Abstract
Complementary and alternative medicine (CAM; 補充與替代醫學 bǔ chōng yǔ tì dài yī xué) is widely practiced among stroke patients globally. We conducted a study to determine the pattern of CAM use and its associated factors in stroke survivors attending a tertiary hospital in Malaysia within 6 months after the stroke. This was a prospective cohort study that included all stroke patients who were admitted to a tertiary center in Malaysia from December 2009 to December 2010. Patients were interviewed and examined within 72 hours of admission. The sociodemographic data and medical history were collected. Clinical examinations were done to assess the stroke severity using the Scandinavian Stroke Scale and functional status based on modified Barthel index (MBI). Patients were reassessed at 6 months after the stroke on the CAM use and functional status (MBI). The response rate was 92%. The study population consisted of 52 men and 41 women with a mean age of 63.7 ± 10.3 years. Sixty-seven percent practiced CAM. Massage was the most frequently used method (63.4%), followed by vitamins (7.5%). In multiple logistic regression analysis, functional status (MBI score) on discharge (p = 0.004, odds ratio 1.034, 95% confidence interval 1.01–1.06) and Scandinavian Stroke Scale score (p = 0.045, odds ratio 1.87, 95% confidence interval 1.01–3.43) were significant predictors for use of CAM. In conclusion, the use of CAM among stroke survivors is high. Patients who have better functional status on discharge and less severe stroke are more likely to use CAM.
Keywords: cerebrovascular accident, complementary and alternative medicine, stroke, traditional medicine, functional status
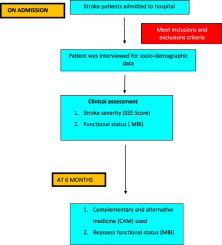
Graphical abstract
1. Introduction
Stroke is a worldwide health problem and a leading cause of adult disability.1 Annually, 15 million people worldwide suffer a stroke. Of this total, 5 million die and another 5 million are left permanently disabled.1,2 Stroke is one of the top five leading causes of disability-adjusted life years in Malaysia.3 Currently, there is a significant proportion of stroke patients who choose to use complementary and alternative medicine (CAM; 補充與替代醫學 bǔ chōng yǔ tì dài yī xué).4,5
In the United States, CAM use has increased from 33.7% to 42.1% in the 1990s.6
One study on stroke patients reports that 46% of stroke survivors engage in some form of complementary medicine.6 Acupuncture was chosen more frequently by stroke survivors in the United States.7 In Korea, 54% of stroke patients used CAM.8 The reasons why people chose such therapies include positive views of complementary therapies; this translates to 57% of users who felt that CAM is effective, 84% who believed that it improved the symptoms of stroke, and 16% who felt that it was effective in achieving psychological relaxation.8 In a study done in one of the outpatient clinic in Kelantan, the authors found that the prevalence of CAM use among adult patients is high (63%) during their lifetime, with herbal medicine as the most frequently used therapy.9
Patients who use CAM are typically unaware of the its potential toxicities and possible adverse interactions with prescription medications.10,11 Although there are reports on CAM use among stroke patients in the United States and Korea, to our knowledge there are no corresponding data available among Malaysian stroke survivors.6,8 Understanding of the prevalence and patterns of CAM use among stroke survivors is important in the education of patients and in improving patient–doctor relationship. Therefore, we conducted a study to assess the pattern of CAM use and its associated factors among stroke survivors in a tertiary center in Malaysia.
Many CAM modalities have been used by stroke survivors all over the world especially traditional Chinese medicine. Thus, it would be beneficial to know if there are associations between these CAM practices and the functional status of stroke survivors. This knowledge can be explored in further studies looking into these matters.
2. Patients and methods
The study was conducted from December 2, 2009 until December 31, 2010, featuring a prospective cohort of 101 stroke patients with acute stroke admitted to the medical wards of a tertiary hospital (Hospital Raja Perempuan Zainab II) in the northeast region of Peninsular Malaysia.
Stroke was defined as clinical syndromes characterized by rapidly developing clinical symptoms and/or signs of focal (or at times global) loss of cerebral function of sudden onset and lasting for more than 24 hours (or leading to death) with no apparent cause rather than vascular in origin.12
CAM is defined as the use of any medication or nonmedication therapy that was different from allopathic medicine within 6 months of the study period with the intention of curing stroke.13 The types of CAM that were included in the study were massage, herbal medicines, vitamins, homeopathy, reflexology, traditional healers that used special ceremonies and special spells, self-prayer or intercessory prayer or any solemn act requesting help from God, traditional Chinese medicine, and “others,” which referred to other types of nonallopathic therapies that did not match the above definition.
The study included all patients aged older than 18 years with clinical diagnosis of first-ever stroke and did not require intensive care. Premorbidly bedridden patients, pregnant women, patients with preexisting neuron/motor disorders, patients with mental illness, and patients with computed tomography brain findings that showed findings other than vascular in origin were excluded. The criterion on mental illness was based on medical history and medical records of the patients. There was no specific time frame and those individuals were excluded because we postulated difficulty in compliance to follow-up as well as difficulty in verifying the history of CAM used.
All stroke patients who were admitted and fulfilled the inclusion criteria were included in the study because only a few eligible patients were available. Informed consent forms were obtained from the patients or caregivers for participation into the study after the study protocol was explained to them.
Sociodemographic data of the patients were obtained within 72 hours of admission. The patients were then clinically assessed by the study investigator using the Scandinavian Stroke Scale (SSS) score.14 The patients' functional status was assessed using the modified Barthel index (MBI)15 by the study investigator and/or allocated physiotherapist when they were discharged. The SSS was used to assess the stroke severity on admission.14 The SSS evaluated the level of consciousness, eye movement, motor power in arm, hand and leg, orientation, aphasia, facial paresis, and gait of the participants with the total score ranging from 0 to 58.14 A higher score indicates less severe neurological impairment.
On follow-up at 6 months, patients were interviewed regarding the use of CAM during the past 6 months, the types of CAM used, and attendance in rehabilitation program(s). Functional status of the patients was then reassessed (using the MBI score) by the same study investigator at baseline.
2.1. Data entry and statistical analysis
All data were entered and analyzed using the Statistical Program for Social Sciences (SPSS) version 12.0 (SPSS Inc. 2003). Multiple logistic regression analysis was used to assess the factors associated with CAM used. The outcome variable centers on whether CAM was used. The method used for variable selection was the backward and forward stepwise procedure. All possible two-way interactions were checked, and those significant variables were included in the model. The independent variables were fitted into multiple logistic regression, and multicollinearity was checked. Fitness of model was tested using the Hosmer–Lemeshow goodness-of-fit test, the classification table, and the receiver operator characteristic curve.
2.2. Approval by research and ethics committee
The protocol was approved by the Research Ethics Committee (Human), School of Medical Sciences, Universiti Sains Malaysia, on August 13, 2009, and the Ministry of Health Malaysia on November 17, 2009.
3. Results
A total of 101 patients were recruited into the study. However, eight had passed away owing to other medical causes (3 patients died because of acute myocardial infarction, 2 died because of acute renal failure, 2 died because of sepsis, and another died because of recurrent stroke) prior to completing the study, leaving a total of 93 patients who completed the study. Thus, the response rate of the study was 92%. Table 1 shows the demographic and clinical characteristics of the study participants. Types of strokes were predominantly ischemic in origin (81.7%).
Table 1.
Sociodemographic and medical characteristic of study patients.
| Variables | Total | CAM user | Nonuser |
|---|---|---|---|
| Age | 63.7 (10.3)a | 64.3 (9.6)a | 62.5 (11.5)a |
| Sex | |||
| Male | 52 (55.9%) | 34 (54.8%) | 18 (58.1%) |
| Female | 41 (44.0%) | 28 (45.2%) | 13 (41.9%) |
| Education | |||
| Tertiary | 14 (15.0%) | 9 (14.5%) | 5 (16.1%) |
| Secondary | 33 (35.5%) | 18 (29.0%) | 15 (48.4%) |
| Primary | 17 (18.3%) | 13 (30.0%) | 4 (12.9%) |
| No formal education | 29 (31.2%) | 22 (35.5%) | 7 (22.6%) |
| Total income/mo | 1120.8 (1048.1)a | 1143.2 (1141.3)a | 1075.8 (846.6)a |
| Diabetes | 28 (30.0%) | 17 (27.4%) | 11 (35.5%) |
| Hypertension | 57 (61.3%) | 37 (60.0%) | 20 (64.5%) |
| CAD | 12 (12.9%) | 6 (0.1%) | 6 (19.4%) |
| Diagnosis | |||
| Ischemic | 76 (81.7%) | 50 (80.6%) | 26 (83.9%) |
| Hemorrhage | 17 (18.3%) | 12 (19.4%) | 5 (16.1%) |
| Attend rehabilitation | 18 (19.4%) | 11 (17.7%) | 7 (22.6%) |
| SSS score | 33.2 (11.3)a | 33.2 (11.7)a | 33.3 (11.5)a |
| MBI on admission | 42.4 (24.5)a | 40.47 (21.1)a | 52.84 (26.8)a |
| MBI at 6 mo | 73.7 (31.2)a | 76.63 (25.9)a | 84.6 (21.2)a |
CAD = coronary artery disease; CAM = complementary and alternative medicine; MBI = modified Barthel index; SSS = Scandinavian Stroke Scale.
Mean and standard deviation.
Table 2 shows the pattern of CAM practice among the stroke survivors. Nearly two-thirds of study participants used CAM. Among the choices of CAM practice, massage was the top choice (63.4%).
Table 2.
Characteristics of CAM use among stroke patients.
| Variables | Total, n = 93 (%) | |
|---|---|---|
| TCM use | ||
| Yes | 62 (66.7) | |
| No | 31 (33.3) | |
| Number of TCM | ||
| 1 | 52 (83.8%) | |
| 2 | 8 (12.9%) | |
| 3 | 1 (0.2%) | |
| 4 | 1 (0.2%) | |
| Type of TCM | ||
| Massage | ||
| Yes | 34 (36.6) | |
| No | 59 (63.4) | |
| Herbal | ||
| Yes | 91 (97.8) | |
| No | 2 (2.2) | |
| Vitamins | ||
| Yes | 86 (92.5) | |
| No | 7 (7.5) | |
| Traditional healers | ||
| Yes | 91 (97.8) | |
| No | 2 (2.2) | |
| Diet | No | 93 (100) |
| Reflexology | No | 93 (100) |
| Traditional Chinese Medicine | No | 93 (100) |
| Homeopathy | No | 93 (100) |
| Others | No | 90 (96.8) |
| Yes | 3 (3.2) | |
CAM = complementary and alternative medicine; TCM = traditional Chinese medicine.
In the multiple logistic regression analysis, we included age, education, total monthly income, SSS score, and functional status (MBI score) during admission. Based on this analysis, we found that functional status (MBI score) on discharge (p = 0.004, odds ratio 1.034, 95% confidence interval 1.01–1.06) and SSS score (p = 0.045, odds ratio 1.87, 95% confidence interval 1.01–3.43) were the significant associated factors for CAM used among the stroke survivors.
4. Discussion
We found that more than 60% of the stroke survivors reported using some form of CAM. In this study, the patients used CAM as adjunct to the conventional medications. This figure is higher compared to other studies conducted among stroke patients.7,8,14,16 The estimates of CAM use in this study are comparable with other studies done among individuals with chronic illnesses such as diabetes,17 rheumatology,18 or physical disabilities.19 The rate of CAM use in our study is also comparable with that in a study done in an outpatient setting in Malaysia.9 The highly prevalent use of CAM in our study could be attributable to several factors. One of them could be the perceived belief in CAM that would motivate the patients. Another reason would be the perceived lack of community-based therapy for stroke patients. For example, some of the patients perceived that psychosocial care is not satisfactorily attended to by allopathic practitioners.
The most commonly used CAM in this study is massage. This may be attributable to massage being considered by our patients as traditional practice. Majority of the patients in this study are Malays who generally believe massage can improve circulation and muscle tone, and thus expedite the healing process in stroke patients.
In comparison, a study conducted in the United States7 among stroke survivors found that the most commonly used is CAM is herbal medicine. A study in Korea showed that traditional Chinese medicine or oriental medicine is the most common CAM used among stroke survivors. Interestingly, none of the stroke survivors in our study had chosen acupuncture, which is one of the common CAM options among stroke patients.7,8 This is most probably attributable to the small number of Chinese respondents in this study, which reflects the population sampled.
In this study, we found that patients with less severe stroke and better functional status on discharge were more likely to use CAM. We could not find other studies that had looked into the relationship between severity of stroke, patients' functional status, and CAM use. Further studies are necessary to clarify this matter. However, unlike other studies performed among stroke survivors,7,8,16 we found no correlation between sociodemographic factors and the use of CAM. We also found that there was no correlation between use of CAM and functional status at 6 months after the stroke.
This study has several limitations. First, we did not assess CAM use prior to the stroke and also compliance to the prescription of conventional medicines used in this study to look for possible drug interaction. We also did not inquire whether the patients had a discussion with their physicians about the use of CAM. The number of stroke patients in this study is small, and thus the results cannot be generalized to all stroke patients in Malaysia.
5. Conclusion
In conclusion, the prevalence of CAM use among stroke patients is high. Patients who have better functional status on discharge and less severe stroke are more likely to use CAM. Among the types of CAM, massage is highly practiced among stroke patients. Use of CAM is not associated with functional outcome at 6 months after the stroke; therefore, the benefit of CAM in this group of patients is still questionable. Future studies are needed to assess the benefit(s) of specific CAM practices for stroke patients.
Conflicts of interest
We declare there is no financial and personal relationship with other people or organizations that could inappropriately influence this research.
Acknowledgments
We acknowledge Universiti Sains Malaysia (304/PPSP/6139074) for the grants that enabled this study to be conducted. We also gratefully acknowledge the cooperation of all the staff involved in this study.
Footnotes
Peer review under responsibility of The Center for Food and Biomolecules, National Taiwan University.
References
- 1.Merican J.S., Piaw C.S., Basri H. MOH Clinical Practice Guidelines: Management of Ischaemic Stroke. 1st ed. Malaysia Ministry of Health; Malaysia: 2006. Malaysia Ministry of Health; p. 1. [Google Scholar]
- 2.Report W.H.O. 2003. http://www.who.int/cardiovascular_diseases/en/cvd_atlas_15_burden_stroke.pdf Available from:
- 3.Loo K.W., Gan S.W. Burden of stroke in Malaysia. Int Stroke J. 2012;7:165–167. doi: 10.1111/j.1747-4949.2011.00767.x. [DOI] [PubMed] [Google Scholar]
- 4.Wainapel S.F., Thomas A.D., Kahan B. Use of alternative therapies by rehabilitation outpatients. Arch Phys Med Rehabil. 1998;79:1003–1005. doi: 10.1016/s0003-9993(98)90102-2. [DOI] [PubMed] [Google Scholar]
- 5.Jaya F., Win N.M., Abdullah M.R., Abdullah J.M. Stroke patterns in Northeast Malaysia: a hospital-based prospective study. Neuroepidemiology. 2002;21:28–35. doi: 10.1159/000048611. [DOI] [PubMed] [Google Scholar]
- 6.Eisenberg D.M., Davis R.B., Ettner S.L. Trends in alternative medicine use in the United States, 1990–1997: results of a follow-up national survey. JAMA. 1998;280:1569–1575. doi: 10.1001/jama.280.18.1569. [DOI] [PubMed] [Google Scholar]
- 7.Shah S.H., Engelhardt R., Ovbiagele B. Patterns of complementary and alternative medicine use among United States stroke survivors. J Neurol Sci. 2008;271:180–185. doi: 10.1016/j.jns.2008.04.014. [DOI] [PubMed] [Google Scholar]
- 8.Shin Y.I., Yang C.Y., Joo M.C., Lee S.G., Kim J.H., Lee M.S. Patterns of using complementary and alternative medicine by stroke patients at two university hospitals in Korea. Evid Based Complement Alternat Med. 2008;5:231–235. doi: 10.1093/ecam/nem025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hassan F., Shaaban J. Use of traditional/complemetary medicine (T/CM) among adult patients attending family medicine clinic at Hospital Universiti Sains Malaysia. Int Med J. 2005;12:133–138. [Google Scholar]
- 10.Taylor D., Walsham N., Taylor S.E., Wong L.F. Complementary and alternative medicines versus prescription drugs: perceptions of emergency department patients. Emerg Med J. 2006;23:266–268. doi: 10.1136/emj.2005.026138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Drew Ak, Myers S.P. safety issues in herbal medicine:implications for the health professionals. Med J Aust. 1997;166:538–541. doi: 10.5694/j.1326-5377.1997.tb123246.x. [DOI] [PubMed] [Google Scholar]
- 12.Malaysia M.O.H. 2006. Clinical Practice Guideline : Management of Ischaemic Stroke; pp. 1–5. [Google Scholar]
- 13.World Health Organisation. WHO Traditional Medicine Strategy 2002–2005.
- 14.Christensen H., Boysen G., Truelsen T. The Scandinavian stroke scale predicts outcome in patients with mild ischemic stroke. Cerebrovasc Dis. 2005;20:46–48. doi: 10.1159/000086280. [DOI] [PubMed] [Google Scholar]
- 15.Mahoney F.I., Barthel D.W. Functional evaluation: the Barthel index. Md State Med J. 1965;14:61–65. [PubMed] [Google Scholar]
- 16.Blackmer J., Jefromova L. The use of alternative therapies in Sasketchwan stroke rehabilitation stroke population. BMC Complement altern Med. 2000;2:7. doi: 10.1186/1472-6882-2-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Garrow D., Egede L.E. Association between complementary and alternative medicine use, preventive care practices, and use of conventional medicne services among adults with diabetes. Diabetes Care. 2006;29:15–19. doi: 10.2337/diacare.29.01.06.dc05-1448. [DOI] [PubMed] [Google Scholar]
- 18.Boisset M., Fitzcharles M.A. Alternatives medicne use by rheumatology patients in a universal health care setting. J Rheumatol. 1994;21:148–152. [PubMed] [Google Scholar]
- 19.Herbert H.K., Christopher G., Jean K., David M.E. Alternative health care: its use by individuals with physical disabilities. Arch Phys Med Rehabil. 1998;79:1440–1447. doi: 10.1016/s0003-9993(98)90241-6. [DOI] [PubMed] [Google Scholar]


