacturer (model C1010) were used and divided into two groups: test and control. In the test group, fixation of an osteotomy was performed with 70° of inclination at the level of the femoral neck, using DHS with an anti-rotation screw. The resistance of this fixation was evaluated, along with its rotational deviation at 5 mm of displacement (phase 1) and at 10 mm of displacement (phase 2), which was considered to be failure of synthesis. In the control group, the models were tested in their entirety until femoral neck fracturing occurred.
Results
The test values in the test group (samples 1–5) in phase 1 were: 1512 N, 1439 N, 1205 N, 1251 N and 1273 N, respectively (mean = 1336 N; standard deviation [SD] = 132 N). The rotational deviations were: 4.90°, 3.27°, 2.62°, 0.66° and 0.66°, respectively (mean = 2.42°; SD = 1.81°). In phase 2, we obtained: 2064 N, 1895 N, 1682 N, 1713 N and 1354 N, respectively (mean = 1742 N; SD = 265 N). The failure loading values in the control group were: 1544 N, 1110 N, 1359 N, 1194 N and 1437 N, respectively (mean = 1329 N; SD = 177 N). The statistical analysis using the Mann–Whitney test showed that the test group presented maximum loading at a displacement of 10 mm, i.e. significantly greater than the failure loading of the control group (p = 0.047).
Conclusion
The mechanical resistance of the test group was significantly greater than that of the control group.
Keywords: Femoral neck fractures, Internal fixators, Biomechanics
Resumo
Objetivo
Analisar estatisticamente resultados obtidos em ensaios biomecânicos de fixação de fratura do colo femoral tipo Pauwels III, em osso sintético, com o uso do sistema dinâmico do quadril (DHS) com parafuso antirrotatório vs um grupo controle.
Métodos
Foram usados dez ossos sintéticos, de um fabricante nacional, do modelo C1010, divididos em dois grupos: teste e controle. No grupo teste foi feita fixação de osteotomia, com 70° de inclinação em nível de colo femoral, com o uso de DHS com parafuso antirrotatório. Avaliou-se a resistência dessa fixação e seu desvio rotacional em 5 mm de deslocamento (fase 1) e em 10 mm de deslocamento, considerado como falência da síntese (fase 2). No grupo controle, os modelos foram ensaiados em sua integridade até que ocorresse a fraturado colo femoral.
Resultados
Os valores do ensaio no grupo teste na fase 1, nas amostras de 1 a 5, foram:1.512 N, 1.439 N, 1.205 N, 1.251 N e 1.273 N, respectivamente (média = 1.336 N; desvio padrão [DP] = 132 N). Os desvios rotacionais foram: 4,90°; 3,27°; 2,62°; 0,66° e 0,66°, respectivamente (média = 2,42°; DP = 1,81°). Na fase 2, obtivemos: 2.064 N, 1.895 N, 1.682 N, 1.713 N e 1.354 N,respectivamente (média = 1.742 N; DP = 265 N). Os valores da carga de falência no grupo con-trole foram: 1.544 N, 1.110 N, 1.359 N, 1.194 N e 1.437 N, respectivamente (média = 1.329 N; DP = 177 N). A análise estatística pelo teste de Mann-Whitney demonstrou que o grupo testeapresentou carga máxima, em 10 mm de deslocamento, significativamente maior do que acarga de falência do grupo controle (p = 0,047).
Conclusão
A resistência mecânica do grupo teste foi significativamente superior à do grupo controle.
Palavras-chave: Fraturas do colo femoral, Fixadores internos, Biomecânica
Introduction
Hip fractures account for around 20% of the surgical fractures seen at orthopedic trauma units and generate significant annual cost in any healthcare system. Femoral neck fractures account for approximately 50% of all fractures of the hip region. They mainly affect elderly people and are uncommon among individuals under the age of 60 years.1
The World Health Organization has predicted that the incidence of osteoporotic fractures of the proximal femur will triple by 2050.2 In the population under the age of 65 years, the incidence of femoral neck fractures is 2–4 cases per 10,000 inhabitants. However, the incidence is much higher in the population over the age of 70 years: 28/10,000 among men and 64/10,000 among women.3, 4
Among young adults, fractures in the hip region are generally uncommon. However, because of high-energy accidents involving sports practices and traffic accidents, this incidence has been increasing. The pattern of this type of fracture frequently has a vertical line with unstable characteristics, classified as Pauwels III. This classification correlates the prognosis with the angle of the fracture plane: as the angle increases, the instability of the fracture also increases and the complications relating to its fixation and consolidation worsen.1
The treatment for femoral neck fractures varies according to the patient's age and the fracture pattern.5 In young patients, osteosynthesis should always be prioritized, while in older patients, arthroplasty should be cogitated. For middle-aged patients (40–65 years), the indication should be defined individually.6
For femoral neck fractures without displacement, rigid fixation with early mobility for the patients is the standard treatment. Multiple cannulated screws (MCS) or the Dynamic Hip System (DHS) is commonly used in the treatment.5
Failure of fixation and pseudarthrosis are the main forms of complication following fixation of femoral neck fractures, with or without displacement. Pseudarthrosis occurs more commonly and affects between 3.1% and 8.8% of the cases, with a mean of around 6%.1
In the light of the situation described above, we proposed to conduct a statistical analysis in order to evaluate the mechanical resistance of the fixation of femoral neck fractures classified as Pauwels III, in which the DHS and antirotational screws were used in synthetic bones, in comparison with a control group.
Material and methods
Ten synthetic bones for the proximal third of the femur were used. These were from a Brazilian manufacturer (model C1010) and were made of rigid polyurethane for the cortical layer and trabeculated material for the spongy layer. The samples were divided into two groups: control and test.
All the samples of the test group were previously drilled for the initial placement of the implant under fluoroscopic guidance before the osteotomy, in order to facilitate anatomical reduction and ideal positioning for the implant. The osteotomies of the test group were performed using a prefabricated template so that there would not be any angular difference between them and in order to simulate a femoral neck fracture of Pauwels III type that would be the same in all the bones.
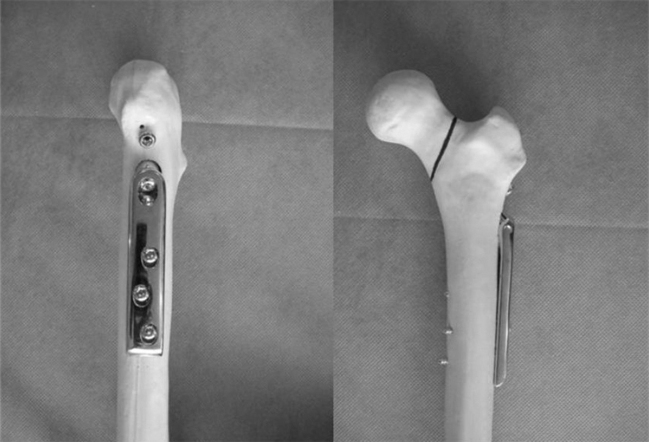
The fixations of the five bones of the test group were performed one by one using the DHS, with three holes and a guide of 135°. The reference point established for placing the 90 mm sliding screw was 2 cm distally to the lesser trochanter, at the center of the lateral diaphysis. The plate was fixed to the femoral diaphysis using three 4.5 mm cortical screws. Lastly, the system was locked using a cotterpin, which provided compression to the focus of the osteotomy. An antirotational screw was then placed by hand, positioned parallel to and above the sliding screw. To check for correct positioning, fluoroscopy in anteroposterior and lateral views was used during each stage of the procedure. After the procedure, all the bones in the test group (Fig. 1) were subjected to radiography to evaluate the reduction and whether the synthesis was well positioned (Fig. 2).
Fig. 1.
Synthetic bone fixed using DHS before the test.
Fig. 2.

Radiograph on synthetic bone fixed with DHS before the test.
The other five bones were used without interference with their integrity and were identified as the control group. In this manner, they simulated the maximum resistance load of the femoral neck of intact synthetic bone. Thus, they defined the gold standard for resistance prior to the occurrence of the fracture and the comparison parameter for the need for resistance in the synthesis method used in the test group (Fig. 3A and B).
Fig. 3.
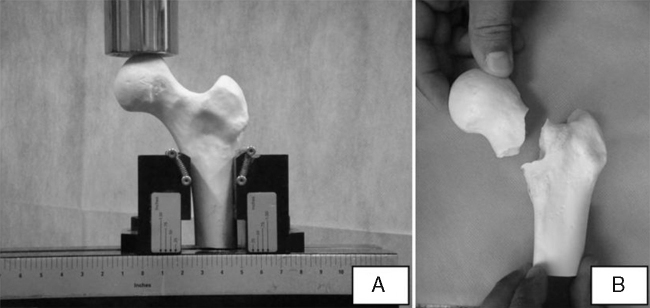
(A) Control in the machine before the test. (B) Control after the test, showing failure.
Test group
The fixed synthetic femurs were 200 mm in length and were positioned vertically with an inclination of 25° of valgus (Fig. 4A). The load application system transmitted the force on the apex of the femoral head and determined the force applied and load at the time of failure. The analysis on the mechanical test on this group was divided into two phases:
Fig. 4.
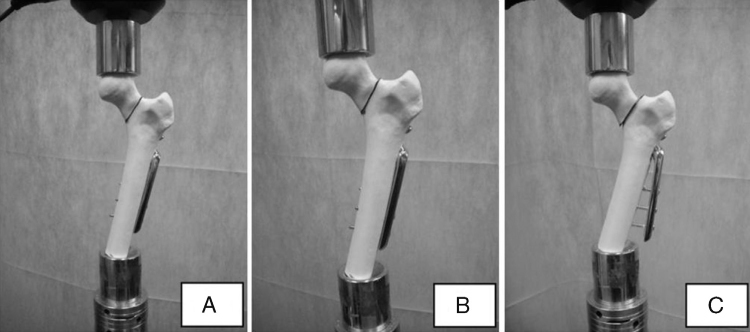
(A) DHS in the machine before the test. (B) DHS in phase 1 of the test. (C) DHS in phase 2 of the test.
Phase 1: resistance of the fixation with 5 mm of displacement (Fig. 4B).
Phase 2: resistance of the fixation with 10 mm of displacement, which was taken to be failure of the osteosynthesis (Fig. 4C).
During phase 1, the rotational displacements of the femoral neck were also evaluated (Fig. 5).
Fig. 5.
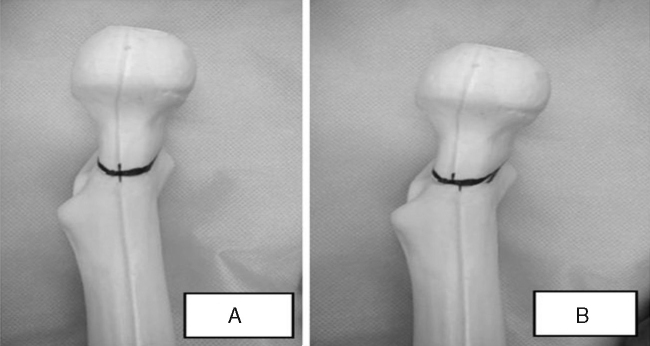
(A) DHS before the test, without rotational displacement. (B) DHS after the test, with rotational deviation.
The format of this test sought to concentrate the force applied on the focus of the osteotomy, in order to make a more appropriate analysis on the resistance of the synthesis assembly.
Control group
The non-fixed synthetic femurs were 125 mm in length and were positioned vertically, with neutral inclination. The load application system transmitted the force at the apex of the femoral head and this was applied until the femoral neck fractured (Fig. 3), in order to simulate the maximum pre-fracture resistance.
A load application velocity of 20 mm/min was used, in the Materials Testing System (MTS) machine (model 810 – FlexTest 40) with a capacity of 100 kN. In the test, a calibrated and measured load cell of capacity 10 kN was used. An axial force was applied to the femoral head by means of fitting it to the surface of the piston of the equipment (Fig. 6).
Fig. 6.
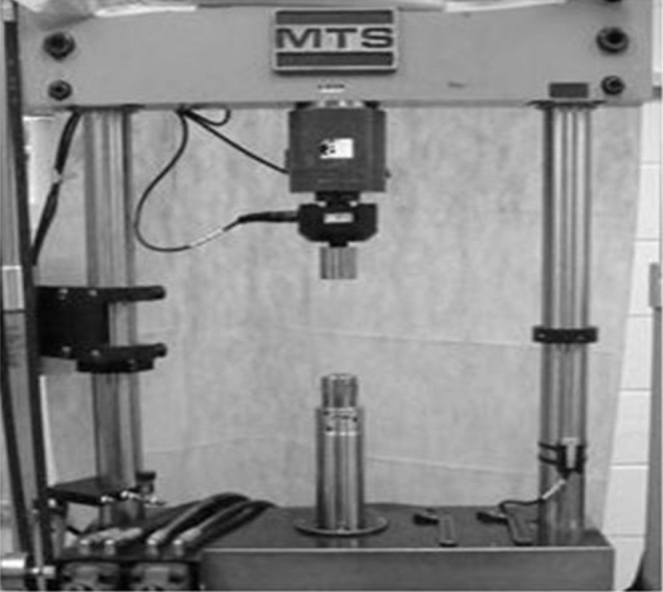
Test machine used.
Statistical analysis
The statistical method for comparing the maximum force (N) between the groups was the Mann–Whitney test. A nonparametric method was used because the maximum force did not present normal distribution (Gaussian distribution), due to the small number of samples analyzed in each group.
The criterion used for determining significance was the level of 5%. The statistical analysis was processed using the SAS 6.11 software (SAS Institute, Inc., Cary, North Carolina, USA).
Results
Test group
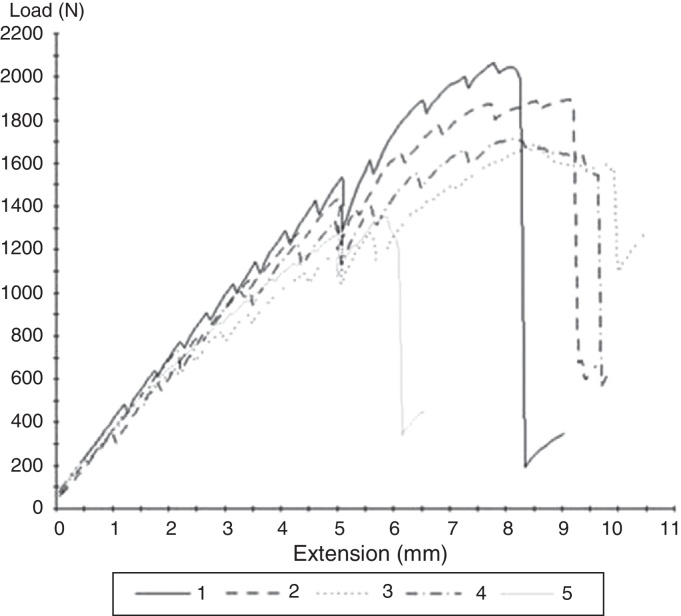
The load values in Newtons (N) that were applied until displacement of the fracture by 5 mm were: 1512, 1439, 1205, 1251 and 1273, respectively, for samples 1–5. The mean value was 1336 N, with a standard deviation of 132 N (Table 1, Fig. 7).
Table 1.
Load values in N with 5 mm of displacement, maximum load values and rotational displacement, in the test group.
| Sample | Load with 5 mm of displacement (N) | Maximum load (N) | Rotation (degrees) |
|---|---|---|---|
| 1 | 1512 | 2064 | 4.9 |
| 2 | 1439 | 1895 | 3.27 |
| 3 | 1205 | 1682 | 2.62 |
| 4 | 1251 | 1713 | 0.66 |
| 5 | 1273 | 1354 | 0.66 |
| Mean | 1336 | 1742 | 2.42 |
| Standard deviation | 132 | 265 | 1.81 |
Fig. 7.
Force vs. displacement curve for the test group.
The maximum load values in Newtons that were applied until displacement of the fracture by 10 mm were: 2064, 1895, 1682, 1713 and 1354, respectively, for samples 1–5. The mean value was 1742 N, with a standard deviation of 265 N (Table 1, Fig. 7).
The rotational displacement values for the five samples in degrees, after phase 1, were: 4.90°, 3.27°, 2.62°, 0.66° and 0.66°, respectively. The mean was 2.42° and the standard deviation was 1.81° (Table 1).
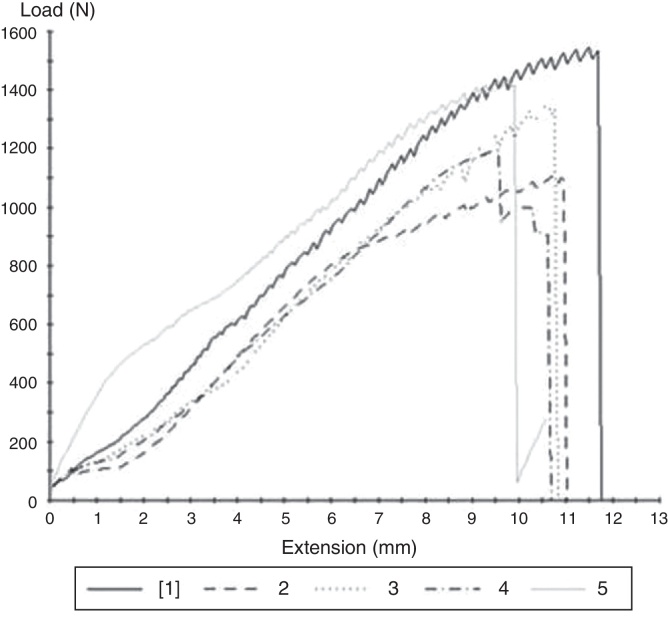
Control group
The maximum load values in Newtons in the five samples of the control group were, respectively, 1544, 1110, 1359, 1194 and 1437. The mean value was 1329 N and the standard deviation was 177 N (Table 2, Fig. 8).
Table 2.
Maximum load values in N in the control group.
| Sample | Maximum load (N) |
|---|---|
| 1 | 1544 |
| 2 | 1110 |
| 3 | 1359 |
| 4 | 1194 |
| 5 | 1437 |
| Mean | 1329 |
| Standard deviation | 177 |
Fig. 8.
Force vs. displacement curve for the control group.
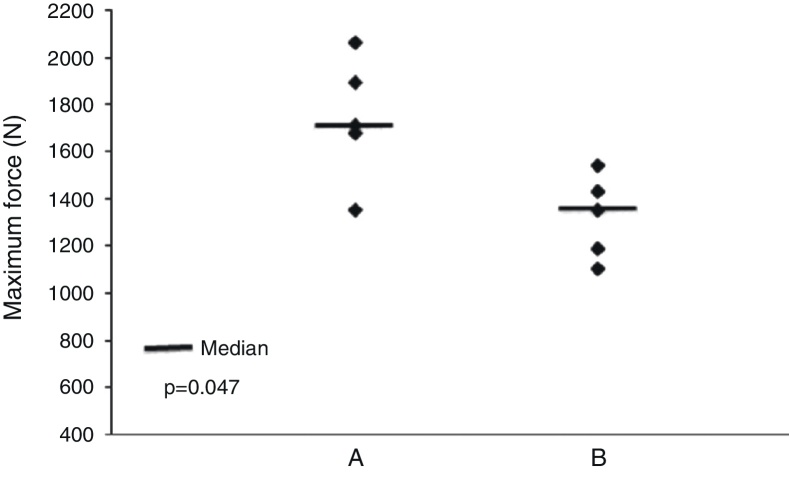
According to the Mann–Whitney test, it was observed that the test group presented a maximum force at 10 mm of displacement that was significantly greater than that of the control group (p = 0.047), as shown in Fig. 9.
Fig. 9.
Comparison between the test group (A) and the control group (B).
Discussion
The ideal surgical fixation for femoral neck fractures should be capable of resisting weight-bearing forces and restricting movement throughout the fracture site during the bone healing process, so as to allow rapid and secure recovery for the patient and a return to activities of daily living. Secure fixation also reduces the high rates of complications relating to treatments for this type of fracture.7
During daily activities, the load on the femoral head alternates anteriorly and posteriorly and causes varus forces. In the presence of fractures this load causes vertical shearing. The force applied to the head of the femoral neck depends on the patient's weight and on the activity carried out. These parameters are fundamental for evaluating the resistance of the implant in cases of femoral neck fracture. In our study, we used an axial force of 1400 N as the force applied to the hip of an individual weighing 70 kg who is standing on one leg.8 The values obtained in these tests using the DHS and antirotational screws, with 5 mm of displacement, reached a mean load of 1336 N and a mean rotational displacement of 2.42°. However, this osteosynthesis withstood a mean maximum load of 1742 N before failure, with 10 mm of displacement. This value was significantly higher (p = 0.047) than the load withstood by an intact synthetic femur (control group), which withstood a mean of 1329 N.
Stiasny et al. conducted a study that compared the surgical results from 112 patients who were treated using MCS, DHS or DHS plus antirotational screws. They concluded that comparable results could be obtained through using MCS or DHS for surgical treatment of stable fractures of the femoral neck (Garden types 1 and 2). In cases of unstable fractures of the femoral neck (Garden types 3 and 4), good results from the treatment depend on good reduction and stabilization of the fracture, which can be achieved through using the DHS. In these patients, with fractures of Garden types 3 and 4, the likelihood of obtaining good results through using the DHS was three times greater than in those who underwent fixation using MCS. In the evaluation on the use of antirotational screws, it was concluded that their use in addition to the DHS prolonged the duration of the surgery, increased the blood loss and did not improve the biomechanics of the femoral neck fixation.9
In a study on cadaver bones, Blair et al. compared the resistance of basicervical fracture fixation using MCS, DHS or DHS plus antirotational screws and reached mean values for resistance to axial loading of 1736 ± 494 N for MCS, 2880 ± 679 N for DHS and 2903 ± 598 N for DHS plus antirotational screws. They concluded that the DHS was biomechanically superior to MCS for treating femoral neck fractures at the base of the neck. Moreover, they observed that although a spongy screw located superiorly would be able to control rotation during the insertion of the sliding screw of the hip, it would not provide additional fixation after placement of this sliding screw.10
Biomechanical tests on implants perform a vital role in evaluating any new implant technology.11 It is difficult and may be extremely expensive to obtain fresh cadaveric bone that is free from diseases, for use in mechanical tests on orthopedic implants.12 Another problem is that cadaver samples are not uniform, which results in inclusion of samples with bone quality and strength that is very variable.13, 14 Differences in age and degree of osteoporosis among specimens from cadavers may also partially influence the variability of the mechanical properties.15, 16 This variability in geometric and material properties of cadaver specimens frequently requires prohibitively large sample sizes, in order to detect statistically significant differences in implant performance.17
We recognize the limitations of our study. Use of synthetic bones instead of bones from cadavers does not correctly translate the anatomy of the femoral trabeculae and the forces that they can withstand. We did not simulate all the physiological components of the force (cyclical, torsional and axial) to which the hip is subjected during the processes of walking or muscle contraction alone. Directional force vectors may have resulted in changes to the load values and consequently changes to the stabilization of the implant. An axial load in a single direction does not simulate the complex load system that is applied to the hip while walking, given that the torsional forces and the orientation of the vectors change during hip movements. However, the insufficiencies of the present study probably give rise to quantitative differences (i.e. regarding the level of force applied), rather than qualitative differences.
Synthetic bones were chosen to ensure comparable biomechanical properties between the groups and eliminate certain variables.13 Thus, we removed possible variations inherent to human bones that would cause difficulty in evaluating the methodology of fixation because of their non-uniform characteristics (bone density, diameter and length).
We believe that the principle of osteosynthesis for treating femoral neck fractures requires methodology that provides absolute stability and that it is improved when performed in a minimally invasive manner. Although the DHS does not include the principle of absolute stability, with or without antirotational screws, it presents surprisingly favorable results.9, 10 This may contribute towards a less pessimistic prognosis in treating unstable fractures of the femoral neck.
We suggest that new studies should be conducted. These could make use of the present results to develop new implants that would respect the need for absolute stability and could be implemented in a minimally invasive manner.
Conclusion
The analysis showed that the mechanical resistance of the test group was significantly greater than that of the control group and established the possibility that the DHS and antirotational screws can be used for osteosynthesis of femoral neck fractures, especially those of Pauwels type III.
Conflicts of interest
The authors declare no conflicts of interest.
Acknowledgement
To Prof. Ana Patrícia Paula, supervisor of the master's program of the Foundation for Teaching and Research in Health Sciences (FEPECS), for her unconditional assistance.
Footnotes
Please cite this article as: Freitas A, Torres GM, Souza ACAM, Maciel RA, Souto DRM, Ferreira GNB. Análise da resistência mecânica de fixação de fratura do colo femoral em osso sintético com DHS e parafuso antirrotatório. Rev Bras Ortop. 2014;49:586–592.
Work developed at the Orthopedic Hospital for Specialized Medicine, Brasília, Federal District, Brazil, and at the Mechanical Test Laboratory, Department of Materials Engineering, School of Mechanical Engineering, State University of Campinas (UNICAMP), Campinas, SP, Brazil.
References
- 1.Keating J. Fractures of the neck of femur. In: Bucholz R.W., Heckman J.D., Court-Brown C.M., editors. Rockwood and Green's fractures in adults. 7th ed. Lippincott Williams & Wilkins; Philadelphia: 2010. pp. 1561–1587. [Google Scholar]
- 2.Cooper C., Campion G., Melton L.J., 3rd. Hip fractures in the elderly: a world-wide projection. Osteoporos Int. 1992;2(6):285–289. doi: 10.1007/BF01623184. [DOI] [PubMed] [Google Scholar]
- 3.Singer B.R., McLauchlan G.J., Robinson C.M., Christie J. Epidemiology of fractures in 15,000 adults: the influence of age and gender. J Bone Joint Surg Br. 1998;80(2):243–248. doi: 10.1302/0301-620x.80b2.7762. [DOI] [PubMed] [Google Scholar]
- 4.Cummings S.R., Nevitt M.C., Browner W.S., Stone K., Fox K.M., Ensrud K.E. Risk factors for hip fracture in white women. Study of Osteoporotic Fractures Research Group. N Engl J Med. 1995;332(12):767–773. doi: 10.1056/NEJM199503233321202. [DOI] [PubMed] [Google Scholar]
- 5.Yih-Shiunn L., Chien-Rae H., Wen-Yun L. Surgical treatment of undisplaced femoral neck fractures in the elderly. Int Orthop. 2007;31(5):677–682. doi: 10.1007/s00264-006-0243-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sendtner E., Renkawitz T., Kramny P., Wenzl M., Grifka J. Fractured neck of femur – internal fixation versus arthroplasty. Dtsch Arztebl Int. 2010;107(23):401–407. doi: 10.3238/arztebl.2010.0401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kaplan T., Akesen B., Demirağ B., Bilgen S., Durak K. Comparative results of percutaneous cannulated screws, dynamic compression type plate and screw for the treatment of femoral neck fractures. Ulus Travma Acil Cerrahi Derg. 2012;18(1):65–70. doi: 10.5505/tjtes.2011.33427. [DOI] [PubMed] [Google Scholar]
- 8.Denham R.A. Hip mechanics. J Bone Joint Surg Br. 1959;41B:550–557. doi: 10.1302/0301-620X.41B3.550. [DOI] [PubMed] [Google Scholar]
- 9.Stiasny J., Dragan S., Kulej M., Martynkiewicz J., Płochowski J., Dragan S.Ł. Comparison analysis of the operative treatment results of the femoral neck fractures using side-plate and compression screw and cannulated AO screws. Ortop Traumatol Rehabil. 2008;10(4):350–361. [PubMed] [Google Scholar]
- 10.Blair B., Koval K.J., Kummer F., Zuckerman J.D. Basicervical fractures of the proximal femur. A biomechanical study of 3 internal fixation techniques. Clin Orthop Relat Res. 1994;(306):256–263. [PubMed] [Google Scholar]
- 11.Choueka J., Koval K.J., Kummer F.J., Crawford G., Zuckerman J.D. Biomechanical comparison of the sliding hip screw and the dome plunger effects of material and fixation design. J Bone Joint Surg Br. 1995;77(2):277–283. [PubMed] [Google Scholar]
- 12.Szivek J.A. Synthetic materials and structures used as models for bone. In: An Y.H., Draughn R.A., editors. Mechanical testing of bone and the bone-implant interface. CRC Press; Boca Raton: 1999. pp. 159–175. [Google Scholar]
- 13.Cristofolini L., Viceconti M., Cappello A., Toni A. Mechanical validation of whole bone composite femur models. J Biomech. 1996;29(4):525–535. doi: 10.1016/0021-9290(95)00084-4. [DOI] [PubMed] [Google Scholar]
- 14.Marti A., Fankhauser C., Frenk A., Cordey J., Gasser B. Biomechanical evaluation of the less invasive stabilization system for the internal fixation of distal femur fractures. J Orthop Trauma. 2001;15(7):482–487. doi: 10.1097/00005131-200109000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Heiner A.D., Brown T.D. Structural properties of a new design of composite replicate femurs and tibias. J Biomech. 2001;34(6):773–781. doi: 10.1016/s0021-9290(01)00015-x. [DOI] [PubMed] [Google Scholar]
- 16.Bolliger Neto R., Rossi J.D., Leivas T.P. Experimental determination of bone cortex holding power of orthopedic screw. Rev Hosp Clin Fac Med Sao Paulo. 1999;54(6):181–186. doi: 10.1590/s0041-87811999000600003. [DOI] [PubMed] [Google Scholar]
- 17.O’Neill F., Condon F., McGloughlin T., Lenehan B., Coffey C., Walsh M. Validity of synthetic bone as a substitute for osteoporotic cadaveric femoral heads in mechanical testing: a biomechanical study. Bone Joint Res. 2012;1(4):50–55. doi: 10.1302/2046-3758.14.2000044. [DOI] [PMC free article] [PubMed] [Google Scholar]