Abstract
Objective
To compare the results from two of the most commonly used surgical techniques: in situ decompression and subcutaneous transposition. The processes of patients treated surgically in a public university hospital between January 2004 and December 2011 were reviewed. Cases of proximal compression of the nerve, angular deformity of the elbow and systemic diseases associated with non-compressive neuropathy were excluded.
Methods
Ninety-seven cases were included (96 patients). According to the modified McGowan score, 14.4% of the patients presented grade Ia, 27.8% grade II, 26.8% grade IIb and 30.9% grade III. In situ neurolysis of the cubital was performed in 64 cases and subcutaneous anterior transposition in 33.
Results
According to the modified Wilson and Knout score, the results were excellent in 49.5%, good in 18.6%, only satisfactory in 17.5% and poor in 14.4%. In comparing the two techniques, we observed similar numbers of excellent and good results. Grades IIb and III were associated with more results that were less satisfactory or poor, independent of the surgical technique.
Conclusion
Both techniques were shown to be efficient and safe for treating cubital tunnel syndrome.
Keywords: Ulnar nerve, Elbow, Pain, Paresthesia, Ulnar tunnel syndrome
Resumo
Objetivo
Comparar os resultados de duas das técnicas cirúrgicas mais usadas, a descompressão in situ e a transposição subcutânea. Foram revistos os processos dos doentes tratados cirurgicamente num hospital universitário público entre janeiro de 2004 e dezembro de 2011. Foram excluídas compressões proximais do nervo, deformidades angulares do cotovelo e doenças sistêmicas associadas a neuropatia não compressiva.
Metodos
Foram incluídos 97 casos (96 doentes). Segundo o escore modificado de McGowan, 14,4% dos pacientes encontravam-se no Grau Ia, 27,8% no II, 26,8% no IIb e 30,9% no III. A neurólise in situ do cubital foi feita em 64 casos e a transposição anterior subcutânea em 33.
Resultados
Segundo o escore modificado de Wilson e Knout, os resultados foram excelentes em 49,5%, bons em 18,6%, apenas satisfatórios em 17,5% e pobres em 14,4%. Na comparação das duas técnicas observamos valores similares de resultados excelentes ou bons. Os graus IIb e III estão associados a mais resultados menos satisfatórios ou maus independentemente da técnica cirúrgica.
Conclusão
As duas técnicas se revelam eficientes e seguras no tratamento do síndrome do túnel cubital.
Palavras-chave: Nervo ulnar, Cotovelo, Dor, Parestesia, Síndrome do túnel ulnar
Introduction
After observing that the cubital nerve was compressed at the elbow, in a fibro-osseous space defined by a ligament between the medial epicondyle and the olecranon, Feindel and Stratford1 used the term “cubital tunnel syndrome” for the first time. One year earlier, Osborne2 had described simple decompression of the nerve by means of sectioning this same ligament. However, the first published papers date from 1878, the year in which Panas3 described the condition and Marchand4 described a procedure for releasing and stretching the cubital nerve. The condition of “toxic neuritis of the cubital nerve” was also described by Buzzard5 in 1922 and, two decades later, Learmonth6 also described techniques for submuscular and intramuscular decompression and transposition.
Compression of the cubital nerve is a common condition and may occur at several levels. Compression at the elbow is the commonest form of cubital compression7, 8, 9 and is the second commonest compression neuropathy of the upper limbs.
The diagnosis is based on symptoms, signs, orthopedic tests and electrophysiological studies.
Many cases of cubital tunnel syndrome can be treated conservatively without surgery. Nevertheless, some cases require surgical treatment with a view to avoiding persistence of the symptoms and progression of the neurological deterioration. The surgical treatment should be guided by the following principles: (1) release of all the possible compression sites; (2) preservation of the vascularization of the cubital nerve at the elbow; and (3) early mobilization of the elbow.
The commonest surgical options include simple decompression, medial epicondylectomy, subcutaneous anterior transposition, intramuscular anterior transposition and submuscular anterior transposition.
The elbow is a dynamic joint. Over the course of the day, it flexes and extends to place the hand in functional positions. Through this mobility, changes to the shape and space of the cubital tunnel take place. When the elbow is flexed, the tunnel becomes flatter10 and the arcuate ligament becomes tensioned,11 which leads to reduction of the space available for the nerve11, 12 and increased pressure inside the tunnel.13
Feindel and Stratford1 and Osborne2 advocated that sectioning the fibrotic band that forms the ceiling of this tunnel would be sufficient for relieving the pressure and consequently relieving the symptoms in the majority of the cases.
Under natural conditions, the nerve is also subject to traction and excursion during the normal movement of the elbow.
Anterior transposition has the aim of transferring the nerve to a point anterior to the axis of mobilization of the elbow. This diminishes the tension and also eliminates the pressure on the cubital tunnel.
There is no consensus in the literature regarding the best surgical treatment for cubital tunnel syndrome. Anterior transposition is perhaps the procedure most often effected.14 Nonetheless, other authors have defended the notion that simple decompression is just as effective as transposition and presents a similar success rate and lower complication rate.15, 16, 17
The present study had the aim of expanding the information available on comparisons of results between two techniques that are widely used for treating cubital tunnel syndrome: in situ decompression and subcutaneous anterior transposition.
Material and methods
The records of all patients who were treated surgically at our institution between January 2004 and December 2011 were reviewed. The inclusion criterion was taken to be a diagnosis of idiopathic cubital tunnel syndrome based on physical examination and electromyographic analysis. Cases of proximal compression of the nerve, angular deformities of the elbow and systemic diseases associated with non-compressive neuropathy were excluded.
In this manner, 97 cases were obtained, corresponding to 96 patients (56 men and 40 women), with a mean age of 51.91 years (range: 15–84). The right side was involved in 51 patients and the left side in 46 (Table 1).
Table 1.
Demographic characteristics of the patients included in the study.
| Total | Neurolysis | Transposition | p | |
|---|---|---|---|---|
| No. of patients (n) | 97 | 64 | 33 | |
| Sex (n) | ||||
| Male | 56 (58.3%) | 38 (60.3%) | 18 (54.5%) | 0.373 |
| Female | 40 (41.7%) | 25 (39.7%) | 15 (45.5%) | |
| Mean age (SD) | 51.9 (14.9) | 51.2 (14.7) | 53.3 (15.6) | 0.535 |
| Follow-up (months) | 10.3 (4–33) | 9.3 (4–29) | 11.7 (6–33) | |
| Reinterventions | 2 | 2 | 0 | |
| Side | 50 R; 47 L | 28 R; 37 L | 22 R; 10 L | |
All the patients were classified on a scale of four grades, in accordance with the modified McGowan classification system.18 Thus, patients with subjective symptoms and without objective findings were classified as grade I; those with good intrinsic strength without atrophy of the intrinsic muscles were classified as IIA; those presenting atrophy of the intrinsic muscles were classified as IIB; and those with marked sensory disturbance in association with marked atrophy of the intrinsic muscles were classified as III.
Thus, 14.4% (14) of the patients were in grade I, 27 (27.8%) in IIa, 26 (26.8%) in IIb and 30 (30.9%) in III (Table 2).
Table 2.
Characterization of the sample in absolute and relative frequencies.
| n | % | |
|---|---|---|
| Type of surgery | ||
| Neurolysis | 64 | 66.0 |
| Transposition | 33 | 34.0 |
| Total | 97 | 100.0 |
| Sex | ||
| Male | 56 | 58.3 |
| Female | 40 | 41.7 |
| Total | 96 | 100 |
| Postoperative result | ||
| Excellent | 48 | 49.5 |
| Good | 18 | 18.6 |
| Satisfactory | 17 | 17.5 |
| Poor | 14 | 14.4 |
| Total | 97 | 100.0 |
| Preoperative grade | ||
| I | 14 | 14.4 |
| IIA | 27 | 27.8 |
| IIB | 26 | 26.8 |
| III | 30 | 30.9 |
| Total | 97 | 100.0 |
|
Mean (min–max) |
SD | |
| Age | 51.91 (15–84) | 14.9 |
In situ neurolysis of the cubital nerve was performed in 64 cases, while subcutaneous anterior transposition was performed in 33 cases. Among the patients who underwent neurolysis, 12.5% were in grade I, 29.7% in IIA, 28.1% in IIB and 29.7% in III. Among those who underwent anterior transposition, 18.2% were in grade I, 24.2% in IIA, 24.2% in IIB and the remaining 33.3% in III (Table 3). No statistically significant differences in the patients’ preoperative stage according to surgery group were observed (p = 0.817).
Table 3.
Comparison of preoperative grade among the patients according to surgery group (neurolysis or transposition).
| Preoperative grade based on the modified McGowan score | |||||
|---|---|---|---|---|---|
| Grade I | Neurolysis |
Transposition |
p | ||
| Preoperative grade | n | % | n | % | |
| I | 8 | 12.5 | 6 | 18.2 | 0.817 |
| IIA | 19 | 29.7 | 8 | 24.2 | |
| IIB | 18 | 28.1 | 8 | 24.2 | |
| III | 19 | 29.7 | 11 | 33.3 | |
| Total | 64 | 33 | |||
The postoperative evaluation was stratified in accordance with the system of Wilson and Knout,19 in which an excellent result corresponded to minimal sensory and motor alterations, without tension at the incision site; good signified moderate sensory and motor alterations; satisfactory signified improved, but with persistent alterations; and poor signified no improvement or even worsening of the state.
In the descriptive analysis, the continuous variables were represented by the mean and standard deviation. The categorical variables were represented by the absolute frequency (n) and the relative frequency (%). With the aim of selecting appropriate statistical tests, the Kolmogorov–Smirnov test was used to ascertain whether the study variables followed normal distribution. To compare means, Student's t test for independent samples was used. The chi-square test or Fisher's exact test (when applicable) were used to analyze associations between pairs of categorical variables.
The four grades of the modified McGowan scale were regrouped into two levels: grade I with IIA; and grade IIB with III. The postoperative evaluation using the Wilson and Knout system was reclassified into two groups: excellent and satisfactory, good and poor. The statistical tests were conducted bilaterally with a significance level of 5%. The statistical analysis on the data was performed using the IBM SPSS Statistics 20.0 software.
Results
From the modified Wilson and Knout classification, out of the 97 operations performed, 48 (49.5%) produced an excellent result, 18 (18.6%) good, 17 (17.5%) satisfactory and 14 (14.4%) poor. A new surgical intervention was only necessary in relation to two patients (Table 1).
No differences relating to sex were observed with regard to the surgical technique. The mean age was 52 (14.9) years. The patients who underwent transposition surgery were two years older than those who underwent neurolysis (53.3 versus 51.2).
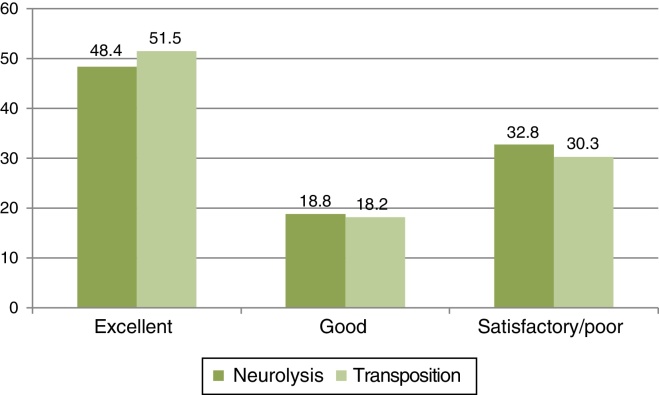
Comparison between the results from the two surgical techniques showed that there were no statistically significant differences, with similar values for the rates of excellent results (48.4% for neurolysis versus 51.5% for anterior transposition) and good results (18.8% versus 18.28%). Regarding the results that were only satisfactory or poor, the rates were 32.8% for neurolysis and 30.3% for subcutaneous transposition (Table 4).
Table 4.
Comparison of the postoperative results according to the surgical technique used.
| Modified Wilson and Knout score | |||||
|---|---|---|---|---|---|
| Result | Neurolysis |
Transposition |
p | ||
| n | % | n | % | ||
| Excellent | 31 | 48.4 | 17 | 51.5 | 0.957 |
| Good | 12 | 18.8 | 6 | 18.2 | |
| Satisfactory/poor | 21 | 32.8 | 10 | 30.3 | |
| Total | 64 | 33 | |||
In the analysis stratified according to the initial grade for the two techniques (Table 5, Table 6), it was seen that 41 patients were in grades I and IIa, of whom 27 underwent neurolysis and 14, transposition. Among the patients who underwent neurolysis, 55.6% achieved an excellent result and 44.4% a good, satisfactory or poor result. An excellent result was also achieved by 64.3% of the 14 patients who underwent transposition. Among the patients initially classified in grades IIB or III, 37 underwent neurolysis and 19 transposition, and excellent results were attained by 43.2% and 42.1%, respectively, while the results were good, satisfactory or poor in 56.8% and 57.9%, respectively.
Table 5.
Comparison of the postoperative results according to preoperative grade for the surgical technique of neurolysis.
| Result | Preoperative grade |
p | |||
|---|---|---|---|---|---|
| I/IIA |
IIB/III |
||||
| n | % | n | % | ||
| Excellent | 15 | 55.6 | 16 | 43.2 | 0.559 |
| Good + satisfactory + poor | 12 | 44.4 | 21 | 56.8 | |
| Total | 27 | 37 | |||
Table 6.
Comparison of the postoperative results according to preoperative grade for the surgical technique of transposition.
| Result | Preoperative grade |
p | |||
|---|---|---|---|---|---|
| I/IIA |
IIB/III |
||||
| n | % | n | % | ||
| Excellent | 9 | 64.3 | 8 | 42.1 | 0.208 |
| Good + satisfactory + poor | 5 | 35.7 | 11 | 57.9 | |
| Total | 14 | 19 | |||
Only two patients had the need for further surgical intervention. Both of these had undergone simple decompression (Table 2).
Discussion
Several surgical techniques have been put forward for treating compression of the cubital nerve in the elbow. Medial epicondylectomy is rarely performed.20, 21 Subcutaneous anterior transposition and simple decompression are the procedures most used. In our study, only patients who underwent operations using these two techniques were included, given that by a large majority, these are the techniques most performed in our department.
In analyzing the results, it seems that there was no preponderance of one technique over the other. Independent of the technique, the rate of excellent results among the patients reached 48.5%. When compared according to technique, the rates of excellent results were close: 48.4% for neurolysis and 51.5% for transposition. Satisfactory or poor results were obtained by 32.8% and 30.3%, respectively, which reinforced the similarity (Fig. 1). This analysis also showed that there was a tendency for patients with higher grades at the time of the surgery (IIB and III) to have lower rates of excellent results (43.2% and 42.1%), although no statistically significant different was observed in this regard (neurolysis p = 0.957; and transposition p = 0.559). This tendency was shown to be independent of the technique and confirms what has been widely disseminated in the literature, i.e. that the chances of alleviating the pain and recovering sensitivity and motor strength are inversely related to the initial grade of neuropathy.
Fig. 1.
Postoperative results according to the surgical technique used, expressed as relative frequencies (%).
The notable study on cadavers by Gelberman et al.22 demonstrated that intraneural pressure increases more than does extraneural pressure when flexion is greater than 90°. Gelberman therefore concluded that traction contributes toward nerve compression and took the view that the increase in intraneural pressure could not be due solely to extraneural compression. Despite this work, controversy continues to surround the evidence for nerve distress due to traction, rather than distress due to compression.9, 11, 22, 23, 24, 25, 26, 27 Cubital tunnel syndrome is not the only case of compressive neuropathy in the upper limb. In most other neuropathies, a compressive factor seems to be implicated. It is also known that nerves are capable of stretching and growing at a velocity of 1 mm/day. This raises the question of what might explain why the normal functioning of the elbow would require greater excursion of the nerve and why the organism is incapable of responding to and accommodating this need? Iba et al.28 brought up the issue of the clinical validity of the pressure values found by Gelberman et al.22 when they found in vivo intraneural pressure values that were high all the time, even in extension, and which were around four times higher in flexion.
More recent studies,29 also conducted on cadavers, have demonstrated that elongation of the nerve occurs especially in the segment proximal to the epicondyle and between 30° and 90° and then the length remains constant until 135°. However, at around 135°, the area and sagittal curvature of the tunnel decrease and force the nerve into a flattened shape. These findings suggest that the compression is greatest at 135°.
Based on the findings of Gelberman et al.,22 many orthopedists abandoned the surgical technique initially described by Osborne and started to perform anterior transpositions. However, over the last few years, several studies have demonstrated not only that simple decompression may be just as effective as anterior transposition, but also that the latter may be associated with a greater number of complications. One of the factors may be the possibility that blood vascularization might be disturbed during the transposition.30, 31, 32 Ogata et al.33 demonstrated in an experimental study that this transposition is associated with decreased regional blood flow for at least three days after the surgery. In a randomized prospective study on 44 patients, Biggs and Curtis16 concluded that there were no differences in the results between simple neurolysis and anterior transposition and recommended the former because of the lower number of complications. In another randomized prospective study on 152 patients, Bartels et al.15 compared subcutaneous anterior transposition and simple decompression and also concluded that simple decompression had equal efficacy but with a lower complication rate (23 versus 7, among a total of 30), which would also be associated with lower cost. In another randomized study on 70 patients and 48 months of follow-ups, Gervasio et al.17 also did not find any statistically significant differences between simple decompression and submuscular transposition. In a fourth prospective study with a follow-up of 63.1 months, Keiner et al.34 concluded that the two techniques led to similar results and that simple decompression should be preferred because it was less invasive. Nabhan et al.35 also prospectively compared simple decompression and subcutaneous anterior transposition and reported that there were no differences in the results and therefore also recommended simple decompression as the preferred treatment because it is a simpler procedure. Furthermore, two meta-analyses conducted by Macadam et al.36 and Zlowodzki et al.37 did not find any statistically significant differences between the various techniques.
Our study seems to be concordant with most of the recently published papers on surgical treatment of this pathological condition. Despite the need for reintervention in the cases of two patients who were initially treated by means of simple decompression, most of the patients treated using this technique achieved the same result as those who underwent subcutaneous transposition, independent of the initial grade. The absence of complications in our study, in comparison with the others cited, can be explained by the fact that in some of these other studies, anterior transposition that sometimes was intra or submuscular was used as the comparison. This is generally associated with a higher complication rate.
From the analysis on the literature, it also seems that medial epicondylectomy has an increasingly limited role. Muermans et al.38 analyzed their results from 60 epicondylectomy procedures performed on 51 patients and found excellent results in 75% of them. However, 21 of these 51 patients reported pain in the medial epicondyle after the operation. This was similar to the result obtained by Efstathopoulos et al.,39 in which 45% of the patients operated continued to present pain six months afterwards.
Conclusion
This study was limited by its retrospective nature and by the small number of patients in some of the subgroups analyzed. The postoperative results did not present any correlation with the surgical technique used, given that independent of the technique, most of the patients achieved an excellent result. This reinforces the idea that simple decompression enables results similar to those from subcutaneous anterior transposition. Therefore, with due regard for the greater technical simplicity of simple decompression, we would reserve transposition only for cases of nerves with a potential for subluxation, post-traumatic stiffness, valgus instability, late paralysis of the cubital nerve or failure of simple decompression.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Please cite this article as: Sousa M, Aido R, Trigueiros M, Lemos R, Silva C. Neuropatia compressiva cubital no cotovelo: neurólise in situ versus transposição anterior–Estudo comparativo. Rev Bras Ortop. 2014;49:647–652.
Work developed in the Department of Orthopedics and Traumatology, Porto Hospital Center, Porto, Portugal.
References
- 1.Feindel W., Stratford J. Cubital tunnel compression in tardy ulnar palsy. Can Med Assoc J. 1958;78(5):351–353. [PMC free article] [PubMed] [Google Scholar]
- 2.Osborne G.V. The surgical treatment of tardy ulnar neuropathy. J Bone Joint Surg Br. 1957;39:782. [Google Scholar]
- 3.Panas J. Sur une cause connue de paralysie due nerfcubital. Arch Gen Med. 1878;2:5–22. [Google Scholar]
- 4.Marchand A.H. Sur la distension chirurgicale des nerfs. Gazete Hebdomadaire de Médecine et de Chirurgie. 1878;25:209–212. [Google Scholar]
- 5.Buzzard E.F. Some varieties of traumatic and toxic ulnar neuritis. Lancet. 1922;1:317–319. [Google Scholar]
- 6.Learmonth J.R. A technique for transplanting the ulnar nerve. Surg Gynecol Obstet. 1942;75:792–793. [Google Scholar]
- 7.Dellon A.L. Review of treatment results for ulnar nerve entrapment at the elbow. J Hand Surg Am. 1989;14(4):688–700. doi: 10.1016/0363-5023(89)90192-5. [DOI] [PubMed] [Google Scholar]
- 8.Bednar M.S., Blair S.J., Light T.R. Complications of the treatment of cubital tunnel syndrome. Hand Clin. 1994;10(1):83–92. [PubMed] [Google Scholar]
- 9.Apfelberg D.B., Larson S.J. Dynamic anatomy of the ulnar nerve at the elbow. Plast Reconstr Surg. 1973;51(1):76–81. [PubMed] [Google Scholar]
- 10.Patel V.V., Heidenreich F.P., Jr., Bindra R.R., Yamaguchi K., Gelberman R.H. Morphologic changes in the ulnar nerve at the elbow with flexion and extension: a magnetic resonance imaging study with 3-dimensional reconstruction. J Shoulder Elbow Surg. 1998;7(4):368–374. doi: 10.1016/s1058-2746(98)90025-8. [DOI] [PubMed] [Google Scholar]
- 11.Vanderpool D.W., Chalmers J., Lamb D.W., Whiston T.B. Peripheral compression lesions of the ulnar nerve. J Bone Joint Surg Br. 1968;50(4):792–803. [PubMed] [Google Scholar]
- 12.Pechan J., Julius I. The pressure measurement in the ulnar nerve at the elbow. Plast Reconst Surg. 1973;51(1):79–81. [Google Scholar]
- 13.Werner C.O., Ohlin P., Elmqvist D. Pressures recorded in ulnar neuropathy. Acta Orthop Scand. 1985;56(5):404–406. doi: 10.3109/17453678508994358. [DOI] [PubMed] [Google Scholar]
- 14.Bartels R.H., Menovsky T., Van Overbeeke J.J., Verhagen W.I. Surgical management of ulner nerve compression at the elbow: an analysis of the literature. J Neurosurg. 1998;89(5):722–727. doi: 10.3171/jns.1998.89.5.0722. [DOI] [PubMed] [Google Scholar]
- 15.Bartels R.H., Verhagen W.I., van der Wilt G.J., Meulstee J., van Rossum L.G., Grotenhuis J.A. Prospective randomized controlled study comparing simple decompression versus anterior subcutaneous transposition for idiopathic neuropathy of the ulnar nerve at the elbow: Part 1. Neurosurgery. 2005;56(3):522–530. doi: 10.1227/01.neu.0000154131.01167.03. [DOI] [PubMed] [Google Scholar]
- 16.Biggs M., Curtis J.A. Randomized, prospective study comparing ulnar neurolysis in situ with submuscular transposition. Neurosurgery. 2006;58(2):296–304. doi: 10.1227/01.NEU.0000194847.04143.A1. [DOI] [PubMed] [Google Scholar]
- 17.Gervasio O., Gambardella G., Zaccone C., Branca D. Simple decompression versus anterior submuscular transposition of the ulnar nerve in severe cubital tunnel syndrome: a prospective randomized study. Neurosurgery. 2005;56(1):108–117. doi: 10.1227/01.neu.0000145854.38234.81. [DOI] [PubMed] [Google Scholar]
- 18.McGowan A.J. The results of transposition of the ulnar nerve for traumatic ulnar neuritis. J Bone Joint Surg Br. 1950;32(3):293–301. doi: 10.1302/0301-620X.32B3.293. [DOI] [PubMed] [Google Scholar]
- 19.Wilson D.H., Knout R. Surgery of ulnar neuropathy at the elbow: 16 cases treated by decompression without transposition. Technical note. J Neurosurg. 1973;38(6):780–785. doi: 10.3171/jns.1973.38.6.0780. [DOI] [PubMed] [Google Scholar]
- 20.Amako M., Nemoto K., Kawaguchi M., Kato N., Arino H., Fujikawa K. Comparison between partial and minimal medial epicondylectomy combined with decompression for the treatment of cubital tunnel syndrome. J Hand Surg Am. 2000;25(6):1043–1050. doi: 10.1053/jhsu.2000.17864. [DOI] [PubMed] [Google Scholar]
- 21.Froimson A.I., Anouchi Y.S., Seitz W.H., Jr., Winsberg D.D. Ulnar nerve decompression with medial epicondylectomy for neuropathy at the elbow. Clin Orthop Relat Res. 1991;(265):200–206. [PubMed] [Google Scholar]
- 22.Gelberman R.H., Yamaguchi K., Hollstien S.B., Winn S.S., Heidenreich F.P., Jr., Bindra R.R. Changes in interstitial pressure and cross sectional area of the cubital tunnel and of the ulnar nerve with flexion of the elbow: an experimental study in human cadavera. J Bone Joint Surg Am. 1998;80(4):492–501. doi: 10.2106/00004623-199804000-00005. [DOI] [PubMed] [Google Scholar]
- 23.Wadsworth T.G. The external compression syndrome of the ulnar nerve at the cubital tunnel. Clin Orthop Relat Res. 1977;(124):189–204. [PubMed] [Google Scholar]
- 24.Pechan J., Julis I. The pressure measurement in the ulnar nerve. A contribution to the pathophysiology of the cubital tunnel syndrome. J Biomech. 1975;8(1):75–79. doi: 10.1016/0021-9290(75)90045-7. [DOI] [PubMed] [Google Scholar]
- 25.Osborne G. Compression neuritis of the ulnar nerve at the elbow. Hand. 1970;2(1):10–13. doi: 10.1016/0072-968x(70)90027-6. [DOI] [PubMed] [Google Scholar]
- 26.Ferlic D.C. In situ decompression of the ulnar nerve at the elbow. In: Gelberman R.H., editor. Operative repair and reconstruction. JB Lippincott; Philadelphia: 1991. pp. 1063–1067. [Google Scholar]
- 27.Schuind F.A., Goldschmidt D., Bastin C., Burny F. A biomechanical study of the ulnar nerve at the elbow. J Hand Surg Br. 1995;20(6):623–627. doi: 10.1016/s0266-7681(05)80124-x. [DOI] [PubMed] [Google Scholar]
- 28.Iba K., Wada T., Aoki M., Tsuji H., Oda T., Yamashita T. Intraoperative measurement of pressure adjacent to the ulnar nerve in patients with cubital tunnel syndrome. J Hand Surg Am. 2006;31(4):553–558. doi: 10.1016/j.jhsa.2006.01.009. [DOI] [PubMed] [Google Scholar]
- 29.James J., Sutton L.G., Werner F.W., Basu N., Allison M.A., Palmer A.K. Morphology of the cubital tunnel: an anatomical and biomechanical study with implications for treatment of ulnar nerve compression. J Hand Surg Am. 2011;36(12):1988–1995. doi: 10.1016/j.jhsa.2011.09.014. [DOI] [PubMed] [Google Scholar]
- 30.Asami A., Morisawa K., Tsuruta T. Funcional outcome of anterior transposition of the vascularized ulnar nerve for cubital tunnel syndrome. J Hand Surg Br. 1998;23(5):613–616. doi: 10.1016/s0266-7681(98)80014-4. [DOI] [PubMed] [Google Scholar]
- 31.Barone C.M., Jimenez D.F., Frempog-Bodeau A. Blood flow measurements of injured peripheral nerves by laser Doppler flowmetry. J Reconstr Microsurg. 1992;8(4):319–323. doi: 10.1055/s-2007-1006715. [DOI] [PubMed] [Google Scholar]
- 32.Lim B.H., Tob C.L., Wong H.P., Pho R.W. Cadaveric study on the vascular anatomy of the ulnar nerve at the elbow – a basis for anterior transposition? Ann Acad Med Singapore. 1992;21(5):689–693. [PubMed] [Google Scholar]
- 33.Ogata K., Manske P.R., Lesker P.A. The effect of surgical dissection on regional blood flow to the ulnar nerve in the cubital tunnel. Clin Orthop Relat Res. 1985;(193):195–198. [PubMed] [Google Scholar]
- 34.Keiner D., Gaab M.R., Schroeder H.W., Oertel J. Comparison of the long-term results of anterior transposition of the ulnar nerve or simple decompression in the treatment of cubital tunnel syndrome – a prospective study. Acta Neurochir. 2009;151(4):311–315. doi: 10.1007/s00701-009-0218-4. [DOI] [PubMed] [Google Scholar]
- 35.Nabhan A., Ahlhelm F., Kelm J., Reith W., Schwerdtfeger K., Steudel W.I. Simple decompression or subcutaneous anterior transposition of the ulnar nerve for cubital tunnel syndrome. J Hand Surg Br. 2005;30(5):521–524. doi: 10.1016/j.jhsb.2005.05.011. [DOI] [PubMed] [Google Scholar]
- 36.Macadam S.A., Ghandi R., Bezuhly M., Lefaivre K.A. Simple decompression versus anterior subcutaneous and submuscular transposition of the ulnar nerve for cubital tunnel syndrome: a meta-analysis. J Hand Surg Am. 2008;33(8):1314.e1–1314.e12. doi: 10.1016/j.jhsa.2008.03.006. [DOI] [PubMed] [Google Scholar]
- 37.Zlowodzki M., Chan S., Bhandari M., Kalliainen L., Schubert W. Anterior transposition compared with simple decompression for treatment of cubital tunnel syndrome. A meta-analysis of randomized controlled trials. J Bone Joint Surg Am. 2007;89(12):2591–2598. doi: 10.2106/JBJS.G.00183. [DOI] [PubMed] [Google Scholar]
- 38.Muermans S., De Smet L. Partial medial epicondylectomy for cubital tunnel syndrome: outcome and complications. J Shoulder Elbow Surg. 2002;11(3):248–252. doi: 10.1067/mse.2002.123901. [DOI] [PubMed] [Google Scholar]
- 39.Efstathopoulos D.G., Themistocleous G.S., Papagelopoulos P.J., Chloros G.D., Gerostathopoulos N.E., Soucacos P.N. Outcome of partial medial epicondylectomy for cubital tunnel syndrome. Clin Orthop Relat Res. 2006;(444):134–139. doi: 10.1097/01.blo.0000201153.36948.29. [DOI] [PubMed] [Google Scholar]