Abstract
Objective
To study the anatomy of the posterior cruciate ligament (PCL) and define anatomical parameters with the knee flexed at 90°.
Methods
Eight knees from cadavers were dissected in order to make measurements from the center of the anterolateral band to the roof (AL1), from the center of the anterolateral band to the anterior cartilage (AL2), from the center of the posteromedial band to the roof (PM1), from the center of the posteromedial band to the anterior cartilage (PM2), from the center of the tibial insertion to the medial region of the tibia (TIM), from the center of the tibial insertion to the lateral region of the tibia (TIL), from the center of the medial insertion to the medial meniscus (IMM) and the width of the origin of the PCL (WO). To obtain the results from each anatomical structure, the means and standard deviations of the measurements were calculated.
Results
The measurements in millimeters that were found were AL1, 6.2; AL2, 4.9; PM1, 11.7; PM2, 5.5; TIM, 32.5; TIL, 40.6; IMM, 9.4; and WO, 32.5.
Conclusions
The PCL has an extensive origin. The center of the anterolateral band is 6 mm from the roof and 5 mm from the anterior cartilage of the knee. The tibial insertion is slightly medial and 10 mm distal to the posterior cornu of the medial meniscus.
Keywords: Posterior cruciate ligament, Anatomy, Cadaver
Resumo
Objetivo
Estudar a anatomia do ligamento cruzado posterior (LCP) e definir parâmetros anatômicos com o joelho em 90° de flexão.
Métodos
Oito joelhos de cadáveres foram dissecados para tirar as medidas do centro da banda anterolateral ao teto (AL1), do centro da banda anterolateral à cartilagem anterior (AL2), do centro da banda posteromedial ao teto (PM1), do centro da banda posteromedial à cartilagem anterior (PM2), do centro da inserção tibial à região medial da tíbia (ITM), do centro da inserção tibial à região lateral da tíbia (ITL), do centro da inserção medial ao menisco medial (IMM) e da largura da origem do LCP (LO). Para a obtenção dos resultados de cada estrutura anatômica foram calculados os valores de média e desvio padrão das medições.
Resultados
As medidas, em milímetros, encontradas foram AL1, 6,2; AL2, 4,9; PM1, 11,7; PM2, 5,5; ITM, 32,5; ITL, 40,6; IMM, 9,4; e LO, 32,5.
Conclusões
O LCP tem uma origem extensa. O centro da banda anterolateral fica a 6 mm do teto e a 5 mm da cartilagem anterior do joelho. A inserção tibial fica levemente medial e 10 mm distal ao corno posterior do menisco medial.
Palavras-chave: Ligamento cruzado posterior, Anatomia, Cadáver
Introduction
The posterior cruciate ligament (PCL) is one of the static stabilizers of the knee. It provides primary restraint in relation to posterior displacement of the tibia and secondary restraint in relation to varus, valgus and external rotation.1
Controversy continues regarding the treatment for PCL injuries.2 There is insufficient data in the literature to be able to standardize the indication.3 Some authors have recommended reconstruction of the PCL in patients with more than 10 mm of posterior displacement who present complaints of pain and instability and who do not improve with conservative treatment.2, 4 This recommendation is based on the fact that 75% of the results from PCL reconstruction are good.5
No technique presenting precision and reproducibility for guiding tunnel positioning in PCL reconstruction has yet been developed. This may be because most studies have been conducted with the knee in the anatomical position (extension), whereas the surgical procedure is performed with the knee flexed.6, 7, 8 The aim of this study was analyze the anatomy of the PCL and define objective anatomical parameters with the knee flexed at 90°.
Materials and methods
Eight knees from cadavers were dissected with the aim of studying the anatomy and making measurements on the structures and anatomical relationships of the PCL.
As an inclusion criterion, we selected knees from cadavers with intact knee structures, including the joint capsule, without any previous arthrotomy. All the knees had been conserved in formol.
To make measurements, 40 × 12 needles were used to mark out specific points and then an Aero Space® metal pachymeter (150 mm) was used.
The following measurements were made:
-
•
center of the anterolateral band to the roof (Fig. 1);
-
•
center of the anterolateral band to the anterior cartilage (Fig. 1);
-
•
center of the posteromedial band to the roof (Fig. 1);
-
•
center of the posteromedial band to the anterior cartilage (Fig. 1);
-
•
center of the tibial insertion to the medial region of the tibia (Fig. 2);
-
•
center of the tibial insertion to the lateral region of the tibia (Fig. 2);
-
•
center of the medial insertion to the medial meniscus (Fig. 2);
-
•
width of the origin of the PCL (Fig. 3).
Fig. 1.
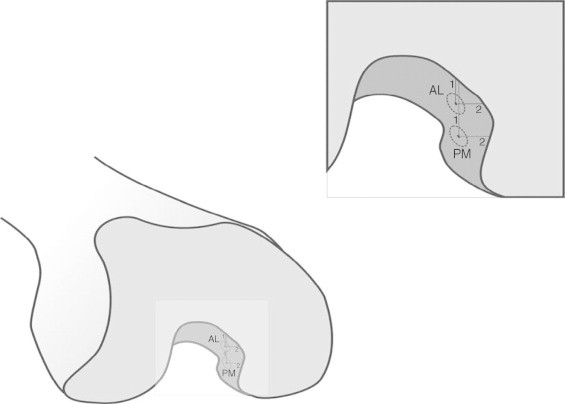
Measurements from the femoral origin of the posterior cruciate ligament. AL1: center of the anterolateral band to the roof; AL2: center of the anterolateral band to the anterior cartilage; PM1: center of the posteromedial band to the roof; PM2: center of the posteromedial band to the anterior cartilage.
Fig. 2.
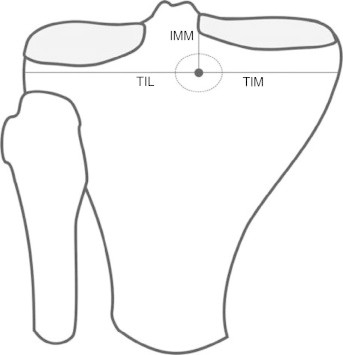
Measurements from the femoral origin of the posterior cruciate ligament. TIL: center of the tibial insertion to the lateral region of the tibia; TIM: center of the tibial insertion to the medial region of the tibia; IMM: center of the medial insertion to the medial meniscus.
Fig. 3.

Measurement of the width of the origin of the posterior cruciate ligament, using colored string.
One of the measurements was the width of the origin of the PCL. This was measured with the aid of a colored string, which was laid along the entire length of the ligament (Fig. 3).
Results
The means and standard deviations (SD) resulting from the measurements on the PCL at the femoral origin and tibial insertion are presented in Table 1, Table 2.
Table 1.
Means and standard deviations (SD) of the PCL measurements at the femoral origin.
| Values | WO | AL1 | AL2 | PM1 | PM2 |
|---|---|---|---|---|---|
| Mean | 28.6 | 6.2 | 4.9 | 11.7 | 5.5 |
| SD | 1.7 | 1.2 | 1.1 | 2 | 1.2 |
WO, width at origin; AL1, center of the anterolateral band to the roof; AL2, center of the anterolateral band to the anterior cartilage; PM1, center of the posteromedial band to the roof; PM2, center of the posteromedial band to the anterior cartilage.
Table 2.
Means and standard deviations (SD) of the PCL measurements at the tibial insertion.
| Values | TIM | TIL | IMM |
|---|---|---|---|
| Mean | 32.5 | 40.6 | 9.4 |
| SD | 3.5 | 4.4 | 2.3 |
TIM, center of the tibial insertion to the medial region of the tibia; TIL, center of the tibial insertion to the lateral region of the tibia; IMM, center of the medial insertion to the medial meniscus.
Discussion
Most studies have measured the cruciate ligaments in the anatomical position, i.e. with the knee extended. These measurements have been based on the sagittal view, with removal of the femoral condyle.8 In the present study, the anatomical measurements were made with the knee flexed at 90°, with the intention of increasing the applicability of the study to arthroscopic procedures.6 Even with similar measurements, the results may show discrepancies if obtained in different manners.7, 8
The PCL originates from a large area of the medial femoral condyle and is inserted in a depression between the tibial plateaus called the fossa of the PCL.1 It is slightly medial to the imaginary axis of knee rotation.9 The results from anatomical studies on the tibial insertion of the PCL corroborate this affirmation. Lorenz et al.10 found the center of the tibial insertion 45 mm from the lateral edge of the tibial plateau and 43 mm from the medial edge. The results from the present study demonstrated an even more medial position, with the center of the PCL in the tibia at 40.6 mm from the lateral edge and 32.5 mm from the medial edge.
Girgis et al.11 evaluated the length of the femoral origin of the PCL and arrived at a value of 32 mm. They made the measurement as a straight line between the two furthest extremities and neglected its oval format. In the present study, the measurement was made in a similar manner, but the half-circumference was evaluated and a value of 28.6 mm was obtained.
The great extent of the origin means that the fibers of the PCL behave differently according to the degree of knee flexion. Thus, there will always be some fibers under tension, independent of the position of the knee. This phenomenon was analyzed back in the 1970s, but in a description of the PCL as a single structure.11 Studies conducted more recently have separated the PCL into two bands: the anterolateral band remains tense during flexion and the posteromedial, during extension.12
The oval origin measuring 30 mm makes reproduction in surgical procedures difficult. One of the proposals for coming closer to the original anatomy has been to perform the reconstruction as a double band. Nonetheless, although double bands demonstrate greater in vitro stability, clinical studies have not demonstrated any advantages in comparison with single bands.8 Even some biomechanical studies have not found any difference between the two techniques, especially in clinical analyses.13
There were five studies in the literature, in which the methodology enabled comparisons with some of the results from the present study. The distance from the center of the anterolateral band to the roof was found to range from 13 to 4.8 mm. In the present study, this distance was 6.2. The distance from the posteromedial band to the roof ranged from 20 to 11.4 mm. In the present study, it was 11.7.8, 14, 15, 16 Differences of this type between studies are common, because they are absolute measurements and are influenced by the evaluator, the sample and the material used for collection.
Regarding the measurements from the center of the bands to the anterior cartilage, there was a discrepancy in relation to the data found in the literature. The distance from the anterolateral band to the anterior cartilage ranged from 13 to 7 mm. In the present study, this distance was 4.9. For the posteromedial band, the range was from 10.6 to 8 mm. The value found was 5.5.8, 14, 15, 16 One possibility for this difference, in addition to those put forward in the above paragraph, was undervaluation of Hamphey's ligament.
The arthroscopic reference points for determining the position of the PCL are a source of confusion in the literature. One of the methods used has been a clock-face method. However, studies have shown that there is imprecision in reproducing this technique. In some cases, differences of more than one hour were found in the evaluations between observers.17, 18
Another method used consists of a tabulated guide. This is useful for guiding the tunnels on lateral images. This method standardizes the individualization of the bands and their positions in relation to the size of the knee. This method should perhaps be the standard for navigated surgery, since it is mathematically more precise. On the other hand, for application to conventional arthroscopic surgery, it is very limited.18
Even with all these parameters, some decisions regarding the positioning of the tunnel during the surgery, in relation to both the joint face and the tunnel direction, are dependent on the surgeon's subjective choices and the particular features of the case operated.
Conclusions
The PCL has an extensive origin. The center of the anterolateral band is 6 mm from the roof and 5 mm from the anterior cartilage of the knee. The tibial insertion is slightly medial and 10 mm distal to the posterior cornu of the medial meniscus.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Please cite this article as: Cho DK, Rosa SP, Prestes GB, da Cunha LAM, de Moura MFA, Stieven Filho E. Estudo anatômico do ligamento cruzado posterior com o joelho em 90° de flexão. Rev Bras Ortop. 2014;49(5):494–8.
Work developed in the Biological Sciences Sector, Universidade Federal do Paraná (UFPR), Curitiba, PR, Brazil.
References
- 1.Fanelli G.C., Beck J.D., Edson C.J. Current concepts review: the posterior cruciate ligament. J Knee Surg. 2010;23(2):61–72. doi: 10.1055/s-0030-1267466. [DOI] [PubMed] [Google Scholar]
- 2.Montgomery S.R., Johnson J.S., McAllister D.R., Petrigliano F.A. Surgical management of PCL injuries: indications, techniques, and outcomes. Curr Rev Musculoskelet Med. 2013;6(2):115–123. doi: 10.1007/s12178-013-9162-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Peccin M.S., Almeida G.J.M., Amaro J., Cohen M., Soares B.G.O., Atallah A.N. Interventions for treating posterior cruciate ligament injuries of the knee in adults. Cochrane Database Syst Rev. 2005;18(2):CD002939. doi: 10.1002/14651858.CD002939.pub2. [DOI] [PubMed] [Google Scholar]
- 4.Camargo O.P.A., Chamecki A. Lesão do ligamento cruzado posterior: incidência e tratamento. Rev Bras Ortop. 1996;31(6):491–496. [Google Scholar]
- 5.Kim Y.M., Lee C.A., Matava M.J. Clinical results of arthroscopic single-bundle transtibial posterior cruciate ligament reconstruction: a systematic review. Am J Sports Med. 2011;39(2):425–434. doi: 10.1177/0363546510374452. [DOI] [PubMed] [Google Scholar]
- 6.Stieven-Filho E., Garschagen E.T., Namba M., Silva J.L.V., Malafaia O., Cunha L.A.M. Estudo anatômico das duas bandas do ligamento cruzado anterior com o joelho em 90o de flexão. Rev Col Bras Cir. 2011;38(5):338–342. [PubMed] [Google Scholar]
- 7.Johannsen A.M., Anderson C.J., Wijdicks C., Engebretsen L., LaPrade R.F. Radiographic landmarks for tunnel positioning in posterior cruciate ligament reconstructions. Am J Sports Med. 2013;41(1):35–42. doi: 10.1177/0363546512465072. [DOI] [PubMed] [Google Scholar]
- 8.Anderson C.J., Ziegler C.G., Wijdicks C.A., Engebretsen L., Laprade R.F. Arthroscopically pertinent anatomy of the anterolateral and posteromedial bundles of the posterior cruciate ligament. J Bone Joint Surg Am. 2012;94(21):1936–1945. doi: 10.2106/JBJS.K.01710. [DOI] [PubMed] [Google Scholar]
- 9.Cury R.P.L., Severino N.R., Camargo O.P.A., Aihara T., Batista Neto L.V., Goarayeb D.N. Estudo anatômico da inserção femoral do ligamento cruzado posterior. Rev Bras Ortop. 2011;46(5):591–595. doi: 10.1016/S2255-4971(15)30417-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lorenz S., Elser F., Brucker P.U., Obst T., Imhoff A.B. Radiological evaluation of the anterolateral and posteromedial bundle insertion sites of the posterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2009;17(6):683–690. doi: 10.1007/s00167-009-0770-8. [DOI] [PubMed] [Google Scholar]
- 11.Girgis F.G., Marshall J.L., Monajem A. The cruciate ligaments of the knee joint. Anatomical, functional and experimental analysis. Clin Orthop Relat Res. 1975;(106):216–231. doi: 10.1097/00003086-197501000-00033. [DOI] [PubMed] [Google Scholar]
- 12.Amis A.A., Gupte C.M., Bull M.J., Edwards A. Anatomy of the posterior cruciate ligament and the meniscofemoral ligaments. Knee Surg Sports Traumatol Arthrosc. 2006;14(3):257–263. doi: 10.1007/s00167-005-0686-x. [DOI] [PubMed] [Google Scholar]
- 13.Bergfeld J.A., Graham S.M., Parker R.D., Valdevit A.D.C., Kambic H.E. A biomechanical comparison of posterior cruciate ligament reconstructions using single- and double-bundle tibial inlay techniques. Am J Sports Med. 2005;33(7):976–981. doi: 10.1177/0363546504273046. [DOI] [PubMed] [Google Scholar]
- 14.Lopes O.V., Ferretti M., Shen W., Ekdahl M., Smolinski P., Fu F.H. Topography of the femoral attachment of the posterior cruciate ligament. J Bone Joint Surg Am. 2008;90(2):249–255. doi: 10.2106/JBJS.G.00448. [DOI] [PubMed] [Google Scholar]
- 15.Takahashi M., Matsubara T., Doi M., Suzuki D., Nagano A. Anatomical study of the femoral and tibial insertions of the anterolateral and posteromedial bundles of human posterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2006;14(11):1055–1059. doi: 10.1007/s00167-006-0192-9. [DOI] [PubMed] [Google Scholar]
- 16.Morgan C.D., Kalman V.R., Grawl D.M. The anatomic origin of the posterior cruciate ligament: where is it? Reference landmarks for PCL reconstruction. Arthroscopy. 1997;13(3):325–331. doi: 10.1016/s0749-8063(97)90029-3. [DOI] [PubMed] [Google Scholar]
- 17.Apsingi S., Bull A.M., Deehan D.J., Amis A.A. Review: femoral tunnel placement for PCL reconstruction in relation to the PCL fibre bundle attachments. Knee Surg Sports Traumatol Arthrosc. 2009;17(6):652–659. doi: 10.1007/s00167-009-0747-7. [DOI] [PubMed] [Google Scholar]
- 18.Edwards A., Bull A.M., Amis A.A. The attachments of the fiber bundles of the posterior cruciate ligament: an anatomic study. Arthroscopy. 2007;23(3):284–290. doi: 10.1016/j.arthro.2006.11.005. [DOI] [PubMed] [Google Scholar]


