Abstract
Background
Femoral head is the most common bone affected by avascular necrosis. Core decompression procedure, when done in the initial stages, before collapse, may arrest or reverse the progress of avascular necrosis and thereby may preserve the normal femoral head. Hence, we have analysed the clinical, functional and radiological outcome of core decompression and bone grafting in patients with Osteonecrosis of the femoral head (ONFH) upto stage IIB (Ficat & Arlet).
Materials and method
A study was undertaken at our institute from June 2010 to June 2013 wherein 20 patients (28 hips) of ONFH upto grade II B (Ficat & Arlet) were treated with core decompression and the outcomes were studied. Patients were subjected to core decompression of the affected hip. All the patients were operated in lateral position. In 26/28 hips, cancellous grafting was done after harvesting graft from the posterior iliac crest. In 2 patients cortical non-vascularised fibular graft was used.
Results
Functional outcome was assessed by Harris hip score, wherein 19 hips (67.85%) had good or excellent outcome; 1 hip (3.57%) had fair out come. However, 8 hips (28.57%) showed poor result. For stage I, 12/13 hips (92.3%) improved, whereas for Stage IIA, 6/11 hips (54.54%) showed improvement and for stage IIB, only 2/4 hips (50%) showed improvement. Less than 25% of the hips required a replacement or salvage procedure. Strict non weight bearing was complied by 23 hips (82.14%), whereas 5 hips (17.85%) were not compliant. If we exclude non compliant patients, our success rate was 92.3% for grade I, 100% for grade IIA and 50% for grade IIB.
Conclusion
Core decompression and bone grafting provide satisfactory outcome when patients are carefully selected in early stages of the disease, before the stage of collapse.
Keywords: Avascular necrosis, Core decompression, Bone grafting
1. Introduction
Avascular necrosis (AVN) is defined as a cellular death of bone components due to interruption of blood supply. The bone structures then collapse, resulting in bone destruction, pain, and loss of joint function.1 Certain bones have precarious blood supply; hence even a small vascular insult can result in avascular necrosis of the part supplied by it. The head of femur is the most common bone affected by avascular necrosis. Clinically the pain may be minimal at onset, but if no active intervention is done it may worsen gradually, affecting the activities of daily living. It affects young population and if not managed timely, leads to the collapse of femoral head eventually requiring hip arthroplasty.
Avascular necrosis of femoral head (ONFH) is associated with many etiological factors and usually one or more risk factors are present but approximately two-thirds of this is related to alcohol abuse and corticosteroid intake. Rest are mainly idiopathic.2 The rationale for the use of core decompression is based on the concept that increased intra-medullary pressure is involved in the pathogenesis of avascular necrosis. Thus by core decompression, creeping substitution to the necrotic area occurs by bringing the blood supply through the drilled channels thereby decreasing the intra-medullary pressure. This may arrest or reverse the progress of avascular necrosis before the collapse occurs thereby avoiding articular collapse and its sequelae. Hence when acted, vigilantly at initial stages before collapse occurs, core decompression may preserve the normal femoral head.
In this study, we have analysed the clinical, functional and radiological outcome of core decompression and bone grafting in patients with ONFH upto stage IIB (Ficat & Arlet).
2. Materials and method
The current study was undertaken at our institution from June 2010 to June 2013 wherein 20 patients (28 hips) of AVN of femoral head upto grade II B (Ficat & Arlet) were treated with core decompression. Patients with sickle cell disease were excluded as these patients are expected to have recurrent vascular infarcts thereby nullifying the principle of core decompression.
The patients meeting the inclusion criteria were evaluated in terms of age, sex, occupation, pain with its detailed characteristics, limp, duration of symptoms, progression of symptoms, deformity, support required to walk or not, any history of trauma and history of other joint pain. History of risk factors like steroids and alcoholism was also noted. They were thoroughly examined for their pre-operative hip range of movement as well as their debility and their Harris hip score was noted. They were also investigated by routine blood investigations (complete hemogram, ESR, CRP, liver and kidney function tests) and radiologically by hip AP and Frog leg view X-rays and MRI of both hips to know the amount of involvement of the femoral head, stage the disease as well as to check the status of contralateral hip. It also helped to map out the affected areas of the hip.
Following adequate explanation about the procedure and necessary consent, patients were subjected to core decompression of the affected hip. Patients were operated in lateral position and guide-wire was inserted through lateral cortex just below the base of greater trochanter under image intensifier. Based on primary mapping of the affected area in head and under image intensifier guidance, the guide pin was directed towards the affected area. Confirming position of the guide pins in both AP and lateral views (taken by keeping the leg in flexion, abduction and external rotation), serial reaming was done by DHS reamer to scrape out the necrotic sclerotic part.
The affected part being sclerotic was harder to scrape out as compared to the normal bone and this gives an indirect confirmation of the affected area. The margins of the core created were thereafter curetted till normal feel of the bone is achieved and confirmed under image intensifier. The core thus created was filled by bone grafts. In 26/28 hips, cancellous grafting was done after harvesting graft from the posterior iliac crest. As patients were placed in lateral position it was easier to harvest graft from posterior iliac crest and also larger quantity of graft can be obtained to fill the larger void.
Cancellous bone graft has both osteogenic as well as osteo-inducing properties, thereby facilitating the scaffold for new bone formation. However, in 2 patients cortical non-vascularised fibular graft was used to provide mechanical support. However, decision of the type of graft was purely surgeon based.
Patients were advised strict non weight bearing for atleast 3 months though hip range of movement exercises in bed were started from 2nd post-operative day as per pain tolerance.
The patients were followed at an interval of 1, 3 and 6 months post-operatively and at the latest follow-up were re evaluated clinic-radiologically by X-rays. Weight bearing was started after 3 months only after the void in the femoral head showed new bone formation. If patient agreed, a repeat MRI was done at 6 months or later to compare the outcome of core decompression. The outcomes were judged based on Harris hip score.
3. Results
There were 20 patients in our study, out of which 14 (70%) were with bilateral and 6 (30%) with unilateral involvement (total number of hips involved with ONFH were 34). 6 out of 34 hips with stage 3 or 4 ONFH were excluded, leaving 28 hips. Male (80%): Female (20%) ratio was 4:1. Majority of patients (60%) found in our series were chronic alcoholics. A majority of patients (53.57%) had encountered difficulties in daily living. There were 13 hips (46.42%) of Ficat & Arlet grade I, 11 hips (39.28%) of grade IIA and remaining 4 hips (14.28%) were grade IIB (Table 1).
Table 1.
Distribution of patients according to grade of ONFH.
| X-ray | MRI | |
|---|---|---|
| Normal | 13 (46.42%) | |
| Grade I | 13 (46.42%) | |
| Grade II A | 11 (39.28%) | 11 (39.28%) |
| Grade II B | 4 (14.28%) | 4 (14.28%) |
| Total | 28 | 28 |
The procedure adopted in 26 hips (92.85%) was core decompression and cancellous bone grafting. Remaining 2 hips (7.14%) were treated with core decompression and fibular grafting.
Alcohol consumption contributed in majority of patients 12/20 (60%) for AVN. 1 patient had AVN following long term steroid use and 1 had HIV infection (stage 3). Whereas, no contributing cause was found in 6/20 patients.
15/20 presented within 6 months of onset of pain. Majority of presenting patients had more restriction of cross leg sitting (13/20) and squatting (14/20) as compared to climbing stairs (9/20).
16/28 hips had flexion >90° but extension was restricted in >80% hips (23/28). Similarly, almost half of the hips (13 hips) had significant restriction of abduction (less than 30°) and 22/28 hips had appreciable restriction in adduction (less than 20°). Also two-thirds of the presenting hips had appreciable restriction in internal rotation, both in flexion (20/28) and extension (19/28), which was less than 10° and 22/28 hips had appreciable restriction (<30°) in external rotation in flexion and 18/28 had in extension (Table 2).
Table 2.
Range of movements of hip.
| Degree | On presentation |
3 Months |
6 Months |
Final follow-up |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| F | E | AB | AD | F | E | AB | AD | F | E | AB | AD | F | E | AB | AD | |
| 0–"10 | 23 | 9 | 22 | 7 | 22 | 3 | 8 | 24 | 3 | 8 | ||||||
| 11–20 | 5 | 3 | 13 | 6 | 5 | 15 | 6 | 4 | 9 | 4 | 4 | 9 | ||||
| 21–30 | 10 | 6 | 7 | 6 | 3 | 11 | 3 | 11 | ||||||||
| 31–40 | 11 | 12 | 10 | 10 | ||||||||||||
| 41–50 | 4 | 4 | 8 | 8 | ||||||||||||
| 51–60 | 2 | 2 | ||||||||||||||
| 61–70 | 4 | 4 | 2 | 2 | ||||||||||||
| 71–80 | ||||||||||||||||
| 81–90 | 8 | 8 | 8 | 8 | ||||||||||||
| 91–100 | 14 | 14 | 14 | 14 | ||||||||||||
| 101–110 | 1 | 2 | 2 | 2 | ||||||||||||
| 111–120 | 1 | |||||||||||||||
| Total | 28 | 28 | 28 | 28 | 28 | 28 | 28 | 28 | 28 | 28 | 28 | 28 | 28 | 28 | 28 | 28 |
All 13 hips which were diagnosed as grade I in MRI appeared completely normal on X-ray. However AVN of higher grade II A and B had similar representation in both X-ray and MRI.
26 hips were treated with core decompression with cancellous bone graft. However in 2 patients non-vascularised fibular strut graft was used instead of cancellous grafts. Both of them were of type II B. However the decision was solely surgeon based. 6 patients having grade 3 and 4 AVN in contralateral hip were treated with replacement surgery. Average follow-up of 20 patients was upto 11 months.
Majority of the patients (16) were immobilized for atleast 12 weeks. However, 5 patients being non-compliant started weight bearing earlier. Out of 28, 26 hips had pain relief immediately after operation. In follow-up at 3 months, 22 hips had complete pain relief and at 6 months and final follow-up 19 had no pain. So it suggests that majority of patients (67.86%) had pain relief after the procedure.
Out of 28 hips, though 27 hips had internal rotation (in flexion) of less than 20° at 3 months of follow-up, 6 patients showed appreciable improvement at final follow-up. Similar improvement was also seen in 5 hips having less than 10° internal rotation in extension at final follow-up. In 3 patients who had less than 30°s of external rotation (in flexion) at 3 months improvement was seen at final follow-up. Appreciable improvement was also seen in 2 hips that had less than 30° of external rotation in extension (Table 3).
Table 3.
Range of internal and external rotation of hip.
| Degree | On presentation |
3 Months |
6 Months |
Final follow-up |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| IR |
ER |
IR |
ER |
IR |
ER |
IR |
ER |
|||||||||
| F | E | F | E | F | E | F | E | F | E | F | E | F | E | F | E | |
| 0–10 | 20 | 19 | 6 | 4 | 14 | 12 | 4 | 4 | 11 | 7 | 3 | 2 | 11 | 7 | 3 | 2 |
| 11–20 | 7 | 7 | 9 | 11 | 13 | 12 | 7 | 7 | 10 | 13 | 7 | 3 | 10 | 13 | 7 | 3 |
| 21–30 | 1 | 2 | 7 | 4 | 1 | 4 | 11 | 8 | 6 | 7 | 9 | 12 | 6 | 7 | 9 | 12 |
| 31–40 | 4 | 9 | 6 | 8 | 1 | 8 | 10 | 1 | 8 | 10 | ||||||
| 41–50 | 2 | 1 | 1 | 1 | 1 | 1 | ||||||||||
| Total | 28 | 28 | 28 | 28 | 28 | 28 | 28 | 28 | 28 | 28 | 28 | 28 | 28 | 28 | 28 | 28 |
Out of 28 hips, 6 hips (21.42%) showed collapse at 3 months. 2 more hips worsened at 6 months follow-up. Thus at final follow-up 8 hips had collapse and worsening.
Out of 28 hips, though 19 hips had no complication, 8 hips showed further advancement of the disease resulting into arthritis. One hip had superficial infection initially which subsided after debridement.
According to Harris hip score, 19 hips (67.85%) had good or excellent outcome whereas 1 hip (3.57%) had fair outcome. However 8 hips (28.57%) showed poor result. For stage I, out of 13 hips, 12 hips (92.3%) improved, whereas for Stage IIA, out of 11 hips, 6 hips (54.54%) showed improvement and for stage IIB, out of 4 hips only 2 hips (50%) showed improvement (Table 4). Also 3 patients who had low pre-operative Harris hip score (<60), did not improve but worsened.
Table 4.
Harris hip score distribution.
| Harris hip score | Pre-operative | Final follow-up |
|---|---|---|
| 0–10 | ||
| 11–20 | 2 | |
| 21–30 | ||
| 31–40 | 1 | |
| 41–50 | 1 | 1 |
| 51–60 | 1 | 0 |
| 61–70 | 15 | 5 |
| 71–80 | 7 | 1 |
| 81–90 | 3 | 10 |
| 91–100 | 9 | |
| Total hip | 28 | 28 |
Strict non weight bearing was complied by 23 hips (82.14%), whereas 5 hips (17.85%) were not compliant. If we exclude non-compliant patients, our success rate was 92.3% for grade I, 100% for grade IIA and 50% for grade IIB.
Thus, based on Harris hip score system, overall out of 28 hips, 20 hips improved and average Harris hip score of those 20 hips was 71.18 (pre-operative) which was increased to 88.23 at final follow-up. Remaining 8 hips did not show improvement. Their score was 58.03 (pre-operative) and 47.68 at final follow-up, which showed deterioration (Fig. 1a–d).
Fig. 1.
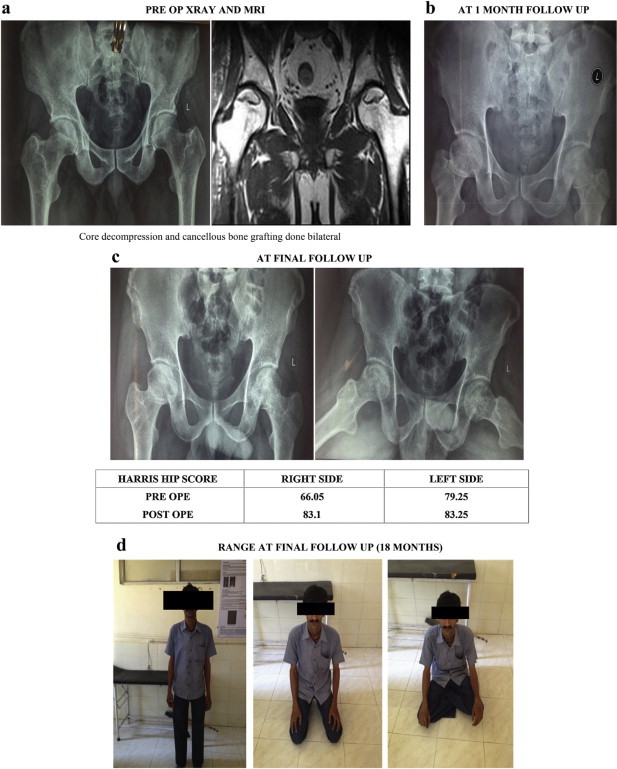
28 yr/M/labourer/pain in Rt hip since 6 months, Lt hip asymptomatic/diagnosed as bilateral AVN grade IIA on Rt side and grade I on Lt side.
4. Discussion
In our study, most of the patients were under the age group of 20–40 years (75%) while rest of them were from the age group 41–50 years (25%). From the above data, it suggests that almost all the patients are from young age group. Similar results were also found in various other studies.3–5 Males were more commonly affected (80%) as compared to females (M:F- 4:1). Similar results were also shown in the study of Babhulkar et al where 81.25% were males.6
In our study, out of 20 patients, 6 (30%) had unilateral involvement and rest 14 (70%) had bilateral involvement. According to Bradway JK and Kozinn, incidence of bilaterality ranges from 6 to 72%, where as Mankin and Brower report an incidence from 20 to 80%.6 As the risk factors of alcohol abuse, steroids intake and HIV have systemic effect, there are comparatively more chances of bilateral involvement.
According to Shannon and Trousdale, most non traumatic cases of femoral head AVN, the disease is often bilateral, due to risk factors like long term corticosteroid use, alcohol abuse and sickle cell disease.6 Out of 34 hips, 6 hips were not considered as they had grade III & IV of AVN (FICAT & ARLET classification). So, only 28 hips were included in our study. In our study, 12 (60%) patients were alcoholic, out of whom 1 was HIV positive and other 1 was taking steroids (for skin disease), remaining 8 (40%) patients had idiopathic AVN. This also shows that chronic alcoholism contributes to development of AVN more than other risk factors. Correlating facts were also observed in Babhulkar et al where approximately more than half cases were related to alcohol abuse.6
Out of 20 patients, 14 patients (70%) had bilateral involvement. Out of 14 patients, 6 patients were asymptomatic clinically and were diagnosed only on MRI. Remaining patients had pain bilaterally.
Activity of daily living were affected in 15 (53.57%) out of 28 hips. Even in early stage of AVN the daily activities of the patients were affected. On the basis of overall review cross leg sitting and squatting is more difficult for patients as compared to stair climbing. Similar statistics in other series is not available.
For the diagnosis and staging of AVN, X-rays and MRI were routinely performed. According to classification of Ficat and Arlet, in our study 13 hips (46.42%) were normal on X-rays but showed in MRI as grade I. Out of 28 hips 11 (39.28%) of them were graded as IIA on X-ray as well as on MRI. Remaining 4 hips (14.28%) were diagnosed as grade II B on X-ray as well as on MRI (Fig. 2a–d).
Fig. 2.
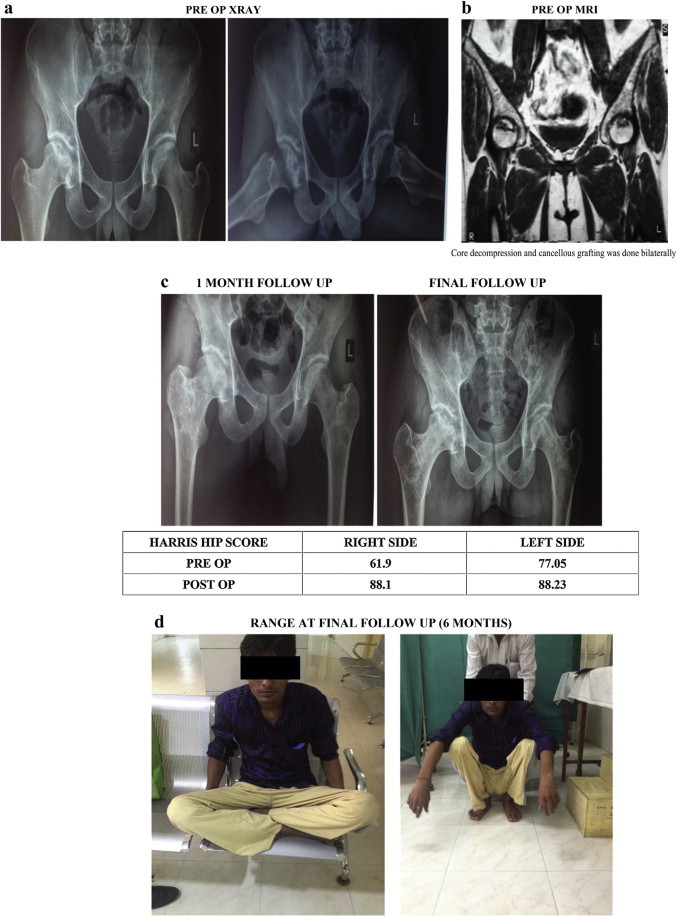
25 yr/M/farmer/pain on Rt hip since 1 year, Lt hip asymtomatic/diagnosed bilateral AVN on MRI (grade IIB on Rt side and grade I on Lt side).
This clearly brings out the fact that X-ray may not be of much help in diagnosing AVN in Stage I. However it is at par with MRI as far as stage IIa and II b is concerned. MRI is more significant as compared to X-rays especially in diagnosing stage I AVN in normal looking contralateral hip on X-ray.
The minimum follow-up was 6 months whereas the maximum follow-up was of 24 months and our average follow-up was 11 months. Though for such study long term follow-up is necessary; hence a drawback in our study.
Core decompression procedures showed improvement in results in patients who had abduction more than 30° and adduction more than 10°. Moreover it also showed more improvement for internal rotation (hip flexion and extension) in comparison with external rotation.
Out of 28, majority had pain relief immediately following operation but as time passed deterioration was seen. At 3 months, 22 hips (78.57%) had pain relief but only 19 hips (67.85%) had pain relief at final follow-up. So it suggests that majority of patients (67.85%) had pain relief after procedure. Out of 28 hips, 2 hips (7.14%) that had started early weight bearing before 3 months had mild pain. However our follow-up is not long enough to comment on long term pain relief. According to Babhulkar et al, 6 patients (19%) had residual pain around 24 weeks following surgery.6 In literature, most of the authors have noted immediate pain relief after core decompression other than Saito et al.
As per our protocol, the common practice was to immobilise patient for 14 weeks in bed so that patient remains non weight bearing and compliant. However 5 hips did not comply with the requirement. 3 of them started weight bearing immediately after surgery whereas 1 started after 4 weeks and another at 6 weeks of surgery. Those 5 hips (17.85%) that were not immobilised adequately had collapse of femoral head. From the remaining 23 hips, 19 hips (82.60%) were successfully prevented from collapsing. This could be because once core decompression is done, the femoral head would require adequate time for regeneration. Hence if weight bearing is started before adequate bone formation, it might lead to collapse of the femoral head under stress. Adequate immobilisation (at least 3 month post-operatively) for AVN patients treated with core decompression for incorporation of the graft and new bone formation is therefore suggested. Similarly, in study by Babhulkar et al, patients were allowed partial weight bearing after 10 weeks and full weight bearing after 14–16 weeks depending upon the incorporation of graft.6
Out of 28 hips, 6 hips (21.42%) showed the collapse at 3 months where as 22 hips didn't show any collapse. Whereas 2 more hips showed collapse at 6 months following initiation of weight bearing. Similar results were also found in study by Carlos et al wherein radiographic progression from pre-collapse to collapsed stage occurred in 21 hips (36.8%) out of 57 hips.7
So it clearly suggested that if worsening occurs it occurs within 6 months only, thereafter no worsening ensues. However our follow-up was too short to comment on this observation.
Out of 28 hips, though 19 hips had no complication, 8 hips (28.57%) showed further advancement of the disease resulting into arthritis and 1 patient had superficial infection which subsided after thorough debridement. Out of 8 patients who had progressed to arthritis, 5 of them had started early weight bearing.
If we exclude 5 hips (all had stage IIA) which worsened due to non compliance, our outcome changes significantly. For stage I, out of 13 hips, 12 hips (92.3%) improved, whereas all 6 hips of Stage IIA, (100%) showed improvement. However in stage IIB, out of 4 hips only 2 hips (50%) showed improvement. Thus over all 8 hips (75%) were improved out of 10 hips of grade II.
A Meta analysis of 24 reports analysing 1206 hips treated by core decompression with or without cancellous bone grafting revealed an overall clinical success rate of 63.5%. Less than 33% of the hips required a replacement or salvage procedure during the follow-up period.8
Ficat reviewed the results of core decompression in 133 patients with ON of the hip (average follow-up, 9 years, 6 months) and reported a successful clinical result in 90% with no radiographic progression in 79% of the patients.9
In 1986, Camp and Colwell reported the results of core decompression in 25 hips. At an average follow-up of 18 months, the success rate for stage I was 37.5% (3 of 8); for stage II, 45.5% (5 of 11); and for stage III, 0% (0 of 6).10
Smith et al 1995 reported their results in 114 patients (follow-up, 40 months) using the modified Ficat staging system. They reported a success rate of 84% (27 of 32) for stage I, 47% (18 of 38) for stage IIA (same as Ficat II), 20% (5 of 20) for stage IIB (crescent sign), and 0% (0 of 19) for stage III (collapse of the femoral head).11 Our results are similar to Ficat and Smith but differ from that of Camp and Colwell.
5. Conclusion
Though our series is small we can suggest that MRI grading along with clinical features put together can give accurate prognosis for the outcome of Core decompression and bone grafting that may provide satisfactory result when patients are carefully selected.
Conflicts of interest
All authors have none to declare.
Acknowledgement
It is indeed a great pleasure to recall all the people who have helped us in completion of this study. We attempt to thank a select few, who have helped me in diverse ways. We owe our gratitude to the institute (Smt. Bhikhiben Kanjibhai Shah Medical Institute & Research Centre) for permitting us to undertake this study. Our sincere thanks to all our post-graduate colleagues, for their whole-hearted support during the study period. We express our thanks to all those patients without whose co-operation, this study would not have been possible.
References
- 1.Mont M.A., Hungenford D.S. Non traumatic osteonecrosis of the femoral head: ten year later-current consepts review. J Bone Joint Surg Am. 2006;88:1107–1129. doi: 10.2106/JBJS.E.01041. [DOI] [PubMed] [Google Scholar]
- 2.Bradway J.K., Morrey B.F. The natural history of the silent hip in bilateral atraumatic osteonecrosis. J Arthroplasty. 1993;8:383–387. doi: 10.1016/s0883-5403(06)80036-7. [DOI] [PubMed] [Google Scholar]
- 3.Glimcher M.J., Kenzora J.E. The biology of osteonecrosis of the human femoral head and its clinical implications: part III, discussion of the etiology and genesis of the pathological sequelae; comments on treatment. Clin Orthop Relat Res. 1979;140:273–312. [PubMed] [Google Scholar]
- 4.Mankin H.J., Brower T.D. Bilateral idiopathic aseptic necrosis of the femur in adults: a Chandler's disease. Bull Hosp Joint Dis. 1962;3:23. [PubMed] [Google Scholar]
- 5.Shannon B.D., Trousdale R.T. Femoral osteotomies for avascular necrosis of the femoral head. Clin Orthop Relat Res. 2004;418:34–40. doi: 10.1097/00003086-200401000-00007. [DOI] [PubMed] [Google Scholar]
- 6.Babhulkar Sudhir. Osteonecrosis of femoral head: treatment by core decompression and vascular pedicle grafting. Indian J Orthop. 2009;43:27–35. doi: 10.4103/0019-5413.45320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lavernia Carlos J., Sierra Rafael J. Core decompression in atraumatic osteonecrosis of the hip. J Arthroplasty. 2000;15 doi: 10.1016/s0883-5403(00)90132-3. [DOI] [PubMed] [Google Scholar]
- 8.Mont M.A., Carbone J.J., Fairbank A.C. Core decompression vs. non-operative management for avascular necrosis of the femoral head. Clin Orthop Relat Res. 1996;324:169–178. doi: 10.1097/00003086-199603000-00020. [DOI] [PubMed] [Google Scholar]
- 9.Ficat R.P. Idiopathic bone necrosis of the femoral head: early diagnosis and treatment. J Bone Joint Surg. 1985;67B:3–9. doi: 10.1302/0301-620X.67B1.3155745. [DOI] [PubMed] [Google Scholar]
- 10.Camp J.F., Calwelf C.W. Core decompression of the femoral head for osteonecrosis. J Bone Joint Surg Am. 1986;68:1313–1319. [PubMed] [Google Scholar]
- 11.Smith S.W., Fehning T.K., Griffin W.L., Beaver W. Core decompression of the osteonecrotic femoral head. J Bone Joint Surg Am. 1995;77:674. doi: 10.2106/00004623-199505000-00003. [DOI] [PubMed] [Google Scholar]


