Abstract
Background
The multidisciplinary tumour conference (MTC) represents the standard of care in the management of hepatocellular carcinoma (HCC). Clinical outcomes in relation to adherence and non-adherence to MTC recommendations have not been studied.
Methods
A total of 137 patients with HCC and cirrhosis whose cases were submitted to a first MTC discussion between 1 January 2009 and 31 December 2010 were identified. Clinical data, management recommendations, adherence, treatment regimens and overall survival were reviewed.
Results
There were 419 MTC discussions on 137 patients with cirrhosis and HCC. The MTC recommendations made in 145 discussions on 90 separate patients were not followed. Patient-related reasons for deviation from MTC recommendations included failure to attend for follow-up (n = 24, 16.6%), clinical deterioration (n = 19, 13.1%) and patient preference (n = 13, 9.0%). Physician-related reasons for discordance included treating physician preference (n = 43, 29.7%) and finding that the patient was not a candidate for the recommended intervention (n = 37, 25.5%). After the first MTC discussion, 62.0% of patients received the recommended treatment; these patients were more likely to be alive at 1 year compared with those who did not receive the recommended treatment (P = 0.007). More of the patients who followed recommendations underwent liver transplantation (25.6% versus 14.4%; P = 0.10).
Conclusions
There are patient-related as well as physician-related reasons for non-adherence to recommendations. Non-adherence affects clinical outcomes and can be avoided in selected cases.
Introduction
Hepatocellular carcinoma (HCC) is the fastest-growing cause of cancer-related death in the USA.1 There are several explanations for the rising burden of disease, including the natural history of the national hepatitis C epidemic, the immigration of people from endemic hepatitis B regions, increased implementation of HCC screening protocols, the increasing prevalence of non-alcoholic steatohepatitis, and the ageing of the population.
Fortunately, to meet the needs of the growing, complex population with HCC, great strides have been achieved over the past two decades and have resulted in excellent surgical and locoregional as well as pharmacologic options. As a result, several disciplines have a stake in the management of an HCC patient. From his or her initial evaluation to confirmation of diagnosis and treatment, the HCC patient is cared for by a combination of internists, hepatologists, pathologists, radiologists (diagnostic and interventional), surgeons and oncologists (medical and radiation). To coordinate HCC treatment, the new standard of care involves interdisciplinary collaboration initiated as multidisciplinary tumour conferences (MTCs).
A wealth of data on the outcomes of HCC management have been published in journals that cater to any of the aforementioned disciplines. Issues include the primacy of liver transplantation for HCC,2,3 resection versus ablation for small tumours,4 the impact of Child–Turcotte–Pugh class on outcome,5 radiofrequency ablation (RFA) versus transarterial chemoembolization (TACE),6 and the treatment of very early HCC.7 Clearly, caring for patients with HCC requires collaboration among the aggregate specialists.
The matching of the patient with HCC and the correct therapy requires deliberation and multidisciplinary input. Accordingly, the MTC is a good example of personalized medicine. The MTC is also, in effect, a tool. Tools can be inefficient, misused or misunderstood. Especially complex tools require pause for re-evaluation. They can be crafted and improved. Tools should be judged by their ability to satisfy their intended aims.
The primary aim of this retrospective analysis was to describe the reasons for non-adherence to MTC management recommendations. The secondary aim was to correlate adherence patterns with clinical outcomes, particularly with respect to liver transplantation. The present paper describes the 3.5-year experience of a single referral centre in the MTC.
Materials and methods
Setting and patients
The Beth Israel Deaconess Medical Center (BIDMC) is a 649-bed teaching hospital affiliated with Harvard Medical School and located in Boston, Massachusetts. It is one of the main referral centres for liver transplantation in New England. Within the BIDMC liver centre, there is a liver tumour clinic that aims to coordinate care among subspecialists in the treatment of patients with both primary and metastatic tumours. An MTC is held weekly to discuss patients with suspected or established HCC. Attendees include five hepatologists, three oncologists, one radiation oncologist, three interventional radiologists, one pathologist, three surgeons, three radiologists, and five mid-level staff including nurses, nurse practitioners and physician assistants. The goal of this meeting is to construct an individualized diagnostic and treatment plan for each of the patients discussed.
At every MTC, a designated team member, typically a nurse practitioner or physician assistant, inserts a short summary of each discussion into the BIDMC online medical records (OMR). This documentation includes a pertinent history of the patient’s underlying liver disease and tumour, completed diagnostic studies, and any prior treatment. The recorder also includes relevant changes that have occurred in the interim between meetings, and a brief description of imaging reviewed during the MTC. Lastly, the specific recommendations for each patient, such as follow-up imaging [ultrasound, computed tomography (CT), magnetic resonance imaging (MRI)] with a timeframe for completion, biopsy, RFA, TACE, cyberknife (CK), surgical resection, systemic therapy and/or liver transplantation are documented. The MTC recommendations are specific and therefore any deviation is considered a discrepancy.
In this retrospective cohort study, data were collected for 137 patients diagnosed with cirrhosis and HCC whose cases were presented to a first MTC discussion between January 2009 and December 2010. The diagnosis of HCC was confirmed for every patient according to National Comprehensive Cancer Network guidelines using radiographic, biochemical and histologic findings. The mean number of discussions per patient was three (median: 2; mode: 2). The mean follow-up time from first discussion until the primary outcome (death, transplantation, alive without transplant at 15 July 2012, or loss from follow-up) was 16.7 months or 502 days. Patients were excluded from the study if they did not have a confirmed diagnosis of HCC, if their first MTC discussion was prior to 2009 or after 2010, or if there was insufficient documentation in the OMR (n = 2).
Database and data collection
A database was constructed using Microsoft Access to securely store all collected information. A retrospective chart review was performed to determine basic demographic information and underlying liver disease in all patients who met the inclusion criteria. Clinical characteristics as well as details of all MTC case discussions were available through the hospital’s OMR. Each MTC meeting prior to 15 July 2012 was reviewed as a separate event. At every discussion, Child–Turcotte–Pugh status was determined. Prior treatments including liver-directed therapy (RFA, TACE, CK), surgical resection, transplantation and systemic therapy were noted. The MTC plan for observation, diagnostic workup or preferred treatment was documented. In addition, actual actions were identified, and whether or not they differed from the original recommendations was noted. The primary outcomes were death, transplantation, alive without transplant at 15 July 2012 and loss from follow-up. The date of a patient’s death was confirmed using the Social Security Death Master File (SSDMF). The date of liver transplantation was confirmed by review of the hospital OMR.
Statistics
Information stored in Microsoft Access was exported to Microsoft Excel for analysis. All data were kept in a firewall-secured server and/or password-protected Microsoft Excel file (Version Info; Microsoft Corp., Redmond, WA, USA). Data were analysed using jmp sas Version 8 (SAS Institute, Inc., Cary, NC, USA). Data are recorded as the median (days) or as percentages as noted in the tables. Descriptive statistics included the mean and standard deviation (SD) for normal distributions and the median and range for non-normal distributions (e.g. distributions in which the SD exceeded the mean). Means were compared using the Wilcoxon rank sum method and proportions were compared using Fisher’s exact method.
Results
Patient characteristics
A total of 137 unique patients met the study inclusion criteria (Fig. 1). Patients were verified as having a diagnosis of HCC and cirrhosis on manual chart review. Table 1 summarizes the baseline characteristics of all included patients categorized according to the Child–Pugh class designated at the initial discussion. In two patients, Child–Pugh class could not be determined based on the limited information available in the OMR. The median age of the patients was 60 years. The majority of patients were male (n = 116, 84.7%) and White (n = 99, 72.3%). The most common aetiologies of underlying liver disease were hepatitis C (n = 85, 62.0%), alcohol consumption (n = 45, 32.8%), and hepatitis B (n = 17, 12.4%). Some patients had multiple aetiologies of cirrhosis (n = 28, 20.4%). Prior HCC treatment had been delivered in 36 patients; the most common treatment prior to the first MTC discussion was RFA (n = 16, 11.7%), followed by TACE (n = 10, 7.3%) and resection (n = 10, 7.3%).
Figure 1.
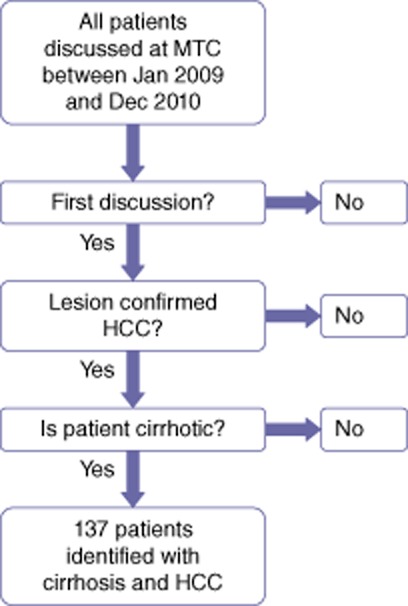
Patient selection for the present study according to date of first presentation at a multidisciplinary tumour conference (MTC) and diagnosis of hepatocellular carcinoma (HCC) and cirrhosis
Table 1.
Characteristics of patients with cirrhosis and hepatocellular carcinoma at first presentation at a multidisciplinary tumour conference
| Child–Pugh status | Total | ||||
|---|---|---|---|---|---|
| Class A | Class B | Class C | Unknown | ||
| Patients, n (%) | 81 (59.1%) | 34 (24.8%) | 20 (14.6%) | 2 (1.5%) | 137 |
| Age, years, median | 62.0 | 58.5 | 60.0 | 63.5 | 60.0 |
| Sex, n (%) | |||||
| Male | 68 (84.0%) | 29 (85.3%) | 17 (85.0%) | 2 | 116 (84.7%) |
| Female | 13 (16.0%) | 5 (14.7%) | 3 (15.0%) | 0 | 21 (15.3%) |
| Race, n (%) | |||||
| White | 48 (59.3%) | 31 (91.2%) | 20 (100%) | 0 | 99 (72.3%) |
| African-American | 8 (9.9%) | 1 (2.9%) | 0 | 0 | 9 (6.6%) |
| Hispanic | 8 (9.9%) | 0 | 0 | 0 | 8 (5.8%) |
| East Asian | 9 (11.1%) | 1 (2.9%) | 0 | 0 | 10 (7.3%) |
| Southeast Asian | 3 (3.7%) | 0 | 0 | 0 | 3 (2.2%) |
| Unknown | 5 (6.2%) | 1 (2.9%) | 0 | 2 (100%) | 8 (5.8%) |
| Aetiology of liver diseaseb, n (%) | |||||
| Hepatitis B | 13 (16.0%) | 3 (8.8%) | 1 (5.0%) | 0 | 17 (12.4%) |
| Hepatitis C | 48 (59.3%) | 24 (70.6%) | 13 (65.0%) | 0 | 85 (62.0%) |
| Alcohol | 18 (22.2%) | 16 (47.1%) | 11 (55.0%) | 0 | 45 (32.8%) |
| NASH | 6 (7.4%) | 3 (8.8%) | 0 | 1 (50.0%) | 10 (7.3%) |
| Haemochromatosis | 3 (3.7%) | 0 | 1 (5.0%) | 0 | 4 (2.9%) |
| Other/unknown | 3 (3.7%) | 0 | 1a (5.0%) | 1 (50.0%) | 5 (3.6%) |
| Multiple aetiologies, n (%) | |||||
| HBV + HCV | 1 (1.2%) | 0 | 0 | 0 | 1 (0.7%) |
| HCV + alcohol | 7 (8.6%) | 12 (35.3%) | 5 (25.0%) | 0 | 24 (17.5%) |
| HBV + HCV + alcohol | 0 | 0 | 1 (5.0%) | 0 | 1 (0.7%) |
| HCV + haemochromatosis | 2 (2.5%) | 0 | 0 | 0 | 2 (1.5%) |
| Prior treatmentb, n (%) | |||||
| All patients | 24 (29.6%) | 6 (17.6%) | 5 (25.0%) | 1 (50.0%) | 36 (26.3%) |
| RFA | 12 (14.8%) | 2 (5.9%) | 2 (10.0%) | 0 | 16 (11.7%) |
| TACE | 8 (9.9%) | 0 | 1 (5.0%) | 1 (50.0%) | 10 (7.3%) |
| CK | 3 (3.7%) | 0 | 0 | 0 | 3 (2.2%) |
| Resection | 8 (9.9%) | 2 (5.9%) | 0 | 0 | 10 (7.3%) |
| Systemic treatment | 1 (1.2%) | 2 (5.9%) | 2 (10.0%) | 0 | 5 (3.6%) |
Schistosomiasis.
As a result of multiple aetiologies or treatments, sum may be greater than 100%.
NASH, non-alcoholic steatohepatitis; HBV, hepatitis B virus; HCV, hepatitis C virus; RFA, radiofrequency ablation; TACE, transarterial chemoembolization; CK, cyberknife.
Survival after first treatment
Treatment recommendations after the first MTC, the first treatment completed, and survival data are summarized in Table 2. Thirty-six patients (26.3%) had received treatment prior to their first MTC presentation. Patients with no prior treatment survived longer [mean: 603 days, 95% confidence interval (CI) 395–673 days] than those with prior treatment (mean: 368 days, 95% CI 231–471 days), although the difference did not reach statistical significance (P = 0.248). In two-thirds of patients, at least one treatment was recommended at the first discussion. A total of 92 patients (67.2%) received at least one treatment after their initial MTC presentation. Overall, patients who received at least one treatment after their first MTC were more likely to be alive at 1 year after their first treatment than those without treatment (58.7% versus 39.5%; P = 0.043). Notably, patients in whom liver transplantation represented the first treatment achieved 100% survival at 1 year.
Table 2.
First treatment after first presentation at a multidisciplinary tumour conference (MTC) and survival
| Recommended treatment, na | Completed treatment, n (%) | Time from MTC to treatment, days, median | Survival at 1 year after MTC n (%)c | Survival at 1 year after first treatment n (%)c d | |
|---|---|---|---|---|---|
| Liver-directedb | 57 | 66 (48.2%) | 49 | 46 (69.7%) | 44 (66.7%) |
| Resection | 15 | 9 (6.6%) | 28 | 5 (55.6%) | 4 (44.4%) |
| Transplant | 18 | 8 (5.8%) | 398 | 8 (100%) | 8 (100%) |
| Systemic treatment | 12 | 9 (6.6%) | 32 | 5 (55.6%) | 4 (44.4%) |
| No treatment | 47 | 45 (32.8%) | n/a | 16 (35.6%) | NA |
| Any treatment | 88 | 92 (67.2%) | 49 | 64 (69.6%) | 60 (65.2%) |
Sum of recommended treatments may be greater than 100% as a result of multiple treatment recommendations.
Liver-directed therapy includes radiofrequency ablation, transarterial chemoembolization, cyberknife.
Percentage within treatment group.
Assumes those with treatment within 1 year of study end date are alive.
NA, not applicable.
Liver transplantation and the MTC
Of the 137 patients discussed, 43 (31.4%) were listed for liver transplant. A total of 23 patients actually underwent liver transplantation, representing 53.5% of patients listed and 16.8% of all patients discussed. Thirty-two of the 43 patients listed for transplant were listed after their first MTC presentation, and 19 of these patients (59.4%) underwent liver transplantation. Time from first discussion to listing and time from listing to transplantation are summarized in Table 3. None of the 19 transplanted patients had received any treatment prior to their first MTC presentation. However, 13 patients did undergo at least one liver-directed treatment (RFA, n = 12; TACE, n = 4; CK, n = 1) prior to transplantation. For one patient, complications related to the MTC-recommended procedure led to transplantation. In this patient, surgical resection was performed and the postoperative course was complicated by liver failure, resulting in liver transplantation. Remarkably, all of the patients who underwent transplantation were still alive at the conclusion of the study.
Table 3.
Data for patients submitted to transplantation according to multidisciplinary tumour conference (MTC) recommendations
| Patients listed after first MTC, n | Time from first MTC to listing, days, median | Patients successfully transplanted, n | Time from listing to transplant, days, median | |
|---|---|---|---|---|
| Child–Pugh class A | 18 | 134 | 8 | 98 |
| Child–Pugh class B | 11 | 83 | 10 | 156 |
| Child–Pugh class C | 3 | 56 | 1 | 350 |
| Total | 32 | 89.5 | 19 | 142 |
Of the remaining 13 patients listed for liver transplantation after their first MTC presentation, eight did not undergo transplantation for the following reasons: death (n = 2); progression of disease outside the Milan criteria (n = 2); deciding against liver transplantation (n = 1), listed and awaiting transplant (n = 3). The reasons why the remaining five patients did not undergo liver transplantation were multifactorial and related to periods of deactivation and subsequent delisting for substance abuse, non-adherence, worsening of clinical status, progression of HCC, patient choice or a new additional cancer diagnosis.
Concordance with MTC recommendations
A total of 419 discussions of 137 distinct patients took place during the period under study. The recommendations made in MTCs were not followed after 145 discussions of 90 individual patients. Table 4 summarizes this information. There were patient-related reasons for discordance, which included failure to attend for follow-up (n = 24, 16.6%), clinical deterioration (n = 19, 13.1%) and patient preferences (n = 13, 9.0%). Physician-related reasons for deviations from MTC recommendations included the preference of the treating physician (n = 43, 29.7%) and the discovery that the patient was not a candidate for the recommended treatment (n = 37, 25.5%). The top three reasons why these 37 patients were considered not to represent appropriate candidates were that the recommendation was inappropriate for the stage of disease or was contraindicated (n = 18, 48.6%), the intervention was not technically feasible (n = 12, 32.4%), and new clinical information became available and led to a change in the initial MTC plan (n = 7, 18.9%).
Table 4.
Reasons why multidisciplinary tumour conference recommendations were not followed
| Patient-related reasons | Physician-related reasons | Otherc | Totalb n (%) | ||||
|---|---|---|---|---|---|---|---|
| Patient did not follow up | Patient deteriorated | Patient preference | Patient not a candidate | Treating physician preferred alternative | |||
| Child–Pugh class A, n | 14 | 4 | 6 | 20 | 24 | 2 | 70 (48.3%) |
| Child–Pugh class B, n | 5 | 4 | 3 | 12 | 12 | 3 | 39 (26.9%) |
| Child–Pugh class C, n | 4 | 10 | 4 | 5 | 7 | 4 | 34 (23.4%) |
| Child–Pugh class unknown, n | 1 | 1 | 0 | 0 | 0 | 0 | 2 (1.4%) |
| Totala, n (%) | 24 (16.6%) | 19 (13.1%) | 13 (9.0%) | 37 (25.5%) | 43 (29.7%) | 9 (6.2%) | 145 |
Percentage within reason recommendation not followed.
Percentage within Child–Pugh class.
Chart review does not show a clear reason why the recommendation was not followed.
Table 5 summarizes the frequencies with which certain recommendations were not followed. Locoregional procedures as a group, including RFA, TACE and CK, were less likely to be followed. Radiofrequency ablation accounted for half of these locoregional procedures. In only seven cases was the recommendation changed from one locoregional procedure to another (i.e. from RFA to TACE) or an additional locoregional procedure was performed in addition to that originally recommended.
Table 5.
Recommendations not followed
| Recommendation not followed | n (%)a |
|---|---|
| Imaging | 25 (17.2%) |
| Biopsy | 31 (21.4%) |
| Resection | 9 (6.2%) |
| Transplant | 9 (6.2%) |
| Radiofrequency ablation | 31 (21.4%) |
| Transarterial chemoembolization | 15 (10.3%) |
| Cyberknife | 19 (13.1%) |
| Systemic therapy | 16 (11.0%) |
| Other | 8 (5.5%) |
Because of multiple recommendations per multidisciplinary tumour conference, sum may be greater than 100%.
A comparison of those patients in whom all MTC recommendations were followed with those in whom at least one recommendation was not followed shows rates of survival to 1 year after the first MTC presentation of 61.7% and 56.7%, respectively (P = 0.29). Although the difference is not statistically significant, there were trends towards improved survival from first MTC presentation in patients whose treatment adhered to recommendations compared with those whose treatment did not by Child–Pugh class. In patients with Child–Pugh class A status, mean ± SD survival was 610.7 ± 407.6 days in those who adhered and 523.5 ± 340.5 days in those who did not (P = 0.33). In patients with Child–Pugh class B status, mean ± SD survival was 519.6 ± 390.4 days in those who adhered and 474.7 ± 391.7 days in those who did not (P = 0.74). In patients with Child–Pugh class C status, mean ± SD survival was 467.2 ± 542.3 days in those who adhered and 302.7 ± 268.1 days in those who did not (P = 0.37). More patients who followed recommendations underwent liver transplantation (25.6% and 14.4%, respectively; P = 0.10).
Discussion
Hepatocellular carcinoma is the third most common cause of cancer-related death and the most common cause of death among patients with cirrhosis.8,9 In patients with HCC and cirrhosis, liver transplantation represents the most effective treatment option.10 Because the management of patients with HCC is complex, a multidisciplinary approach is crucial.11,12 Increased survival in patients with cirrhosis who develop HCC has been demonstrated in recent years.13 This is likely to in part reflect the imposition of standardized screening guidelines, advances in therapy, and perhaps the tool of interdisciplinary collaboration. As with all therapies for HCC, the function of an MTC requires examination in order to maximize patient benefit and to address any shortcomings.
In this study, the function of a multidisciplinary HCC tumour conference at a tertiary referral centre was examined and the outcomes of patients with HCC and cirrhosis were described. The principle finding of the current study is that in two-thirds of all patients discussed, at least one MTC recommendation was not followed. In fact, one-third of all MTC discussions included recommendations that were not adhered to, a statistic much higher than expected. Secondly, the present study found that there were both patient and physician explanations for the discrepancy, and that locoregional procedures as a group were least likely to be followed. Thirdly, the study showed clinical trends towards improved survival, and an increased likelihood of transplantation when MTC recommendations were followed. This study suggests that an informed, multidisciplinary approach to patients with cirrhosis and HCC is valuable. Future studies with larger sample sizes may help to disprove the null hypothesis.
Patients with no prior treatment survived longer than patients who were treated before their first MTC presentation. There were many reasons for this difference in the present study. Firstly, patients with prior treatment had been diagnosed with HCC for longer than patients with no prior treatment, and therefore their disease may have been more advanced at the time of their first MTC. Secondly, patients with prior treatment had often been referred from outside institutions in order to obtain a second opinion in relation to liver transplantation and hence represented a selected group of medically complex individuals. Lastly, patients with prior treatments were likely to have been subject to treatment decisions made outwith a multidisciplinary setting, which may have contributed to a poorer outcome.
Adherence to MTC decisions is a complex issue. Each patient has unique characteristics, and decisions on observation, additional diagnostics and treatment modalities are not straightforward. Despite initial agreement among specialists at the weekly MTC meetings, many reasons for diverting from the management plan may have arisen. There were often unforeseen aspects of a patient’s clinical trajectory or missing data that led to a change of plan. Patient-related factors that affect adherence, such as personal choice, failure to attend for follow-up and clinical decline, may be unavoidable in some cases but are clearly important areas for improvements in education and patient compliance. Physician-related reasons for non-adherence are also notable and may represent areas for quality improvement. Two of the reasons for discordance between recommendations and actual actions referred to the recommendation being unfeasible and the recommendation being inappropriate or contraindicated for the stage of disease. Whether these problems could have been prevented is speculative but conceivable.
What might account for the discrepancy? Is it an endogenous risk factor such as incomplete knowledge of the clinical aspects of the case or of scientific (i.e. evidence-based) standards? Should there be a standard of clinical data, such as Child–Pugh class or α-fetoprotein trend, to enable the better presentation of a case? Should a citation of evidence-based practice be recorded with each decision made? Is there adequate representation at MTC meetings of treatment providers? Are the laboratory and imaging data for outside referrals presented prior to the patient’s first visit with a new provider? The introduction of new rules that address these concerns might perhaps help to decrease the discrepancy. However, it may be that there are exogenous reasons for discrepancy, such as that too many case discussions take place on a given day and thus the time and attention given to each are insufficient. A risk factor like this is easily remedied. The design of this study does not lend itself to answering all of these queries.
An ‘ideal’ MTC is one that meets regularly to individually review each patient’s case in order to determine a personalized diagnostic and treatment plan. There is a designated chair and a coordinator, who is responsible for conference management. Representatives from each specialty, including hepatology, transplant surgery, medical oncology, radiation oncology, radiology, interventional radiology and nursing, are present at each meeting to provide a complete range of expert opinion about the disease process. Attendance should be mandatory for all clinicians directly involved in the care of the patient being presented. Input should be encouraged from all members of the team, and the outcome of each meeting should be clearly documented in the medical record.
This study brings to attention some imperfections of the MTC. In the present institution, MTC attendance is not perfect and the treating clinician may not be present at all MTC meetings. Outside referrals are sometimes presented at the MTC before the patient has been seen in clinic, and thus the group is not aware of the patient’s functional status or preferences, knowledge of which is essential to making an informed recommendation. In this study, recommendations for locoregional procedures were least likely to be followed. The interventional radiologist performing the procedure may not be the physician who was present at the MTC meeting. Policies that mandate attendance by treating providers, discussion only after initial patient evaluation, and scheduling of locoregional treatment by the interventional radiologist present for the MTC discussion may limit this discordance. In situations in which the MTC recommendation is found to be unfeasible or inappropriate, the treating clinician often determines the next appropriate treatment or waits until the patient’s status improves to provide the recommended treatment. Strict rules should be created to ensure that patients under these circumstances are represented in a timely fashion at the next MTC meeting. This intervention would also serve as quality improvement for the MTC so that the group can be made more aware of these situations.
The role of the MTC in liver transplantation is also important because transplantation represents the best cure for patients with cirrhosis and HCC. By having an instrument such as the MTC that functions to bring together HCC specialists, newly diagnosed cases of HCC can be discussed in a timely manner, and suggestions regarding appropriate follow-up, further testing and treatment can be made. Furthermore, the coordination of the care necessary to complete a transplant workup of those patients who do meet the criteria can be put into place promptly to enable these patients to be listed. Once a patent has been listed for transplant, liver-directed bridging therapies are important to consider, especially in patients who are expected to experience a prolonged wait time.14–17 The MTC represents an opportunity to review each case routinely with all of the specialists involved in order to develop the best personalized treatment plan. When all of these variables work together, patients should do better, but external validation from other MTC groups is needed.
The present study has some limitations. Firstly, it represents a single-centre experience with a regional and small population, which may diminish the generalizability of the results. Future studies should combine data from multiple referral centres. This study may also be subject to self-selection bias in that patients who are more motivated are more likely to follow MTC recommendations and do better. In addition, this study is retrospective and data collection was limited by the documentation available in the OMR.
Multidisciplinary collaboration among physicians in the management of patients with HCC has been previously shown to improve patient survival.18 The present data suggest an insignificant trend towards improved survival and transplantation when management recommendations are carried out. Larger multicentre studies examining the function of an MTC are needed. The defining of physician-related reasons for non-adherence to MTC recommendations will make it possible to work towards developing and implementing strategies to minimize discordance and impact on patient survival.
Conflicts of interest
None declared.
References
- El-Serag HB. Hepatocellular carcinoma. N Engl J Med. 2011;365:1118–1127. doi: 10.1056/NEJMra1001683. [DOI] [PubMed] [Google Scholar]
- Maggs JR, Suddle AR, Aluvihare V, Heneghan MA. Systematic review: the role of liver transplantation in the management of hepatocellular carcinoma. Aliment Pharmacol Ther. 2012;35:1113–1134. doi: 10.1111/j.1365-2036.2012.05072.x. [DOI] [PubMed] [Google Scholar]
- Colella G, Bottelli R, De Carlis L, Sansalone CV, Rondinara GF, Alberti A, et al. Hepatocellular carcinoma: comparison between liver transplantation, resective surgery, ethanol injection, and chemoembolization. Transpl Int. 1998;11(Suppl. 1):193–196. doi: 10.1007/s001470050459. [DOI] [PubMed] [Google Scholar]
- Huang J, Yan L, Cheng Z, Wu H, Du L, Wang J, et al. A randomized trial comparing radiofrequency ablation and surgical resection for HCC conforming to the Milan criteria. Ann Surg. 2010;252:903–912. doi: 10.1097/SLA.0b013e3181efc656. [DOI] [PubMed] [Google Scholar]
- Margarit C, Escartín A, Castells L, Vargas V, Allende E, Bilbao I. Resection for hepatocellular carcinoma is a good option in Child-Turcotte-Pugh class A patients with cirrhosis who are eligible for liver transplantation. Liver Transpl. 2005;11:1242–1251. doi: 10.1002/lt.20398. [DOI] [PubMed] [Google Scholar]
- Chok KS, Ng KK, Poon RT, Lam CM, Yuen J, Tso WK, et al. Comparable survival in patients with unresectable hepatocellular carcinoma treated by radiofrequency ablation or transarterial chemoembolization. Arch Surg. 2006;141:1231–1236. doi: 10.1001/archsurg.141.12.1231. [DOI] [PubMed] [Google Scholar]
- Farinati F, Sergio A, Baldan A, Giacomin A, Di Nolfo MA, Del Poggio P, et al. Early and very early hepatocellular carcinoma: when and how much do staging and choice of treatment really matter? A multi-centre study. BMC Cancer. 2009;9:33. doi: 10.1186/1471-2407-9-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forner A, Llovet JM, Bruix J. Hepatocellular carcinoma. Lancet. 2012;379:1245–1255. doi: 10.1016/S0140-6736(11)61347-0. [DOI] [PubMed] [Google Scholar]
- Cabrera R, Nelson DR. Review article: the management of hepatocellular carcinoma. Aliment Pharmacol Ther. 2010;31:461–476. doi: 10.1111/j.1365-2036.2009.04200.x. [DOI] [PubMed] [Google Scholar]
- Mazzaferro V, Regalia E, Doci R, Andreola S, Pulvirenti A, Bozzetti F, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996;334:693–699. doi: 10.1056/NEJM199603143341104. [DOI] [PubMed] [Google Scholar]
- Sangiovanni A, Del Ninno E, Fasani P, De Fazio C, Ronchi G, Romeo R, et al. Increased survival of cirrhotic patients with a hepatocellular carcinoma detected during surveillance. Gastroenterology. 2004;126:1005–1014. doi: 10.1053/j.gastro.2003.12.049. [DOI] [PubMed] [Google Scholar]
- Christians KK, Pitt HA, Rilling WS, Franco J, Quiroz FA, Adams MB, et al. Hepatocellular carcinoma: multimodality management. Surgery. 2001;130:554–559. doi: 10.1067/msy.2001.117106. ; discussion 559–560. [DOI] [PubMed] [Google Scholar]
- Rilling WS, Drooz A. Multidisciplinary management of hepatocellular carcinoma. J Vasc Interv Radiol. 2002;13(9 Pt 2):259–263. doi: 10.1016/s1051-0443(07)61794-1. ) (Suppl.): [DOI] [PubMed] [Google Scholar]
- DuBay DA, Sandroussi C, Kachura JR, Ho CS, Beecroft JR, Vollmer CM, et al. Radiofrequency ablation of hepatocellular carcinoma as a bridge to liver transplantation. HPB. 2011;13:24–32. doi: 10.1111/j.1477-2574.2010.00228.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heckman JT, Devera MB, Marsh JW, Fontes P, Amesur NB, Holloway SE, et al. Bridging locoregional therapy for hepatocellular carcinoma prior to liver transplantation. Ann Surg Oncol. 2008;15:3169–3177. doi: 10.1245/s10434-008-0071-3. [DOI] [PubMed] [Google Scholar]
- Belghiti J, Carr BI, Greig PD, Lencioni R, Poon RT. Treatment before liver transplantation for HCC. Ann Surg Oncol. 2008;15:993–1000. doi: 10.1245/s10434-007-9787-8. [DOI] [PubMed] [Google Scholar]
- Mazzaferro V, Battiston C, Perrone S, Pulvirenti A, Regalia E, Romito R, et al. Radiofrequency ablation of small hepatocellular carcinoma in cirrhotic patients awaiting liver transplantation: a prospective study. Ann Surg. 2004;240:900–909. doi: 10.1097/01.sla.0000143301.56154.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang TT, Sawhney R, Monto A, Davoren JB, Kirkland JG, Stewart L, et al. Implementation of a multidisciplinary treatment team for hepatocellular cancer at a Veterans Affairs Medical Center improves survival. HPB. 2008;10:405–411. doi: 10.1080/13651820802356572. [DOI] [PMC free article] [PubMed] [Google Scholar]


