Abstract
Objective
To describe the path of the infrapatellar branch of the saphenous nerve (IBSN) using the medial joint line, anterior tibial tuberosity (ATT), tibial collateral ligament and a horizontal line parallel to the medial joint line that passes over the ATT, as reference points, in order to help surgeons to diminish the likelihood of injuring this nerve branch during reconstruction of the anterior cruciate ligament (ACL) using flexor tendons.
Methods
Ten frozen knees that originated from amputations were examined. Through anatomical dissection performed with the specimens flexed, we sought to find the IBSN, from its most medial and proximal portion to its most lateral and distal portion. Following this, the anatomical specimens were photographed and, using the ImageJ software, we determined the distance from the IBSN to the medial joint line and to a lower horizontal line going through the ATT and parallel to the first line. We also measured the angle of the direction of the path of the nerve branch in relation to this lower line.
Results
The mean angle of the path of the nerve branch in relation to the lower horizontal line was 17.50 ± 6.17°. The mean distance from the IBSN to the medial joint line was 2.61 ± 0.59 cm and from the IBSN to the lower horizontal line, 1.44 ± 0.51 cm.
Conclusion
The IBSN was found in all the knees studied. In three knees, we found a second branch proximal to the first one. The direction of its path was always from proximal and medial to distal and lateral. The IBSN was always proximal and medial to the ATT and distal to the medial joint line. The medial angle between its direction and a horizontal line going through the ATT was 17.50 ± 6.17°.
Keywords: Knee, Anterior cruciate, Ligament/innervation, Anterior cruciate, Ligament/surgery
Resumo
Objetivo
Descrever o trajeto do ramo infrapatelar do nervo safeno (RIPNS) com o uso da linha articular medial, da tuberosidade anterior da tíbia (TAT), do ligamento colateral tibial e de uma linha horizontal, paralela à linha articular medial e que passa sobre a TAT, como pontos de referência, a fim de poder auxiliar os cirurgiões a diminuir a probabilidade de lesão desse ramo nervoso na reconstruc¸ão do ligamento cruzado anterior (LCA) com tendões flexores.
Métodos
Foram examinados 10 joelhos congelados, originados de amputac¸ões. Na dissecação anatômica, feita com as pec¸as flexionadas, procuramos encontrar o RIPNS, desde a sua porc¸ão mais medial e proximal até sua porc¸ão mais lateral e distal. Em seguida, as peças anatômicas foram fotografadas e, com o programa ImageJ, determinamos a distância do RIPNS até a linha articular medial e até uma linha horizontal inferior, que passa pela TAT e é paralela à primeira. Medimos, também, o ângulo da direc¸ão do trajeto do ramo nervoso em relac¸ão a essa linha horizontal inferior.
Resultados
O ângulo médio do trajeto do ramo nervoso, em relac¸ão à linha horizontal inferior, foi de 17,50° ± 6,17°. A distância média do RIPNS até a linha articular medial foi de 2,61 ± 0,59 cm e até a linha horizontal inferior, de 1,44 ± 0,51 cm.
Conclusão
O RIPNS foi encontrado em todos os joelhos estudados; em três, encontramos um segundo ramo, proximal ao primeiro. A direc¸ão de seu trajeto foi sempre de proximal e medial para distal e lateral. O RIPNS esteve sempre proximal e medial à TAT e distal à linha articular medial. A angulac¸ão média de sua direc¸ão, em relac¸ão a uma linha horizontal que passa pela TAT, foi de 17,50° ± 6,17°.
Palavras-chave: Joelho, Ligamento cruzado, anterior/inervacão, Ligamento cruzado anterior/cirurgiar
Introduction
Surgical reconstruction of the anterior cruciate ligament (ACL) is a very frequently performed procedure. It has been estimated that 100,000 of these procedures are performed in the United States every year and that this is the sixth commonest orthopedic surgical procedure in that country.1
Use of grafts from the tendons of the gracilis and semitendinosus muscles for surgical reconstruction of the ACL is increasingly common, because these grafts withstand high loads before failure; their cross-sectional area is large; they pass easily though the tunnels; they only need a small incision; they present low postoperative morbidity; and give rise to lower morbidity at the donor site.2
However, because of their anatomical location, there is a potential risk of injury to the infrapatellar branch of the saphenous nerve (IPBSN) during harvesting of autologous tendons from the gracilis and semitendinosus muscles.3, 4, 5, 6
In the literature, the percentage occurrence of iatrogenic lesions of the IPBSN during reconstruction of the ACL using flexor tendons ranges from 14.9% to 77%.5, 6, 7, 8, 9, 10
The orientation of the surgical incision for harvesting the tendons may, theoretically, influence the risk of injury to the IPBSN.11 Tifford et al.12 reported that vertical incisions are perpendicular to the nerve trunk and put the IPBSN at risk. According to Sabat and Kumar,13 vertical incisions have greater incidence of injuries to the IPBSN, with persistent hyperesthesia, extensive areas of sensory loss and worse subjective results. Several authors have recommended that this incision should preferentially be oblique.3, 4, 6, 8, 9, 11, 13
The aim of our study was to describe the path of the IPBSN in the region of flex or tendon harvesting, in order to provide information on where this branch is commonly encountered and thus to diminish the chances of iatrogenic injuries.
Materials and methods
Ten frozen knees originating from amputations were dissected. Six were from men and four from women. Six were right knees and four were left knees. The patients’ ages ranged from 28 to 72 years, with a mean of 41.
We removed the skin from the proximal and medial thirds of the lower leg and from the distal and medial thirds of the thigh. We then carefully searched for the IPBSN from its most medial and proximal portion to its most lateral and distal portion. The dissection was performed with the specimens flexed.
After isolating the IPBSN, we photographed each specimen using a Nikon D 3100 digital camera. The images obtained were evaluated using the ImageJ software.
On each photo, we outlined a rectangle with its sides drawn as follows: a medial vertical line that went along the lateral edge of the tibial collateral ligament; an upper horizontal line that went along the medial joint line; a lateral vertical line that went through the center of the anterior tibial tuberosity (ATT); and a lower horizontal line that also went through the ATT, perpendicular to the two vertical lines and parallel to the upper horizontal line.
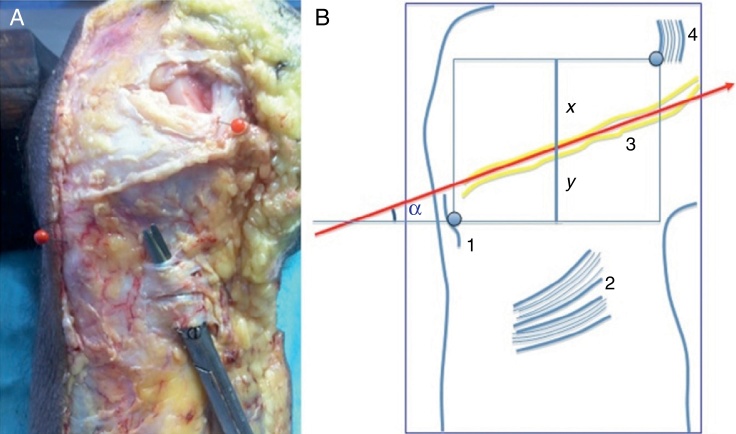
We measured the angle of the direction of the path of the nerve branch in relation to the lower side of the rectangle. We drew a straight-line segment with its ends at the midpoints of the horizontal sides of the rectangle. On this segment, we measured the distances from the nerve branch to the upper horizontal branch and to the lower horizontal branch (Fig. 1).
Fig. 1.
Photograph of a dissected right knee (A) and an illustration from this (B) showing: 1 = anterior tibial tuberosity; 2 = insertion of the flexor tendons; 3 = IPBSN; 4 = tibial collateral ligament; x = distance to the medial joint line; and y = distance to the lower horizontal line.
Results
In all the anatomical specimens, the IPBSN was found to be distal to the medial joint line and proximal and medial in relation to the ATT, and it presented a path that headed from proximal and medial to distal and lateral.
In three knees, we found a second branch located proximally to the first and distally to the medial joint line (Fig. 2).
Fig. 2.

Photograph of a dissected right knee that shows the main IPBSN (wide arrow) and another proximal branch (narrow arrow).
The mean angle of the path of the nerve branch in relation to the lower side of the rectangle was 17.50 ± 6.17°. The mean distance from the IPBSN at the straight-line segment to the medial joint line was 2.61 ± 0.59 cm and to the lower side of the rectangle (parallel to the medial joint line) was 1.44 ± 0.51 cm. All these measurements are shown in Table 1.
Table 1.
Distances from the IPBSN to the medial joint line (x) and to the lower side of the rectangle (y), in cm; length of the straight-line segment (x + y) in cm and mean angle of the direction of the path of the nerve branch (in degrees).
| Distribution of the measurements and angles | ||||
|---|---|---|---|---|
| Knee | X | y | x + y | Angle |
| 1 | 2.50 | 1.00 | 3.50 | 15.00 |
| 2 | 2.50 | 2.10 | 4.60 | 25.00 |
| 3 | 2.30 | 1.50 | 3.80 | 22.00 |
| 4 | 3.30 | 1.00 | 4.30 | 25.00 |
| 5 | 2.00 | 1.40 | 3.40 | 9.00 |
| 6 | 2.30 | 0.70 | 3.00 | 9.00 |
| 7 | 4.00 | 1.10 | 5.10 | 22.00 |
| 8 | 2.30 | 1.40 | 3.70 | 12.00 |
| 9 | 2.50 | 2.10 | 4.60 | 20.00 |
| 10 | 2.40 | 2.10 | 4.50 | 16.00 |
| Mean | 2.61 | 1.44 | 4.05 | 17.50 |
| SD | 0.59 | 0.51 | 0.67 | 6.17 |
| Minimum | 2.00 | 0.70 | 3.00 | 9.00 |
| Maximum | 4.00 | 2.10 | 5.10 | 25.00 |
Discussion
After leaving the adductor canal, the saphenous nerve follows a posteromedial course towards the medial line of the knee, where it emerges between the tendons of the gracilis and semitendinosus muscles. The IPBSN emerges proximally to the point where the saphenous nerve crosses the tendon of the gracilis and curves under the patella to supply the skin over the anterior face of the proximal tibia.3
In harvesting the flexor tendons of the gracilis and semitendinosus for ACL reconstruction, there is imminent danger of injuring the IPBSN.3, 4, 5, 6
Ebraheim and Mekhail14 reported that injuries to this branch could be caused by the incision that is made to harvest the tendons. Figueroa et al.5 believed that the injury occurred during the removal of the tendons, rather than during the skin incision. On the other hand, Kartus et al.15 believed that this inadvertent injury could occur during the procedures of skin incision, initial exposure of the tendons or drilling the tibial tunnel.
The incidence of iatrogenic injuries to the IPBSN during ACL reconstruction using flexor tendons may reach as much as 77%.5
Injury to the IPBSN may cause hypoesthesia in the anterolateral region of the proximal third of the lower leg,3, 7, 11, 16 painful neuroma,12 sympathetic reflex dystrophy17 or pain on kneeling7, 12, 18, 19 or when pressure is applied directly to the site.20 However, these symptoms only cause limitations to daily activities in a small percentage of the patients with injuries to the IPBSN.4, 7, 10, 13
Exploration of the branches of the saphenous nerve causes an enormous effect on the rate of sensory deficits.6 Changes to sensitivity at the upper extremities are considered to be of extreme importance. Sensory protection of the lower limbs perhaps also deserves great effort, especially for the sensory area of the knee that is used for kneeling.19 Therefore, it is important to locate these sensory branches, in order to avoid injury to them.
Our objective was to determine the course of the IPBSN in the region of flexor tendon harvesting, in order to provide references regarding where this branch is most frequently encountered and thus with the purpose of diminishing the likelihood of injury when the autologous tendons of the gracilis and semitendinosus are used in ACL reconstruction.
The anatomical study that we conducted was done with the specimens flexed, in the same way in which harvesting of the flexor tendons is most commonly done in ACL reconstruction. On the other hand, in the literature, some authors have reported that they conducted their studies with the knee extended.14, 20
Tifford et al.12 evaluated the effect that dynamic knee mobility might have in relation to the position of the nerve, in 20 knees from recent cadavers. They concluded that the nerve moved distally with flexion and recommended that incisions in the anterior face of the knee should be performed with the knee flexed, so as to avoid nerve injuries.
In all the knees studies, the IPBSN presented a consistent anatomical pattern: the direction of its path was always from proximal and medial to distal and lateral, and it was always located distally to the medial joint line and proximally and medially in relation to the ATT. A second branch, proximal to the first and distal to the medial joint line, was found in three knees.
In a study conducted on 129 knees from cadavers, Mochida and Kikuchi20 described two patterns for the IPBSN: type I, present in 68.2%, in which the branch crosses the medial edge of the tibia; and type II, present in 31.8%, in which the branch passes proximally to the medial joint line.
Tifford et al.12 found two main trunks of the nerve that penetrated the knee going from medial to lateral and from proximal to distal in all the knees evaluated.
In our study, the path of the IPBSN presented a mean angle of 17.50 ± 6.17° in relation to a horizontal line passing through the ATT.
It is important to determine this angle of the IPBSN in order to be able to plan an incision for harvesting the flex or tendons that diminishes the possibility of injuring this branch. If the direction of the incision is similar to that of the path of the IPBSN, it becomes easier to identify and retract this nerve.19
Several authors have recommended using oblique and horizontal incisions to expose the tibial insertions of the hamstring tendons and harvest them, since there is less chance of causing damage to the nerve branch, in comparison with vertical incisions.3, 4, 6, 8, 9, 11, 13
We can confirm that, in our hands, it was not easy to identify the IPBSN in the anatomical specimens evaluated here, even with careful dissection.
Mirzatolooei and Pisoodeh6 performed meticulous dissection in order to find and spare the superficial and sensory branches of the saphenous nerve in 98 patients, during ACL reconstruction using quadruple tendons from the hamstrings. Despite using a relatively constant type of incision, they only found the sensory branches in 44.8% of the cases and attributed this to anatomical variations.
In fact, the tourniquet that is applied during ACL reconstruction surgery may cause difficulty in differentiating between vessels and nerves, and anatomical variations may be present.6, 12, 14, 19, 20, 21
As a practical consequence of our study, we have started to perform an oblique incision that tends towards horizontal, medially to the ATT, in the region of the hamstring insertions, in performing ACL reconstruction using flexor tendons. We are seeking to push away the soft tissues proximally, towards the periosteum, in order to drill the tunnels. We believe that in this way, we may diminish the chance of injury to the sensory branch of the saphenous nerve.
Conclusion
In our study, the infrapatellar branch of the saphenous nerve was present in all the knees studied. In three of them, we found a second branch, located proximally to the first branch. The direction of the path of the nerve was always from proximal and medial to distal and lateral. In all of the specimens, the IPBSN was proximal and medial to the ATT and distal to the medial joint line. The mean angle of its direction, in relation to a horizontal line passing through the ATT was 17.50 ± 6.17 degrees.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Please cite this article as: Gali JC, Resina AF, Pedro G, Neto IAM, Almagro MAP, da Silva PAC, Caetano EB. Importância da localização anatômica do ramo infrapatelar do nervo safeno na reconstrução do ligamento cruzado anterior com tendões flexores. Rev Bras Ortop. 2014;49:625–629.
Work developed in the School of Medical Sciences and Health of Sorocaba, PUC-SP, Sorocaba, SP, Brazil.
References
- 1.Brown C.H., Jr., Carson E.W. Revision anterior cruciate ligament surgery. Clin Sports Med. 1999;18(1):109–171. doi: 10.1016/s0278-5919(05)70133-2. [DOI] [PubMed] [Google Scholar]
- 2.Bartlett R.J., Clatworthy M.G., Nguyen T.N. Graft selection in reconstruction of the anterior cruciate ligament. J Bone Joint Surg Br. 2001;83(5):625–634. doi: 10.1302/0301-620x.83b5.12308. [DOI] [PubMed] [Google Scholar]
- 3.Pagnani M.J., Warner J.J., O’Brien S.J., Warren R.F. Anatomic considerations in harvesting the semitendinosus and gracilis tendons and a technique of harvest. Am J Sports Med. 1993;21(4):565–571. doi: 10.1177/036354659302100414. [DOI] [PubMed] [Google Scholar]
- 4.Boon J.M., Van Wyk M.J., Jordaan D. A safe area and angle for harvesting autogenous tendons for anterior cruciate ligament reconstruction. Surg Radiol Anat. 2004;26(3):167–171. doi: 10.1007/s00276-003-0213-z. [DOI] [PubMed] [Google Scholar]
- 5.Figueroa D., Calvo R., Vaisman A., Campero M., Moraga C. Injury to the infrapatellar branch of the saphenousnerve in ACL reconstruction with the hamstrings technique: clinical and electrophysiological study. Knee. 2008;15(5):360–363. doi: 10.1016/j.knee.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 6.Mirzatolooei F., Pisoodeh K. Impact of exploration of sensory branches of saphenous nerve in anterior cruciate ligament reconstructive surgery. Arch Iran Med. 2012;15(4):219–222. [PubMed] [Google Scholar]
- 7.Spicer D.D., Blagg S.E., Unwin A.J., Allum R.L. Anterior knee symptoms after four-strand hamstring tendon anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2000;8(5):286–289. doi: 10.1007/s001670000139. [DOI] [PubMed] [Google Scholar]
- 8.Mochizuki T., Muneta T., Yagishita K., Shinomiya K., Sekiya I. Skin sensory change after arthroscopically-assisted anterior cruciate ligament reconstruction using medial hamstring tendons with a vertical incision. Knee Surg Sports Traumatol Arthrosc. 2004;12(3):198–202. doi: 10.1007/s00167-003-0451-y. [DOI] [PubMed] [Google Scholar]
- 9.Papastergiou S.G., Voulgaropoulos H., Mikalef P., Ziogas E., Pappis G., Giannakopoulos I. Injuries to the infrapatellar branch(es) of the saphenousnerve in anterior cruciate ligament reconstruction with four-strand hamstring tendon autograft: vertical versus horizontal incision for harvest. Knee Surg Sports Traumatol Arthrosc. 2006;14(8):789–793. doi: 10.1007/s00167-005-0008-3. [DOI] [PubMed] [Google Scholar]
- 10.Sanders B., Rolf R., McClelland W., Xerogeanes J. Prevalence of saphenous nerve injury after autogenous hamstring harvest: an anatomic and clinical study of sartorial branch injury. Arthroscopy. 2007;23(9):956–963. doi: 10.1016/j.arthro.2007.03.099. [DOI] [PubMed] [Google Scholar]
- 11.Kjaergaard J., Faunø L.Z., Faunø P. Sensibility loss after ACL reconstruction with hamstring graft. Int J Sports Med. 2008;29(6):507–511. doi: 10.1055/s-2008-1038338. [DOI] [PubMed] [Google Scholar]
- 12.Tifford C.D., Spero L., Luke T., Plancher K.D. The relationship of the infrapatellar branches of the saphenous nerve to arthroscopy portals and incisions for anterior cruciate ligament surgery. An anatomic study. Am J Sports Med. 2000;28(4):562–567. doi: 10.1177/03635465000280042001. [DOI] [PubMed] [Google Scholar]
- 13.Sabat D., Kumar V. Nerve injury during hamstring graft harvest: a prospective comparative study of three different incisions. Knee Surg Sports Traumatol Arthrosc. 2013;21(9):2089–2095. doi: 10.1007/s00167-012-2243-8. [DOI] [PubMed] [Google Scholar]
- 14.Ebraheim N.A., Mekhail A.O. The infrapatellar branch of the saphenous nerve: an anatomic study. J Orthop Trauma. 1997;11(3):195–199. doi: 10.1097/00005131-199704000-00010. [DOI] [PubMed] [Google Scholar]
- 15.Kartus J., Movin T., Karlsson J. Donor-site morbidity and anterior knee problems after anterior cruciate ligament reconstruction using autografts. Arthroscopy. 2001;17(9):971–980. doi: 10.1053/jars.2001.28979. [DOI] [PubMed] [Google Scholar]
- 16.Kartus J., Magnusson L., Stener S., Brandsson S., Eriksson B.I., Karlsson J. Complications following arthroscopic anterior cruciate ligament reconstruction. A 2–5-year follow-up of 604 patients with special emphasis on anterior knee pain. Knee Surg Sports Traumatol Arthrosc. 1999;7(1):2–8. doi: 10.1007/s001670050112. [DOI] [PubMed] [Google Scholar]
- 17.Poehling G.G., Pollock F.E., Jr., Koman L.A. Reflex sympathetic dystrophy of the knee after sensory nerve injury. Arthroscopy. 1988;4(1):31–35. doi: 10.1016/s0749-8063(88)80008-2. [DOI] [PubMed] [Google Scholar]
- 18.Corry I.S., Webb J.M., Clingeleffer A.J., Pinczewski L.A. Arthroscopic reconstruction of the anterior cruciate ligament. A comparison of patellar tendon autograft and four-strand hamstring tendon autograft. Am J Sports Med. 1999;27(4):444–454. doi: 10.1177/03635465990270040701. [DOI] [PubMed] [Google Scholar]
- 19.Hunter L.Y., Louis D.S., Ricciardi J.R., O’Connor G.A. The saphenous nerve: its course and importance in medial arthrotomy. Am J Sports Med. 1979;7(4):227–230. doi: 10.1177/036354657900700403. [DOI] [PubMed] [Google Scholar]
- 20.Mochida H., Kikuchi S. Injury to infrapatellar branch of saphenous nerve in arthroscopic knee surgery. Clin Orthop Relat Res. 1995;320:88–94. [PubMed] [Google Scholar]
- 21.Arthornthurasook A., Gaew-Im K. Study of the infrapatellar nerve. Am J Sports Med. 1988;16(1):57–59. doi: 10.1177/036354658801600110. [DOI] [PubMed] [Google Scholar]