Abstract
Given the well-known linkage between diabetes mellitus (DM) and tuberculosis (TB), the World Health Organization recommends bidirectional screening. Here we report the first screening effort of its kind from a chest clinic in the Ampara district of Sri Lanka. Of 112 TB patients registered between January 2013 and October 2014, eight had pre-existing DM. Of those remaining, 83 (80%) underwent fasting plasma glucose testing, of whom two (2%) and 17 (20%) were found to have diabetes and impaired fasting glucose, respectively. All of these were enrolled in care. Screening TB patients for DM was found to be feasible at the district level. Further studies at the provincial/country level are required before making any decision to scale up bidirectional screening.
Keywords: tuberculosis, diabetes mellitus, screening
Abstract
Etant donné le lien bien connu entre diabète (DM) et tuberculose (TB), l'Organisation Mondiale de la Santé recommande un dépistage bidirectionnel. Nous rapportons ici le premier effort de dépistage de ce type au Sri Lanka dans un centre de maladies respiratoires du district d'Ampara. Sur 112 patients TB enregistrés entre janvier 2013 et octobre 2014, huit avaient un DM préexistant. Parmi les autres, 83 (80%) ont eu une glycémie à jeun et parmi eux, respectivement deux (2%) et 17 (20%) ont eu un diabète et une glycémie à jeun trop élevée; tous ont été enrôlés dans un programme de soins. Le dépistage du DM chez des patients TB s'est avéré faisable au niveau du district. D'autres études au niveau provincial/national sont nécessaires avant de décider l'extension de la stratégie.
Abstract
Dado el vínculo reconocido entre la diabetes (DM) y la tuberculosis (TB), la Organización Mundial de la Salud recomienda la detección sistemática bidireccional. En el presente estudio se comunica la primera campaña de detección de este tipo emprendida en Sri Lanka, en un consultorio de neumología del distrito de Ampara. De los 112 pacientes notificados al registro de TB de enero del 2013 a octubre del 2014, en ocho prexistía el diagnóstico de DM. De los casos restantes (80%), en 83 se practicó la glucemia plasmática en ayunas y se puso en evidencia el diagnóstico de DM en dos de ellos (2%) y 17 pacientes presentaron una glucemia basal alterada (20%); todos los pacientes ingresaron a un programa de atención. Se confirmó que es factible practicar la detección sistemática de la DM en los pacientes con diagnóstico de TB a escala distrital. Será necesario realizar estudios a escala de la provincia y del país antes de adoptar decisiones de ampliación de escala de la medida.
Diabetes mellitus (DM) is an independent risk factor for developing tuberculosis (TB) and for adverse anti-tuberculosis treatment outcomes such as failure, relapse and death.1 It is estimated that 9 million new TB cases and 1.5 million TB deaths occurred globally in 2013.2 The burden of DM is increasing worldwide, and concerns have been raised about the emerging co-epidemics of DM and TB, especially in low- to middle-income countries.3,4 In 2013, according to the International Diabetes Federation, an estimated 381 million people had DM, a figure that is likely to have doubled by 2030.5 A study performed in Sri Lanka during 2005 and 2006 found that 10.3% of the population aged ⩾20 years had DM, while 21.8% of the population had some form of dysglycaemia.6
It has been recommended that TB patients be routinely screened for DM and linked to DM care services if diagnosed with the disease.7 In Sri Lanka, there are currently no records or screening programmes to evaluate DM status among TB patients at district or national level. A system was developed to screen for DM among TB patients at the District Chest Clinic (DCC) in the Ampara district from January 2013 onward as part of regular routine clinic work. These data would be useful to estimate the needs for DM care services required among patients on anti-tuberculosis treatment, and would assist in establishing linkages between TB and DM care services. In this study, we report the prevalence of DM and impaired fasting glucose (IFG) in a cohort of TB patients registered in Ampara, Sri Lanka.
METHODS
This was a cross-sectional pilot study involving a review of clinic records. The Ampara DCC provides services for a population of 280 000. Patients with presumptive or confirmed TB are referred from primary health care facilities in the district.
All TB patients registered in the Ampara DCC from 1 January 2013 to 15 October 2014 were asked if they had DM or whether they had symptoms suggestive of DM, such as polyuria, polydipsia or weight loss. All non-diabetic TB patients were requested to undergo a fasting blood glucose (FBG) test at the nearby general hospital. Patients with FBG levels ⩾126 mg/dl (⩾7 mmol/l) were diagnosed as having DM, while those with FBG levels between 100 and 125 mg/dl (5.6–6.9 mmol/l) were diagnosed as having IFG. All patients newly diagnosed with DM and IFG were enrolled into diabetes care.8
Data variables were extracted from the District TB register and treatment cards, double-entered, validated and analysed using EpiData v. 31 for data entry and v. 2.2.2.182 for analysis (EpiData Association, Odense, Denmark). The number needed to screen (NNS) for diagnosing TB patients with newly diagnosed DM and IFG was calculated in proportion to the total screened.
Ethics approval was obtained from the Ethics Review Committee of the Faculty of Medicine, Sri Jayawardhanapura, Colombo, Sri Lanka, and the Ethics Advisory Group of the International Union Against Tuberculosis and Lung Disease, Paris, France.
RESULTS
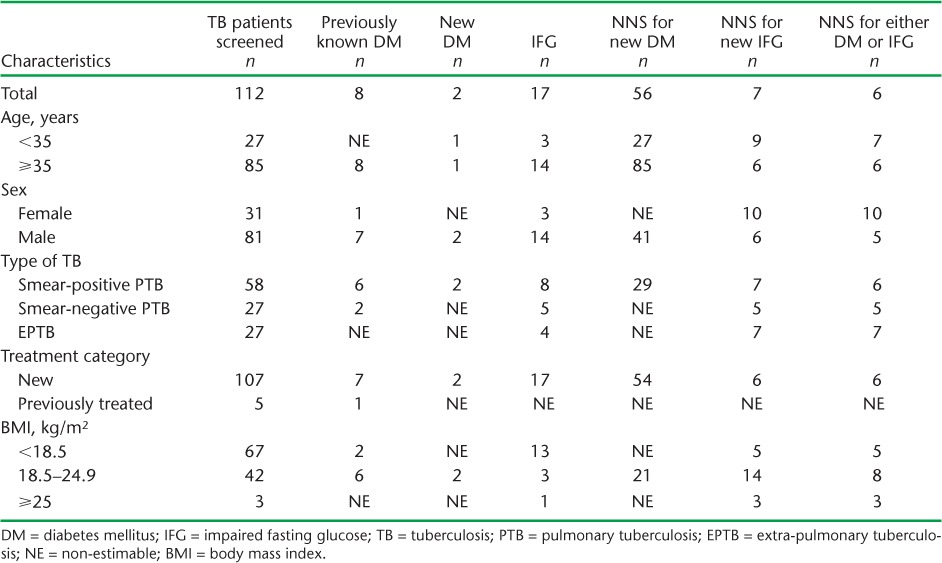
Of 112 patients screened (71% males, median age 51 years, 60% with body mass index <18.5 kg/m2), pulmonary TB (PTB) was diagnosed in 76% and smear-positive PTB in 52%. Ninety-six per cent of the patients were classified as ‘new’ and received Category 1 treatment. There were eight pre-diagnosed DM patients. Of the 104 patients eligible for FBG screening, 80% underwent testing; respectively 2 (2%) and 17 (20%) were found to have DM and IFG (Figure). The number of TB patients with DM and the NNS for diagnosing DM and IFG are shown in the Table. All those diagnosed with DM and IFG were enrolled for care at the Diabetes Clinic.
FIGURE.
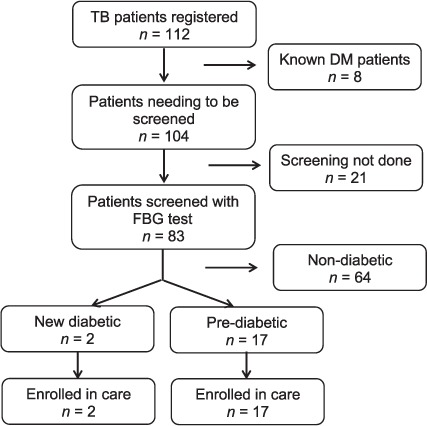
Flow chart of diabetes screening among TB patients registered in the District Chest Clinic, Ampara, Sri Lanka, January 2013–October 2014. TB = tuberculosis; DM = diabetes mellitus; FBG = fasting blood glucose.
TABLE.
Number of TB patients needed to screen (NNS) to identify one new case of DM, one new case with IFG, and both DM and IFG, in the district chest clinic in Ampara, Sri Lanka, January 2013–October 2014
DISCUSSION
To our knowledge this is the first documentation of a pilot screening activity for DM among TB patients in Sri Lanka. We found that it is feasible to screen for DM among TB patients at the district level using a simple screening strategy that included a brief history and a single FBG test. We also found that it was feasible to link all newly diagnosed DM or pre-diabetes patients to care.
Despite the good performance of the Sri Lankan National Programme for Tuberculosis Control and Chest Diseases (NPTCCD), several co-morbidities, such as DM, which have the potential to affect TB control efforts, have not been adequately addressed. Twenty-one patients were not screened with FBG as they were followed up in different chest clinics, although registration and clinical screening were undertaken at the Ampara DCC. This operational problem has now been resolved, as the NPTCCD made baseline FBG testing mandatory in 2014. Systematic reviews have highlighted the need for increased attention to the treatment of TB in people with DM, including systematic testing for early detection, intensified glucose control and increased clinical monitoring.1,4 Our study provides field experience that such activities can be easily integrated into the services of existing chest clinics.
The proportion of DM among TB patients in Ampara was similar to that of the general population found in the national DM survey, unlike studies in India, where DM prevalence among TB patients has been higher overall (25–44%) and about two–three times higher than in the general population.6,9 India has passed a government policy directive that all registered TB patients should be screened for DM.10
It was estimated that the NNS to detect one previously undiagnosed case of DM ranges from 4 to 50, depending on the TB and DM epidemiology of the setting, the age group screened and the sensitivity of the screening algorithm.9,10 In our study, the NNS for identifying a new DM case was relatively high, at 56, thus begging the question as to whether routine testing of all TB patients is cost-effective.
The strength of this study is that we implemented and documented screening as routine practice in the Ampara DCC without the allocation of a special budget. Nearly 80% of all non-diabetic patients were screened, indicating the feasibility and patient acceptability of the strategy.
There are some limitations in this pilot study. First, as it was implemented in a single district, the findings may not be generalisable to the whole country. Moreover, the size of the TB cohort screened was small and only FBG was performed to screen for DM; FBG is known to be less sensitive compared to glycosylated haemoglobin or oral glucose tolerance tests. Furthermore, some of the cases could be due to stress-induced hyperglycaemia (caused by a chronic infection such as TB), and would need to be re-tested for confirmation after completion of anti-tuberculosis treatment.
In conclusion, our study demonstrates that it is feasible to screen TB patients for DM at district level and link TB-DM patients to DM care. We recommend that further studies be conducted at the province and country level before making decisions around scale-up.
Acknowledgments
This research was conducted through the Structured Operational Research and Training Initiative (SORT IT), a global partnership led by the Special Programme for Research and Training in Tropical Diseases at the World Health Organization (WHO/TDR). The model is based on a course developed jointly by the International Union Against Tuberculosis and Lung Disease (The Union) and Médecins Sans Frontières (MSF). The specific SORT IT programme that resulted in this publication was jointly developed and implemented by The Union South-East Asia Regional Office, New Delhi, India; the Centre for Operational Research, The Union, Paris, France; the Operational Research Unit (LUXOR), MSF, Brussels Operational Centre, Luxembourg; and the Burnet Institute, Melbourne, Victoria, Australia. We thank S Talagala (Regional Director of Health Service, Ampara), S Indralal (consultant physician, TH, Rathnapura) and the staff of the District Chest Clinic, Ampara, for support.
Footnotes
Conflicts of interest: none declared.
References
- 1.Baker M A, Harries A D, Jeon C Y et al. The impact of diabetes on tuberculosis treatment outcomes: a systematic review. BMC Med. 2011;9:81. doi: 10.1186/1741-7015-9-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Global tuberculosis control, 2014. Geneva, Switzerland: WHO; 2014. WHO/HTM/TB/2014.15. [Google Scholar]
- 3.Lönnroth K, Roglic G, Harries A D. Improving tuberculosis prevention and care through addressing the global diabetes epidemic: from evidence to policy and practice. Lancet Diabetes Endocrinol. 2014;2:730–739. doi: 10.1016/S2213-8587(14)70109-3. [DOI] [PubMed] [Google Scholar]
- 4.Harries A D, Satyanarayana S, Kumar A M V et al. Epidemiology and interaction of diabetes mellitus and tuberculosis and the challenges for care: a review. Public Health Action. 2013;3(Suppl 1):S3–S9. doi: 10.5588/pha.13.0024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wild S, Roglic G, Green A et al. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;5:1047–1053. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 6.Katulanda P, Constantine G R, Mahesh J G et al. Prevalence and projections of diabetes and pre-diabetes in adults in Sri Lanka—Sri Lanka Diabetes, Cardiovascular Study (SLDCS) Diabet Med. 2008;25:1062–1069. doi: 10.1111/j.1464-5491.2008.02523.x. [DOI] [PubMed] [Google Scholar]
- 7.India Tuberculosis-Diabetes Study Group. Screening of patients with tuberculosis for diabetes mellitus in India. Trop Med Int Health. 2013;18:636–645. doi: 10.1111/tmi.12084. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization/International Diabetes Federation. Definition and diagnosis of diabetes mellitus and intermediate hyperglycaemia. Summary of technical report and recommendations. Report of a WHO/IDF consultation. Geneva, Switzerland: WHO; 2006. [Google Scholar]
- 9.Balakrishnan S, Vijayan S, Nair S et al. High diabetes prevalence among tuberculosis cases in Kerala, India. PLOS ONE. 2012;7:e46502. doi: 10.1371/journal.pone.0046502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization/International Union Against Tuberculosis and Lung Disease. Provisional collaborative framework for care and control of tuberculosis and diabetes. Geneva, Switzerland: WHO; 2011. WHO/HTM/TB/2011.15. [Google Scholar]


