Abstract
A 17-year-old young girl was seen by us with complaints of progressive, painless decreasing vision in one eye for the last 4 years. No other supporting history could be elucidated. On examination, a large choroidal mass was found. Since the features were suggestive of malignant melanoma of the choroid, an enucleation of the eye was performed. Subsequently, histopathological examination of the enucleated eye revealed findings consistent with melanocytoma of the choroid. This case is unique in that the patient was of relatively young age and the tumor was huge compared to previous such reports.
Keywords: Melanocytoma, Choroid, Enucleation
Introduction
Intraocular melanocytomas are relatively rare, benign, tumors. They are usually diagnosed in patients between the ages of 30 and 50 years.1 Commonly occurring near or on the optic disk, they have also been reported to develop in the choroid, ciliary body, iris, conjunctiva or sclera.2–5 The differential diagnosis of melanocytomas includes a number of conditions such as malignant melanoma, nevi, hyperplasia of the retinal pigmentary epithelium (RPE) and hamartomas of the RPE/sensory retina.6 Unfortunately, melanocytomas may clinically and/or radiologically mimic malignant melanomas, leading to drastic procedures such as enucleation.7,8
This case report describes a 17 year old girl who was found to have a huge intraocular tumor on initial presentation. The clinical examination and subsequent investigations pointed to the possibility of a malignant melanoma. Thus, an enucleation was performed. However, on subsequent histopathological examination, it was found to be a benign melanocytoma.
Thus, this case is a pointer that proper diagnosis of benign intraocular tumors can lead to a more conservative approach. This can avoid unnecessary enucleations and thereby protect the quality of life in a young individual from being considerably affected.
Case report
A 17-year-old female reported to the ophthalmology clinic of Queen Elizabeth Hospital, Kota Kinabalu, Malaysia, with complaints of progressive decreasing vision in the right eye for the past 4 years. There was no pain, redness or swelling noticed in or around the eye. The patient also denied any history of trauma or other systemic symptoms such as weight loss or headaches. No other supporting history could be elicited.
Ocular examination revealed a visual acuity of no-perception-to-light in the right eye and 6/6 in the left eye. Intra-ocular pressures were 18 mm Hg in right eye and 14 mm Hg in the left eye. The anterior segment in the right eye showed a mid-dilated and non-reacting pupil. The iris was normal in appearance with no evidence of rubeosis iridis. A retrolental brownish mass with overlying blood vessels could be seen on slit-lamp biomicroscopy (Fig. 1a). No orange pigments or drusens were visible on the tumor. The anterior segment examination of the left eye did not reveal any abnormality. Gonioscopically, both eyes showed open angles.
Figure 1.
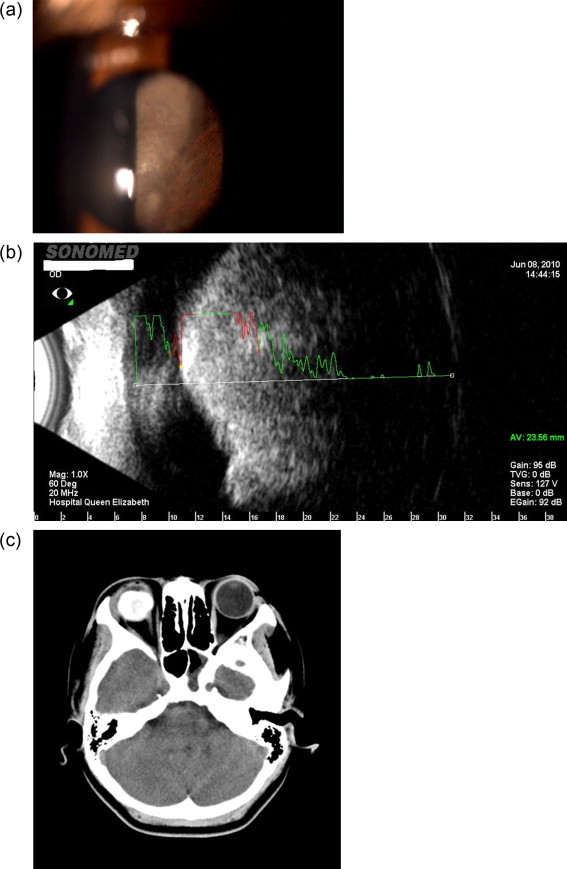
(a) Slit-lamp image of the right eye, showing the retrolental tumor. (b) Ultrasound image showing the huge choroidal tumor, with areas of high internal reflectivity. (c) CT-scan image shows the 12mm × 20 mm intraocular tumor without any extension.
Fundus examination of the right eye showed a large brownish mass occupying most of the posterior segment except for the nasal periphery. The tumor was large enough to obscure most of the fundal details and it could not be ascertained if the tumor was arising from a juxtapapillary location. The posterior segment of the left eye was within normal limits.
A B-scan ultrasonography of the right eye revealed a large choroidal, dome-shaped mass, without sub-retinal fluid, arising from the posterior pole without any acoustic hollowing or calcification. High internal reflectivity was observed in some parts of the tumor (Fig. 1b). Subsequently, a CT (Computerized Tomography)-scan of the orbit reported a large intraocular hyperdense mass measuring 20 mm × 12 mm, occupying most of the posterior segment (Fig. 1c). No scleral invasion was noted. A CT-scan of the brain, chest X-ray and an ultrasound of the liver did not reveal any signs suggestive of metastasis. The full blood count, erythrocyte sedimentation rate, hepatic and renal functions were also within normal limits.
The clinical appearance was suggestive of a choroidal melanoma (young age, large tumor). However, the B-scan and CT scan findings were equivocal. Subsequently, the patient was counseled for enucleation, for which she consented. Subsequently, an enucleation of the right eye with Medpor (Stryker Co., USA) implantation was uneventfully done.
The enucleated eye was sent for histopathological examination (Fig. 2a–c) which reported a brownish-black pigmented tumor arising from the choroid. Bleaching of tissue demonstrated uniformly large, round to polygonal cells with small nuclei. These are the inactive or benign Type 1 cells. This appearance was consistent with a choroidal melanocytoma and not a choroidal melanoma which was suspected on clinical examination, B-scan and CT-scan findings.
Figure 2.
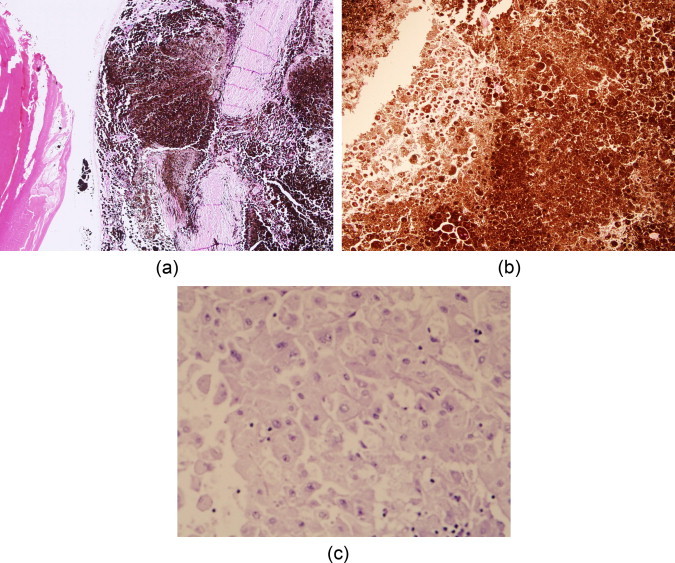
(a) A 4× high-power magnification through the lens and the black pigmented tumor. (b) A 20× examination shows cells with heavily pigmented cytoplasm obscuring the visualization of nuclei. (c) A 40× examination after permanganate bleaching shows large, uniform, polygonal cells with distinct cytoplasmic membranes, abundant cytoplasm and centrally placed small round nuclei which are cytologically bland, with inconspicuous nucleoli.
The patient was implanted with a prosthesis 6 weeks after the enucleation. Subsequently, she has been followed up regularly for the past 4 years without recurrence of any tumors.
Discussion
Intraocular melanocytomas are rare, benign tumors. They were first described by Zimmerman. However, later he agreed that the term was non-specific and credited Cogan for recommending the term Magnocellular Nevus in its place.9 Recently, Shields proposed the term Hyperpigmented Magnocellular Nevus.10 In a study of iris and ciliary body lesions only 5% specimens were found to be of melanocytomas.11 A review of literature reported about a dozen cases of choroidal melanocytomas published so far.1
Choroidal melanocytomas can also form a part of paraneoplastic syndromes (super nevus syndrome or bilateral diffuse uveal melanocytic proliferation syndrome). In such a condition, they tend to be very dark, multiple, occur bilaterally and may grow rapidly. This is unlike melanocytomas in other situations, where mild growth is seen in 10–15% cases.12,13 Choroidal melanocytomas are also reported not to exceed 1 disk diameter in size.14 In this regard, our patient is unusual in that she had a very large tumor.
Melanocytomas have been observed to have high levels of internal reflectivity on B-scan ultrasonography.6 However, this is not a characteristic feature. Haas reported a patient of choroidal melanocytoma who had relatively low levels of internal reflectivity.15 In our case; ultrasonography demonstrated a large choroidal mass without any acoustic hollowing and areas of high internal reflectivity. In comparison, a malignant melanoma has low internal reflectivity but is more vascular compared to melanocytomas.3
Melanocytomas and benign pigmented tumors are dense and relatively avascular. Thus, they usually give rise to blocked background choroidal fluorescence on fundus fluorescein angiography (FFA). However, some reports have shown that these tumors can also develop vascularization, though less frequently compared to melanomas. Thus, benign and malignant lesions should not be differentiated on the basis of FFA findings alone.16–18 In our patient, the tumor was too large in size to consider for FFA.
Histologically, melanocytomas are characterized by abundant cytoplasmic pigments which obscure the nuclear features. Bleached sections disclose large, uniform cells with a distinct cytoplasmic membrane, abundant cytoplasm with a rounded, small, bland-appearing nucleus which may or may not have an inconspicuous nucleolus.1,11
Ultrastructural studies of melanocytomas have shown 2 types of melanocytoma cells. The Type 2 melanocytoma cells contain small melanosomes and are considered more metabolically active than Type 1 cells. The Type 2 cells are supposedly responsible for growth of the tumor and invasion of surrounding structures.3
Histopathological examination of the specimen in our case demonstrated uniformly large, round to polygonal cells with small nuclei. This appearance was consistent with the diagnosis of melanocytoma.
Some authors have pointed out that the gross appearance of the lesion, ultrasonography, FFA and P32 uptake may neither be specific nor sensitive to detect melanocytomas. Thus, these patients often end up with drastic procedures such as enucleation or exentration.11,18,19
As these tumors usually do not affect vision, are slow growing and rarely undergo malignant transformation review of the patients can be done at 3 monthly intervals initially and yearly thereafter.20 Melanocytomas can undergo spontaneous necrosis causing inflammation and pain. They can also cause vasoocclusion, especially at the optic disk with the development of neovascular glaucoma. Other potential complications of melanocytomas include ischemic retinopathy and melanocytic glaucoma from pigment dispersion.3,21
When less than 3 clock hours of iris or ciliary body are involved, local resection of the tumor is technically possible.11 Melanocytomas can be excised, if required, by lifting a partial-thickness scleral flap backward, doing an irido-cyclectomy, often combined with a lensectomy. However, most often the diagnosis is unconfirmed and the eye is enucleated fearing a malignant lesion.22 As in this case, it is only post-operatively that a histopathological examination reveals a melanocytoma.
In our patient, the gross features of malignant tumors such as subretinal fluid and orange lipofuscin pigment were absent. Although some recent reports suggest these findings are non-specific and could be present in both benign and malignant tumors. However, the size of the tumor and other radiologic features did not suggest a melanocytoma. Thus, an enucleation was performed.
This patient is unique in having a choroidal melanocytoma at an early age in her teens. Secondly, the tumor is relatively large in size and showed some features suggestive of malignant melanoma. Thus, though rare, melanocytomas should be considered in the differential diagnosis of uveal tract or optic disk tumors. A conservative approach can have a sight saving effect and allow a stable quality of life for the patient.
Conflict of interest
The authors declared that there is no conflict of interest.
References
- 1.Xiao Z., Rong-ping D., Wei-Jing C., Fong-tian D. Atypical presentations of choroidal melanocytoma. Chin Med J. 2009;122:1238–1240. [PubMed] [Google Scholar]
- 2.Kurli M., Finger P.T., Manor T., McCormick S.A., Grossniklaus H.E. Finding malignant change in a necrotic choroidal melanocytoma: a clinical challenge. Br J Ophthalmol. 2005;89:921–922. doi: 10.1136/bjo.2004.060038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mohamed M.D., Gupta M., Parsons A., Rennie I.G. Ultrasound biomicroscopy in the management of melanocytoma of the ciliary body with extrascleral extension. Br J Ophthalmol. 2005;89:14–16. doi: 10.1136/bjo.2004.048967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim M., Lee S.J. Melanocytoma of the ciliary body misdiagnosed as iridodialysis. Clin Ophthalmol. 2014;29(8):1051–1053. doi: 10.2147/OPTH.S63328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sharma H., Puri L.R. Melanocytoma of the optic disc – a case report. Nepal J Ophthalmol. 2012;4:323–325. doi: 10.3126/nepjoph.v4i2.6553. [DOI] [PubMed] [Google Scholar]
- 6.Gologorsky D., Schefler A.C., Ehlies F.J., Raskauskas P.A., Pina Y., Williams B.K. Clinical imaging and high-resolution ultrasonography in melanocytoma management. Clin Ophthalmol. 2010;4:855–859. doi: 10.2147/opth.s11891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Odashiro M., Odashiro A., Leite L., Melo M., Odashiro P., Miiji L. Melanocytoma of ciliary body and choroids simulating melanoma. Pathol Res Pract. 2010;206:130–133. doi: 10.1016/j.prp.2009.03.006. [DOI] [PubMed] [Google Scholar]
- 8.Shammas H.J., Minckler D.S., Hulquist R., Sherins R.S. Melanocytoma of the ciliary body. Ann Ophthalmol. 1981;13:1381–1383. [PubMed] [Google Scholar]
- 9.Zimmerman L.E., Garron L.K. Melanocytoma of the optic disc. Int Ophthalmol Clin. 1962;2:431–440. [Google Scholar]
- 10.Shields J.A., Font R.L. Melanocytoma of the choroid clinically simulating a malignant melanoma. Arch Ophthalmol. 1972;87:396–400. doi: 10.1001/archopht.1972.01000020398006. [DOI] [PubMed] [Google Scholar]
- 11.Raichand M., Peyman G.A., Juarez C.P., Seetner A.A., Sugar J., Goldberg M.F. Resection of uveal melanocytoma: clinicopathological correlation. Br J Ophthalmol. 1983;67:236–243. doi: 10.1136/bjo.67.4.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yu S., Ikeda T., Ikeda N., Mimura O., Sato K. Coloration of fundus lesions in bilateral diffuse uveal melanocytic proliferation. Jpn J Ophthalmol. 2003;47:612–615. doi: 10.1016/j.jjo.2003.09.003. [DOI] [PubMed] [Google Scholar]
- 13.Robertson D.M., Campbell R.J., Salomão D.R. Mushroom-shaped choroidal melanocytoma mimicking malignant melanoma. Arch Ophthalmol. 2002;120:82–85. [PubMed] [Google Scholar]
- 14.Al-Rasheed S., Abboud E.B., Nowilaty S.R. Characteristics of optic disc melanocytomas presenting with visual dysfunction. Middle East Afr J Ophthalmol. 2010;17:242–245. doi: 10.4103/0974-9233.65488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Haas B.D., Jakobeic F.A., Iwamoto T., Cox M., Bernacki E.G., Pokorny K.L. Diffuse choroidal melanocytoma in a child. A lesion extending the spectrum of melanocytic hamartomas. Ophthalmology. 1986;93:1632–1638. doi: 10.1016/s0161-6420(86)33519-x. [DOI] [PubMed] [Google Scholar]
- 16.Rubin M.L. Disciform lesion overlying melanocytoma simulating progression of choroidal melanoma. Trans Am Ophthalmol Soc. 1976;74:282–294. [PMC free article] [PubMed] [Google Scholar]
- 17.Singh P., Singh A. Choroidal melanoma. Oman J Ophthalmol. 2012;5:3–9. doi: 10.4103/0974-620X.94718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gahankari M.D., Jehangir R., Bhatti S.S. Melanocytoma of the optic disc. J Postgrad Med. 1992;38:135–136. [PubMed] [Google Scholar]
- 19.Khadem J.J., Weiter J.J. Melanocytomas of the optic nerve and uvea. Int Ophthalmol Clin. 1997;37:149–158. doi: 10.1097/00004397-199703740-00013. [DOI] [PubMed] [Google Scholar]
- 20.Melanocytoma-Choroidal. <www.opticiaonline.net/wp-content/uploads/importedimages/az78.pdf> [accessed on 01.12.14].
- 21.Awaji S., Alkatan H., Al-Kharashi S., Al-Rajhi A. Iris melanocytoma in child diagnosed by fine needle aspiration biopsy. Saudi J Ophthalmol. 2013;27:277–280. doi: 10.1016/j.sjopt.2013.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee C.S., Kim do K., Lee S.C. A case of ciliary body melanocytoma presenting as a painful iris mass. Korean J Ophthalmol. 2010;24:44–46. doi: 10.3341/kjo.2010.24.1.44. [DOI] [PMC free article] [PubMed] [Google Scholar]


