Abstract
Background
This study provides new information on how rapidly and extensively alcohol is absorbed following Roux-en-Y Gastric Bypass (RYGB). Prior alcohol pharmacokinetic research in RYGB patients has not reported blood alcohol concentrations in this early time-period following ingestion.
Objectives
The objective of this study was to examine the rate and extent of alcohol absorption, particularly in the first ten minutes following a dose of alcohol.
Setting
The study was conducted at a nonprofit research organization within the United States.
Methods
Five female participants who had undergone RYGB three to four years prior completed the study. Participants were given 0.3 grams/kilogram of actual body weight of ethanol. Following the dose of alcohol, blood samples were collected through an indwelling intravenous catheter every minute for the first five minutes and at 7.5, 10, 20, and 60 minutes.
Results
The observed mean Cmax was 138.4 ± 28.6 mg/dl (range 98.0–170.0 mg/dl) and the observed mean Tmax was 5.4 ± 3.1 minutes (range 2–10 minutes) following alcohol consumption.
Conclusions
Within minutes following consumption of a beverage containing a modest amount of alcohol, post-RYGB patients achieve disproportionately high blood alcohol concentrations. All five patients in this study reached blood alcohol concentrations above 0.08%, the legal driving limit in the United States, within ten minutes following a dose of alcohol. Clinicians are encouraged to educate patients about the marked changes in alcohol pharmacokinetics that are they are likely to experience post-RYGB and to guide patients in making modifications to alcohol intake following surgery accordingly.
Keywords: alcohol, gastric bypass, pharmacokinetics, absorption
INTRODUCTION
Patients who undergo Roux-en-Y Gastric Bypass (RYGB) may be at increased risk of an alcohol use disorder post-surgery(1,2,3). One theoretical contributor to this phenomenon may be the alterations in the pharmacokinetics (PKs) of alcohol that have been reported following RYGB. It is known that substances which reach peak concentrations more rapidly are associated with higher addictive potential(4,5). The current study extends the prior alcohol PK literature by examining the rate and extent of alcohol absorption post-RYGB. These data may have implications for alcohol use disorders following RYGB as well as for patient safety and education following surgery.
Alterations in alcohol PK post-RYGB have been reported relative to pre-surgery(6) and to nonsurgical comparison groups(7,8). Data have consistently shown higher maximum alcohol concentrations in patients who are post-RYGB. Data with other bariatric procedures is more limited. A recent study found that alcohol metabolism is unaltered in patients who underwent gastric banding or sleeve gastrectomy(9) although an earlier study found higher alcohol levels and altered metabolism following sleeve gastrectomy(10). Following RYGB, there may be a reduction in first-pass metabolism through a decrease in stomach alcohol dehydrogenase(7). A more probable explanation is the reduced stomach volume and acceleration in gastric emptying time following surgery lead to rapid, extensive absorption from the jejunum(7).
Klockhoff and colleagues(7) found that RYGB patients achieved a faster and higher blood alcohol concentration (BAC) relative to controls. However, the first BAC measurement in their study occurred at 10 minutes post-drink and other studies involving RYGB patients have similarly first measured BAC at 10–15 minutes post-drink(6,8). Generally, the first measurement time-point in these studies has corresponded with the maximum alcohol concentration (Cmax). Observations from research in our lab suggested that prior studies may have measured BAC too late to capture the actual Cmax following RYGB. We designed the current study to test our hypothesis that in RYGB patients, the Cmax would be significantly higher, and the time to Cmax (Tmax) would be faster, following alcohol ingestion than previous research has reported.
MATERIALS and METHODS
This study was Institutional Review Board approved. Five participants completed the study who underwent RYGB surgery within the past 18–60 months, were 21–65 years of age, had a body mass index (BMI) of ≥ 18.5kg/m2 and regularly consumed alcohol (≥ one standard drink ≥ once/month on average in the past three months) without significant adverse effects. Participants could be excluded for several reasons, most commonly including: 1) medical or psychiatric contraindication to receiving a dose of alcohol or 2) medication which inhibits gastric alcohol dehydrogenase (H2 antagonist, aspirin).
Participants who qualified on telephone interview were invited to the research facility for a screening appointment. All participants provided written Informed Consent before undergoing screening procedures, which included a history and physical, vital signs, height and weight, serum pregnancy, glucose, and hepatic tests, and a urine toxicology screen.
The alcohol dose and administration protocol used in this study replicates the approach used by Klockhoff and colleagues7. Participants were asked to fast for a minimum of four hours prior to coming to the laboratory. Each participant consumed 0.3 grams of ethanol per kilogram of body weight. The alcohol was administered in the form of 40% vodka, which contains 14 grams of ethanol per 1.5 ounces (~45 ml). Vodka was mixed with orange juice in a 1:1 ratio to yield a 50% v/v concentration. Participants were instructed to consume the drink evenly over five minutes.
Blood was obtained through an intravenous catheter to facilitate rapid collection of specimens. Blood was collected on 9 occasions; at 1, 2, 3, 4, 5, 7.5, 10, 20 and 60 minutes after ingesting the full dose of alcohol. Participants were allowed to leave the facility when BAC obtained by breathalyzer was ≤ 0.01%.
Sanford Health Systems’ performed BAC quantification. BAC was determined through a colorimetric assay using the VITROS Chemistry Products Calibrator Kit 8 with quantification limits of 10mg/dl-600 mg/dl. PASW Statistics 18 was used to generate descriptive demographic and PK data. Area under the concentration-time curve (AUC) from 0–60 minutes (AUC0–60) was calculated using the linear trapezoidal method. Observed Cmax and Tmax data are presented.
RESULTS
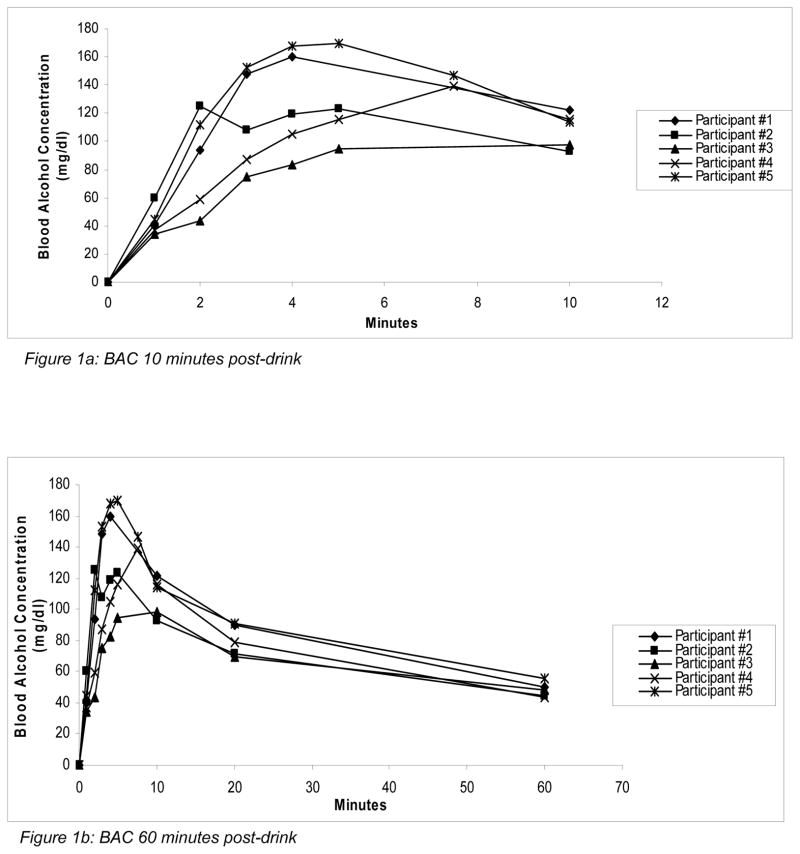
Participant demographics and PK values can be found in Table 1. The mean dose of ethanol given was 26.9 ± 2.3 grams (mean of ~86 mL vodka). The mean observed Cmax was 138.4 ± 28.6 mg/dl (range 98–170 mg/dl). The mean observed Tmax was 5.4 ± 3.1 minutes (range 2–10 minutes). At one minute post-drink, mean BAC was 43.4 ± 10.2 mg/dl and by two minutes the group reached a mean BAC of 86.8 ± 34.5 mg/dl, which is over the legal driving limit in the United States. Figures 1a and 1b depict the BACs in 10 and 60 minutes post-drink, respectively.
Table 1.
Demographics and Pharmacokinetics
| Mean ± SD | Range | ||
|---|---|---|---|
| Demographics | Age (years) | 40.8 ± 5.8 | 35 – 48 |
| Female (N=5, 100%) | --- | --- | |
| Years post-RYGB | 3.5 ± .31 | 3.2 – 4.0 | |
| Height (inches) | 64.2 ± 5.2 | 55 – 67 | |
| Weight (kg) | 89.6 ± 7.5 | 78.4 – 97.7 | |
| BMI (kg/m2) | 31.6 ± 2.1 | 28.7 – 33.7 | |
| Pre-surgery weight (kg) | 125.8 ± 11.1 | 110.5 ± 138.6 | |
|
| |||
| Pharmacokinetics | Dose of alcohol (gm) | 26.9 ± 2.3 | 23.5 – 29.3 |
| Cmax (mg/dl) | 138.4 ± 28.6 | 98.0 – 170.0 | |
| Tmax (min) | 5.4 ± 3.1 | 2 –10 | |
| AUC0–60min (mg/dl x min)* | 4574.1 ± 569.9 | 3965.8 – 5269.5 | |
|
| |||
| BAC mg/dL (minutes post-drink) | 1 | 43.4 ± 10.2 | 34.0 – 60.0 |
| 2 | 86.8 ± 34.5 | 44.0 –125.0 | |
| 3 | 114.2 ± 35.2 | 75.0 –153.0 | |
| 4 | 127.0 ± 36.2 | 83.0 –168.0 | |
| 5 | 126.0 ± 31.7 | 95.0 –170.0 | |
| 7.5 (N=2) | 143.0 ± 5.7 | 139.0 –147.0 | |
| 10 | 108.6 ± 12.4 | 93.0 –122.0 | |
| 20 | 80.2 ± 10.0 | 70.0–91.0 | |
| 60 | 48.6 ± 4.8 | 44.0 – 56.0 | |
0 time-point in AUC calculation confirmed by Breathalyzer assessment before the dose was administered. All other alcohol concentrations obtained from blood.
Figure 1.
Figure 1a: BAC 10 minutes post-drink
Figure 1b: BAC 60 minutes post-drink
DISCUSSION
Consistent with prior literature, the results of our study show that patients who have undergone RYGB rapidly achieve disproportionately high BAC concentrations in response to a modest amount of alcohol. As hypothesized, our data show that prior literature has underestimated the time and extent to which patients who’ve undergone RYGB may become intoxicated following alcohol ingestion.
The average dose of alcohol administered in this study equated to approximately 63 ml vodka for a 70 kg individual, with a mean dose of ~86 mL (roughly two standard 45 ml “shots”) administered. The mean Cmax observed in this study (1.384 ± 0.286 g/l) was approximately double the mean Cmax (0.741 ± 0.221 g/l) reported by Klockhoff and colleagues(7). In our study, Tmax ranged from 2–10 minutes post-drink (mean 5.4 ± 3.1 minutes) whereas the median Tmax was ten minutes in the study by Klockhoff and colleagues(7) which was the first measurement time.
CONCLUSION
All five participants achieved substantially exceeded the legal driving limit of 80 mg/dl (0.08%) within minutes following a dose of alcohol that should, under normal circumstances, produce a BAC significantly under 0.08% in individuals who have not undergone RYGB. Clinicians should educate patients to modify alcohol intake accordingly and to avoid engaging in potentially hazardous activities after drinking.
Acknowledgments
Supported by NIH Grants: 1R03AA019573-02, 1K23DK085066-03.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Conason A, Teixeira J, Hsu CH, Puma L, Knafo D, Geliebter A. Substance use following bariatric weight loss surgery. Arch Surg. 2012;15:1–6. doi: 10.1001/2013.jamasurg.265. [DOI] [PubMed] [Google Scholar]
- 2.King WC, Chen JY, Mitchell JE, et al. Prevalence of alcohol use disorders before and after bariatric surgery. JAMA. 2012;307(23):2516–25. doi: 10.1001/jama.2012.6147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Suzuki J, Haimovici F, Chang G. Alcohol use disorders after bariatric surgery. Obes Surg. 2012;22(2):201–7. doi: 10.1007/s11695-010-0346-1. [DOI] [PubMed] [Google Scholar]
- 4.Longo LP, Johnson B. Addiction: Part 1. Benzodiazepines-side effects, abuse risk and alternatives. Am Fam Physician. 2000;61:2121–28. [PubMed] [Google Scholar]
- 5.National Institute on Drug Abuse. DrugFacts: Cocaine. 2010 Retrieved September 2012 at: http://www.drugabuse.gov/publications/drugfacts/cocaine.
- 6.Woodard GA, Downey J, Hernandez-Boussard T, Morton JM. Impaired alcohol metabolism after gastric bypass surgery: a case-crossover trial. J Am Coll Surg. 2011;212(2):209–14. doi: 10.1016/j.jamcollsurg.2010.09.020. [DOI] [PubMed] [Google Scholar]
- 7.Klockhoff H, Naslund I, Jones AW. Faster absorption of ethanol and higher peak concentration in women after gastric bypass surgery. Br J Clin Pharmacol. 2002;54(6):587–91. doi: 10.1046/j.1365-2125.2002.01698.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hagedorn JC, Encarnacion B, Brat GA, Morton JM. Does gastric bypass alter alcohol metabolism? Surg Obes Relat Dis. 2007;3(5):543–8. doi: 10.1016/j.soard.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 9.Changchein EM, Woodard GA, Hernandez-Boussard T, Morton JM. Normal alcohol metabolism after gastric banding and sleeve gastrectomy: a case-cross-over trial. J Am Coll Surg. 2012;215(4):475–9. doi: 10.1016/j.jamcollsurg.2012.06.008. [DOI] [PubMed] [Google Scholar]
- 10.Maluenda F, Csendes A, De Aretxabala X, et al. Alcohol absorption modification after alaparoscopic sleeve gastrectomy due to obesity. Obes Surg. 2010;20(6):744–8. doi: 10.1007/s11695-010-0136-9. [DOI] [PubMed] [Google Scholar]