Introduction
Prior to World War I, German medical education strongly influenced training in the United States. One example of this influence is William Steward Halsted MD, a young surgeon from New York who observed postgraduate education while traveling to Germany and Austria in the late 19th century. When Halsted returned to New York, he created the Halsted residency, which set itself apart from less-formal training programs by educating surgeons for a set period of time with a slow, but progressive increase in responsibility and operating time, culminating with independent practice [10, 14].
Surgical education in Germany has a long tradition of excellence [2, 3, 5, 6, 10, 11, 13, 14], producing giants in the field like Billroth [1], Volkmann [18], and Kirschner [9]. In the past, the United States and Europe took their cues from German postgraduate surgical training, which relied heavily on mentorship. But the traditional postgraduate surgical training model in Germany has recently been challenged on several fronts. First, by the ever-increasing specialization of medicine, which required more sophisticated, innovative, and dynamic training programs. Second, by the formation of the European Union and the reunification of Germany, which underscored the need to have a similar, streamlined educational experience throughout the European Union. Because of these pressures, German postgraduate education became more aligned with other European Union educational standards.
In this column, we will examine the educational structure of German postgraduate training, review the recent changes to residency programs in Germany, and determine how those changes have influenced the quality of German medical education.
Residency Programs in Germany
Postgraduate surgical education in Germany was previously based on a preliminary general surgery experience of 6 years, followed by the subspecialty experience (thoracic, cardiovascular, orthopaedic, or plastic surgery). Many countries followed a similar educational structure at the time, which provided a foundation for additional surgical subspecialties. But through the years, injury patterns, as well as treatment of certain fractures, dramatically changed. Fracture care became more sophisticated with operative internal fixation, as opposed to largely plaster methods that were more common even into the 1980s.
German orthopaedic surgery postgraduate training adapted, changing from “orthopaedics and traumatology” to “orthopaedic surgery” in 2003 to match similar educational residency programs in the European Union [2, 5, 11, 13, 16, 17]. Standardization of training in Europe would allow for easier migration within the European Union. More importantly, a standardized curriculum allowed for a more consistent education and postgraduation performance.
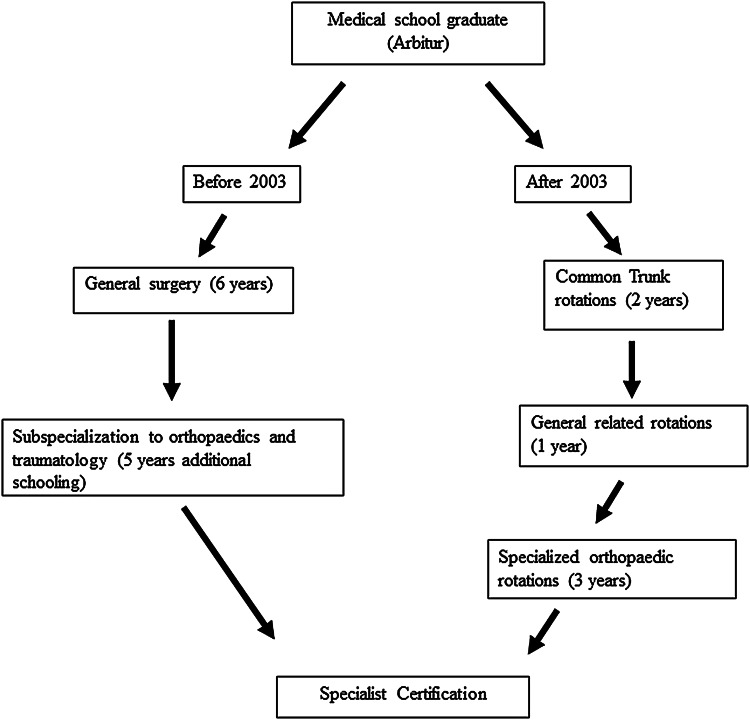
By 2003, 6 years of preliminary general surgery education plus 5 years of additional schooling in orthopaedics and traumatology was considered excessive and led to longer postgraduate training with education in areas not commonly practiced by orthopaedic surgeons. The new German residency structure requires 2 years of common trunk rotations, 1 year of general related rotations, and 3 years for specialized orthopaedic rotations. At minimum, the German medical school graduate (“Arbitur”) will obtain his or her specialist certification in 6 years (Fig. 1). However, the post-2003 structure allows for a more flexible timeline to graduate compared to other countries. The program Chairman (“Chefarzte”) now determines when the resident is ready to graduate, as opposed to a resident completing the program based only on strict timelines.
Fig. 1.
This flowchart compares German orthopaedic surgery residency education before and after 2003.
The new educational structure for German orthopaedic surgery residency is a large departure from the previous educational experience. German doctors ultimately spend less time in training to become practicing orthopaedic surgeons. The average US resident performs 1572 procedures during their 5 years of residency compared to German residents who are eligible to be certified orthopaedic surgeons after performing 730 operative and nonoperative procedures [7]. Still, the new residency model is more consistent with residency programs in other European countries. It is hard to assess how well these changes help produce better doctors when compared to other countries since there is no universal formula for the best residency program. However, future initiatives, in which resident rotations become more focused in both content and assessment, are being discussed by German orthopaedic educators (as with educators in other countries).
German Fellowships and Limitations
A fellowship for an elective orthopaedic surgery like arthroplasty or orthopaedic trauma generally follows training. There are prerequisites for those who choose to work in a certified arthroplasty unit or a Level I trauma center [2, 5, 6]. Further specialization in either “Specialized Trauma Surgery” or “Specialized Orthopaedic Surgery” requires another 2 to 3 years of training. “Specialized Trauma Surgery” requires an additional 420 surgical cases.
One way to “harmonize” surgical standards across Europe is by the European Board of Surgery Qualification, a relatively new, but well-respected, board of trauma surgery standardized exam that consists of an oral exam, a written test, and an exam to assess the ability to speak and understand the English language [8]. The exam is held annually during the German Orthopaedic meeting and in association with the European Society of Trauma and Emergency Surgery. Upon successful completion of the exam, candidates are awarded the title of Fellow of the European Board of Surgery. Other fellowships do exist in Germany, but differ in structure and content from those in other countries. “Special orthopaedic surgery” requires an additional 36 months of education. In the United States, orthopaedic fellowships are generally 1-year in length [5, 11, 12].
Both faculty and those in training have raised concerns that there is insufficient time for certain rotations to provide continuity of care or sufficient surgical volume, though recent documentation shows that residents can document adequate case volumes. The European Working Time Directive officially allows for a total of 48 hours of in-house service per week. The application of the European Working Time Directive has been slow to occur, and residency training programs across the European Union were initially given several years to phase in the work-hour restrictions. Concerns regarding the rigid time directives still remain, and some flexibility in these rules for those in training to assure adequate breadth of experience will still need to be discussed [15].
To put the work-hour restrictions in perspective, Luring et al. [11] surveyed orthopaedic training programs in Germany to determine how many of the procedures were performed by trainees as opposed to faculty. For 35,654 knee arthroscopies, 49% were performed by senior surgeons, 28% by junior attendings, and 27% by trainees. Of 30,642 shoulder arthroscopies, the percentages were 78%, 18%, and 7%, respectively. Of 31,138 knee arthroplasties, the respective percentages were 80%, 14%, and 7%. The authors concluded that there are opportunities to improve the hands-on experience of those in training [11].
Researchers conducted a survey of academic orthopaedic chairmen from the German Society of Trauma and the German Society of Orthopaedic Surgery [13] to assess their perception of the capabilities of new graduates in clinical knowledge and patient care. The survey, which was sent to 954 chairmen and included 220 respondents, showed a perception of limited competence for the graduates. Respondents felt that only 52% of new graduates could handle standard surgical approaches to large joints, and only 24% could independently conduct standard surgical procedures. A recent survey [5] voted against a reduction of the minimum number of surgical cases required by graduates, and are interested in keeping the specialty primarily operative in nature. Additionally, the survey also reported that 86% of those surveyed felt that surgery should be done by the residents themselves, with appropriate supervision. This concern about graduates being ready to practice is also found in other countries. For example, a recent survey of orthopaedic program directors in the United States found that only 17% agreed that all graduates were ready to be attending surgeons [4].
Conclusions
While the above is a snapshot of the German programs in the recent past, this data does support two points: (1) Graduates may need further experience as they “transition to practice” after graduation and (2) the rigid work-hour restrictions may adversely affect the educational experience of residents. Orthopaedic surgery has become a more complex field, often requiring more skill, than the previous generation. These perceptions are bolstered by the longer fellowship times in German orthopaedic education, as well as the opinions derived from both those in training and the orthopaedic chairmen.
Allowing residents to obtain their skills more efficiently is the goal of all educators. Given the constraints on graduate education for work hours and patient safety, producing a safe-practicing surgeon at the end of residency is becoming more difficult. As more centralization occurs, the focus on surgical education should be more diverse. In Germany, by starting a specialty earlier (Levels I–III), there would be more opportunity to obtain orthopaedic experience.
These constraints placed upon orthopaedic surgery educators are not unique to Germany, and this discussion of how to produce competent orthopaedic surgeons in the 21st century is universal to all countries. How Germany has adapted to both external and internal change represents an interesting example for us all.
Footnotes
Note from the Editor-In-Chief: We are pleased to offer the next installment of CORR® Curriculum – Orthopaedic Education, a quarterly column. The goal of this column is to focus on the mechanics of resident education. We welcome reader feedback on all of our columns and articles; please send your comments to eic@clinorthop.org.
The authors certify that they, or any members of their immediate families, have no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
The opinions expressed are those of the writers, and do not reflect the opinion or policy of CORR ® or the Association of Bone and Joint Surgeons®.
References
- 1.Absolon KB. The Surgeon’s Surgeon. Theodor Billroth 1829–1894. Lawrence, KS: Coronado Press; 1979.
- 2.Achatz G, Perl M, Stange R, Mutschler M, Jarvers JS, Münzberg M. How many generalists and how many specialists does orthopedics and traumatology need? [in German] Unfallchirg. 2013;116:29–33. doi: 10.1007/s00113-012-2303-z. [DOI] [PubMed] [Google Scholar]
- 3.Andruszkow H, Haaster C, Lob G, Pfeifer R, Stengel D, Hildebrand F, Pape HC. Status of Road Safety and Injury Burden: Europe. J Orthop Trauma. 2014;29:S39–40. doi: 10.1097/BOT.0000000000000110. [DOI] [PubMed] [Google Scholar]
- 4.Baldwin K, Namdari S, Donegan D, Klamath AF, Mehta S. Early effects of resident work hour restictions on patient safety: systemic review and plea for improved studies. J Bone Joint Surg. 2011;93:e5. doi: 10.2106/JBJS.J.00367. [DOI] [PubMed] [Google Scholar]
- 5.Chances and risks of a new residency program for orthopedics and trauma surgery [in German]. Z Orthop Unfall. 2013;151:126–128. [DOI] [PubMed]
- 6.Chenot JF. Medical studies in germany [in German] German Medical Science. 2009;7:2. doi: 10.3205/000061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Flierl MA. German surgical residency training - quo vadis? Patient Saf Surg. 2008;2:9. doi: 10.1186/1754-9493-2-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Greenhalgh R. The European Board of Surgery Qualification (EBSQ) was born in 1996. Ann R Coll Surg Engl. 1997;79(1 Suppl):3–4. [PubMed] [Google Scholar]
- 9.Hamelmann H. The past, present and future of German surgery [in German] Jpn J Surg. 1984;14:444–451. doi: 10.1007/BF02469785. [DOI] [PubMed] [Google Scholar]
- 10.Johns Hopkins Medicine. Department of surgery. History. Available at: http://www.hopkinsmedicine.org/surgery/about/history.html. Accessed. April 13, 2015.
- 11.Luring C, Tingart M, Beckmann J, Grifka J, Bathis H. Surgical training in orthopaedic and trauma departments in Germany [in German] Z Orthop Unfall. 2010;148:466–470. doi: 10.1055/s-0030-1249792. [DOI] [PubMed] [Google Scholar]
- 12.Medical Association of Lower Saxony, Hannover District Office. Available at: https://www.aekn.de/. Accessed March 12, 2015.
- 13.Niethard M, Depeweg D. 6 years after reformation of the specialty training reglementation–is there still room for improvement? [in German] Z Orthop Unfall. 2010;148:471–475. doi: 10.1055/s-0030-1250170. [DOI] [PubMed] [Google Scholar]
- 14.Olch PD. William Stewart Halsted. Ann Surg. 2006;243:418–425. doi: 10.1097/01.sla.0000201546.94163.00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pape HC. Restricted duty hours and implications on resident education-Are different trauma systems effected in a different way? Injury. 2010;41:125–127. doi: 10.1016/j.injury.2009.12.011. [DOI] [PubMed] [Google Scholar]
- 16.Rixen D, Tempka A, Lob G. Has something in the quality of orthopedic / trauma surgery training changed? [in German] Unfallchirg. 2006;109:339–347. doi: 10.1007/s00113-006-1071-z. [DOI] [PubMed] [Google Scholar]
- 17.Steckel H, Musahl V, Fu FH, Baums MH, Schultz W, Klinger HM. Orthopedic - trauma surgery specialist training in the German and US - American standards [in German] Z orthop. 2006;144:357–361. doi: 10.1055/s-2006-942125. [DOI] [PubMed] [Google Scholar]
- 18.Willy C, Schneider P, Engelhardt M, Hargens AR, Mubarak SJ. Richard von Volkmann: Surgeon and renaissance man. Clin Orthop Relat Res. 2008;466:500–506. doi: 10.1007/s11999-007-0007-4. [DOI] [PMC free article] [PubMed] [Google Scholar]