Abstract
Background
Open reduction and internal fixation (ORIF) is the treatment of choice for displaced intra-articular calcaneal fracture at many orthopaedic trauma centres. In this prospective study, we evaluated the functional outcome and complications of locking compressive calcaneum plate for displaced intra-articular fracture calcaneum.
Methods
Between October 2011 and March 2012, 30 patients with displaced intra-articular fracture calcaneum attending the outdoor and emergency of our institute were included in the study. All the included patients were operated using standard lateral approach and followed up to 1 year.
Results
Of 30 patients, 14 (48%) patients were Sander's type II, 10 (33%) were type III, and 6 (20%) were type IV. All the patients were evaluated post-operatively. Articular surface of posterior facet of calcaneum and crucial angle of Gissane was maintained in all patients. Four patients had post-operative Boehler's angle <20° and 26 patients had between 21° and 40°. All the patients having post-operative Boehler's angle <20° were type IV as compared to types II and III (statistically significant). Ninety-six percentage of patients having post-operative Boehler's angle 21–40° were more satisfied at 1 year as compared to 25% of patients having post-operative Boehler's angle <20° (statistically significant). Complications were present in 6 (20%) patients.
Conclusion
ORIF with locking compressive plate in displaced intra-articular fracture calcaneum gives good outcome. Results are more favourable in less comminuted as compared to more comminuted. Maintenance of Boehler's angle is also necessary for satisfactory results along with maintenance of articular congruence of posterior facet of calcaneum and crucial angle of Gissane.
Keywords: Maryland foot score, Intra-articular calcaneal fracture, Locking calcaneal plate
1. Introduction
Calcaneal fracture is comparatively a rare injury, with reported occurrence of 2% of all fractures. The intra-articular type constitutes 75% of calcaneal fracture.1–3 These fractures occur due to axial force in the axis of crus due to vertical fall from height when processus lateralis tali impacts as a hammer on the area of Gissane's vertex and then breaks through the posterior articular facet. The functional outcome of foot after such a fracture is poor.1–3
Controversy remains with respect to whether displaced intra-articular calcaneal fracture ought to be treated operatively or non-operatively.4–9 Historically, displaced intra-articular fracture and calcaneal fractures were treated conservatively, as predictable operative reduction and fixation were not possible.7,8,11 Operative treatment became more popular, as fracture care improved.12–15 Reviews on this subject, however, have failed to demonstrate indisputable superior results of a single line of treatment for displaced intra-articular calcaneal fracture.10,14,16–18
The locking compression plate has improved the functional results, limited indications for bone grafting and shortened recovery time, i.e. decreased morbidity.4,5 The purpose of our study was to evaluate the functional outcome and complications of fracture treated with calcaneal-locking compression plate in Indian population.
2. Materials and methods
2.1. Design of the study
This was a prospective interventional study.
Thirty patients of age group 18–50 years attending to Orthopaedics Emergency and the Out Patient Department of our institute, with fracture of the calcaneus without any other life threatening injury were included in the study after thorough clinical and radiological examination. Informed written consent was obtained from the patients prior to inclusion in the study.
All the patients with fracture of intra-articular calcaneum that were included in the study were selected according to the following inclusion criteria.
2.1.1. Inclusion criteria
-
1.
Displaced intra-articular fracture involving posterior facet.
-
2.
Fracture of anterior process of calcaneum with more than 25% involvement of calcaneo-cuboid joint.
-
3.
Displaced fracture of calcaneal tuberosity.
-
4.
Fracture – dislocation of calcaneus.
2.1.2. Exclusion criteria
The factors amounting to exclusion are given as follows:
-
a.
Nondisplaced or minimally displaced extra-articular fractures.
-
b.
Fractures in patients with peripheral vascular disease, diabetes mellitus, bleeding disorders and neuropathic foot.
-
c.
Grossly contaminated wound.
-
d.
Pathological fracture of calcaneum.
2.2. Pre-op evaluation
After admission, the patients were worked up clinically and radiologically, and they underwent routine investigations and pre-anaesthetic check-up. The following were considered: X-ray calcaneum anteroposterior view to assess involvement of calcaneocuboid joint and fracture of anterior process, lateral view (Figs. 1 and 2) to assess Boehler's angle and crucial angle of Gissane and Harris-heel axial view X-ray to assess posterior articular facet along with a CT-scan calcaneum in sagittal (Figs. 3 and 4) and axial plane (Fig. 5) with 3D reconstruction to assess and classify the fracture according to Sander's classification.
Fig. 1.

(Case 1) Pre-op X-ray calcaneum lateral view.
Fig. 2.

(Case 2) Pre-op X-ray calcaneum lateral view.
Fig. 3.
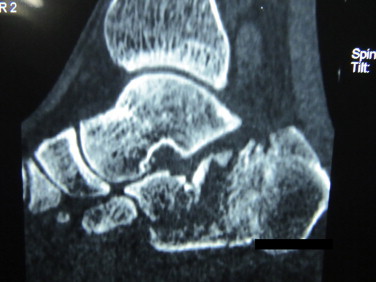
(Case 1) Pre-op CT-scan calcaneum – sagittal plane.
Fig. 4.
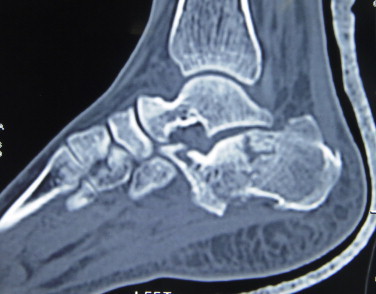
(Case 2) Pre-op CT-scan calcaneum – sagittal plane.
Fig. 5.
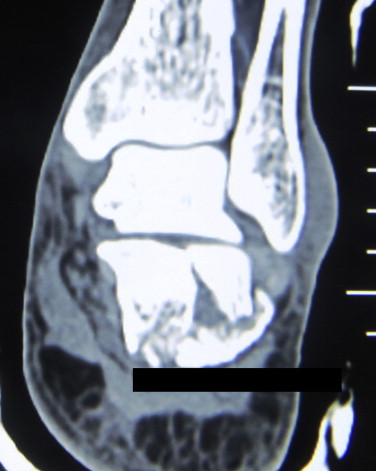
(Case 2) Pre-op CT scan calcaneum – axial plane.
2.3. Procedure
All surgeries were performed under anaesthesia with the patient in lateral position. The affected limb was cleaned, painted and draped.
In all patients, calcaneum was approached through lateral approach. An L-shaped skin incision given with vertical limb extends from 2 cm above the tip of lateral malleolus, just lateral to the Achilles tendon continued vertically towards the plantar surface of heel, and horizontal limb extends from base of fifth metatarsal anteriorly to meet the vertical limb posteriorly at the junction of skin and heel. Thick single layered flap elevated, calcaneo-fibular ligament incised and peronei tendons subluxed to expose the subtalar joint completely. After a complete exposure of subtalar joint, the flap was retracted with the help of three k-wires inserted at lateral malleoli, neck of talus and at the base of fifth metatarsal. Subtalar joint was exposed; fracture was assessed and reduced along with correction and maintenance of Boehler's angle and crucial angle of Gissane. Fracture was fixed internally with locking calcaneal plate without bone grafting. k-Wires were removed and wound was closed meticulously with monofilament suture using Allgower–Donati technique.
The limb was immobilized in below knee posterior splint. Strict limb elevation was maintained and patients were asked to do active toe movement to avoid swelling.
2.4. Post-operative plan
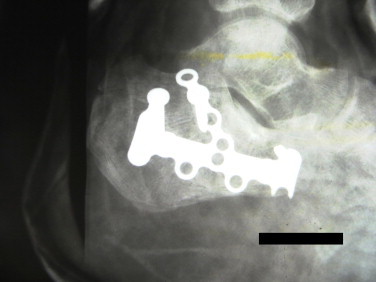
The patient was given post-operative dose of second or third generation cephalosporin and aminoglycoside. First post-operative wound inspection was done at 3rd to 5th day. Post-op X-rays were taken (Figs. 6 and 7). Active range of motion exercises of ankle and subtalar joint were started in 2nd post-op week. Stitches were removed after 3 weeks.
Fig. 6.

(Case 1) Post-op X-ray calcaneum lateral view.
Fig. 7.

(Case 2) Post-op X-ray calcaneum lateral view.
Till 12 weeks, patients were allowed for non-weight bearing walking only. Weight bearing allowed after 12 weeks.
Patients were followed up at 3 weeks, 6 weeks, 12 weeks (Fig. 8), 6 months and 1 year by radiographs (Figs. 9 and 10) and clinically using Maryland foot score.
Fig. 8.
(Case 2) Follow-up at 3-month X-ray calcaneum lateral view.
Fig. 9.

(Case 1) Follow-up at 1-year X-ray calcaneum lateral view.
Fig. 10.

(Case 1) Follow-up at 1-year X-ray calcaneum axial view.
3. Results
Mean age of patients in our study was 35.5 ranging from 18 to 50 years. Out of 30 patients in our study 23 (77%) were males and 7 (23%) were females. All the patients had a fall from height as a mode of injury. Average duration between injury and surgery was 11 days with a range between 8 and 17 days and a standard deviation of 2.12 days. Out of total 30 patients, 14 (47%) were Sander's type II, 10 (33%) were type III and 6 (20%) were type IV. Out of 30 patients 4 (13%) had Boehler's angle <20° and 26 (87%) patients had Boehler's angle of 21–40° post-operatively. Crucial angle of Gissane and articular congruence of posterior facet was obtained. Patients were evaluated both radiologically by radiographs and clinically using Maryland foot score. All the patients had an improvement in the functional score with time, with mean score of 53.9 at 6 weeks, 63.3 at 12 weeks, 83 at 6 months and 93.7 at 1 year (Graph 1). At 1 year of follow-up 26 (87%) patients were satisfied with excellent results (functional score >90), 4 (13%) patients were not satisfied with functional score <75. Out of 30 patients, 24 patients had no complications and 6 (20%) had complications (delayed wound healing in 1, stiffness of ankle and subtalar joint in 2 and 3 patients having pain and implant prominence).
Graph 1.
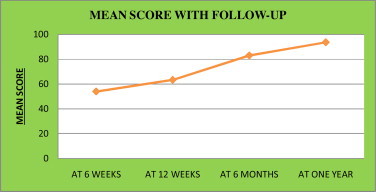
Mean score with follow-up.
There was a significant correlation between the type of fracture and post-operative Boehler's angle obtained. The proportion of patients having Boehler's angle <20° were more in Sander's type IV as compared to types II and III (Table 1) (sig. two-tailed test values 0.005 and 0.008, i.e. significant).
Table 1.
Correlation of type of fracture (Sander's classification) to post-operative Boehler's angle (sig. two-tailed test values 0.005 and 0.008), i.e. significant.
| Post-operative Boehler's angle ≤20° |
Post-operative Boehler's angle 21–40° |
|
|---|---|---|
| Sander's type II | 1 (25%) | 13 (50%) |
| Sander's type III | 1 (25%) | 9 (34.6%) |
| Sander's type IV | 2 (50%) | 4 (15.4%) |
| Total | 4 (100%) | 26 (100%) |
There was a significant correlation between post-operative Boehler's angle and final outcome, i.e. functional score at 1 year (Table 2). Proportion of patients having satisfactory result at 1 year were more in group having Boehler's angle 21–40° as compared to group having Boehler's angle <20° (significant, standard error difference of means, p value < 0.05).
Table 2.
Correlation of post-operative Boehler's angle to functional outcome at 1 year (standard error of difference of proportion, p value < 0.05), i.e. significant.
| Maryland foot score <90 | Maryland foot score >90 | Total | |
|---|---|---|---|
| Post-operative Boehler's angle <20° |
3 (75%) | 1 (25%) | 4 (100%) |
| Post-operative Boehler's angle 21–40° |
1 (4%) | 25 (96%) | 26 (100%) |
4. Discussion
In the last few decades, operative treatment of displaced intra-articular calcaneal fracture has become a preferred treatment method with low complication rate and better quality of life after the surgery.1–3,19–26 The method has been improved by implanting locking compressive plate, the osteosynthesis is more stable, to enable early weight bearing and bone grafting is rarely required.4,5,23,26 Brauer's cost effectiveness analysis of surgery versus conservative treatment for intra-articular calcaneal fracture showed economical advantages of open reduction internal fixation2 in 2004.
In our study only 6 (20%) patients had complications. These were superficial wound healing problem, pain and implant prominence. In other studies, complication rate was as high as 25%. The follow-up period in our study was 1 year, which could be a possible difference, due to which late complications could not be included in our study. Moreover with passage of time, the literature had helped us understand the fracture and improve the surgical skills of surgeon further leading to decreased complications.
In our study, we confirm the benefit of locking compressive plate implant in fracture calcaneum by assessing the patients in follow-up by both radiologically by radiographs and functional evaluation using Maryland foot score.
At 6th week, the mean score was 53.7, i.e. Fair. Twenty-eight (93%) patients had Fair (score 51–75) and 2 (7%) had Failure (score <50). This could be because of complication, i.e. delayed wound healing and pain. At 12th week, 29 (97%) had Fair results with mean score of 63.3. Both patients having Failure results improved to Fair because of resolution of pain and healing of stitch line. At 1 year, 29 (97%) had gained excellent results (score 91–100). All the patients had improvement in score and satisfaction after surgery in long-term.
We operated in the first 2 weeks of injury, because the surgery in 3rd week of injury is associated with high percentage of soft tissue healing complications, and open reduction internal plate fixation with more than 3 weeks delay is not recommended.1,4,19,20,22,25
In our study, we confirm the correlation between post-operative Boehler's angle size and patient's satisfaction, as well as articular congruence. This fact is verified and confirmed by a lot of authors.21,22 Loucks, in his prospective randomized study, pointed out that initial negative size of Boehler's angle negatively influences the post-operative results.26
In our opinion, there is no indication of bone grafting except Sander'S type IV injury with huge defect after reduction. Longino had compared post-operative radiological and clinical results of locking compressive plate osteosynthesis with and without bone grafting and found no significant difference between two groups.23 In accordance with other authors, for intra-articular calcaneal fracture treatment, we emphasize perfect posterior facet fragment reduction in subtalar joint, restoration of calcaneal height width and length with restoration of Boehler's angle along with crucial angle of Gissane. Inaccurate reduction and malposition lead to persistent complaints.
Well-timed open reduction and internal fixation (ORIF) with locking compressive plate in an indicated case, with respect to soft tissue envelope and early rehabilitation, leads to therapeutic success. We, through our study and by reviewing the literature, concluded that locking compressive calcaneal plate, being a low profile, mouldable, multiplanar with locking screws, gives satisfactory results with improved functional outcome and less complications.
Conflicts of interest
All authors have none to declare.
References
- 1.Zwipp H., Rammelt S., Barthell S. Fracture of the calcaneus. Unfallchirug. 2005;108:737–748. doi: 10.1007/s00113-005-1000-6. [DOI] [PubMed] [Google Scholar]
- 2.Brauer C.A., Manns B.J., Ko M., Donaldson C., Buckley R. An economic evaluation of operative compared with nonoperative management of displaced intra-articular calcaneal fractures. J Bone Joint Surg. 2005;87:2471–2479. doi: 10.2106/JBJS.E.00166. [DOI] [PubMed] [Google Scholar]
- 3.Lim E.A., Leung J.P. Complications of intra-articular calcaneal fracture. Clin Orthop Relat Res. 2001;391:7–16. doi: 10.1097/00003086-200110000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Rammelt S., Amlang M., Barthel S., Zwipp H. Minimally-invasive treatment of calcaneal fractures. Injury. 2004;35:SB55–SB63. doi: 10.1016/j.injury.2004.07.012. [DOI] [PubMed] [Google Scholar]
- 5.Sanders R. Current concepts review displaced intra-articular fractures of the calcaneus. J Bone Joint Surg. 2000;82:225–250. doi: 10.2106/00004623-200002000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Palmer I. The mechanism and treatment of fractures of calcaneus. Open reduction with the use of cancellous graft. J Bone Joint Surg Am. 1948;30:2–8. [PubMed] [Google Scholar]
- 7.Lindsay R., Dewar F. Fractures of the os calcis. Am J Surg. 1958;95:555–576. doi: 10.1016/0002-9610(58)90438-0. [DOI] [PubMed] [Google Scholar]
- 8.Rowe C., Sakellarides H., Freeman P., Sorbie C. Fractures of the os calcis. JAMA. 1963;184:920–923. [Google Scholar]
- 9.Jarvholm U., Korner L., Thoren O., Wiklund L.M. Fracture of the calcaneus. A comparison of open and closed treatment. Acta Orthop Scand. 1984;55:652–656. doi: 10.3109/17453678408992416. [DOI] [PubMed] [Google Scholar]
- 10.Giachino A.A., Uthoff H.K. Intra-articular fracture of calcaneus. J Bone Joint Surg Am. 1989;71:784–787. [PubMed] [Google Scholar]
- 11.Pozo J.L., Kirwan E.O., Jackson A.M. The long-term results of conservative management of severely displaced fractures of calcaneus. J Bone Joint Surg Br. 1984;66:386–390. doi: 10.1302/0301-620X.66B3.6725350. [DOI] [PubMed] [Google Scholar]
- 12.Stephenson J.R. Displaced fractures of the os calcis involving the subtalar joint: the key role of superomedial fragment. Foot Ankle. 1983;4:91–101. doi: 10.1177/107110078300400210. [DOI] [PubMed] [Google Scholar]
- 13.Hammesfahr J.F. Surgical treatment of calcaneal fractures. Orthop Clin North Am. 1989;20:679–689. [PubMed] [Google Scholar]
- 14.Sanders R. Intra-articular fractures of calcaneus: present state of the art. J Orthop Trauma. 1992;6:252–265. doi: 10.1097/00005131-199206000-00022. [DOI] [PubMed] [Google Scholar]
- 15.Leung K.S., Yuen K.M., Chan W.S. Operative treatment of displaced intra-articular fracture of calcaneum. Medium-term results. J Bone Joint Surg Br. 1993;75:196–201. doi: 10.1302/0301-620X.75B2.8444936. [DOI] [PubMed] [Google Scholar]
- 16.Sanders R. Displaced intra-articular fractures of the calcaneus. J Bone Joint Surg Am. 2000;82:225–250. doi: 10.2106/00004623-200002000-00009. [DOI] [PubMed] [Google Scholar]
- 17.Zwipp H., Tscherne H., Thermann H., Weber T. Osteosynthesis of displaced intraarticular fracture of the calcaneus. Results in 123 cases. Clin Orthop. 1993;290:76–86. [PubMed] [Google Scholar]
- 18.Thordarson D.B., Krieger L.E. Operative vs. nonoperative treatment of intra-articular fractures of the calcaneus: a prospective randomized trial. Foot Ankle Int. 1996;17:76–86. doi: 10.1177/107110079601700102. [DOI] [PubMed] [Google Scholar]
- 19.Rammelt S., Zwipp H. Calcaneus fractures. Trauma. 2006;8:197–212. [Google Scholar]
- 20.Zwipp H., Rammelt S., Barthel S. Calcaneal fractures – open reduction and internal fixation (ORIF) Injury. 2004;35:SB46–SB54. doi: 10.1016/j.injury.2004.07.011. [DOI] [PubMed] [Google Scholar]
- 21.Buckley R. Letters to the Editor. J Orthop Trauma. 2002;16:210–211. [Google Scholar]
- 22.Hart A.J., Eastwood D.M. Displaced intra-articular fractures of the calcaneus: what is new? Trauma. 2003;5:9–21. [Google Scholar]
- 23.Longino D., Buckley R.E. Bone graft in the operative treatment of displaced intraarticular calcaneal fractures: is it helpful? J Orthop Trauma. 2001;15:280–286. doi: 10.1097/00005131-200105000-00008. [DOI] [PubMed] [Google Scholar]
- 24.Simpson R.B. Fractures of the calcaneus. Curr Opin Orthop. 2007;18:124–127. [Google Scholar]
- 25.Benirschke S.K., Kramer P.A. Wound healing complications in closed and open calcaneal fractures. J Orthop Trauma. 2004;18:1–6. doi: 10.1097/00005131-200401000-00001. [DOI] [PubMed] [Google Scholar]
- 26.Loucks C., Buckley R. Bohler's angle: correlation with outcome in displaced intra-articular calcaneal fractures. J Orthop Trauma. 1999;13:554–558. doi: 10.1097/00005131-199911000-00007. [DOI] [PubMed] [Google Scholar]


