Abstract
This retrospective observational review documents the efforts of the Swaziland National Tuberculosis (TB) Control Programme between 2004 and 2014. The objective is to describe the disparity between actual declines in case notification and increases in estimated incidence. The review of policies and practices shows the most influential factors associated with the decrease in TB case notification to be an increase in access to antiretroviral therapy for co-infected TB patients, the general success of TB and human immunodeficiency virus service integration in the country and improvements in implementation of all components of directly observed treatment, active case finding, and rapid diagnosis using new technologies.
Keywords: TB case notification, new and recurrent TB, smear-negative TB, antiretroviral therapy
Abstract
Cette étude d'observation rétrospective documente les efforts du programme de lutte contre la tuberculose (TB) du Swaziland entre 2004 et 2014. L'objectif est de décrire la disparité entre un réel déclin dans la déclaration des cas et une augmentation de l'incidence estimée. La revue des politiques et des pratiques montre que les facteurs les plus influents associés au déclin de la déclaration des cas de TB sont liés à une augmentation de l'accès aux antirétroviraux pour les patients tuberculeux co-infectés, au succès d'ensemble de l'intégration des services pour la TB et ceux pour le virus de l'immunodéficience humaine dans le pays et aux améliorations dans la mise en œuvre de tous les composants du traitement sous observation directe, de la recherche active des cas et d'un diagnostic rapide grâce aux techniques nouvelles.
Abstract
Con el presente análisis observacional retrospectivo se documentan las iniciativas emprendidas por el Programa de Control de la Tuberculosis (TB) de Swazilandia del 2004 al 2014. El objetivo del estudio fue describir la discrepancia existente entre la disminución en la notificación de casos de TB y el aumento en las estimaciones de incidencia de la enfermedad. El análisis de las políticas y las prácticas puso de manifiesto que los factores que más influyen sobre la disminución de la notificación de casos de TB es un aumento en el acceso al tratamiento antirretrovírico por parte de los pacientes coinfectados por el virus de la inmunodeficiencia humana y la TB, el éxito general de la integración de los servicios que se ocupan de ambas enfermedades en el país y los progresos en la aplicación de todos los componentes del tratamiento directamente observado, la búsqueda activa de casos y el diagnóstico rápido mediante nuevas tecnologías.
At 1382 cases per 100 000 population, Swaziland has the highest estimated incidence of tuberculosis (TB) in the world, along with a high burden of drug-resistant TB.1 The country also has the highest prevalence of human immunodeficiency virus (HIV) in the world (31% of adults aged 18–49 years), with 74% of TB patients co-infected with HIV.2
In 1999 and 2011, the Swaziland government declared both HIV and TB to be national emergencies (http://www.who.int/hiv/HIVCP_SWZ.pdf and http://stoptb.org/news/stories/2011/ns11_019.asp). The Ministry of Health (MoH), working with technical assistance partners and donors, has implemented systematic responses to curb the dual epidemic. Over a period of ten years, significant changes were made to policy and practice for both diseases.
ASPECTS OF INTEREST
Although World Health Organization (WHO) reports continue to show an increase in the estimated incidence and prevalence of TB in Swaziland, the actual notification of new and relapse cases has decreased since 2010.1 This retrospective observational review examines this disparity in the context of actions taken by the MoH through the National Tuberculosis Control Programme (NTCP) and the Swaziland National AIDS Programme.
As this review used existing data, ethical approval was not required.
Although the implementation of a prevalence survey is recommended to provide a definitive measure of the tuberculosis situation in a country, no such survey has as yet been conducted in Swaziland. A detailed analysis of country data reported to the WHO between 1995 and 2013 showed an overall increase in the notification of all types of TB cases until 2010 and a decline thereafter, most dramatically among smear-negative patients (Figure 1). Notification of previously treated cases, excluding relapse cases, also decreased, from 1045 in 2010 to 437 in 2013.1
FIGURE 1.
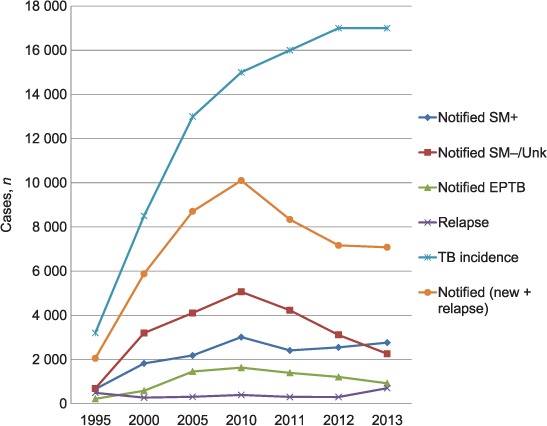
Estimated TB incidence, notification and notification by TB category, Swaziland, 1995–2013.1 SM+ = smear-positive; SM− = smear-negative; Unk = unknown; EPTB = extra-pulmonary tuberculosis; TB = tuberculosis.
The HIV incidence rate has declined from a peak of 6% in 1999, and is projected to fall to 2.3% by 2015.2,3 The MoH has dramatically expanded antiretroviral therapy (ART) since 2003, and has succeeded in achieving 90% coverage among individuals with WHO Stage III/IV or with a CD4 count <350 cells/mm3, with 85% retention at 12 months; 85% of clients reported to be on ART have a viral load <1000 cp/ml.2 The pre-ART programme was prioritised to promote a package of services that included TB screening and provision of cotrimoxazole preventive therapy (CPT) and isoniazid preventive therapy (IPT). A WHO and joint external TB programme review in 2014 highlighted significant achievements in collaborative TB-HIV activities, with over 98% of TB-HIV co-infected patients on CPT and over 70% on ART.4
DISCUSSION
Settings with high TB-HIV co-infection rates experience a reduction in the sensitivity of sputum microscopy as a diagnostic tool, resulting in higher smear negativity rates among patients with low CD4 levels.5 The results of this review showed that, in 2010, the increasing trend in TB case notification reversed, with a more pronounced decrease among smear negatives. There was a plateau in the total number of cases notified, a slight increase in bacteriologically confirmed cases and at the same time a substantial decrease in smear-negative cases between 2012 and 2013 (Figure 1). In addition, the 58% decrease in retreatment cases far outpaces the 10–20% given in the WHO guidelines as a marker for an effective TB control programme.6
Swaziland has implemented all components of the DOTS strategy since 2006, which might explain the increasing case notifications until 2010 and the improved treatment success rates between 2006 and 2013 (from 42% to 73%).1 Moreover, Swaziland was one of the first countries to adopt the WHO recommendation to use the Xpert® MTB/RIF assay (Cepheid, Sunnyvale, CA, USA) as the primary diagnostic test for TB among people living with HIV (PLHIV) with signs and symptoms of TB, possibly explaining the increase in bacteriologically confirmed cases between 2012 and 2013.7 A policy change in 2010 to implement intensified case finding, infection control and IPT, coupled with task shifting for TB screening, led to almost universal screening in HIV clinics, out-patient departments, specialty clinics, in-patient wards and, more recently, communities. High-quality TB screening and rapid testing for presumptive cases can result in earlier detection, reduced transmission of TB and reduced TB-related morbidity and mortality. The fact that numbers of smear-negative cases are still decreasing may indicate successful collaborative TB-HIV activities and ART scale-up in the general population (Figure 2).8 High ART implementation is associated with significant declining trends in new and recurrent TB case notifications at population level.9
FIGURE 2.

Comparison of TB case finding against national ART scale-up, Swaziland, 2001–2013.8 TB = tuberculosis; ART = antiretroviral therapy; EPTB = extra-pulmonary tuberculosis; PTB = pulmonary tuberculosis.
The importance of early ART initiation for co-infected patients has been emphasised in recent years as one of the most critical means of reducing HIV-related TB incidence and TB-related morbidity and mortality among PLHIV.9 ART may reduce the individual risk for developing TB disease among PLHIV by 65%, and rapid initiation of ART may improve outcomes among smear-negative patients.10 In 2009, Swaziland expanded treatment eligibility to CD4 <350 cells/mm3 for adults with HIV, and recommended testing and treating all TB-HIV-co-infected patients, regardless of CD4 count. As a result, access to ART for TB patients has steadily increased (Figure 2).
We believe that the interventions by the MoH to curb the dual epidemic warrant a re-examination of the current projected TB incidence trend. The case detection rate in Swaziland reached a maximum of 70% in 2009; however, since then, the increasing estimated incidence has led to a decline in case detection.1 For countries without recent prevalence or incidence studies, the WHO produces annual estimates using information drawn from surveillance systems, special studies, expert opinion and country consultations. However, alternative calculations for the incidence estimates determined that the methods used by the WHO in its annual estimates and in the Global burden of disease report 2010 are not representative,11 and suggest that improvements are needed at the country level to make case notification a better proxy for TB incidence. The possible overestimation of the number of annual cases could skew the case detection rate to indicate that a lower proportion of cases are being picked up than are actually being detected and treated.
CONCLUSION
Several factors have impacted the TB epidemic in Swaziland in recent years, including implementation of DOTS, ART scale-up and increased ART for HIV-co-infected TB patients, nationwide implementation of TB screening and rapid diagnosis using new technologies. The significant discrepancies between the WHO estimates and current programme data warrant further investigation, preferably in the form of a prevalence study. Resources should be mobilised to undertake a prevalence survey to gain an accurate picture of the country's disease burden, update the WHO estimates, and guide future strategies.
Acknowledgments
The authors acknowledge the Monitoring and Evaluation Unit of the Swaziland National TB Control Programme, the World Health Organization-led 2014 TB review team, which conducted a detailed analysis of the data, and the Ministry of Health and University Research Co., LLC staff, who have been part of the improvements in TB and HIV care in Swaziland. Funding for this work was provided by the US President's Emergency Fund for AIDS Relief (PEPFAR) through the United States Agency for International Development (USAID) and its Applying Science to Strengthen and Improve Systems (ASSIST) Project, managed by the University Research Co., LLC.
Footnotes
Conflicts of interest: none declared.
References
- 1.World Health Organization. Global tuberculosis control, 2014. Geneva, Switzerland: WHO; 2014. WHO/HTM/TB/2014. [Google Scholar]
- 2.Bicego G T, Nkambule R, Peterson I et al. Recent patterns in population-based HIV prevalence in Swaziland. PLOS ONE. 2013;8:e77101. doi: 10.1371/journal.pone.0077101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.United Nations in Swaziland. Joint United Nations Programme of support on HIV and AIDS (JUNPS), 2005–2015. Mbabane, Swaziland: UNICEF; 2009. [Google Scholar]
- 4.Ministry of Health. Report of joint external review of the Kingdom of Swaziland National TB Programme, April 2014. Kingdom of Swaziland Ministry of Health; Mbabane, Swaziland: 2015. [Google Scholar]
- 5.Cattamanchi A, Dowdy D W, Davis J L et al. Sensitivity of direct versus concentrated sputum smear microscopy in HIV-infected patients suspected of having pulmonary tuberculosis. BMC Infect Dis. 2009;9:53. doi: 10.1186/1471-2334-9-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stop TB Partnership. Compendium of indicators for monitoring and evaluating national tuberculosis programs. Geneva, Switzerland: WHO; 2004. WHO/HTM/TB/2004.344. [Google Scholar]
- 7.World Health Organization. WHO policy on collaborative TB/HIV activities: guidelines for national programmes and other stakeholders. Geneva, Switzerland: WHO; 2012. WHO/HTM/TB/2012.1. [PubMed] [Google Scholar]
- 8.Houben R M, Glynn J R, Mboma S et al. The impact of HIV and ART on recurrent tuberculosis in a sub-Saharan setting. AIDS. 2012;26:2233–2239. doi: 10.1097/QAD.0b013e32835958ed. [DOI] [PubMed] [Google Scholar]
- 9.Van Schalkwyk C, Mndzebele S, Hlophe T et al. Outcomes and impact of HIV prevention, ART and TB Programs in Swaziland — early evidence from public health triangulation. PLOS ONE. 2013;8:e69437. doi: 10.1371/journal.pone.0069437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Blanc F X, Sok T, Laureillard D et al. Earlier versus later start of antiretroviral therapy in HIV-infected adults with tuberculosis. N Engl J Med. 2011;365:1471–1481. doi: 10.1056/NEJMoa1013911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ortblad K F, Lozano R, Murray C J L. An alternative estimation of tuberculosis incidence from 1980 to 2010: methods from the Global Burden of Disease 2010. Lancet. 2013;381(Suppl):S104. [Google Scholar]


