Abstract
Background
The growing number of people living with HIV/AIDS (PLWHA) in China points to an increased need for case management services of HIV/AIDS. This study sought to explore the challenges and enablers in shifting the HIV/AIDS case management services from Centers for Disease Control and Prevention (CDCs) to Community Health Service Centers (CHSCs) in urban China.
Methods
A qualitative method based on the Health Policy Triangle (HPT) framework was employed to gain in-depth insights into four elements of the task shifting strategy. This included a review on published literature and health policy documents, 15 focus group discussions (FGDs) and 30 in-depth interviews (IDIs) with four types of key actors from three cities in China. A total of 78 studies and 17 policy files at the national, municipal and local levels were obtained and reviewed comprehensively. Three semi-structured interview guides were used to explore key actors’ views on shifting the HIV/AIDS case management services to CHSCs.
Results
It is necessary and feasible for CHSCs to engage in case management services for PLWHA in local communities. The increasing number of PLWHA and shortage of qualified health professionals in CDCs made shifting case management services downwards to CHSCs an urgent agenda. CHSCs’ wide distribution, technical capacity, accessibility and current practice enabled them to carry out case management services for PLWHA. However our findings indicated several challenges in this task shifting process. Those challenges included lack of specific policy and stable financial support for CHSCs, inadequate manpower, relatively low capacity for health service delivery, lack of coordination among sectors, PLWHA’s fear for discrimination and privacy disclosure in local communities, which may compromise the effectiveness and sustainability of those services.
Conclusions
Shifting the HIV/AIDS case management services from CDCs to CHSCs is a new approach to cope with the rising number of PLWHA in China, but it should be implemented alongside with other efforts and resources such as increasing public funding, planned team building, professional training, coordination with other sectors and education on privacy protection as well as non-discrimination to make this approach more effective and sustainable. Policy makers need to ensure both political feasibility and resources accessibility to facilitate this shifting process.
Keywords: Task shifting, Community Health Service Center, Policy analysis, HIV/AIDS
Background
The number of people living with HIV/AIDS (PLWHA) was estimated 780 000 in China as of 2011, among which approximately 154 000 had developed AIDS [1]. Since the launch of the national free Antiretroviral Treatment (ART) program in 2003, China has achieved impressive ART coverage. By the end of 2011, a total of 122 613 individuals had been receiving ART, accounting for 79.6 % of the total estimated eligible AIDS cases [2–4]. HIV/AIDS case management, which refers to regular follow-up intervention services, plays a key role in improving adherence to ART and reducing risk behaviors. In China, these services are usually carried out by health professionals from Centers for Disease Control and Prevention (CDCs) at the municipal, district and county levels throughout the country [5, 6].
However, as the reported number of PLWHA increased partially due to the scaling up of HIV testing and ART programs in recent years [7], the expanding workload and shortage of human resources in local CDCs have emerged as new challenges and compromised the quality of HIV/AIDs case management services in recent years [8, 9].To respond to these challenges, task shifting approach recommended by World Health Organization (WHO) can be applied to expand health care workforce and improve access to HIV/AIDS services rapidly. The task shifting approach is based on reorganization and decentralization of health care services, which may be particularly suitable in resource-constrained regions with high HIV/AIDS disease burden [10–12].
China has enhanced health care services for PLWHA in many rural areas with high HIV prevalence supported by the “Four Frees and One Care” program since 2004, which was particularly known as free voluntary counseling and testing and free ART drugs to AIDS patients who were rural residents or lived in urban areas without health insurance. In rural areas, local village doctors were assigned tasks such as health education and case management services. But this type of decentralization was not obvious in urban areas where HIV/AIDS preventive services were mostly administered by local CDCs [13–15]. Hence in urban areas, shifting a part of HIV/AIDS services from CDCs to Community Health Service Centers (CHSCs) has gained much attention both at the national and local level [16, 17]. CHSCs are essential components of China’s three-tier health delivery system providing basic medical and public health services in urban areas. Up till 2010, China has built 33 000 CHSCs in 625 cities nationwide with a total of 295 000 well-trained health providers [18, 19]. Current health policies such as the “Action Plan for HIV/AIDS prevention and Control in China (2010–2015)” and the “National Regulations on Basic Public Health Care (2011)” recommended CHSCs to involve in the HIV/AIDS preventive services. However these policies did not provide specific details or instructions on how CHSCs can fulfill the task of HIV/AIDS case management [20, 21]. In order to develop detailed strategies, we conducted this qualitative policy study to explore the challenges and enablers in the process of shifting the HIV/AIDS case management services from CDCs to CHSCs.
Methods
Conceptual framework
The health policy triangle (HPT) framework was applied as the conceptual framework in this study. Developed by Walt and Gilson, this simplified approach helps researchers to understand and analyze health-related policies systematically [22, 23]. It consists of four elements: context (why), content(what), process(how) and actors (who) (See Fig. 1). Walt and Gilson believed that certain health policy-making was an interactive process within special social-economic and cultural context where actors were at the center of this process. In this study, the context of task shifting strategies was examined mainly from four dimensions of factors: situational factors, structural factors, technical factors and cultural factors [24]. HPT is a useful tool to explore different factors that might affect health policy and its implementation [25].
Fig. 1.
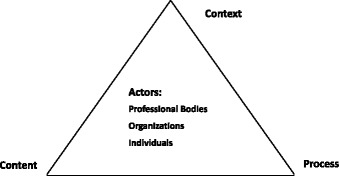
Policy analysis triangle (adapted from Walt and Gilson 1994). Detailed legends: The Policy analysis triangle consists of four elements: context (why need this policy), content (what is the policy mainly about), process (how was the policy brought forward and implemented) and actors (who participates in and influences formulation and implementation of the policy). In this study, actors mainly include officials and health professionals from different levels of health agencies, participants from community-based organizations and people living with HIV/AIDS (PLWHA) in local communities
Study sites and participants
This study was conducted in Guangzhou, Nanjing and Changsha city in 2013, all of which are capital cities of three provinces located in southeast of China. We selected four CHSCs in each city where a pilot program for comprehensive HIV/AIDS case management services was implemented at the time of study. Key actors were invited to attend focus group discussions (FGDs) and individual-based in-depth interviews (IDIs). Key actors were defined as those involved in provision, coordination or utilization of the aforementioned services and therefore could potentially influence relevant policies. We included four types of key actors: (1) 2 officials from the Bureau of Health (BH) and 27 health professionals from CDCs at the provincial, municipal and district levels; (2)37 administrators and health care providers from 12 CHSCs; (3)15 managers and volunteers from 8 local community-based organizations (CBOs); and (4)14 PLWHA in local communities. A purposive sampling method was used to select participants from the health agencies (BH, CDCs and CHSCs) and CBOs. PLWHA participants were recruited with assistance from the local CHSCs and CBOs. A total of 95 participants from three cities were included in the study. About two thirds of the participants from the health agencies had experiences in HIV/AIDS prevention services for more than one year (See Table 1).
Table 1.
Socio-demographic characteristics of four categories of study participants
| Characteristic | BH and CDCs | CHSCs | CBOs | PLWHA | Total |
|---|---|---|---|---|---|
| No. (%) | No. (%) | No. (%) | No. (%) | No. (%) | |
| City | |||||
| Guangzhou | 14(48.3) | 19(51.4) | 4(26.7) | 6(42.9) | 43(45.3) |
| Nanjing | 10(34.5) | 9(24.3) | 6(40.0) | 6(42.9) | 31(32.6) |
| Changsha | 5(17.2) | 9(24.3) | 5(33.3) | 2(14.2) | 21(22.1) |
| Gender | |||||
| Male | 16(55.2) | 9(24.3) | 12(80.0) | 10(71.4) | 47(49.5) |
| Female | 13(44.8) | 28(75.7) | 3(20.0) | 4(28.6) | 48(50.5) |
| Age | |||||
| 18–30 | 9(31.1) | 11(29.7) | 7(46.7) | 3(21.4) | 30(31.6) |
| 31–45 | 17(58.6) | 19(51.4) | 5(33.3) | 8(57.2) | 49(51.6) |
| 46 and above | 3(10.3) | 7(18.9) | 3(20.0) | 3(21.4) | 16(16.8) |
| Education | |||||
| Middle/High school | 0(0) | 0(0) | 1(6.7) | 7(50.0) | 8(8.4) |
| Associate college | 0(0) | 17(45.9) | 0(0) | 5(35.7) | 22(23.2) |
| College and above | 29(100.0) | 20(54.1) | 14(93.3) | 2(14.3) | 65(68.4) |
| HIV/AIDS service years | |||||
| 1 and below | 3(10.4) | 18(48.6) | 1(6.7) | --- | 22(27.2) |
| 2–5 | 13(44.8) | 13(35.2) | 11(73.3) | --- | 37(45.8) |
| 6 and above | 13(44.8) | 6(16.2) | 3(20.0) | --- | 22(27.2) |
BH, Bureau of Health; CDCs, Centers for Disease Control and Prevention; CHSCs, Community Health Service Centers; CBOs, Community-based organizations; PLWHA, People living with HIV/AIDS
Data collection and analysis
We used a three-pronged approach in this study: (1) literature and health policy document review. A total of 78 studies and 17 policy files at the national, municipal and local levels were obtained and reviewed comprehensively, including strategic plans, regulations, technical guidelines and announcements regarding HIV/AIDS preventive services in CHSCs; (2) 15 FGDs with key actors from health agencies and CBOs were organized and conducted; (3) IDIs with 14 PLWHA and 16 participants from local CDCs, CHSCs and CBOs. Three semi-structured interview guides were applied to explore their views on shifting HIV/AIDS case management services from CDCs to CHSCs. In the FGDs and IDIs, we focused on four categories of issues: (1) challenges and enablers in the task shifting of HIV/AIDS case management services; (2) roles and views of different actors in shifting these services; (3) current practice of HIV/AIDS preventive services in CHSCs; and (4) acceptance of and access to case management services in CHSCs among PLWHA.
Both FGDs and IDIs were conducted in Chinese by experienced investigators for approximately 60–120 min in private rooms. All interviews were audio-taped except for some cases where only notes were taken at the request of the interviewees. Audiotapes were transcribed verbatim and the final transcripts were discussed among the investigators. All audio files and transcripts were anonymous. Using a qualitative content analysis method, information in the final transcripts were coded and placed in content tables under specific themes. Quotes, excerpts and summaries were extracted from the content tables and were discussed within the research team to reach a consensus. All transcriptions, coding and analyses were completed in Chinese and the results were translated into English. A narrative approach was used to summarize the data based on the HPT framework.
Ethics statement
The participants were informed of the study purposes before the interviews and FGDs. All participants were voluntary and PLWHA respondents in the study received a cash reward for their participation and a travel expense reimbursement. However we didn’t obtain the consent for publishing the participants’ identification details. To protect their confidentiality, only two identifiers (sex and role) were presented after the quotes from the study participants. The study was approved by the Institutional Review Boards in the National Centers for AIDS/STD Control and Prevention (NCAIDS).
Results
Data collected from three approaches were synthesized based on the HPT framework and particular attention was paid to the responses of key actors to the task shifting of HIV/AIDS case management services to CHSCs.
Context of the task shifting
The context of shifting HIV/AIDS case management services to CHSCs was presented at four levels of factors (See Table 2). Currently, the increasing number of PLWHA and shortage of qualified health professionals in CDCs made shifting of case management services to CHSCs an urgent agenda. Meanwhile, the nationwide distribution of CHSCs with a large number of health care providers, broad coverage of the ART program, easily accessible skill training and promotion of anti-discrimination environment facilitated this task shifting in CHSCs in urban China.
“There are more than 100 CHSCs in Nanjing city. We integrated HIV/AIDS case management into the basic public health services in CHSCs. This approach greatly improved the HIV/AIDS prevention and control in our city.” (Female, official from a municipal Bureau of Health)
“We have only two health professionals in our department engaging in all kinds of HIV/AIDS preventive services but have managed 300 PLWHA. Sometimes we seek help from other departments to finish the work.” (Female, health professional from a district CDC)
Table 2.
Context and process analysis on task shifting of HIV/AIDS case management services to CHSCs
| Element | Description | Evidence |
|---|---|---|
| Context | ||
| 1. Situational factors | • A nationwide public health delivery system had been established defining CHSCs as the primary care institutions. | • Over 33 000 CHSCs and a total of about 300 000 trained employees around the country by 2010. |
| • A large number of well-trained community doctors. | • An average of 100 CHSCs in each selected city. | |
| 2. Structural factors | • The number of PLWHA is increasing. | • The estimated and the reported number of PLWHA is continuously increasing in 2007, 2009 and 2011 in China. |
| • The workload for HIV/AIDS prevention is expanding in CDCs. | ||
| 3. Technical factors | • CHSCs provide comprehensive medical and public health services including HIV/AIDS prevention and control. | • CHSCs serve as gate-keeper of health care delivery system in China. |
| • The expansion of ART program in the country; | • Free ART became available for AIDS patients who were rural residents or urban residents with no health insurance since 2004. | |
| 4. Cultural factors | • The anti-discrimination campaign and human rights protection for PLWHA create supportive and legal environment for HIV/AIDS case management services in CHSCs. | • Issuance of the “Regulations on HIV/AIDS Prevention and Treatment” by the State Council in 2006. |
| •The “Zero discrimination” goal and campaign in the society. | ||
| Process | ||
| 1. Agenda setting | • CHSCs need to participate in HIV/AIDS preventive services. | • China’s second Action Plan for the Containment and Control Of HIV/AIDS (2006–2010) by the State Council in 2006. |
| 2. Policy development | • CHSCs need to assist upper level health institutions in HIV/AIDS health education and case management services. | • National Regulations on Basic Public Health Care by Ministry of Health in 2011. |
| • CHSCs work as platform of China’s HIV/AIDS Care System. | • China’s Action Plan for the Containment and Control of HIV/AIDS (2011–2015) by the State Council in 2011. | |
| • Expansion the coverage of ART. | ||
| • HIV/AIDS case management services were included in the annual assessment of the basic public health services in three cities. | • The regulations or assessment announcements for community health service in Guangzhou, Nanjing and Changsha in 2012. | |
| 3. Implementation | • A pilot program integrating HIV/AIDS case management with routine health services in 42 CHSCs of eight cities (Beijing, Shanghai, Chongqing, Harbin, Nanjing, Hangzhou, Changsha and Guangzhou) was implemented from 2011 to 2013. | • China-Gates Foundation HIV Cooperation Program. |
| • 77.6 % (1046/1348) of PLWHA have been receiving health management services in pilot CHSCs by the end of 2012 according to the program report. |
Process of the task shifting
Table 2 also showed main stages of the task shifting process. The State Council of China began to promote CHSCs’ participation in HIV/AIDS preventive services in 2006. A series of national policies were issued afterwards that guided CHSCs to assist or engage in HIV/AIDS case management services, which created an encouraging and legal environment for HIV/AIDS-related services in CHSCs.
Under the support of the China-Gates Foundation HIV/AIDS Cooperation Program, a pilot program which aimed at integrating HIV/AIDS case management with routine health care services has been initiated in 42 CHSCs of eight cities since 2011. Health care providers from those CHSCs were trained by the program experts following the national technical guideline. According to the program report, about 77.6 % of PLWHA have been receiving health management services in those CHSCs by the end of 2012. And with the promotion of this program, Guangzhou and Nanjing developed their own technical guidelines and regulations for delivery of case management services in CHSCs. All three cities in our study have included the HIV/AIDS case management service in the annual assessment of the basic public health services in CHSCs, which could influence their funding for each subsequent year.
Content of the task shifting
As an integral part of a series of national and local HIV/AIDS policies, case management services in CHSCs aim to reduce HIV new infections as well as mortality rate, expand access to ART program and improve life quality of PLWHA. To achieve these goals, health care providers in CHSCs were required or encouraged to provide comprehensive case management services for PLWHA living in their communities with the support from local CDC and CBOs. The tasks were mainly included as follows:
Entering medical records: to enter medical records for all PLWHA and update their information regularly.
Follow-up interventions: to carry out intervention services for PLWHA, including counseling, psychological support and ART adherence education (twice for HIV-infected persons and four times for AIDS patients in a year, covering at least 85 % of PLWHA).
Testing: to provide CD4 count test for all PLWHA and HIV test for their HIV-negative spouses or regular sexual partners annually.
Treatment: to provide treatment for opportunistic infections, methadone maintenance treatment and ART for PLWHA with instruction from HIV/AIDS specialists.
Key actors and their views on task shifting
Table 3 contains a summary of the key actors and their views on task shifting. Actors played different roles in the shifting process whose views were broadly positive or negative.
Table 3.
Key actors and their views on task shifting of HIV/AIDS case management services to CHSCs
| Actors | Roles in the task shifting | Positive Views | Negative Views |
|---|---|---|---|
| Officials and health professionals from BH and CDCs | Planning, organizing, supporting and evaluating the implementation of HIV/AIDS case management. | • It can improve the quality of services and effectiveness of case management. | • Lack of specific policy and financial support. |
| • It is more geographically convenient and time-saving. | • Low capacity of health service provision for PLWHA in CHSCs. | ||
| • Concerns about loss to follow-up in the referral process from CDCs to CHSCs. | |||
| Administrators and health care providers in CHSCs | Providing the HIV/AIDS case management services for PLWHA. | • Case management in CHSCs have better accessibility and integrated capacity of health care provision. | • Lack of specific funding and manpower. |
| • Health care providers in CHSCs were less experienced and unstable in their position. | |||
| • Health care providers in CHSCs have limited knowledge and skills in HIV/AIDS case management. | |||
| • Lack of coordination and support among government sectors, hospitals, CDCs and CHSCs. | |||
| • Discrimination against PLWHA by health care providers in CHSCS. | |||
| Managers and volunteers from CBOs | Assisting in counseling and referral of HIV/AIDS case management services. | • CBOs have good relationships with PLWHA and flexibility in working hours. | • Inadequate financial and policy support by governments. |
| • CBOs can provide comprehensive counseling for PLWHA. | |||
| PLWHA | Utilization of HIV/AIDS case management services. | • It is more convenient and accessible to utilization related health services in CHSCs. | • Fear for discrimination and lack of confidentiality when receiving health care services in local communities. |
| •Fear for running into acquaintance in CHSCs. |
Participants from BH and CDCs
Most officials from BH and health professionals from CDCs favored CHSCs’ engagement in HIV/AIDS case management services. On the one hand, they considered that the increasing number of managed HIV/AIDS cases and shortage of health professionals made it difficult to improve the service quality and effectiveness. On the other hand, they thought it would be more convenient geographically and would be time-saving for PLWHA to utilize related services in CHSCs in their communities. However, their main concerns were the corresponding financial and strong policy support, CHSCs’ capacity of providing health care for PLWHA and loss to follow-up in the referral process from CDCs to CHSCs.
“Case management services provided by CHSCs have many advantages. Firstly, it is more convenient and economical for PLWHA to come to CHSCs in such a big city. Secondly, CHSCs have both general practitioners and public health professionals who can meet the health service demands of most PLWHA.” (Male, program manager from a municipal CDC)
“It is necessary to transfer this service to CHSCs, but the financial support and manpower issues must be considered to ensure the service quality and sustainability of this work.” (Female, program manager from district CDC)
Administrators and health care providers in CHSCs
Albeit some improvement in accessibility and capacity of integrated health care provision, many CHSCs still faced difficulties after one-year implementation of HIV/AIDS case management services. Firstly, specific funding and manpower were listed as top concerns for administrators in CHSCs. They were not certain whether the services were sustainable after the program ends. Secondly, many health care providers in CHSCs were young women. They were temporarily employed but charged with several tasks. It’s hard for them to keep a stable work relationship with PLWHA. Thirdly, the health care providers had limited knowledge and skills in dealing with complicated psychological and pharmacological problems such as ART side effects. They all claimed the urgent need for professional training on case management services. Fourthly, they also concerned about the lack of coordination among government sectors, hospitals, CDCs and CHSCs in service provision, which could hardly be accomplished by CHSCs alone.
“We could have regular interviews with most PLWHA living in our community and collect their blood sample for CD4 count test. The interview was usually arranged in our CHSC, considering the medical convenience and our personal safety.” (Female, health care provider from a CHSC)
“Our health providers are all part-time employers with a heavy workload. Without the program support, I am afraid this work will not be continued.” (Male, administrator from a CHSC)
“Most health care providers are young women and not stable in their position. The frequent labor turnover of health care provider will surely affect the follow-up intervention. Besides, our knowledge on HIV/AIDS is very limited, for example, if there is an ART side effect, we don’t know how to deal with it.” (Female, administrator from a CHSC)
Managers and volunteers from CBOs
Most managers and volunteers from CBOs supported this task shifting strategy. They thought that CBOs could serve as a bridge between PLWHA and CHSCs if they were given sufficient financial and policy support. Good relationships with PLWHA and flexibility in working hours were their advantages. However, they were concerned that CHSCs had inadequate skills in providing health services such as comprehensive counseling and treatment for opportunistic infections, which might cause loss to follow-up in the process of referral when PLHWA distrusted the health care providers in CHSCs. They also concerned about potential discrimination against PLWHA by some health care providers in CHSCs.
“The resources are controlled by government and we can get little of them. We are good at HIV/AIDS-related counseling. If we assist in managing the PLWHA in CHSCs, their loss to follow-up will be very low.” (Male, CBO volunteer)
“There are some challenges for case management in CHSCs: the knowledge and skill of health care providers is insufficient and some of them have discriminative attitude towards PLWHA, thus PLWHA would not like to go to CHSCs.” (Male, CBO manager)
PLWHA
About half of the PLWHA agreed to transfer the comprehensive management services to local CHSCs, convenience was their main preference for receiving health services in CHSCs including health education and blood sample collection for CD4 count test. Nevertheless, some PLWHA were reluctant to see community doctors. They feared discrimination and lack of confidentiality when receiving health services in local communities. They were also afraid that they would run into an acquaintance in local CHSCs.
“I received follow-up services from doctors in local CHSCs. They also held some health lectures for us. I feel it is very good and convenient here. At the beginning, I really feared that my privacy would be disclosed, but doctors were very considerate about it.” (Male, PLWHA)
“I usually received related health services at CDC in our district and the doctors there were very nice. But now they would transfer me to local CHSC for health services. I would be mad in that case, because my parents still don’t know my HIV positive status. In such a small area, they would inevitably know it. I would be a little better if I could choose to go to another CHSC.” (Male, PLWHA)
Discussion
In the present study, we used the HPT as conceptual framework to explore the challenges and enablers in the task shifting of HIV/AIDS case management services. HPT was widely used in studying HIV/AIDS prevention strategies, especially in evaluating prevention policies and human resources in areas with high HIV/AIDS prevalence [26]. The HPT framework can help both decision-makers and health care providers understand previous policy failures and plan for future policy implementations [23, 24]. Our study included key actors from different professional bodies and interest groups, especially from PLWHA groups to make the policy analysis less top-down and more evidence-based. To our knowledge, this is the first study that employed the HPT framework to assess HIV/AIDS related health services in China. As China’s HIV/AIDS response policies became increasingly information-driven [27], valuable information obtained from this study can help formulate more specific and tailored policies to guide HIV/AIDS prevention and control in urban areas.
Our study showed that shifting HIV/AIDS case management services downwards to CHSCs was feasible in terms of the policy environment, infrastructure and technical capacity of the CHSCs in urban China. Their wide distribution, technical capacity and current practice enabled them to carry out the HIV/AIDS case management services for PLWHA in local communities. Other studies have shown that community support can effectively improve PLWHA’s access to related health care services [28, 29]. Community-based case management services for PLWHA such as follow-up interventions, psychosocial counseling and education for ART adherence can improve their health outcomes, especially in a resource-constrained setting facing a shortage of health workers and/or facilities [30, 31]. Also, the increasing number of PLWHA and expansion of HIV/AIDS preventive services posed challenges to CDCs such as lack of workforce and sub-optimal quality of services. Our analysis indicated that task shifting of case management is a necessary response to the changing epidemic of HIV/AIDS in urban China. Policy makers need to ensure both political feasibility and resources accessibility to facilitate this process [32, 33].
However, the reluctant acceptance among some health care providers and PLWHA may compromise the effectiveness and sustainability of those services. Our findings indicated several challenges in the task shifting. Those challenges included lack of specific policy and stable financial support for CHSCs, inadequate manpower, relatively low capacity for health service delivery, lack of coordination among sectors, PLWHA’s fear for discrimination and privacy disclosure in local communities. As pointed out in the WHO guidelines, task shifting is not merely the move of health services from qualified health workers to less specialized health care providers, it should be implemented alongside with other efforts and resources such as financial support, skill training and supportive environment to sustain the services [11, 34].
CHSCs in urban China are mostly publicly-owned. Their funding was allocated in proportional to the number of residents in their catchment areas, whereas many PLWHA in local communities were not counted as community residents since they were migrants. Moreover, HIV/AIDS related health services were not in the priority among 11 health service tasks in the National Regulations on Basic Public Health Care, which may also discourage decision-makers from funding those services [20]. Although all CHSCs in our study were located in relatively affluent areas with well-built health service facilities and higher level of funding than the national average, financial and human resources constraint were still their top concerns for providing those case management services. As our study indicated that the transfer of certain health services should be accompanied by adequate funding. Furthermore, cultivation and cooperation with local CBOs could facilitate the task shifting process [35].
PLWHA’s concerns about confidentiality and potential discrimination were crucial factors preventing them from utilizing services at CHSCs, as was also revealed in other studies [36, 37]. Therefore, we highly recommended CDCs and CHSCs to train health care providers to improve their awareness of patients’ confidentiality and to create an anti-discrimination environment for PLWHA. Individual-based communication with PLWHA could be an appropriate way to help reduce their mistrust of community health care providers and ensure the success of task shifting process.
It should be noted that there were some limitations in this study. First, all three cities were selected from relatively affluent areas with good community health service environment, so findings of this study may reflect a higher acceptance for the task shifting than those in other urban areas of China. Secondly, actors from the national level were not included in this study, so information about how the nation-level HIV/AIDS related policies were shaped and how the program initiated was very limited. Thirdly, this study mainly focused on task shifting to community health care facilities, whereas other lay health personnel such as community health volunteers and retired nurses may also be effective shifting pathways that deserves further studies [29, 38]. Finally, evidence from one qualitative study was not sufficient for developing and modifying the task shifting policy, more quantitative research on health services are needed to comprehensively assess the impact of this task shifting strategy on the access and quality of health care for PLWHA.
Conclusions
This study presented preliminary but informative evidence for the current policy of shifting HIV/AIDS case management services to CHSCs in urban China. Our study pointed out the feasibility and necessity of HIV/AIDS case management in terms of response to HIV/AIDS epidemic, policy environment, wide distribution and technical capacity of CHSCs. In addition, the study also suggested that this shifting strategy should be implemented with more targeted funding, planned team building, professional skill training, coordination with other sectors and education on privacy protection and non-discrimination to make the services more successful and sustainable.
Acknowledgements
This study was supported by China-Gates Foundation HIV Prevention Cooperation Program (OPP49277) and National Science Foundation of China (71373008, 71473234). We thank the health administrative departments, CDCs and involved CHSCs in Hunan Province (Changsha), Guangdong Province (Guangzhou) and Jiangsu Province (Nanjing) for their efforts in the study. Appreciation is also owed to Donglan Zhang for her help in writing assistance. The authors are grateful to all study participants.
Abbreviations
- PLWHA
People living with HIV/AIDS
- ART
Antiretroviral Treatment
- CDCs
Centers for Disease Control and Prevention
- WHO
World Health Organization
- CHSCs
Community Health Service Centers
- HPT
Health policy triangle
- FGDs
Focus group discussion
- IDIs
In-depth interviews
- BH
Bureau of Health
- CBOs
Community-based organizations
- NCAIDS
National Centers for AIDS/STD Control and Prevention
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
FL PX ZW JS DZ and FM conceived and designed the study. FM PX DZ SM LJ HJ and LM participated in the data collection, analysis and interpretation. FM drafted the manuscript. All authors read and approved the final manuscript.
Contributor Information
Fuchang Ma, Email: mafc.key@163.com.
Fan Lv, Email: fanlv@vip.sina.com.
Peng Xu, Email: xupeng2007@163.com.
Dapeng Zhang, Email: zhangdapeng@chinaaids.cn.
Sining Meng, Email: meng_sn@hotmail.com.
Lahong Ju, Email: julahong@chinaaids.cn.
Huihui Jiang, Email: jhh235@163.com.
Liping Ma, Email: malp1710@163.com.
Jiangping Sun, Email: jpsun@chinaaids.cn.
Zunyou Wu, Email: wuzy@263.net.
References
- 1.Ministry of Health, UNAIDS, World Health Organization . 2011 Report on the estimation of HIV epidemic in China. Beijing: Ministry of Health; 2011. [Google Scholar]
- 2.Ming ZQ, Cheng F, Liu Q, Airawanwat R, Chen YH, Zhu QY, Liu W, Wang Y, Zhang KL. A qualitative exploration of the role of antiretroviral therapy on Chinese rural life. Biomed Environ Sci. 2012;25(1):69–76. doi: 10.3967/0895-3988.2012.01.010. [DOI] [PubMed] [Google Scholar]
- 3.Zhao DC, Wen Y, Ma Y, Zhao Y, Zhang Y, Wu YS, Liu X, Au E, Liu ZF, Zhang FJ. Expansion of China’s free antiretroviral treatment program. Chin Med J (Engl) 2012;125(19):3514–3521. [PubMed] [Google Scholar]
- 4.Luo L, Li TS. Overview of antiretroviral treatment in China: advancement and Challenges. Chin Med J (Engl) 2011;124(3):440–444. [PubMed] [Google Scholar]
- 5.Zhang Y, Lu L, Li HQ, Liu W, Tang ZR, Chen JY, Ma Y, Zhao Y, Chen RY, Zhang FJ. Engaging HIV-infected patients in antiretroviral therapy services:CD4 cell count testing after HIV diagnosis from 2005 to 2009 in Yunnan and Guangxi, China. Chin Med J (Engl) 2011;124(10):1488–1492. [PubMed] [Google Scholar]
- 6.Kushel MB, Colfax G, Ragland K, Heineman A, Palacio H, Bangsberg DR. Case management is associated with improved antiretroviral adherence and CD4+ cell counts in homeless and marginally housed individuals with HIV infection. Clin Infect Dis. 2006;43(2):234–242. doi: 10.1086/505212. [DOI] [PubMed] [Google Scholar]
- 7.Xing H, Ruan YH, Li JY, Shang H, Zhong P, Wang X, Liao LJ, Li HP, Zhang M, Xue YL, Wang Z, Su B, Liu W, Dong YH, Ma YL, Li HQ, Qin GM, Chen L, Pan XH, Chen X, Peng GP, Fu JH, Chen RY, Kang LY, Shao YM, Chinese National HIVDR Surveillance and Monitoring Network HIV drug resistance and its impact on antiretroviral therapy in Chinese HIV-infected patients. PLoS ONE. 2013;8(2) doi: 10.1371/journal.pone.0054917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shao YM. AIDS epidemic at age 25 and control efforts in China. Retrovirology. 2006;3:87. doi: 10.1186/1742-4690-3-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li L, Liang LJ, Wu ZY, Lin CQ, Wu S. Institutional support for HIV/AIDS care in China: a multilevel analysis. AIDS Care. 2008;20(10):1190–1196. doi: 10.1080/09540120801919394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization . Task shifting global recommendations and Guidelines. Geneva: World Health Organization; 2008. [Google Scholar]
- 11.El-Sadr WM, Abrams EJ. Scale-up of HIV care and treatment: can it transform healthcare services in resource-limited settings. AIDS. 2007;21(suppl 5):S65–70. doi: 10.1097/01.aids.0000298105.79484.62. [DOI] [PubMed] [Google Scholar]
- 12.Walsh A, Ndubani P, Simbaya J, Dicker P, Brugha R. Task sharing in Zambia: HIV service scale-up compounds the human resource crisis. BMC Health Serv Res. 2010;10:272. doi: 10.1186/1472-6963-10-272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang XL, Miege P, Zhang YR. Decentralization of the provision of health services to people living with HIV/AIDS in rural China: the case of three counties. Health Res Policy Syst. 2011;9:9. doi: 10.1186/1478-4505-9-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ministry of Health . 2012 China AIDS Response Progress Report. Beijing: Ministry of Health; 2012. [Google Scholar]
- 15.Wu ZY, Wang Y, Mao YR, Sullivan SG, Juniper N, Bulterys M. The integration of multiple HIV/AIDS projects into a coordinated national programme in China. Bull World Health Organ. 2011;89(3):227–233. doi: 10.2471/BLT.10.082552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.The State Council of the People's Republic of China . Action Plan for HIV/AIDS prevention and Control in China (2010–2015) Beijing: The State Council of the People's Republic of China; 2012. [Google Scholar]
- 17.Jiang Z, Wang DB, Yang S, Duan MY, Bu PB, Green A, Zhang XJ. Integrated response toward HIV: a health promotion case study from China. Health Promot Int. 2011;26(2):196–211. doi: 10.1093/heapro/daq044. [DOI] [PubMed] [Google Scholar]
- 18.Zhou W, Dong YM, Lin XZ, Lu WL, Tian X, Yang LP, Zhang XP. Community health service capacity in China: a survey in three municipalities. J Eval Clin Pract. 2013;19(1):167–172. doi: 10.1111/j.1365-2753.2011.01788.x. [DOI] [PubMed] [Google Scholar]
- 19.Zhang XP, Xiong YQ, Ye J, Deng ZH, Zhang XP. Analysis of government investment in primary healthcare institutions to promote equity during the three-year health reform program in China. BMC Health Serv Res. 2013;13:114. doi: 10.1186/1472-6963-13-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ministry of Health . National Regulations on Basic Public Health Care (2011) Beijing: Ministry of Health; 2011. [Google Scholar]
- 21.Sun JP, Liu H, Li H, Wang LQ, Guo HY, Shan D, Bulterys M, Korhonen C, Hao Y, Ren MH. Contributions of international cooperation projects to the HIV/AIDS response in China. Int J Epidemiol. 2010;39 Suppl 2:ii14–20. doi: 10.1093/ije/dyq208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Taegtmeyer M, Martineau T, Namwebya JH, Ikahu A, Ngare CW, Sakwa J, Lalloo DG, Theobald S. A qualitative exploration of the human resource policy implications of voluntary counseling and testing scale-up in Kenya: applying a model for policy analysis. BMC Public Health. 2011;11:812. doi: 10.1186/1471-2458-11-812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Walt G, Shiffman J, Schneider H, Murray SF, Brugha R, Gilson L. Doing health policy analysis: methodological and conceptual reflections and challenges. Health Policy Plan. 2008;23(5):308–317. doi: 10.1093/heapol/czn024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Buse K, Mays N, Walt G. Making Health Policy. Maidenhead: Open University Press; 2004. [Google Scholar]
- 25.Hercot D, Meessen B, Ridde V, Gilson L. Removing user fees for health services in low-income countries: a multi-country review framework for assessing the process of policy change. Health Policy Plan. 2011;26 Suppl 2:ii5–15. doi: 10.1093/heapol/czr063. [DOI] [PubMed] [Google Scholar]
- 26.Walt G, Gilson L. Reforming the health sector in developing countries: the central role of policy analysis. Health Policy Plan. 1994;9(4):353–370. doi: 10.1093/heapol/9.4.353. [DOI] [PubMed] [Google Scholar]
- 27.Sun XH, Lu F, Wu ZY, Poundstone K, Zeng G, Xu P. Evolution of information-driven HIV/AIDS policies in China. Int J Epidemiol. 2010;39:ii4–ii13. doi: 10.1093/ije/dyq217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Li L, Cao HJ, Wu ZY, Wu S, Xiao L. Diffusion of positive AIDS care message among service providers in China. AIDS Educ Prev. 2007;19(6):511–518. doi: 10.1521/aeap.2007.19.6.511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wouters E, Van Damme W, van Rensburg D, Masquillier C, Meulemans H. Impact of community-based support services on antiretroviral treatment programme delivery and outcomes in resource-limited countries: a synthetic review. BMC Health Serv Res. 2012;12:194. doi: 10.1186/1472-6963-12-194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wilson MG, Husbands W, Makoroka L, Rueda S, Greenspan NR, Eady A, Dolan LA, Kennedy R, Cattaneo J, Rourke S. Counselling, case management and health promotion for people living with HIV/AIDS: an overview of systematic reviews. AIDS Behav. 2013;17(5):1612–1625. doi: 10.1007/s10461-012-0283-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Duwell MM, Knowlton AR, Nachega JB, Efron A, Goliath R, Morroni C. Patient-nominated, community-based HIV treatment supporters: patient perspectives, feasibility, challenges, and factors for success in HIV-infected South African adults. AIDS Patient Care and STDs. 2013;27(2):96–102. doi: 10.1089/apc.2012.0348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lu F. Improving the system to ensure good quality and high coverage of HIV/AIDS response. Chin J Prev Med. 2013;47(11):984–987. [Google Scholar]
- 33.Samb B, Celletti F, Holloway J, Van Damme W, De Cock KM, Dybul M. Rapid expansion of the health workforce in response to the HIV epidemic. N Engl J Med. 2007;357(24):2510–2514. doi: 10.1056/NEJMsb071889. [DOI] [PubMed] [Google Scholar]
- 34.Lehmann U, Van Damme WV, Barten F, Sanders D. Task shifting: the answer to the human resources crisis in Africa. Hum Resour Health. 2009;7:49. doi: 10.1186/1478-4491-7-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Xu H, Zeng Y, Anderson AF. Chinese NGOs in action against HIV/AIDS. Cell Res. 2005;15(11–12):914–918. doi: 10.1038/sj.cr.7290368. [DOI] [PubMed] [Google Scholar]
- 36.Wu S, Li L, Wu ZY, Liang LJ, Cao HJ, Yan ZH, Li JH. A brief HIV stigma reduction intervention for service providers in China. AIDS Patient Care STDS. 2008;22(6):513–520. doi: 10.1089/apc.2007.0198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chan KY, Yang Y, Zhang KL, Reidpath DD. Disentangling the stigma of HIV/AIDS from the stigmas of drugs use, commercial sex and commercial blood donation-a factorial survey of medical students in China. BMC Public Health. 2007;7:280. doi: 10.1186/1471-2458-7-280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wouters E, Van Damme W, Van Loon F, van Rensburg D, Meulemans H. Public-sector ART in the Free State Province, South Africa: Community support as an important determinant of outcome. Soc Sci Med. 2009;69(8):1177–1185. doi: 10.1016/j.socscimed.2009.07.034. [DOI] [PubMed] [Google Scholar]


