Abstract
Background
The epidemiology of femoroacetabular impingement (FAI) is important but incompletely understood, because most reports arise from symptomatic populations. Investigating the prevalence of FAI in a community-based cohort could help us better understand its epidemiology and in particular the degree to which it might or might not be associated with hip pain.
Questions/purposes
The purposes of this study were (1) to evaluate the proportion of older (≥ 65 years of age) men with morphologic abnormalities consistent with FAI; and (2) to assess the association of the morphologic abnormalities with prevalent radiographic hip osteoarthritis (OA) and hip pain.
Methods
Anteroposterior radiographs were obtained in 4140 subjects (mean age ± SD, 77 ± 5 years) from the Osteoporotic Fractures in Men study. We assessed each hip for cam, pincer, and mixed FAI types using validated radiographic definitions. Both intra- and interobserver reproducibility were > 0.9. Radiographic hip OA was assessed by an expert reader (intraobserver reproducibility, 0.7–0.8) using validated methods, and summary grades of 2 or greater (on a scale from 0 to 4) were used to define radiographic hip OA. Covariates including hip pain in the last 30 days were collected by questionnaires that were answered by all patients included in this report. Logistic regressions with generalized estimating equations were performed to evaluate the association of radiographic features of FAI and arthrosis.
Results
Pincer, cam, or mixed types of radiographic FAI had a prevalence of 57% (1748 of 3053), 29% (886 of 3053), and 14% (419 of 3053), respectively, in this group of older men. Both pincer and mixed types of FAI were associated with arthrosis but not with hip pain (odds ratio [OR], 1.63; 95% confidence interval [CI], 1.25–2.13; p < 0.001 for pincer and OR, 2.49; 95% CI, 1.65–3.76; p < 0.001 for mixed type). Patients with hips characterized by cam-type FAI had slightly reduced hip pain without the presence of arthrosis compared with hips without FAI (OR, 0.82; 95% CI, 0.68–0.99; p = 0.037). A center-edge angle > 39° and a caput-collum-diaphyseal angle < 125° were associated with arthrosis (OR, 1.53; 95% CI, 1.22–1.94; p < 0.001 and OR, 2.09; 95% CI, 1.24–3.51; p = 0.006, respectively), but not with hip pain (OR, 0.89; 95% CI, 0.77–1.03; p < 0.108 and OR, 0.99; 95% CI, 0.67–1.45; p = 0.945, respectively). An impingement angle < 70° was associated with less hip pain compared with hips with an impingement angle ≥ 70° (OR, 0.76; 95% CI, 0.61–0.95; p = 0.015).
Conclusions
FAI is common in older men and represents more of an anatomic variant rather than a symptomatic disease. This finding should raise questions on how age, activities, and this anatomic variant each contribute to result in symptomatic disease.
Level of Evidence
Level III, prognostic study.
Introduction
Recent studies have reported that morphologic abnormalities of the hip are associated with early-onset and rapidly progressive hip osteoarthritis (OA) [6, 17, 18]. Radiologic characteristics of femoroacetabular impingement (FAI) are also present in individuals without clinical symptoms either because the symptoms only develop in more advanced stages of arthrosis associated with FAI features or because FAI features in some individuals may be only an anatomic variant [38]. Radiographic features of FAI have been defined by three distinct definitions of the underlying anatomic deformity: pincer, cam, and mixed. Pincer impingement is characterized by focal or general overcoverage of the femoral head and occurs most often in middle-aged women. Cam impingement usually results from abnormal/aspheric morphology of the proximal femur and is most common in young athletic men [1]. The third type of FAI, mixed, has a combination of cam and pincer impingement characteristics [3, 14, 18, 20, 22–24, 30, 42, 43]. FAI probably results from developmental abnormalities of the femur and acetabulum such that there is abnormal contact between the head of the femur and the acetabulum [28, 32, 44].
The prevalence of FAI has been reported to range from 6% to 35%, depending on the criteria of inclusion of the population and the definitions of FAI [16]. In addition, most reports on the prevalence of FAI come from surgical populations and may not represent the prevalence in the general population [2, 16, 21]. Not only is the prevalence of FAI determined for all the ages, but, from recent studies, it is not yet clear (1) if FAI represents a normal variant or a condition associated with severe and aggressive arthritis; and (2) if this relationship changes with age [33, 34]. In young adults, FAI can be associated with severe arthroscopic degeneration of the hip, whereas in older age groups, it can be a normal variant. In addition, there are now a number of reports that describe surgery for FAI in older people (older than 50 years of age) [7, 13, 26, 41]. Therefore, it is critical to study the complete spectrum of FAI, including in older patients, as well as its association with pain and arthritis.
We therefore sought (1) to determine the prevalence of morphometric abnormalities of the hip that define radiographic FAI; and (2) to assess the association of these findings with both arthrosis and hip pain in a cohort of older men (> 65 years).
Patients and Methods
Population
From March 2000 through April 2002, 5994 community-dwelling men at six clinical centers in the United States (Birmingham, AL; Minneapolis, MN; Palo Alto, CA; Monongahela Valley [near Pittsburgh], PA; Portland, OR; and San Diego, CA) participated in the baseline examination for the Osteoporotic Fractures in Men (MrOS) study. Eligible men were at least 65 years of age without bilateral hip replacements. Details of the MrOS design and cohort have been published [8]. Subjects included in our current study were drawn from the population of 4215 MrOS participants who returned for the second clinic visit (2005–2006) and had pelvic radiographs digitized and archived [27]. The majority of the study subjects were white men with a mean age of 77 ± 5 years, who were slightly overweight, with good self-rated health. Seventy-seven percent (3216 of 4140) had at least one comorbid condition and 17% (733 of 4140) had at least one mobility limitation. Twenty-seven percent (1134 of 4140) had hip pain and 16% (675 of 4140) were using nonsteroidal antiinflammatory drugs (Table 1).
Table 1.
Characteristics of subjects from the MrOS cohort Visit 2
| Visit 2 | Whole cohort (N = 4140) |
|---|---|
| Clinical characteristics | |
| Age (years) mean ± SD | 77 ± 5 |
| BMI (kg/m2), mean ± SD | 27 ± 4 |
| Weight (kg), mean ± SD | 82 ± 14 |
| Nonwhite background, number (%) | 395 (10) |
| Self-rated health excellent/good, number (%) | 3588 (87) |
| Functional limitation, number (%) | 607 (15) |
| At least one medical condition, number (%) | 3216 (78) |
| Hip pain on either side, number (%) | 1134 (27) |
| NSAID use, number (%) | 675 (16) |
| Croft grade, number (%) | |
| 0 | 2604 (63) |
| I | 1128 (27) |
| II | 235 (6) |
| III | 126 (3) |
| IV | 46 (1) |
MrOS = Osteoporotic Fractures in Men (study); BMI = body mass index; NSAID = nonsteroidal antiinflammatory drug.
The study protocol, amendments, and informed consent documentation, including analysis plans, were reviewed and approved by the local institutional review boards.
Imaging Techniques and Analyses
Standing pelvis radiographs were taken at the second clinic visit by positioning the patient using a standardized foot mat with toes internally rotated 15° and the x-ray beam directed 2 inches above the pubis symphysis. A standardized exposure technique was used at all sites. The technique required a Bucky imaging system (Agfa, Mortsel, Belgium), 40 inches of focus-to-film distance, 70 to 80 kVp (mAs dependent on the screen/film system), large focal spot, and full size of the film collimation. In addition, a cassette size of 14 inches to 17 inches was used [12].
All images were reviewed on picture archiving communication system workstations (Agfa, Ridgefield Park, NJ, USA). The pelvis radiographs were initially checked for image quality and postsurgical changes that obstructed assessment of FAI features. Of the 4215 (8430 hips), 75 (140 hips) radiographs were excluded from the study at the time of the reading as a result of poor image quality (over-/underexposure, beam-hardening artifacts, motion degradation, and presence of supraimposed metallic structures such as belts). FAI assessment was not done on 127 hips that had previously undergone THA or previous pelvic or femoral fractures; however, the contralateral hips were included, resulting in 8263 hips available for FAI assessment. Furthermore, there were 112 hips that had one or more FAI features that did not classify them as cam, pincer, or mixed FAI; thus, they were not included in the analysis assessing FAI type. The total number of hips available for hip-based analysis was 8151. A musculoskeletal radiologist (LN) with 3 years of experience in musculoskeletal imaging assessed the pelvic AP radiographs. During the readings, cases that did not satisfy study inclusion criteria (listed previously) were excluded and, in the remaining hip radiographs, FAI measurements. Different radiologic criteria based on pelvic radiographs have been evaluated for the diagnosis of FAI [37, 46]. Among the many criteria for FAI that have been studied, the following have been reported to have high degrees of intra- and interobserver agreement on AP-view pelvis radiographs and therefore were assessed: caput-collum-diaphyseal (CCD) angle, impingement angle, and lateral center-edge (CE) angle [4, 5, 9, 10, 14, 20, 24, 25, 45, 48–51, 53] (Figs. 1–3). The CE angle was assessed (Fig. 1) according to a previously described technique [54]. A threshold of 39° was used as a sign of impingement [4]. The impingement angle was measured according to a previously described approach (Fig. 2) [15]. Cam morphology was assessed using the impingement angle and the CCD angle using < 70° [29] and < 125° as abnormal values. The other morphological sign for cam impingement is the CCD angle, defined as the angle between the longitudinal axes of the femoral neck and shaft (Fig. 3) [27].
Fig. 1.
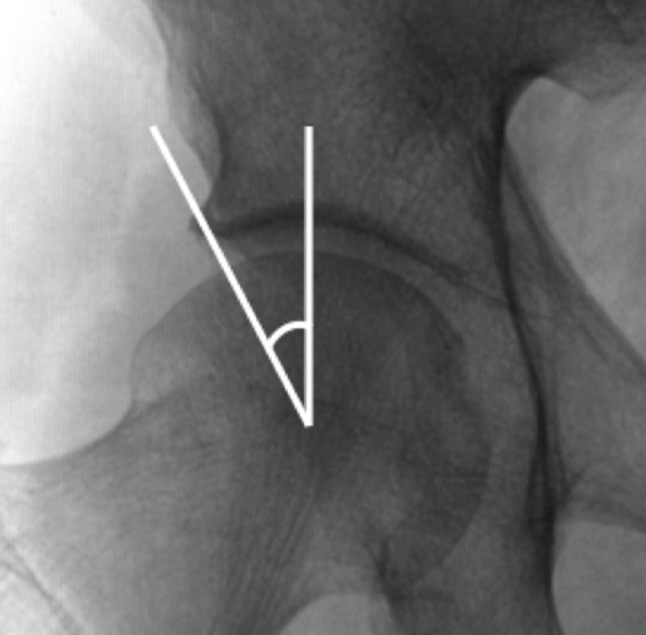
The lateral CE angle is the angle formed by a vertical line and a line connecting the femoral head center with the lateral aspect of the acetabulum.
Fig. 3.
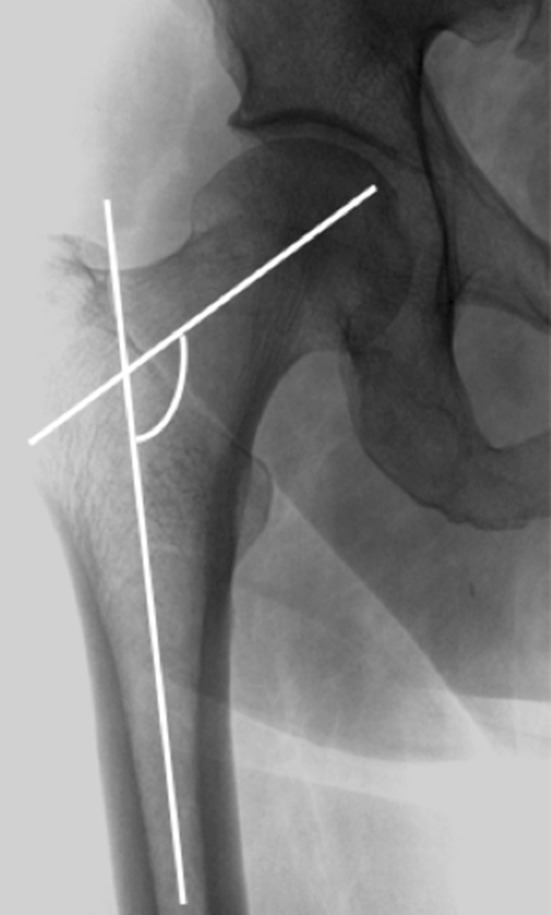
The CCD angle is the angle formed by the long axis of the femoral neck and the long axis of the femoral shaft.
Fig. 2.
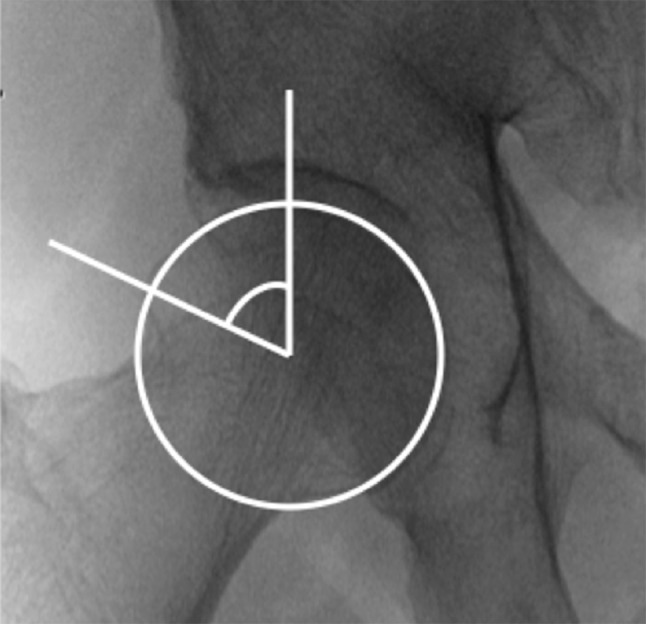
The impingement angle is the angle formed between a vertical line passing through the center of the femur head and the line connecting the center of the femoral head to the first part of the lateral femoral head, which is outside the circle encompassing the femoral head.
The hip was determined to have a radiographic morphology of pincer- or cam-type FAI if it met the diagnostic criteria for at least one diagnostic measure. Mixed-type impingement was defined as having radiographic signs of both pincer and cam FAI types for at least one measure. A normal hip was defined as having all three angles measure within normal limits.
Definition of Arthrosis
Hip radiographs were assessed for five individual radiographic features (IRFs) of arthrosis: (1) joint space narrowing (JSN; 0–4) laterally and medially; (2) osteophyte formation (0–3; femoral or acetabular and either inferiorly or superiorly in each location; (3) cysts (0–3); (4) subchondral sclerosis (0–3); and (5) femoral head deformity (0–3) [32, 44]. Atlas figures were consulted during the readings to improve reliability [44]. These methods have been validated [14, 32, 44]. A summary grade for arthrosis severity of 0 to 4, modified from Croft [4, 32], was assigned to each hip based on individual radiographic features. Grade 0 had no IRFs or was defined as normal. Grade I required either the presence of possible JSN or osteophytes (severity grade = 1). Grade II required the presence of definite (severity grade ≥ 2) JSN or osteophytes plus at least one other feature (cysts or subchondral sclerosis). Grade III required definite JSN or osteophytes plus at least two other features. Grade IV met the criteria for Grade III and also had femoral head deformity. Minimum joint space was measured in millimeters using electronic calipers [4, 11, 14, 32]. In our study, no arthrosis was found as defined by Croft Grade 0 or I, and prevalent arthrosis was defined by Croft Grades II to IV. The prevalence of Croft scores for arthrosis among study patients was distributed as: 2604 (63%), 1128 (27%), 235 (6%), 126 (3%), and 46 (1%) for Grades 0, I, II, III and IV, respectively (Table 1).
Reproducibility Analyses
After a calibration session in which 30 pelvic radiographs were evaluated by two trained musculoskeletal radiologists (LN, SL), 220 (5%) pelvic radiographs that were originally read were reread independently for inter- and intraobserver reproducibility. Reproducibility for radiographic endpoint assessments was calculated using the absolute intraclass correlation coefficient (ICC) [47]. ICC values for intraobserver agreement for the impingement angle, CE angle, and CCD angle were 0.94 (95% confidence interval [CI], 0.92–0.95), 0.98 (95% CI, 0.97–0.981), and 0.99 (95% CI, 0.99–0.99), respectively. The ICC values for interobserver agreement for impingement angle, CE angle, and CCD angle were 0.98 (95% CI, 0.97–0.98), 0.98 (95% CI, 0.97–0.98), and 0.99 (95% CI, 0.99–0.99), respectively.
Clinical Data
All covariates were assessed with validated questionnaires and objective measurements during Visit 2 with the exception of education, which was obtained at the baseline visit [39]. Covariates included patient age, height (measured with a Harpenden stadiometer [Seritex, Tinton Falls, NJ, USA]), weight (measured with a calibrated balance beam or electronic scale), self-rated health status (excellent/good versus fair/poor), and self-reported presence of hip pain (yes/no) ascertained with the questions “in the past 30 days, have you experienced pain in your right hip?” and “in the past 30 days, have you experienced pain in your left hip?” Body mass index (BMI) was calculated (kg/m2). Participants were asked about coexisting morbidities, including stroke, myocardial infarction, cancer, chronic obstructive pulmonary disease, hypertension, congestive heart failure, diabetes, and Parkinson’s disease. Men were classified as having one or more comorbidities or none. Participants were asked to bring in all current medications used within the last 30 days, and a computerized medication-coding dictionary [40] was used to categorize the medications. All prescription medications recorded by the clinics were stored in an electronic medications inventory database (San Francisco Coordinating Center, San Francisco, CA, USA). Each medication was matched to its ingredient(s) based on the Iowa Drug Information Service Drug Vocabulary (College of Pharmacy, University of Iowa, Iowa City, IA, USA).
Statistical Analysis
Subject characteristics for the whole population of men with valid radiographs at Visit 2 were reported as means and SDs for continuous variables and numbers and percentages for categorical variables.
The outcome variable in the analysis was arthrosis and was defined in two ways. The primary definition of arthrosis was a Croft Grade of II or higher. A secondary definition of arthrosis associated with hip symptoms was arthritis: Croft Grade ≥ II and hip pain in the same hip. Arthrosis was defined as Croft Grade ≥ II and no hip pain in the same hip. Hip pain was defined as hip pain only and Croft Grade 0 or I.
The exposure outcomes were each individual radiographic FAI measurement (impingement, CE and CCD angles) and FAI type defined as a three-category variable (cam, pincer, and mixed). The distribution of the individual FAI measurements was explored visually using histograms and normality plots.
Individual radiographic FAI measurements were categorized based on known clinical cut points [15]: (1) impingement < 70°, CCD > 125°, and CE > 39°; (2) CCD < 125°, impingement ≥ 70°, and CE ≤ 40°; and (3) CE > 40°, impingement ≥ 70°, and CCD ≥ 125°. The reference group for the analyses was hips without any radiographic feature of impingement.
We analyzed the association of radiographic signs of radiographic features of FAI with arthrosis in men using a hip-based analysis. Generalized estimating equations were used to test the association between FAI type and arthrosis by accounting for the correlation between the two hips using an unstructured correlation matrix. When analyzing the clinical hip OA definition, we compared the three groups with clinical or radiographic abnormalities (subjects with arthrosis and/or pain) with the reference group (no pain, no arthrosis) using three separate regression models to determine the association of arthrosis and hip pain, independently, and combined with radiographic signs of FAI. Covariates known to be associated with FAI and arthrosis were included in multivariate models. Models were adjusted for age, race, clinic site, BMI, self-rated health status, and at least one medical condition.
Results
Prevalence of Femoroacetabular Impingement Among Older Men
Among the 8051 hips available for analysis, 3053 (38%) hips had radiographic features of cam, pincer, or mixed FAI; in particular, 1748 of 3053 (57%), 886 of 3053 (29%), and 419 of 3053 (14%) had signs of pincer, cam, and mixed-type FAI, respectively (Table 2). The mean values for impingement, CE, and CCD were 78° (± 8°), 36° (± 7°), and 132° (± 4°), respectively. An impingement angle < 70° was found in 268 subjects (12%); a CE angle > 39° was found in 1516 subjects (43%), and a CCD angle < 125° was found in 88 subjects (4%).
Table 2.
OR and 95% CI for hip-based analysis for FAI type with Croft Grade ≥ II compared with Croft Grade < II
| FAI type | Hips (number) | OR* (95% CI) |
|---|---|---|
| No FAI | 5098 | 1 (reference) |
| Cam | 886 | 1.18 (0.89–1.57) |
| Pincer | 1748 | 1.55 (1.23–1.95) |
| Mixed | 419 | 1.96 (1.34–2.89) |
*Adjusted for age, race, clinic location, body mass index, comorbidity, and health status; OR = odds ratio; CI = confidence interval; FAI = femoroacetabular impingement.
Associations of Femoroacetabular Impingement With Arthrosis and Hip Pain
Both the prevalence and the severity of arthrosis, defined by a Croft grade greater than II, was higher in hips with a CE angle > 39° (odds ratio [OR], 1.53; 95% CI: 1.22–1.94; p < 0.001; Table 3) and in hips with a CCD angle < 125° (OR, 2.09; 95% CI, 1.24–3.51; p = 0.006) compared with hips without signs of FAI in multivariate-adjusted models. No association was found between hip OA and an impingement angle < 70°.
Table 3.
Association of major morphologic features that define FAI and radiographic hip OA (Croft Grade ≥ II)
| Angle cutoff | Hips (number) | OR* (95% CI) |
|---|---|---|
| No FAI | 5098 | 1 (reference) |
| Impingement angle < 70° only | 655 | 0.99 (0.69–1.4) |
| CE > 39° only | 1748 | 1.53 (1.22–1.94) |
| CCD < 125° only | 183 | 2.09 (1.24–3.51) |
*Adjusted for age, race clinic, body mass index, comorbidity, and health status; FAI = femoroacetabular impingement; OA = osteoarthritis; OR = odds ratio; CI = confidence interval; CE = center edge; CCD = caput-collum-diaphyseal.
A CE angle > 39° was associated with arthrosis (OR, 1.65; 95% CI, 1.26–2.15; p < 0.001), but not with arthritis (defined as Croft Grade ≥ II and hip pain in the same hip; p = 0.604; Table 4). A CCD angle < 125° had a borderline association with arthritis (OR, 2.52; 95% CI, 1.03–6.16; p = 0.042) and was not associated with arthrosis (p = 0.441). However, patients with an impingement angle < 70° were more likely to report no hip pain compared with patients without signs of FAI (OR, 0.76; 95% CI, 0.61–0.95; p = 0.015). Multiple adjustments for age, race, BMI, clinic site, self-rated health status, and at least one comorbidity did not change the results.
Table 4.
OR and 95% CI for the association of FAI type and radiographic and clinical hip OA*
| FAI type | Symptomatic OA | Asymptomatic OA | Hip pain only | |||
|---|---|---|---|---|---|---|
| Cases (number) | OR (95% CI) | Cases (number) | OR (95% CI) | Cases (number) | OR (95% CI) | |
| No cam and pincer† (n = 5093) | 93 | 1 (reference) | 192 | 1 (reference) | 922 | 1 (reference) |
| Cam (n = 886) | 16 | 0.97 (0.56–1.65) | 40 | 1.14 (0.82–1.6) | 128 | 0.82 (0.68–0.99) |
| Pincer (n = 1745) | 33 | 1.12 (0.73–1.72) | 97 | 1.63 (1.25–2.13) | 288 | 0.88 (0.76–1.01) |
| Mixed (n = 418) | 4 | 0.66 (0.25–1.73) | 31 | 2.49 (1.65–3.76) | 54 | 0.76 (0.58–1) |
| Individual FAI measures | ||||||
| No FAI* (n = 5093) | 93 | 1 (reference) | 192 | 1 (reference) | 922 | 1 (reference) |
| Impingement < 70° (n = 655) | 9 | 0.76 (0.4–1.44) | 26 | 0.96 (0.63–1.45) | 90 | 0.76 (0.61–0.95) |
| CE > 39° (n = 1745) | 33 | 1.11 (0.72–1.72) | 97 | 1.65 (1.26–2.15) | 288 | 0.89 (0.77–1.03) |
| CCD < 125° (n = 183) | 7 | 2.52 (1.03–6.16) | 10 | 1.85 (0.98–3.48) | 31 | 0.99 (0.67–1.45) |
*Models adjusted for age, race, clinic location, body mass index, comorbidity, and health status; †five hips had no information about hip pain and were excluded from the analysis; OR = odds ratio; CI = confidence interval; OA = osteoarthritis; FAI = femoroacetabular impingement; CE = center edge; CCD = caput-collum-diaphyseal.
The presence of arthrosis described by Croft grade was associated with radiographic features of pincer (OR, 1.55; 95% CI, 1.23–1.95; p < 0.001) and mixed FAI types (OR, 1.96; 95% CI, 1.34–2.89; p < 0.001) but not with cam FAI type after controlling for confounding variables (Table 2).
When hip pain and arthrosis were studied independently of each other and then combined (Table 4), we found that radiographic features of pincer and mixed FAI types were both associated with arthrosis (OR, 1.63; 95% CI, 1.25–2.13; p < 0.001 and OR, 2.49; 95% CI, 1.65–3.76; p < 0.001, respectively); however, these types were not associated with hip pain only or with arthritis compared with men without radiological features of FAI in adjusted models. Moreover, hips characterized by cam FAI type had lower odds of hip pain (age-adjusted OR, 0.82; 95% CI, 0.68–0.99; p = 0.037).
Discussion
FAI is a critical topic because it is common, incompletely understood, but certainly associated with pain and perhaps with arthritis progression in some patients. However, it is yet not clear whether FAI represents a normal variant in older patients or whether it is a condition associated with severe and aggressive arthritis even in older patients. Because some studies describe surgical interventions for FAI not only for young athletes, but also for older people [13, 41, 54], it is important to study patients of all ages who have radiographic signs of FAI and also to evaluate the association of FAI with pain and arthrosis in an older community-based cohort. We found that radiographic signs of FAI are common in older men and that the different types of FAI were not associated with increased pain and in fact that patients with cam-type FAI had a slightly lower risk of pain. These findings support the idea that FAI in older men is a common anatomical variant, likely to be associated with age as proposed in previously reports [9, 10].
Our study also has a number of limitations, including the fact that only a single radiographic view (the AP) was used; we did not have a frog-lateral view that would have allowed us to determine other measurements used for FAI radiographic assessment such as the alpha angle. Also, MR multiplanar reconstruction images would have allowed for a precise analysis of the femoral head using three-dimensional analysis. However, the radiological measurements that we used based on AP view have been demonstrated to be reliable in the assessment of FAI. A number of published FAI studies, based on large populations, presents a similar limitation. Another limitation of our study was the lack of any patient historical information about physical activity during teenage and young adult years. It is possible that men with pincer impingement had hip pain with weightbearing exercise as young adults and stopped or reduced this type of exercise before hip damage and were without hip pain at age 70 years or older. Also, the age of our cohort might be a limitation itself, given the higher prevalence of hip OA in elderly people. Our cross-sectional study is not able to determine the temporal relation between FAI radiographic findings and arthrosis or arthritis. Based on our results, we recommend that a longitudinal study be performed, which can address the issue of the cause-effect relationship of activity and FAI. Another shortcoming of our study is selection bias, because patients who had undergone THA were eliminated from the study; it is possible that many patients with symptomatic FAI were previously treated with surgery and our population might have a lower prevalence of pain than a community-based cohort, which includes patients with FAI before surgery. This may explain the cam-type association with less pain than the reference cohort.
The percentage of hips with radiographic features of pincer, cam, and mixed impingement deformity among our entire cohort was 21% (1748 of 8151), 11% (886 of 8151), and 5% (419 of 8151), respectively. These data are comparable to results previously reported by Jung et al [29], Gosvig et al in the Copenhagen OA study [21], and others [31, 35, 44]. Even if Jung et al [29] and Gosvig et al [21] used different criteria to diagnose cam deformity (alpha angle) while we used CCD and impingement angles, the prevalence of cam-type deformity is similar to our study. Leunig et al [36] obtained slightly different results from ours (6%–10%) for pincer impingement; however, they evaluated a younger population and at this time there are no other studies in the literature reporting prevalence of pincer-type FAI in an elderly community-based population.
Analyzing the relationship among radiologic features of FAI, arthrosis, and pain, we found that subjects with radiographic signs of cam-type impingement were less likely to have hip pain compared with patients without signs of FAI. Similar results have been reported in other studies [2, 32]. We determined that a low CCD angle (< 125°) was associated with an increased risk of arthrosis. Interestingly, this result is consistent with biomechanical analysis that reported CCD angle to be associated with cartilage defects [19]. An impingement angle < 70° has been associated with femoral head asphericity and an increased risk of arthrosis [15]. Analyzing radiologic features for pincer impingement, we found that overcoverage of the femoral head also was associated with an increased risk of arthrosis. This result is in agreement with other reports [36, 41, 42]. Although an association between pincer deformity and hip pain has been reported among active young women, and the damage pattern of pincer has been well documented in middle-aged women, we did not find an association between increased CE angle and hip pain in elderly men [52].
In summary, radiographic signs of FAI are common in elderly men. Features of pincer and mixed impingements are associated with arthrosis but not with pain. In addition, hips with radiographic signs of cam FAI are less likely to be painful. This suggests that caution is called for when considering FAI surgery in this population, because the radiographic finding might or might not account for the pain and may indeed represent a normal anatomic variant. We believe the epidemiology of this developmental hip disorder warrants further investigation, and in particular, studies should focus on further clarifying the relationship among patients’ ages, radiographic presentations, and pain patterns, because these may well have important implications that can help some patients avoid needlessly aggressive surgical treatments.
Acknowledgments
The Osteoporotic Fractures in Men (MrOS) Study is supported by National Institutes of Health funding. The following institutes provide support: the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), the National Institute on Aging (NIA), the National Center for Research Resources (NCRR), and NIH Roadmap for Medical Research under the following grant numbers: U01 AR45580, U01 AR45614, U01 AR45632, U01 AR45647, U01 AR45654, U01 AR45583, U01 AG18197, U01-AG027810, and UL1 RR024140.The National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) provided funding for the MrOS Hip OA ancillary study “Epidemiology and Genetics of Hip OA in Elderly Men” under the grant number R01 AR052000. This study was also supported by NIH funding: K24 AR04884, P50 AR060752 and P50 AR063043.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at University of California San Francisco, San Francisco, CA, USA.
References
- 1.Agricola R, Heijboer MP, Ginai AZ, Roels P, Zadpoor AA, Verhaar JA, Weinans H, Waarsing JH. A cam deformity is gradually acquired during skeletal maturation in adolescent and young male soccer players: a prospective study with minimum 2-year follow-up. Am J Sports Med. 2014;42:798–806. doi: 10.1177/0363546514524364. [DOI] [PubMed] [Google Scholar]
- 2.Allen D, Beaule PE, Ramadan O, Doucette S. Prevalence of associated deformities and hip pain in patients with cam-type femoroacetabular impingement. J Bone Joint Surg Br. 2009;91:589–594. doi: 10.1302/0301-620X.91B5.22028. [DOI] [PubMed] [Google Scholar]
- 3.Anderson SE, Siebenrock KA, Tannast M. Femoroacetabular impingement: evidence of an established hip abnormality. Radiology. 2010;257:8–13. doi: 10.1148/radiol.10091480. [DOI] [PubMed] [Google Scholar]
- 4.Barton C, Salineros MJ, Rakhra KS, Beaule PE. Validity of the alpha angle measurement on plain radiographs in the evaluation of cam-type femoroacetabular impingement. Clin Orthop Relat Res. 2011;469:464–469. doi: 10.1007/s11999-010-1624-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bathala EA, Bancroft LW, Peterson JJ, Ortiguera CJ. Radiologic case study. Femoroacetabular impingement. Orthopedics. 2007;30(986):1061–1064. doi: 10.3928/01477447-20071201-04. [DOI] [PubMed] [Google Scholar]
- 6.Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012–1018. doi: 10.1302/0301-620X.87B7.15203. [DOI] [PubMed] [Google Scholar]
- 7.Ben Tov T, Amar E, Shapira A, Steinberg E, Atoun E, Rath E. Clinical and functional outcome after acetabular labral repair in patients aged older than 50 years. Arthroscopy. 2014;30:305–310. [DOI] [PubMed]
- 8.Blank JB, Cawthon PM, Carrion-Petersen ML, Harper L, Johnson JP, Mitson E, Delay RR. Overview of recruitment for the osteoporotic fractures in men study (MrOS) Contemp Clin Trials. 2005;26:557–568. doi: 10.1016/j.cct.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 9.Brian P, Bernard S, Flemming D. Femoroacetabular impingement: screening and definitive imaging. Semin Roentgenol. 2010;45:228–237. doi: 10.1053/j.ro.2009.12.006. [DOI] [PubMed] [Google Scholar]
- 10.Brunner A, Hamers AT, Fitze M, Herzog RF. The plain beta-angle measured on radiographs in the assessment of femoroacetabular impingement. J Bone Joint Surg Br. 2010;92:1203–1208. doi: 10.1302/0301-620X.92B9.24410. [DOI] [PubMed] [Google Scholar]
- 11.Chaganti RK, Parimi N, Cawthon P, Dam TL, Nevitt MC, Lane NE. Association of 25-hydroxyvitamin D with prevalent osteoarthritis of the hip in elderly men: the osteoporotic fractures in men study. Arthritis Rheum. 2010;62:511–514. doi: 10.1002/art.27241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chaganti RK, Parimi N, Lang T, Orwoll E, Stefanick ML, Nevitt M, Lane NE. Bone mineral density and prevalent osteoarthritis of the hip in older men for the Osteoporotic Fractures in Men (MrOS) Study Group. Osteoporos Int. 2010;21:1307–1316. doi: 10.1007/s00198-009-1105-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chladek P, Musalek M, Trc T, Zahradnik P, Kos P. Femoroacetabular impingement syndrome-efficacy of surgical treatment with regards to age and basic diagnosis. Int Orthop. 2014 Nov 8 [Epub ahead of print]. [DOI] [PubMed]
- 14.Domayer SE, Ziebarth K, Chan J, Bixby S, Mamisch TC, Kim YJ. Femoroacetabular cam-type impingement: diagnostic sensitivity and specificity of radiographic views compared to radial MRI. Eur J Radiol. 2011;80:805–810. doi: 10.1016/j.ejrad.2010.10.016. [DOI] [PubMed] [Google Scholar]
- 15.Dudda M, Kim YJ, Zhang Y, Nevitt MC, Xu L, Niu J, Goggins J, Doherty M, Felson DT. Morphologic differences between the hips of Chinese women and white women: could they account for the ethnic difference in the prevalence of hip osteoarthritis? Arthritis Rheum. 2011;63:2992–2999. doi: 10.1002/art.30472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fukushima K, Uchiyama K, Takahira N, Moriya M, Yamamoto T, Itoman M, Takaso M. Prevalence of radiographic findings of femoroacetabular impingement in the Japanese population. J Orthop Surg Res. 2014;9:25. doi: 10.1186/1749-799X-9-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ganz R, Leunig M, Leunig-Ganz K, Harris WH. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res. 2008;466:264–272. doi: 10.1007/s11999-007-0060-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 19.Gierse H, Hackenbroch MH. Relations between degenerative changes in the femoral head and the radiologically determined biomechanical magnitude of effects [in German] Z Orthop Ihre Grenzgeb. 1986;124:732–739. doi: 10.1055/s-2008-1045030. [DOI] [PubMed] [Google Scholar]
- 20.Giori NJ, Trousdale RT. Acetabular retroversion is associated with osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:263–269. doi: 10.1097/01.blo.0000093014.90435.64. [DOI] [PubMed] [Google Scholar]
- 21.Gosvig KK, Jacobsen S, Sonne-Holm S, Palm H, Troelsen A. Prevalence of malformations of the hip joint and their relationship to sex, groin pain, and risk of osteoarthritis: a population-based survey. J Bone Joint Surg Am. 2010;92:1162–1169. doi: 10.2106/JBJS.H.01674. [DOI] [PubMed] [Google Scholar]
- 22.Hack K, Di Primio G, Rakhra K, Beaule PE. Prevalence of cam-type femoroacetabular impingement morphology in asymptomatic volunteers. J Bone Joint Surg Am. 2010;92:2436–2444. doi: 10.2106/JBJS.J.01280. [DOI] [PubMed] [Google Scholar]
- 23.Jaberi FM, Parvizi J. Hip pain in young adults: femoroacetabular impingement. J Arthroplasty. 2007;22:37–42. doi: 10.1016/j.arth.2007.05.039. [DOI] [PubMed] [Google Scholar]
- 24.Jager M, Wild A, Westhoff B, Krauspe R. Femoroacetabular impingement caused by a femoral osseous head-neck bump deformity: clinical, radiological, and experimental results. J Orthop Sci. 2004;9:256–263. doi: 10.1007/s00776-004-0770-y. [DOI] [PubMed] [Google Scholar]
- 25.Jamali AA, Mladenov K, Meyer DC, Martinez A, Beck M, Ganz R, Leunig M. Anteroposterior pelvic radiographs to assess acetabular retroversion: high validity of the ‘cross-over-sign’. J Orthop Res. 2007;25:758–765. doi: 10.1002/jor.20380. [DOI] [PubMed] [Google Scholar]
- 26.Javed A, O’Donnell JM. Arthroscopic femoral osteochondroplasty for cam femoroacetabular impingement in patients over 60 years of age. J Bone Joint Surg Br. 2011;93:326–331. doi: 10.1302/0301-620X.93B3.25262. [DOI] [PubMed] [Google Scholar]
- 27.Jerosch J, Grasselli C, Kothny PC, Litzkow D, Hennecke T. Reproduction of the anatomy (offset, CCD, leg length) with a modern short stem hip design–a radiological study [in German] Z Orthop Unfall. 2012;150:20–26. doi: 10.1055/s-0030-1270965. [DOI] [PubMed] [Google Scholar]
- 28.Johnson AC, Shaman MA, Ryan TG. Femoroacetabular impingement in former high-level youth soccer players. Am J Sports Med. 2012;40:1342–1346. doi: 10.1177/0363546512439287. [DOI] [PubMed] [Google Scholar]
- 29.Jung KA, Restrepo C, Hellman M, AbdelSalam H, Morrison W, Parvizi J. The prevalence of cam-type femoroacetabular deformity in asymptomatic adults. J Bone Joint Surg Br. 2011;93:1303–1307. doi: 10.1302/0301-620X.93B10.26433. [DOI] [PubMed] [Google Scholar]
- 30.Kassarjian A, Brisson M, Palmer WE. Femoroacetabular impingement. Eur J Radiol. 2007;63:29–35. doi: 10.1016/j.ejrad.2007.03.020. [DOI] [PubMed] [Google Scholar]
- 31.Laborie LB, Lehmann TG, Engesaeter IO, Eastwood DM, Engesaeter LB, Rosendahl K. Prevalence of radiographic findings thought to be associated with femoroacetabular impingement in a population-based cohort of 2081 healthy young adults. Radiology. 2011;260:494–502. doi: 10.1148/radiol.11102354. [DOI] [PubMed] [Google Scholar]
- 32.Lamontagne M, Kennedy MJ, Beaule PE. The effect of cam FAI on hip and pelvic motion during maximum squat. Clin Orthop Relat Res. 2009;467:645–650. doi: 10.1007/s11999-008-0620-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lane NE, Lin P, Christiansen L, Gore LR, Williams EN, Hochberg MC, Nevitt MC. Association of mild acetabular dysplasia with an increased risk of incident hip osteoarthritis in elderly white women: the study of osteoporotic fractures. Arthritis Rheum. 2000;43:400–404. doi: 10.1002/1529-0131(200002)43:2<400::AID-ANR21>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 34.Lane NE, Nevitt MC, Cooper C, Pressman A, Gore R, Hochberg M. Acetabular dysplasia and osteoarthritis of the hip in elderly white women. Ann Rheum Dis. 1997;56:627–630. doi: 10.1136/ard.56.10.627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Leunig M, Ganz R. Femoroacetabular impingement. A common cause of hip complaints leading to arthrosis] [in German. Unfallchirurg. 2005;108(9–10):12–17. doi: 10.1007/s00113-004-0902-z. [DOI] [PubMed] [Google Scholar]
- 36.Leunig M, Juni P, Werlen S, Limacher A, Nuesch E, Pfirrmann CW, Trelle S, Odermatt A, Hofstetter W, Ganz R, Reichenbach S. Prevalence of cam and pincer-type deformities on hip MRI in an asymptomatic young Swiss female population: a cross-sectional study. Osteoarthritis Cartilage. 2013;21:544–550. doi: 10.1016/j.joca.2013.01.003. [DOI] [PubMed] [Google Scholar]
- 37.Mathew G, Kowalczuk M, Hetaimish B, Bedi A, Philippon MJ, Bhandari M, Simunovic N, Crouch S, Ayeni OR, Investigators F. Radiographic prevalence of CAM-type femoroacetabular impingement after open reduction and internal fixation of femoral neck fractures. Knee Surg Sports Traumatol Arthrosc. 2014;22:793–800. doi: 10.1007/s00167-014-2835-6. [DOI] [PubMed] [Google Scholar]
- 38.Mori R, Yasunaga Y, Yamasaki T, Nakashiro J, Fujii J, Terayama H, Ohshima S, Ochi M. Are cam and pincer deformities as common as dysplasia in Japanese patients with hip pain? Bone Joint J. 2014;96:172–176. doi: 10.1302/0301-620X.96B2.32680. [DOI] [PubMed] [Google Scholar]
- 39.Orwoll E, Blank JB, Barrett-Connor E, Cauley J, Cummings S, Ensrud K, Lewis C, Cawthon PM, Marcus R, Marshall LM, McGowan J, Phipps K, Sherman S, Stefanick ML, Stone K. Design and baseline characteristics of the osteoporotic fractures in men (MrOS) study–a large observational study of the determinants of fracture in older men. Contemp Clin Trials. 2005;26:569–585. doi: 10.1016/j.cct.2005.05.006. [DOI] [PubMed] [Google Scholar]
- 40.Pahor M, Chrischilles EA, Guralnik JM, Brown SL, Wallace RB, Carbonin P. Drug data coding and analysis in epidemiologic studies. Eur J Epidemiol. 1994;10:405–411. doi: 10.1007/BF01719664. [DOI] [PubMed] [Google Scholar]
- 41.Palmer AJ, Ayyar-Gupta V, Dutton SJ, Rombach I, Cooper CD, Pollard TC, Hollinghurst D, Taylor A, Barker KL, McNally EG, Beard DJ, Andrade AJ, Carr AJ, Glyn-Jones S. Protocol for the Femoroacetabular Impingement Trial (FAIT): a multi-centre randomised controlled trial comparing surgical and non-surgical management of femoroacetabular impingement. Bone Joint Res. 2014;3:321–327. doi: 10.1302/2046-3758.311.2000336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Parvizi J, Leunig M, Ganz R. Femoroacetabular impingement. J Am Acad Orthop Surg. 2007;15:561–570. doi: 10.5435/00124635-200709000-00006. [DOI] [PubMed] [Google Scholar]
- 43.Pulido L, Parvizi J. Femoroacetabular impingement. Semin Musculoskelet Radiol. 2007;11:66–72. doi: 10.1055/s-2007-984413. [DOI] [PubMed] [Google Scholar]
- 44.Reichenbach S, Leunig M, Werlen S, Nuesch E, Pfirrmann CW, Bonel H, Odermatt A, Hofstetter W, Ganz R, Juni P. Association between cam-type deformities and magnetic resonance imaging-detected structural hip damage: a cross-sectional study in young men. Arthritis Rheum. 2011;63:4023–4030. doi: 10.1002/art.30589. [DOI] [PubMed] [Google Scholar]
- 45.Samora JB, Ng VY, Ellis TJ. Femoroacetabular impingement: a common cause of hip pain in young adults. Clin J Sport Med. 2011;21:51–56. doi: 10.1097/JSM.0b013e318205dfde. [DOI] [PubMed] [Google Scholar]
- 46.Scheyerer MJ, Copeland CE, Stromberg J, Ruckstuhl T, Werner CM. Radiographic markers of femoroacetabular impingement: correlation of herniation pit and femoral bump with a positive cross-over ratio. Adv Orthop. 2014;2014:432728. doi: 10.1155/2014/432728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420–428. doi: 10.1037/0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 48.Siebenrock KA, Schoeniger R, Ganz R. Anterior femoro-acetabular impingement due to acetabular retroversion. Treatment with periacetabular osteotomy. J Bone Joint Surg Am. 2003;85:278–286. doi: 10.2106/00004623-200302000-00015. [DOI] [PubMed] [Google Scholar]
- 49.Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis–what the radiologist should know. AJR Am J Roentgenol. 2007;188:1540–1552. doi: 10.2214/AJR.06.0921. [DOI] [PubMed] [Google Scholar]
- 50.Tanzer M, Noiseux N. Osseous abnormalities and early osteoarthritis: the role of hip impingement. Clin Orthop Relat Res. 2004;429:170–177. doi: 10.1097/01.blo.0000150119.49983.ef. [DOI] [PubMed] [Google Scholar]
- 51.Tonnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999;81:1747–1770. doi: 10.2106/00004623-199912000-00014. [DOI] [PubMed] [Google Scholar]
- 52.Visser M, Deurenberg P, van Staveren WA, Hautvast JG. Resting metabolic rate and diet-induced thermogenesis in young and elderly subjects: relationship with body composition, fat distribution, and physical activity level. Am J Clin Nutr. 1995;61:772–778. doi: 10.1093/ajcn/61.4.772. [DOI] [PubMed] [Google Scholar]
- 53.Wagner S, Hofstetter W, Chiquet M, Mainil-Varlet P, Stauffer E, Ganz R, Siebenrock KA. Early osteoarthritic changes of human femoral head cartilage subsequent to femoro-acetabular impingement. Osteoarthritis Cartilage. 2003;11:508–518. doi: 10.1016/S1063-4584(03)00075-X. [DOI] [PubMed] [Google Scholar]
- 54.Werner CM, Ramseier LE, Ruckstuhl T, Stromberg J, Copeland CE, Turen CH, Rufibach K, Bouaicha S. Normal values of Wiberg’s lateral center-edge angle and Lequesne’s acetabular index–a coxometric update. Skeletal Radiol. 2012;41:1273–1278. doi: 10.1007/s00256-012-1420-7. [DOI] [PubMed] [Google Scholar]


