Abstract
Tracheobronchopathia osteochondroplastica (TPO) is a rare disorder characterised by development of cartilaginous and bony nodules in the trachea. It usually affects elderly males with total prevalence of disease reported to be around 0.1%. Even though multiple theories and associations have been described, the exact cause of the disease remains unknown. Its presentation is non-specific with many cases being diagnosed incidentally. Chronic cough and dyspnoea are the most common presenting symptoms, but some cases may present with severe airway compromise. We present a case of a 70-year-old man with IgA λ multiple myeloma, who was diagnosed with TPO by flexible bronchoscopy.
Background
Tracheobronchopathia osteochondroplastica (TPO) is a rare disease entity characterised by development of nodules in the trachea. We present a case of 70-year-old man with multiple myeloma (MM) who was incidentally diagnosed with TPO. It mostly presents as chronic cough and dyspnoea, but can also cause upper airway compromise. It is important for physicians to be alert to this pathological entity in cases of chronic cough and dyspnoea where all other causes have been ruled out. The common modalities used in its management include cryotherapy and mechanical debulking. Further research may provide more sophisticated tools to treat upper airway obstruction due to endotracheal nodules.
Case presentation
We describe a case of a 70-year-old man with IgA λ MM diagnosed 3 years before the current presentation. There was no evidence of a secondary malignancy. The patient was admitted with worsening dyspnoea. On examination, he had increased work of breathing and diffuse crackles in the lung fields, which were more pronounced at the bases. His laboratory tests at presentation to the medical intensive care unit (MICU) were significant for acute kidney injury with creatinine worsening from his baseline of 1.1–2.1 mg/dL, white cell count of 40 K/µL and platelets at 109/L. His respiratory decline was thought to be from a combination of pulmonary oedema and pneumonia on a background of a chronic interstitial process (this process remained undiagnosed due to the rapidity and severity of his decline). The patient was started on broad spectrum antibiotics and initiated on aggressive diuresis. A CT scan of the chest confirmed the suspicion and also demonstrated cartilaginous stalactites encroaching into the tracheal lumen and normal appearing bronchi (figure 1A–C). FB demonstrated nodular deformities along the tracheal cartilages involving both the anterior and lateral wall, but sparing the membranous posterior wall (figure 2). This pattern is classic for TPO. A mucosal biopsy demonstrated submucosal calcified bone without cartilaginous or haematopoietic foci (figure 3). The bronchoalveloar lavage fluid cultures were negative for any pathogens. As the symptoms were not considered to be secondary to TPO no specific treatment was offered. The patient remained in the MICU and later succumbed to multiorgan failure about 30 days after the initial presentation. His death was likely due to a combination of sepsis and relative immunosuppression.
Figure 1.

(A) CT of the chest showing cartilaginous stalactites encroaching into the tracheal lumen. (B) CT scan at the level of the bronchii with normal airways. (C) Lung windows demonstrating severe parenchymal disease.
Figure 2.
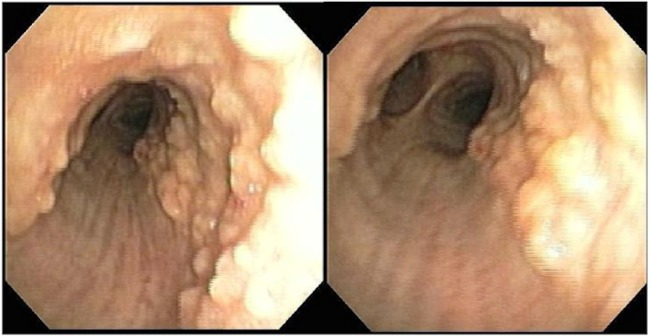
Flexible bronchoscopy showing nodular deformities along the tracheal cartilages involving both the anterior and the lateral wall, but sparing the membranous posterior wall.
Figure 3.
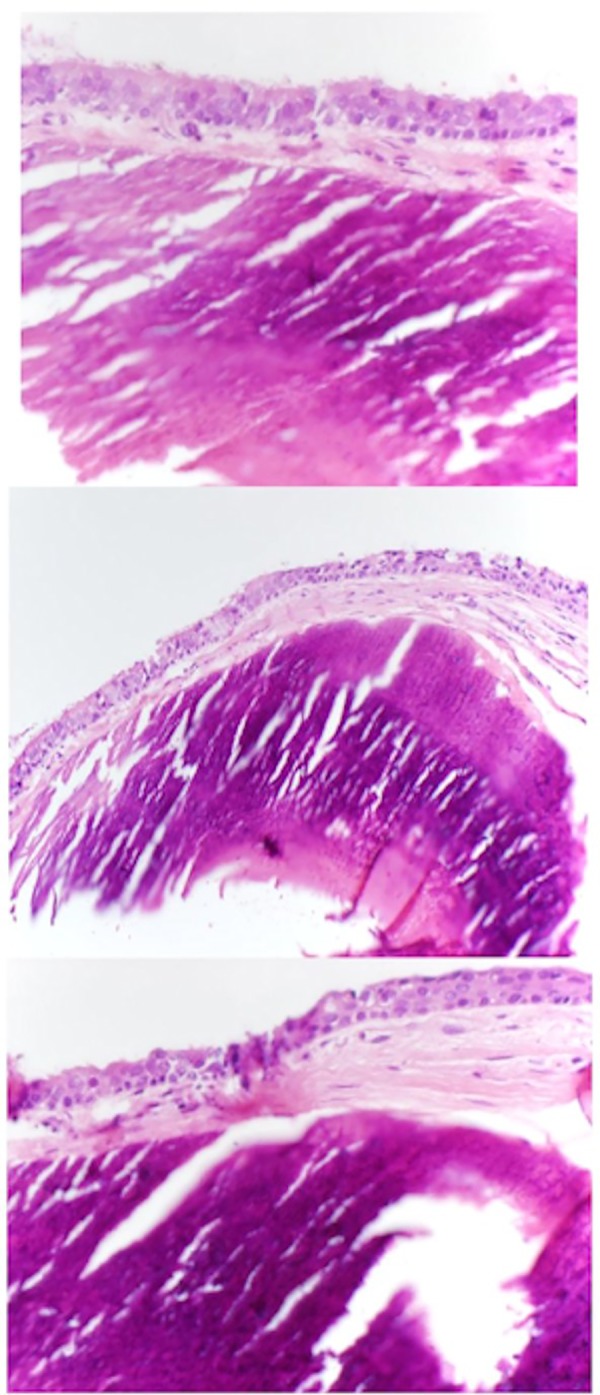
Mucosal biopsy showing (A) calcified bone with overlying ciliated respiratory epithelium (40×); (B) calcified bone with overlying ciliated respiratory epithelium especially on the left (20×); (C) calcified bone with overlying epithelium showing some loss of cilia and squamous metaplasia (40×).
Discussion
TPO is a rare disorder of elderly men that is characterised by submucosal endoluminal projections of cartilaginous and bony nodules in the trachea and bronchi. Involvement of the trachea with sparing of the posterior wall, as in our patient, is considered pathognomonic.1 Wilks first described the disease in 1857 as ossific deposits in the trachea.2 Most of the existing knowledge about this entity is from case reports and case series. The two most extensive case series by Leske et al3 and Harma et al4 involved 41 and 30 patients, respectively. The current incidence of TPO is estimated to be approximately 0.11%.5 It is a benign disease and most of the cases are diagnosed incidentally at autopsies, or through bronchoscopies, MRI and CT scans carried out for other reasons, and, rarely, as a cause of difficult intubation.1 It is considered a disease of the elderly, with a mean age of 63 years.3
The cause of TPO is unknown but several theories have been proposed. Virchow proposed ecchondrosis and exostosis from cartilaginous rings with subsequent ossification as a possible mechanism.6 Metaplasia of elastic tissue has been proposed as a possible mechanism.6 Multiple associations with other diseases have been reported but a causal relationship remains uncertain. Association with atrophic rhinitis (ozena), bacteria such as Klebsiella ozaenae, typical and atypical mycobacteria, pneumoconiosis and amyloidosis, and with malignancies such as lung cancer, have been reported.3 7–9 Our case report may be the first to report a co-existence of MM and TPO. Irrespective of the cause, bone morphogenic protein (BMP-2) and transforming growth factor (TGF-1) have been implicated in pathogenesis of formation of cartilaginous and bony nodules.10 Histopathology, when available, demonstrates cartilaginous nodules with islands of bone formation and, rarely, even marrow formation.
Most patients are asymptomatic at the time of diagnosis. When present, symptoms include chronic cough, haemoptysis, dysphonia and dysphagia.2 3 5 Decreased efficiency of clearing respiratory secretions may lead to lower respiratory infections.11 TPO is usually a non-progressive disorder, but rare cases of severe and rapid airway stenoses have been reported.5 10 12 A diagnosis can be made on imaging alone. However, FB may be useful in ruling out other aetiologies.10 Biopsies can be performed to confirm the diagnosis but are not considered necessary. We can attest from experience that the bony nature of the nodules make biopsies very difficult.
Management is largely symptomatic and involves treating associated conditions, for instance, coughs, infections, chronic obstructive pulmonary disease and bronchiectasis.12 The usual therapies include antitussive medications, antibiotics and clearance therapies.13 14 Specific treatment for TPO is currently only considered in cases with mechanical airway obstruction. Laser/argon plasma coagulation/cryotherapy, combined with mechanical debulking via rigid bronchoscopy, are frequently used in patients with symptomatic airway compromise.5 The ablative therapies are only helpful when TPO is the only lung pathology.5
In our case, the acute decline was likely due to pneumonia and the chronic interstitial process. No specific treatment for TPO was offered to our patient, as TPO was considered to be an incidental finding and his symptoms were mainly thought to be due to the severe lung disease and pneumonia.
Learning points.
While the reported incidence of tracheobronchopathia osteochondroplastica is around 0.1% in patients undergoing thoracic imaging and bronchoscopies, its true prevalence may be higher than currently recognised.
It should be considered as a possible cause of recurrent pulmonary infections, chronic cough, dyspnoea or haemoptysis when the usual causes have been ruled out.
More studies and experience are needed to understand this disease process, so that we can help that rare patient with severe and rapid airway compromise.
Footnotes
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Abu-Hijleh M, Lee D, Braman SS. Tracheobronchopathia osteochondroplastica: a rare large airway disorder. Lung 2008;186:353–9. 10.1007/s00408-008-9113-7 [DOI] [PubMed] [Google Scholar]
- 2.Wilks S. Ossific deposits on the larynx, trachea and bronchi. Trans Pathol Soc Lond 1857;8:88. [Google Scholar]
- 3.Leske V, Lazor R, Coetmeur D et al. Tracheobronchopathia osteochondroplastica: a study of 41 patients. Medicine (Baltimore) 2001;80:378–90. 10.1097/00005792-200111000-00004 [DOI] [PubMed] [Google Scholar]
- 4.Härmä RA, Suurkari S. Tracheopathia chondro-osteoplastica. A clinical study of thirty cases. Acta Otolaryngol 1977;84:118–23. 10.3109/00016487709123949 [DOI] [PubMed] [Google Scholar]
- 5.Jabbardarjani HR, Radpey B, Kharabian S et al. Tracheobronchopathia osteochondroplastica: presentation of ten cases and review of the literature. Lung 2008;186:293–7. 10.1007/s00408-008-9088-4 [DOI] [PubMed] [Google Scholar]
- 6.Rokitansky K, Dalgaard JB. Tracheopathia chondroosteoplastica. A case elucidating the problems concerning development and ossification of elastic cartilage. Acta Pathol Microbiol Scand 1947;24:118–34. [Google Scholar]
- 7.Mariotta S, Pallone G, Pedicelli G et al. Spiral CT and endoscopic findings in a case of tracheobronchopathia osteochondroplastica. J Comput Assist Tomogr 1997;21:418–20. 10.1097/00004728-199705000-00015 [DOI] [PubMed] [Google Scholar]
- 8.Pinheiro GA, Antao VC, Müller NL. Tracheobronchopathia osteochondroplastica in a patient with silicosis: CT, bronchoscopy, and pathology findings. J Comput Assist Tomogr 2004;28:801–3. 10.1097/00004728-200411000-00012 [DOI] [PubMed] [Google Scholar]
- 9.Erelel M, Yakar F, Bingol ZK et al. Tracheopathia osteochondroplastica: two unusual cases. J Bronchology Interv Pulmonol 2010;17:241–4. 10.1097/LBR.0b013e3181e64a00 [DOI] [PubMed] [Google Scholar]
- 10.Tajima K, Yamakawa M, Katagiri T et al. Immunohistochemical detection of bone morphogenetic protein-2 and transforming growth factor beta-1 in tracheopathia osteochondroplastica. Virchows Arch 1997;431:359–63. 10.1007/s004280050111 [DOI] [PubMed] [Google Scholar]
- 11.Hussain K, Gilbert S. Tracheopathia osteochondroplastica. Clin Med Res 2003;1:239–42. 10.3121/cmr.1.3.239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen AY, Donovan DT. Impaired ciliary clearance from tracheopathia osteoplastica of the upper respiratory tract. Otolaryngol Head Neck Surg 1997;117:S102–4. 10.1016/S0194-5998(97)70071-8 [DOI] [PubMed] [Google Scholar]
- 13.Prakash UB, McCullough AE, Edell ES et al. Tracheopathia osteoplastica: familial occurrence. Mayo Clin Proc 1989;64:1091–6. 10.1016/S0025-6196(12)64978-7 [DOI] [PubMed] [Google Scholar]
- 14.Los H, Schramel FM, Van der Harten JJ et al. An unusual cause of recurrent fever. Eur Respir J 1997;10:504–7. 10.1183/09031936.97.10020504 [DOI] [PubMed] [Google Scholar]


