Abstract
Background
A scapular-protecting brace is one option for treating patients with a winging scapula in isolated serratus palsy. However, outcomes after brace treatment have been reported in only a few studies, and to our knowledge, none has results reported at long-term beyond 10 years.
Questions/purpose
We asked: (1) What was the average length of time patients wore the brace? (2) Did scapular winging and ROM improve with brace treatment? (3) Was pain decreased? (4) Did the duration of symptoms before brace treatment influence the outcome?
Patients and Methods
Between 1980 and 1999, we treated 110 patients with a scapular-protecting brace. General indications for this treatment included electroneuromyography-verified isolated serratus palsy, 3 cm or greater scapular winging, and limited ROM. For patients with scapular winging less than 3 cm we used observation and avoidance of all heavy work or lifting. Of the patients treated with a brace, 55 (50%) were available at a minimum followup of 10 years (mean, 22 years; range, 10–28 years). Mean patient age was 30 years at the onset of symptoms (range, 15–52 years). Brace use was based on patient self-report, and we determined the degree of scapular winging and ROM clinically and level of pain by chart review before and after treatment.
Results
The brace was applied a mean 6 months (median, 5 months) after onset of symptoms. Mean duration of brace use was 10 months for 12 hours per day. Winging of the scapula, measured in 90° flexion without resistance, disappeared in 35 patients (64%) with brace use. Flexion averaged 153° and abduction 168°. Ten patients (18%) were pain-free during exertion and 18 (33%) at rest. Pain at rest was present in 37 patients (67%); of those, it was present only seldom in 15 (27%), sometimes present in 21 (38%), and one patient (2%) experienced continuous pain at rest despite brace treatment. With the number of patients available, there were no differences between patients who started brace treatment early (within 6 months of onset of symptoms) and those who started later (more than 6 months after symptom onset) in terms of improvement of scapular winging in flexion at 90° with resistance (mean, 1.2 ± 2.0 cm vs 1.7 ± 2.3 cm; p = 0.415; 95% CI, −1.6 to 0.7), better flexion (mean, 156° ± 17° flexion vs 149° ± 28° flexion; p < 0.253; 95% CI, −5 to 19), or improvement in other parameters that we measured.
Conclusions
Compliance was high for scapular-protecting brace treatment in patients with serratus palsy but recovery was incomplete for many patients, most of whom still had some pain and a large proportion still had some degree of scapular winging. We continue to use scapular bracing for treating patients who have 3 cm or more scapular winging and limited ROM, and whose work or hobbies demand motions causing winging, although we counsel our patients that recovery is likely to be incomplete.
Level of Evidence
Level IV, therapeutic study.
Introduction
The most disabling dysfunction in patients with isolated serratus palsy is the lack of adequate fixation of the scapula against the rib cage during active flexion and abduction [3, 17, 18]. Scapular-protecting bracing may prevent this posterior displacement. Scapula bracing models have ranged from extremely cumbersome plaster shoulder spica models [1] to more comfortable but less-effective models [5, 6, 9, 19] and more recently to a more convenient and effective model used by the senior author (MV) to treat patients with isolated serratus palsy [14, 15]. According to the literature, improvement or recovery after brace treatment has been reported in 50% to 100% of patients [1, 4–6, 8, 9].
Although brace treatment for patients with serratus palsy has been in use for a century and therapeutic outcomes of its use have been reported [1, 4, 6, 8, 9, 13, 19], the designs of these studies and the braces have varied, therefore the results of these studies are not necessarily comparable. To our knowledge, no studies have evaluated the long-term (10-year minimum) results of patients treated with bracing.
We therefore asked: (1) What was the average time of brace use in patients who had brace treatment? (2) Did scapular winging and ROM improve with brace treatment? (3) Was patient pain decreased? (4) Did the duration of symptoms before brace treatment influence the outcome?
Patients and Methods
We retrospectively identified 188 patients with a diagnosis of isolated serratus palsy seen by the senior author (MV) between 1980 and 1999 (Table 1). The symptoms were sufficiently bothersome (scapular winging of 3 cm or more and limited ROM) that we recommended the use of a cumbersome brace (Serratuspareesiortoosi K35; Respecta, Helsinki, Finland) in 110 patients. During the early 1980s we used a heavy, cumbersome brace which provided excellent support but patient compliance was poorer. Our modern brace models, available for women (Fig. 1) and men (Fig. 2), are well tolerated and still provide adequate scapular support with better patient compliance. Of the 188 identified patients, 70 with scapular winging less than 3 cm received no specific treatment [11], and eight whose symptomatic palsy had lasted for many years were treated surgically.
Table 1.
Inclusion and exclusion criteria
| Criteria |
|---|
| Inclusion |
| Scapular winging caused by serratus palsy |
| Isolated long thoracic nerve palsy verified by electroneuromyography |
| Adequate recordings of history and clinical findings at the beginning of symptoms |
| Scapular-protecting brace used as treatment |
| Exclusion |
| More than the long thoracic nerve affected (such as Parsonage-Turner syndrome) on electroneuromyography |
| Neurologic disorders like facioscapulohumeral syndrome |
| Functional palsies caused by shoulder problems causing scapular winging |
| Insufficient patient status recordings |
Fig. 1A–B.
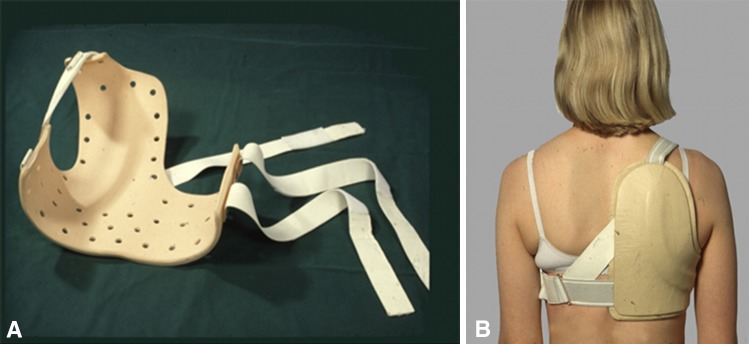
(A) The scapular protecting brace for treatment of women with serratus palsy is shown. (B) A back view is shown.
Fig. 2A–B.
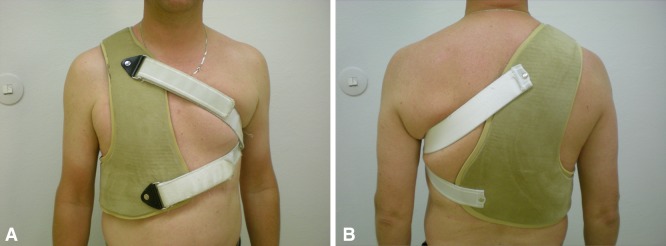
(A) Front and (B) back views of a heavier scapular-protecting brace model for treatment of men with serratus palsy are shown.
Permission to perform this study was received from the ethics committee of the hospital district where the study was conducted.
Of the 110 identified patients with isolated serratus palsies treated with a brace (a custom-made brace made individually for each patient in our brace shop), one had died and 11 had no address available and thus were unreachable. The remaining 98 patients were invited to participate in our study and 67 (68%) attended final followup, which consisted of clinical evaluations and questionnaires. Four of the 67 patients were excluded owing to lack of initial ROM recordings. Four other patients were excluded because brace therapy had been initiated 2 to 5 years after symptom onset which is too long a delay because of longstanding muscle palsy. Another four patients were excluded because they had worn the brace less than 3 months (three patients) or less than 4 hours a day (two patients). The final study group consisted of 55 patients (50% of the total number who were treated with a brace). Of these, 42 were males (76%) and their mean age at onset of symptoms was 30 years (range, 15–52 years). Brace therapy was started a mean 6 months after onset of initial symptoms.
Data for this study were drawn from a chart review performed by the authors (VP, MV). During the period in question, standardized outcome metrics were not in use. Data abstracted included brace use (based on patient self-report), and we determined diagnoses, clinical background, degree of scapular winging, ROM, and level of pain before and after treatment by chart review.
Mean patient followup was 22 years (range, 10–28 years). Of the 55 patients, 48 (87%) were right-handed and the palsy was on the right side in 49 (89%). The dominant side was affected in 80% of patients (Table 2). The etiologies were acute trauma in 18 patients (33%), exertion (heavy pulling or lifting, strenuous tennis) in 28 patients (51%), infection in one patient (3%), and miscellaneous or unknown cause in eight patients (13%) [7, 16]. The palsy was detectable in 29 patients (53%) 1 week after onset of symptoms and in 70% of patients 3 weeks after onset of symptoms.
Table 2.
Characteristics of patients with isolated serratus palsy on baseline*
| Variable | All patients | Females | Males | p value** |
|---|---|---|---|---|
| Sex (number, %) | 55 (100) | 13 (24) | 42 (76) | 0.001 |
| Age at baseline (years, mean, SD) | 30 (10) | 28 (8) | 31 (10) | 0.321 |
| Palsy on right side (number, %) | 49 (89) | 13 (100) | 36 (86) | 0.149 |
| Flexion (°, SD) | 137 (24) | 147 (21) | 133 (25) | 0.115 |
| Abduction (°, SD) | 150 (33) | 161 (29) | 147 (34) | 0.289 |
| Scapular winging noticed by (%) | 0.935 | |||
| Doctor | 26 | 23 | 27 | |
| Physiotherapist | 2 | 0 | 2 | |
| Patient | 57 | 62 | 56 | |
| Family member | 15 | 15 | 15 | |
| Duration of pain (%) | 0.497 | |||
| < 1 week | 31 | 29 | 31 | |
| 1–4 weeks | 44 | 29 | 49 | |
| > 1 month | 25 | 42 | 20 | |
| Intensity of pain (%) | 0.714 | |||
| Mild | 22 | 14 | 24 | |
| Hard | 37 | 43 | 36 | |
| Unbearable | 41 | 43 | 40 | |
| Heaviness of work | 0.122 | |||
| Light | 31 | 50 | 24 | |
| Moderate | 27 | 29 | 27 | |
| Heavy | 42 | 21 | 49 |
* At first examination by the senior author (MV); **age, flexion, and abduction p values between males and females are from independent samples t-test and other p values are from Pearson’s chi-square test.
Initial patient evaluation included a detailed history and physical examination and EMG. After the first consultation, patients went to our prosthesis shop where the brace subsequently was fabricated. We recommended patients wear the brace when doing housework or during their working hours. The first consultation was done within 6 months of onset of symptoms for 68% of patients and within 1 year for 91% of patients. At initial evaluation, flexion was greater than 140° in 40% of patients and abduction was greater than 160° in 46%. Scapular winging was noticed by 32 patients (57%). During the first year of the palsy, 31 patients (56%) underwent no physiotherapy and 38 (69%) had moderate or heavy work at an occupation requiring heavy labor. Pain at onset of the palsy was recorded as “almost unbearable” by 41% of patients, however four patients (7%) were pain-free. Pain continued in 44% of patients for 1 to 4 weeks and was considered severe or “almost unbearable” in 78% (Table 2). At onset of the disease, 15 patients used no medications for pain; however, 14 used analgesics daily during the first 4 weeks and nine (16%) used pain medication daily for more than a month.
At followup, each of the 55 patients underwent a physical examination by an independent observer (VP), who again recorded the medical history and checked for previous treatment records from other hospitals. Scapular winging and active shoulder ROM were measured similarly as during the first consultation. Scapular winging was recorded in centimeters as posterior displacement of the medial border of the scapula from the posterior thorax in three positions: arms at 90° flexion, at 90° resisted flexion, and in a passive crossed-arm position. In some individuals the scapulae are more prominent than in others and we compared the posterior displacement (winging) with the level of the healthy scapula. Shoulder flexion strength was measured with a Salter spring balance (Salter Housewares, Tonbridge, Kent, UK) [2]. Grip strength was measured using a Jamar dynamometer (Lafayette Instrument, Lafayette, IN, USA) for hand-dominance comparison. We also evaluated whether the palsy had resolved completely, partially, or not at all, as indicated by scapular winging, flexion strength, and ROM.
Questionnaires [11] were sent to the patients along with the invitation to participate in the study. The questionnaire included questions regarding demographics, work history, onset of symptoms and preceding factors, treatment, healing, and current condition. Patients completed the questionnaires at home and returned them at followup.
Differences in winging, ROM, and pain were determined using a t-test and differences in dichotomy variables were determined using Pearson’s chi-square test. A paired t-test was used to determine individual patient changes between baseline and followup measures of ROM and winging. A probability less than 0.05 was considered significant. We performed all statistical analyses with SPSS® Statistics Version 20.0 (IBM Corporation, Armonk, NY, USA).
Results
Mean duration of brace use was 10 months for 12 hours per day (Table 3). Forty-eight of the patients (87%) had used the brace according to recommendation; seven used it less often but for more than 4 hours a day and more than 3 months. Five patients reported that they had used the brace longer than recommended, even up to 2 years, because it helped them at work. Thus, brace compliance was 87%. Three patients needed a new brace because the first model was unsuitable.
Table 3.
Demographics of patients treated with a scapular brace
| Variable | All patients n = 55 | Less than 6 months* n = 31 | Six months or greater* n = 24 | p value | 95% CI |
|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | |||
| Followup (years) | 22.4 (4) | 22.6 (4) | 21.7 (4) | 0.398 | −1 to 3 |
| Time between onset of symptoms and brace application (months) | 5.7 (4) | 3.1 (1) | 9.1 (3) | < 0.001 | −7 to −5 |
| Duration of brace use (months) | 10.2 (6) | 10.1 (6) | 10.4 (5) | 0.836 | −3 to 3 |
| Brace use (hours/day) | 11.9 (4) | 11.9 (4) | 12.0 (4) | 0.898 | −2 to 2 |
| Followup flexion (°) | 153 (22) | 156 (17) | 149 (28) | 0.253 | −5 to 19 |
| Followup flexion of unaffected shoulder (°) | 159 (10) | 159 (10) | 159 (11) | 0.945 | −5 to 6 |
| Followup abduction (°) | 168 (27) | 169 (28) | 167 (27) | 0.708 | −13 to 17 |
| Followup abduction of unaffected shoulder (°) | 179 (12) | 180 (12) | 179 (12) | 0.659 | −5 to 8 |
| Strength in flexion of affected shoulder (N) | 81 (29) | 80 (31) | 81 (26) | 0.895 | −17 to 15 |
| Strength in flexion of unaffected shoulder (N) | 90 (26) | 89 (26) | 90 (26) | 0.990 | −14 to 14 |
| No pain related to serratus palsy at followup (number, %) | 17 (30) | 13 (43) | 3 (13) | 0.072 | |
| Paresis at followup (number, %) | 0.716 | ||||
| None | 35 (64) | 20 (64) | 15 (62) | ||
| Partial | 13 (23) | 8 (26) | 5 (21) | ||
| Complete | 7 (13) | 3 (10) | 4 (17) | ||
| Recovery complete (number, %) | |||||
| Subjective | 28 (51) | 18 (58) | 9 (38) | 0.130 | |
| Objective | 35 (64) | 20 (64) | 15 (62) | 0.716 | |
* Months from onset of symptoms to application of brace.
Winging measured in 90° flexion resolved in 38 patients (69%). In the other 17 patients (31%), winging averaged 3.4 cm, and in four of them (7%), winging remained more than 4 cm (Table 4). ROM improved almost to the level of the contralateral shoulder (Table 4). Flexion improved from 137° ± 24° to 156° ± 16° and abduction from 150° ± 33° to 170o ± 24° (p < 0.001; 95% CI, −26° to −12° and −29° to −10o, respectively).
Table 4.
ROM and scapular winging
| Variable | Baseline | Followup | p value | 95% CI | Contra-lateral shoulder | p value | 95% CI | Brace delay < 6 months n = 31 | Brace delay > 6 months n = 24 | p value | 95% CI |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |||||||
| Shoulder flexion (°) n = 34 | 137 (24) | 156 (16) | < 0.001 | −26 to −12 | 159 (10) | 0.027 | −12 to − 0.7 | 156 (17) | 149 (28) | 0.253 | −5 to 19 |
| Shoulder abduction (°) n = 32 | 150 (33) | 170 (24) | < 0.001 | −29 to −10 | 179 (12) | < 0.001 | −17 to −5 | 169 (28) | 167 (27) | 0.798 | −13 to 17 |
| Winging (cm) in 90° flexion, n = 22 | 3.9 (1.4) | 1.0 (1.7) | < 0.001 | 2–4 | 1.1 (1.8) | 1.3 (2.0) | 0.650 | −1 to 0.8 | |||
| Winging in resisted | 4.4 (1.3.) | 0.9 (1.6) | < 0.001 | 3–4 | 1.2 (2.0) | 1.7 (2.3) | 0.415 | −1.6 to 0.7 | |||
| 90° flexion, n = 23 | |||||||||||
| Winging in cross-arm position, n = 55 | 0.3 (1.0) | 0.4 (1.2) | 0.3 (0.9) | 0.817 | −0.5 to 0.6 |
At followup, flexion was greater than 140° for 41 patients (75%; mean, 153°), and abduction was greater than 160° for 39 patients (71%; mean, 168°). Flexion strength at followup was 81 N compared with the contralateral side which was 90 N, with no significant difference (p = 0.128; 95% CI, −19.2 to 2.5). The four patients who were excluded because brace therapy was initiated 2 to 5 years after onset of symptoms had scapular winging at 90° flexion of 5 cm, 3 cm, 4 cm, and 5 cm and all had pain. Four other patients who were excluded because they did not wear the brace long enough had no winging during nonresisted or resisted flexion at final followup; these patients had less-severe winging at baseline than the others. At followup, only 10 patients (18%) were totally free of pain during exertion, with 16 patients still experiencing pain seldom, 21 sometimes, and eight constantly. Ten patients (18%) were pain-free during exertion and 18 (33%) at rest. Pain at rest was present in 37 patients (67%); of those, it was present only seldom in 15 (27%), sometimes present in 21 (38%), and one patient (2%) experienced continuous pain at rest despite brace treatment.
Pain had increased during the previous year for 13 patients (24%), during which time 27 (49%) had used NSAIDS, three of them continuously, and nine (16%) received physiotherapy. At symptom onset, the heaviness of work (a light work occupation like an office worker or executive versus a heavy one like a construction worker) did not correlate with intensity or duration of pain. Pain was vague around the scapular area similar to that reported at the first consultation. We did not find any evidence for cervical radiculopathy or rotator cuff disease.
Patients who received a brace within 6 months of onset of symptoms were not more likely to achieve improvement in scapular winging than those who started wearing the brace later than 6 months (winging, 1.1 ± 1.8 cm vs 1.3 ± 2.0 cm; n = 55; p = 0.650; 95% CI, −1 to 0.8) (Table 4). Patients who received a brace within 6 months of onset of symptoms did not achieve greater mean ROM in flexion than those who started after 6 months (156° ± 17° vs 149° ± 28°; n = 55; p = 0.253; 95% CI, −5 to 19) (Table 3). Patients who received a brace within 6 months of onset of symptoms did not show a difference in average pain scores at latest followup (no pain, 43% [n = 31] vs 13% [n = 24]; p = 0.072) (Table 3). Sick leave taken at the beginning of the disease by 29 patients averaged 4 months (range, 0.5–27 months); 42 patients continued to work with 12 changing to a less physically demanding job, and two listed themselves as unemployed. Of 11 retired patients, five had retired because of serratus palsy.
Discussion
Scapular winging caused by serratus palsy is painful, disabling, and difficult to treat. Some patients can be treated with a brace and although there are studies on bracing, to our knowledge, there are no long-term studies. At a minimum of 10 years of followup, we found that while many patients had improvements in pain and scapular winging, the majority still had some pain and many still had some scapular winging. Because numerous patients were unaccounted for at the 22-year mean followup of our study, we consider our results a best-case estimate of the efficacy of this treatment, suggesting that this condition is rather resistant to nonsurgical treatment with a brace.
We acknowledge limitations in our study. As would be expected for a study that includes patients treated during a three-decade period, the study experienced considerable loss to followup. Forty-three of 110 of our patients (39%) were unaccounted for at the time of this report, while 67 participated in final followup, but 12 of them were excluded owing to inadequate primary patient records or failure to use the brace according to advice. Since the health status of patients lost to followup often is inferior to the status of those who are accounted for, we consider our results to be a best-case analysis of the possible results of this intervention. Next, when patients were seen initially or at followup, we obtained no validated functional scores like a Constant-Murley score, because they were not in common use 20 or more years ago. We consider that in evaluation of serratus palsy, in addition to scapular winging, pain, shoulder ROM, and strength in flexion are decisive. In addition, the amount of winging is not easy to measure in some patients because the shape of the area may differ considerably. We also used no objective measurement techniques such as that reported by Plafcan et al. [12]. Third, our brace design has varied during the decades. During the early years of this study, we used rather cumbersome heavy braces which provided excellent support but had poor patient compliance. In the 1980s, we used simple brace models designed by earlier authors but perhaps not giving adequate support. From the end of the 1980s, we have used our new design (Figs. 1, 2). Finally, we cannot state whether these patients improved more than if they did not use the brace since we have no comparison group. We also do not know whether this treatment is better or worse than the available surgical treatments.
Our study showed that the brace was well tolerated and was worn for the length of time prescribed by the majority of the patients. For stabilizing the winged scapula, devices used earlier were a plaster shoulder spica cast [1], an adjustable elbow rest [5], a metal brace with two metal cups supporting the affected and the unaffected scapulae [19], a simpler version of that orthosis [6], a leather brace with a sleeve preventing elevation of the arm [4], and a bilateral over- or under-the-shoulder brace [13]. Marin`s brace was a thick leather rectangular scapular pad attached to two loops to form a Figure 8 [9]. Klebe et al. [8] used a similar brace, which we used successfully during the early1980s after using a heavy, cumbersome brace in the 1970s. Our modern brace models, which we have used for 25 years (Figs. 1, 2) are well tolerated and still provide adequate scapular support with better patient compliance [15]. We found that many patients who received brace treatment experienced improvements in winging, ROM, and pain, but some symptoms remained in a majority of patients. Some articles of small series [1, 4, 6, 9, 13, 19] and one of a larger series [8] reported short-term outcomes of serratus palsy after brace treatment, but to our knowledge, none reported long-term outcomes (Table 5). We also did not find any articles reporting short- or long-term outcomes of patients with isolated serratus palsy after brace treatment. After using this treatment for 35 years, we believe that it is effective in appropriate patients [10, 14, 15].
Table 5.
Studies on outcomes of serratus palsy in patients treated with a scapular brace
| Study | Number of patients | Mean age (years; range) | Males (%) | Duration of brace use (months; (range) | Mean followup since brace applied (months; range) | Recovery complete (%) |
|---|---|---|---|---|---|---|
| Berkheiser and Shapiro [1] | 4 | 40 (22–63) | 0 | 3.5 (3–6) | 5 (3–8) | 100 |
| Hansson [4] | 5 | 29 (22–50) | 60 | 4.8 (3–9) | 11 (3–24) | 100 |
| Horwitz and Tocantins [5] | 6 | 39 (35–55) | 100 | 11 (1–24) | 60 | |
| Klebe et al. [8] | 64 | 38 (15–75) | 67 | 11 (3–29) | 12 | 50 |
| Marin [9] | 5 | 23 (20–29) | 100 | 3 (2–4) | 3.6 (2–4) | |
| Current study | 55 | 30 (15–52) | 76 | 10.2 (3–24) | 22 years (10–28) | Subjectively 51 Objectively* 64 |
* No winging.
Winging of the scapula at 90° flexion in 55 patients averaged 1.0 cm at followup after brace treatment, whereas it averaged 0.8 cm after the natural course [11]. Most of the patients who received brace treatment, however, had more severe winging. Concerning winging at 90° resisted flexion in 55 patients, the result was similar: 1.2 cm after brace treatment and 0.9 cm after a natural course. We found no mention of winging in centimeters except in the studies cited above. After 1 year, winging was absent after brace treatment in 50% of patients [8] and in 64% of our patients for whom we had complete followup after a mean of 22 years, although as mentioned, numerous patients were unaccounted for at latest followup. ROM in flexion and abduction improved after brace treatment almost to the level of the contralateral shoulder (flexion 153°, abduction 168°), but not as well as after the natural course of healing (flexion 161°, abduction 181°) [11]. Klebe et al. [8] stated that by the 1-year followup, ½ of their patients had regained normal shoulder function. Other studies mention no ROM values.
Pain generally has not been considered a problem, but it was problematic in many of our patients. Only 51% of our patients were pain free after brace treatment, which is similar to the 50% after the natural course of healing [11].
Klebe et al. [8] stated that after 1-year of brace treatment, 50% of patients had no complaints. In addition, our results indicated that pain in our patients seemed to increase with time. At symptom onset, four patients with serratus palsies were pain free; three of the patients, one with posttraumatic and two with postoperative palsies, in an area not related to the course of the long thoracic nerve, recovered but one patient had moderate pain with exertion after surgery and his ROM was limited at the 27-year followup.
Concerning the delay from onset of symptoms to brace application, with the numbers of patients in our study we could not detect a difference in patients who had received a brace during the 6 months after onset of symptoms with respect to winging in nonresisted flexion compared with patients treated after 6 months of onset of symptoms. There also was no detectable difference in flexion and abduction in patients treated before or after 6 months of onset of symptoms. A bracing delay less than 6 months did not affect pain level of patients compared with those who started brace treatment more than 6 months after symptoms began. This has not been discussed in the literature, therefore we conclude that bracing delay has no influence on the outcome of isolated serratus palsy, although that was our impression before this study.
We conclude that the outcome of serratus palsy after brace treatment is not as benign as has been reported in smaller series [1, 4, 5], and we agree with Klebe et al. [8] that recovery is often only partial and may not be achievable in patients with more-severe presentations. Our results may be a best-case scenario since we had no validated outcomes scores, no objective measurements of winging, and a high loss to followup. However, we still believe that the brace is useful for a patient with serratus palsy who has 3 cm or more scapular winging and limited ROM. If bracing is not successful after 1 to 1½ years, surgery might be worth considering in patients who are symptomatic.
Acknowledgments
We thank Carol Norris PhD, Language Services, University of Helsinki (Helsinki, Finland), for language revision.
Footnotes
The institution of one or more of the authors (MV, VP, HV, LR) has received, during the study period, funding from EVO, HUS (government grant from the Helsinki University Hospital District, Helsinki, Finland).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, and that all investigations were concluded in conformity with ethical principles of research, and that informed consent was obtained for participation in the study.
This work was performed at the Research Institute Orton, Invalid Foundation, Helsinki, Finland.
References
- 1.Berkheiser EJ, Shapiro F. Alar scapula: traumatic palsy of serratus magnus. JAMA. 1937;108:1790–1793. doi: 10.1001/jama.1937.02780210030009. [DOI] [Google Scholar]
- 2.Borgmästars N, Paavola M, Remes V, Lohman M, Vastamäki M. Pain relief, motion, and function after rotator cuff repair or reconstruction may not persist after 16 years. Clin Orthop Relat Res. 2010;468:2678–2689. doi: 10.1007/s11999-010-1403-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Friedenberg SM, Zimprich T, Harper CM. The natural history of long thoracic and spinal accessory neuropathies. Muscle Nerve. 2002;25:535–539. doi: 10.1002/mus.10068. [DOI] [PubMed] [Google Scholar]
- 4.Hansson KG. Serratus magnus paralysis. Arch Phys Med Rehabil. 1948;29:156–161. [PubMed] [Google Scholar]
- 5.Horwitz MT, Tocantins LM. Isolated paralysis of the serratus anterior (magnus) muscle. J Bone Joint Surg Am. 1938;20:721–725. [Google Scholar]
- 6.Johnson JT, Kendall HO. Isolated paralysis of the serratus anterior muscle. J Bone Joint Surg Am. 1955;37:567–574. [PubMed] [Google Scholar]
- 7.Kauppila LI, Vastamaki M. Iatrogenic serratus anterior paralysis: long-term outcome in 26 patients. Chest. 1996;109:31–34. doi: 10.1378/chest.109.1.31. [DOI] [PubMed] [Google Scholar]
- 8.Klebe TM, Dossing KV, Blenstrup T, Nielsen-Ferreira J, Rejsenhus I, Aalkjaer G, Breddam M. Scapulae alatae–angels’ wings: a study of 64 patients treated with braces and physical therapy at the Viberg`s hospital [in Danish] Ugeskr Laeger. 2003;165:1179–1182. [PubMed] [Google Scholar]
- 9.Marin R. Scapula winger`s brace: a case series on the management of long thoracic nerve palsy. Arch Phys Med Rehabil. 1998;79:1226–1230. doi: 10.1016/S0003-9993(98)90266-0. [DOI] [PubMed] [Google Scholar]
- 10.Pikkarainen V, Vastamäki M. Serratus palsy: long-term outcome in 85 patients [in Finnish] Suomen Ortop Traumatol. 2009;32:249–251. [Google Scholar]
- 11.Pikkarainen V, Kettunen J, Vastamäki M. The natural course of serratus palsy at 2 to 31 years. Clin Orthop Relat Res. 2013;471:1555–1563. doi: 10.1007/s11999-012-2723-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Plafcan DM, Turczany PJ, Guenin BA, Kegerreis S, Worrell TW. An objective measurement technique for posterior scapular displacement. J Orthop Sports Phys Ther. 1997;25:336–341. doi: 10.2519/jospt.1997.25.5.336. [DOI] [PubMed] [Google Scholar]
- 13.Truong XT, Rippel DV. Orthotic devices for serratus anterior palsy: some biomechanical considerations. Arch Phys Med Rehabil. 1979;60:66–69. [PubMed] [Google Scholar]
- 14.Vastamäki M. Serratus palsy [in Finnish] Duodecim. 1985;101:869–876. [Google Scholar]
- 15.Vastamäki M. Accessory nerve palsy and serratus palsy. Ann Chir Gynaecol. 1996;85:167–171. [PubMed] [Google Scholar]
- 16.Vastamäki M, Kauppila L. Etiologic factors in isolated paralysis of the serratus anterior muscle: a report of 197 cases. J Shoulder Elbow Surg. 1993;2:240–243. doi: 10.1016/S1058-2746(09)80082-7. [DOI] [PubMed] [Google Scholar]
- 17.Warner JJ, Navarro RA. Serratus anterior dysfunction: recognition and treatment. Clin Orthop Relat Res. 1998;349:139–148. doi: 10.1097/00003086-199804000-00017. [DOI] [PubMed] [Google Scholar]
- 18.Wiater JM, Flatow EL. Long thoracic nerve injury. Clin Orthop Relat Res. 1999;368:17–27. [PubMed] [Google Scholar]
- 19.Wolf J. The conservative treatment of serratus palsy. J Bone Joint Surg Br. 1941;23:959–961. [Google Scholar]


