Abstract
Objective
Fractures of patella constitute 1% of all fractures. Various techniques have been described for internal fixation of patella fractures. Superiority of one technique over the other has long been debated. We reviewed a series of fifty-one patients with transverse or comminuted fractures of patella treated with a novel technique to assess if it had any advantages over the existing methods of fixation.
Design
Retrospective.
Setting
A tertiary care centre.
Patients & methods
Fifty-one patients with patella fracture OTA 34C, with a mean age of 39 years (range 18–61) were treated with technique of cerclage and two tension bands at our institute. Forty-eight patients completed the study.
Main outcome measurements
Range of Motion and evidence of radiological union were assessed at regular follow-ups.
Results
Forty-four out of forty-eight patients had gained up-to 90 degrees of active flexion at the end of 1 week. Two patients (4.2%) developed superficial infection. All fractures had united at the end of 12 weeks. Five patients (10.3%) underwent a second surgery; four (8.3%) due to implant related complications. Malunion or non-union was not noted in any of the cases.
Conclusion
The advantages of the described method are early mobilization, elimination of k-wire related complications, and ease of use in comminuted fracture pattern as well and a lower reoperation rates as compared to the available literature. We strongly recommend its use in cases of displaced comminuted/transverse fractures of patella as an alternate method of treatment.
Level of evidence
Level III.
Keywords: Patella fracture, Tension band, Cerclage wiring, k-wire related complications
1. Introduction
Fractures of patella constitute 1% of all fractures.1 Displaced fractures with disruption of the extensor mechanism of knee require operative treatment.2 Various techniques have been described for internal fixation of patella fractures, except for severely comminuted fractures that require partial or total patellectomy. Of the various techniques described, cerclage wiring has been used for many years, however when used alone it is not rigid enough to allow early mobilisation.3 Schauwaker was the first to describe a fixation technique involving open figure of eight wiring of patella.4 The Tension band technique provides strong fixation for transverse fractures. Modification of this method using two longitudinal Kirschener wires(k-wires) has been described as the method of choice by some authors.5 But this technique is associated with complications due to k-wires.6 Subsequently, Pyrford technique was described as a combination of cerclage wiring and anterior tension band principle.4 Superiority of any one technique over the other has long been debated.
We reviewed a series of fifty-one patients with transverse as well as comminuted fractures of patella treated at our hospital with a combination of Pyrford and Schauwaker's “figure of eight” tension band (which is used in Modified AO method as well). Though both of these techniques have been previously described in literature, the aim of combining these two techniques was to eliminate the need of k-wires and their associated complications thus reducing the re-operation rate and to sufficiently strengthen the fixation allowing early mobilisation. The aim of this study was to evaluate the advantages of combining the technique of cerclage wiring with an anterior box type tension band and a figure of eight tension band.
2. Materials & methods
Out of the seventy eight patients of patella fracture treated at our institute from 1991 to 2013, fifty-one patients were treated with the technique of cerclage and two tension band wires, and are included in the study. Thirty seven were males and fourteen were females. The mean age of the patients was 39 (19–61) years. Fracture occurred on the right knee in 29 patients and on left knee in 22 patients. The most common mode of injury was involvement in motor vehicular accident. All the fractures included were closed injuries. The series included comminuted and transverse fractures in near equal numbers with or without separation of fracture fragments. All the fractures belonged to OTA class 34 C.7
Surgery was performed with patients under general or spinal anaesthesia, in supine position with the injured knee extended. A longitudinal midline incision was taken over the patella. After incising the superficial fascia, the extensor apparatus was exposed and any tear in the extensor retinaculum was identified. A 16-gauge needle was passed through the quadriceps, superior to the patella from lateral to medial side as close to the patella as possible. 1 mm gauge stainless steel wire was then passed through the needle exiting at the other end. The procedure was repeated with the needle placed along the medial, inferior and lateral aspects of patella through the corresponding needle entry site, and the wire was railroaded through it as described (Fig. 1).
Fig. 1.
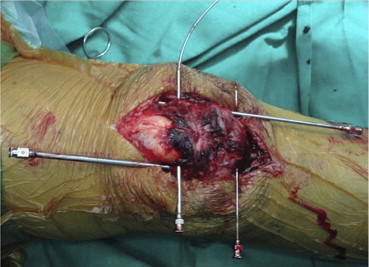
Showing the railroad technique of inserting cerclage wire.
At the end of the procedure the wire ends were next to each other at the supero-lateral corner of the patella. Articular reduction was held with a patellar clamp. The cerclage wire was then tightened to prevent further displacement of the fragments. Two wires were then passed proximally through the quadriceps tendon and distally through the patellar tendon, first in a box pattern and the second wire in a figure of eight pattern (Figs. 2–3).
Fig. 2.
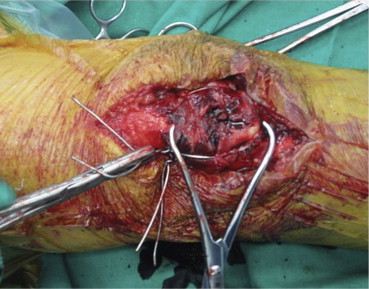
Showing anterior tension band in box pattern.
Fig. 3.
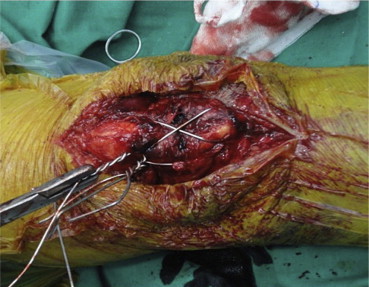
Showing anterior tension band in figure of 8 pattern.
During tightening of the tension band wires, congruity of the articular surface was checked by palpating the retropatellar surface and also under the image intensifier. The tightened wire knots were buried under the soft tissue at the superolateral corner of the patella to prevent impingement related problems post-operatively. The stability of fixation was assessed by bending the knee and looking for any opening under image intensifier.
In the post-operative period, immediate protected knee bending exercises were started and the patients were allowed to bear weight fully as per pain tolerance. The patients were then subsequently followed-up at 1, 4, 8, 12 weeks, 6 months and 1 year.
3. Results
Out of the fifty-one patients included in this study, three were lost to follow up. The mean follow up was 38(15–70) months. A total of forty-eight patients were available for follow-up and were assessed.
Forty-four out of forty-eight patients gained up to 90 degrees of active flexion at the end of the first week. Fifteen patients (31.25%) had 10–15 degrees of extensor lag at the end of the first week which improved after vigorous physiotherapy and none of them had any residual extensor lag at the subsequent follow-up. Four patients (8.3%) developed post-operative knee stiffness. They were managed with Continued Passive Motion machines; active static and dynamic quadriceps exercises and were re-assessed at the 4 weeks follow-up. Two out of the four patients achieved the desired range of motion by then and the remaining two were then subjected to manipulation under general anaesthesia (MUGA) at 4 weeks follow-up. At 12 weeks follow-up, all the patients had full range of movement and could walk, squat, climb up and down stairs without any restrictions (Figs. 4 and 5) (See Table 1). No patient had early displacement after operative fixation.
Fig. 4.

Clinical photograph of range of extension at 12 weeks follow-up.
Fig. 5.

Clinical photograph of range of flexion at 12 weeks follow-up.
Table 1.
Sequential gain in range of motion at subsequent follow-ups.
| Range of motion (in degrees) | Number of patients |
||
|---|---|---|---|
| At 1 week | At 4 weeks | At 12 weeks | |
| < or =50 | 0 | 0 | 0 |
| 51–70 | 3 | 0 | 0 |
| 71–90 | 1 | 2 | 0 |
| 91–110 | 33 | 17 | 0 |
| 111–130 | 11 | 29 | 48 |
Two patients (4.2%) had superficial infection in the post-operative period. One of them healed well with local mupirocin ointment while the other required wash-out, debridement and resuturing of the wound. This superficial infection did not affect the union time.
All the fractures achieved union by the end of 12 weeks like in Figs. 6–8.
Fig. 6.

Preoperative radiograph of patella fracture in a 46 year female.
Fig. 7.
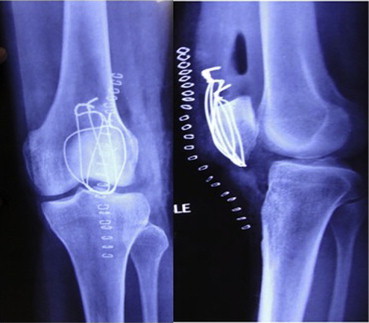
Twenty-four hours postoperative radiograph of patella fracture in a 46 year female.
Fig. 8.
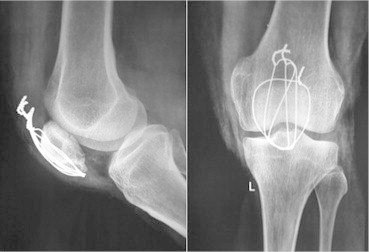
Radiograph showing union at 12 weeks in patella fracture in a 46 year female.
At 1 year follow up three patients (6.3%) had one or more broken wires in the radiographs without any implant related symptoms but union had already been achieved till then. Two patients out of those three opted for implant removal and were operated.
Complications, such as malunion or non-union were not encountered in any of the patients. Two patients underwent implant removal for irritation due to the wire ends at two and three years after the initial surgery respectively.
4. Discussion
A consensus on the ideal method of fixation for patella fractures does not exist. Weber et al. emphasized that cerclage wiring alone was not strong enough to allow early mobilisation, hence prolonged post-operative immobilisation was needed.3 Thus there was a need of a method of fixation that allowed early post-operative mobilization.
Subsequently, surgeons from Rowley Bristow Orthopaedic Hospital, Pyrford described the combination of cerclage wiring and tension band wiring for patella fractures. The Pyrford technique led to a greater strength of fixation, certainly enough to allow early mobilisation.4
Benjamin et al. compared three methods of patellar fixation (Lotke's wiring, Magnusson's wiring and Modified AO technique) and concluded that modified AO tension band wiring is the most stable fixation for patella fractures.6 However, this technique led to k-wire related complications post-operatively like backing out of wires, pain and irritation due to k-wires.8 These complications left the surgeon in dilemma of removing the implant and risking non-union or leaving it inside with the concomitant patient suffering.
Curtis, in a cadaveric study compared the AO method to the Pyrford technique using a cerclage wire and an anterior tension band wire looping through the quadriceps tendon.4 He found that while the AO technique is adequate for most cases, the Pyrford technique led to a greater strength of fixation. The Pyrford technique can also be applied to a comminuted fracture of the patella, which can be difficult to fix with interfragmentary k-wires and a simple tension band.
Symptomatic implant irritation is the most commonly reported complication following fixation of a patellar fracture. Rates of implant removal for symptomatic hardware have ranged from 0% to 50%.8 Although symptomatic implant irritation is not as serious a complication as fixation failure or postoperative infection, it does require the patient to undergo a second operation, which carries inherent surgical risk and increases the overall cost of fracture care.9 Thus a method needs to be devised by which the re-operation rates can be decreased without compromising the union rates. Although there was crowding of the wire knots at the supero-lateral pole of patella in the above described method, but it led to symptomatic implant irritation in only two (4.2%) cases and only four patients (8.3%) underwent second surgery due to implant related complications.
No large study has directly compared the rates of implant removal for specific fixation constructs.10–13 Dy et al. in their metanalysis involving 737 patella fractures fixed with various fixation techniques, reported an infection rate of 3.2%, a non-union rate of mere 1.3% and substantial re-operation rate of 34% after patella fracture fixation.9 The high reoperation rate was attributed to the use of k-wires in the construct. In this study we had a reoperation rate of less than 10.4% which is lower as compared to the available literature.
In summary, with the various methods described in the literature having their own share of merits and demerits, we describe a combination of two fixation methods, the Pyrford technique and the Schauwker's ‘figure of eight’ tension band technique. The advantages of the described method are early mobilization, elimination of k-wire related complications, lower re-operation rates and ease of use in comminuted fracture pattern as well. We strongly recommend its use in cases of displaced comminuted transverse fractures of patella as an alternative method of treatment.
Conflicts of interest
All authors have none to declare.
References
- 1.Campbell W.C., Canale S.T. 2008. Campbell's Operative Orthopaedics; p. 1. [Google Scholar]
- 2.Yang K.H., Byun Y.S. Separate vertical wiring for the fixation of comminuted fractures of the inferior pole of the patella. J Bone Jt Surg Br. 2003 Oct 31;85:1155–1160. doi: 10.1302/0301-620x.85b8.14080. [DOI] [PubMed] [Google Scholar]
- 3.Weber M.J., Janecki C.J., McLeod P., Nelson C.L. Efficacy of various forms of fixation of transverse fractures of the patella. J Bone Jt Surg Am. 1980 Mar;62:215–220. [PubMed] [Google Scholar]
- 4.Curtis M.J. Internal fixation for fractures of the patella. A comparison of two methods. J Bone Jt Surg Br. 1990 Mar;72:280–282. doi: 10.1302/0301-620X.72B2.2312569. [DOI] [PubMed] [Google Scholar]
- 5.Ruedi T.P. Thieme; 2007. AO Principles of Fracture Management; p. 1. [Google Scholar]
- 6.Benjamin J., Bried J., Dohm M. Biomechanical evaluation of various forms of fixation of transverse patellar fractures. J Orthop Trauma. 1987;1:219–222. doi: 10.1097/00005131-198701030-00004. [DOI] [PubMed] [Google Scholar]
- 7.Marsh J.L., Slongo T.F., Agel J. Fracture and dislocation classification compendium - 2007: orthopaedic trauma association classification, database and outcomes committee. J Orthop Trauma. 2007;21:S1. doi: 10.1097/00005131-200711101-00001. [DOI] [PubMed] [Google Scholar]
- 8.Hoshino C.M., Tran W., Tiberi J.V. Complications following tension-band fixation of patellar fractures with cannulated screws compared with Kirschner wires. J Bone Jt Surg Am. 2013 Apr;95:653–659. doi: 10.2106/JBJS.K.01549. [DOI] [PubMed] [Google Scholar]
- 9.Dy C.J., Little M.T.M., Berkes M.B. Meta-analysis of re-operation, nonunion, and infection after open reduction and internal fixation of patella fractures. J Trauma Acute Care Surg. 2012 Oct;73:928–932. doi: 10.1097/TA.0b013e31825168b6. [DOI] [PubMed] [Google Scholar]
- 10.Melvin J.S., Mehta S. Patellar fractures in adults. J Am Acad Orthop Surg. 2011 Apr;19:198–207. doi: 10.5435/00124635-201104000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Lotke P.A., Ecker M.L. Transverse fractures of the patella. Clin Orthop Relat Res. 1981 Jul:180–184. [PubMed] [Google Scholar]
- 12.Torchia M.E., Lewallen D.G. Open fractures of the patella. J Orthop Trauma. 1996;10:403–409. doi: 10.1097/00005131-199608000-00007. [DOI] [PubMed] [Google Scholar]
- 13.Catalano J.B., Iannacone W.M., Marczyk S. Open fractures of the patella: long-term functional outcome. J Trauma: Inj Infect Crit Care. 1995 Sep;39:439–444. doi: 10.1097/00005373-199509000-00007. [DOI] [PubMed] [Google Scholar]


