Abstract
Paranasal sinus infections are very common. Dental infections, tumours and anatomical malformations can cause unilateral sinusitis. Most cases can be treated without complications. However, rare life-threatening intracranial complications can occur. Generally, an intracranial complication progresses rapidly and can cause meningismus, focal neurological disorders, loss of consciousness and seizures. In such cases, an emergency craniotomy and concurrent sinus surgery are required. This article presents a 16-year-old patient with pansinusitis and subdural empyema that developed after a dental abscess.
Background
Paranasal sinus infections are very common. Most cases can be treated without complications. However, rare life-threatening intracranial complications can result from the spread of paranasal sinus infections. Generally, an intracranial infection spreads rapidly and can cause meningismus, focal neurological disorders, loss of consciousness and seizures.1 An emergency craniotomy and concurrent sinus surgery are mandatory. Although Gram-positive bacteria are observed in the majority of microbiological cultures, Gram-negative and anaerobes bacteria can also be seen. This article presents a 16-year-old patient with pansinusitis and subdural empyema that developed after a dental abscess.
Case presentation
A sixteen-year-old male patient was admitted to our clinic with symptoms of a growing facial swelling after dental infection. There was no known disease in the history. The patient started to develop dental and facial pain 1 week earlier. When the swelling on the left side of his face developed, craniofacial CT was conducted. This showed an infected left anterior ethmoidal sinus, a thickening of the maxillary sinus mucosa and a sequestered maxillary premolar. The patient was referred to our clinic with suspected orbital cellulitis. At the initial examination, a left suborbital premaxillary subperiosteal abscess extending to the masseter muscle and a low-grade fever were observed. Pus was aspirated from the swelling with a 7-G needle and sent for microbiological investigation. The patient was diagnosed with a premaxillary abscess resulting from an upper premolar infection and was treated empirically with clindamycin 600 mg two times per day and ceftriaxone 2 g two times per day intravenous. The abscess was drained with a gingivobuccal incision. When the patient developed a severe headache and agitation 24 h after treatment initiation, the repeat CT showed left pansinusitis (figure 1) and subdural empyema. Brain MRI (figure 2) was performed and a neurosurgery consultation was obtained. An emergency craniotomy and subdural empyema drainage were performed. The surgical field was irrigated with saline and a subdural drain was inserted (figure 3). In the same surgical session, a middle meatal antrostomy, anterior ethmoidectomy and frontal sinus recess surgery were performed endoscopically. Since the mucosa in the recess was very oedematous and the sinuses were closed, trepanation of the frontal sinus was performed. All of the paranasal sinuses and the abscess were irrigated three times with oxygenated isotonic solution. A silicon drain was then placed in the frontal sinus ostium. The infected sequestered tooth was removed. Owing to the quite high transition to cerebrospinal fluid of metronidazole, clindamycin 600 mg therapy was changed to metronidazole 500 mg four times a day therapy at the 24th hour of initial therapy. The patient was admitted to the intensive care unit for 3 days postoperatively to monitor any increased intracranial pressure. The cerebrospinal fluid culture was negative, while the abscess culture grew Streptococcus viridans. Treatment was continued for 14 days with ceftriaxone 2 g two times a day and metronidazole 500 mg four times a day. The subdural and frontal sinus drain were removed on the fifth and seventh days, respectively, in the postoperative period. The patient was discharged on the 14th postoperative day. Follow-up assessments 4 and 8 weeks postoperatively were normal.
Figure 1.

A left premaxillary soft tissue swelling (black arrow), an obliterated left maxillary sinus and a sequestered tooth root (*) are seen on the axial paranasal CT.
Figure 2.
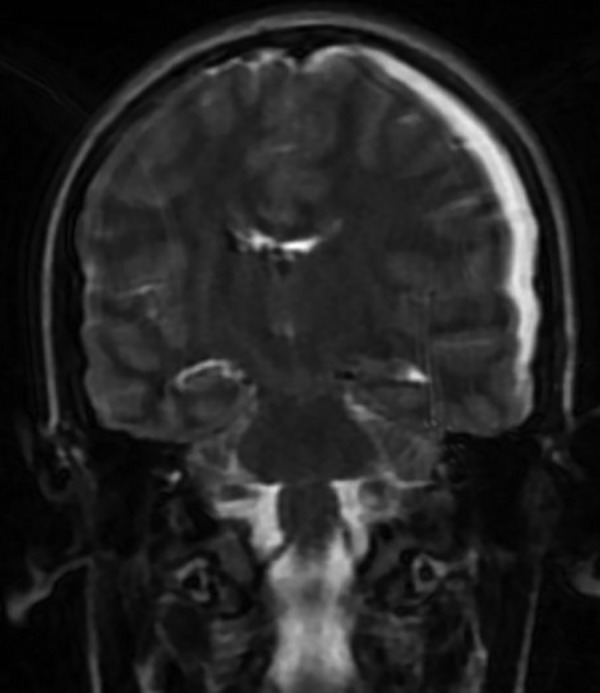
Left subdural empyema in the coronal plane T2-weighted MRI. (The imaging was suboptimal due to the patient's agitation).
Figure 3.
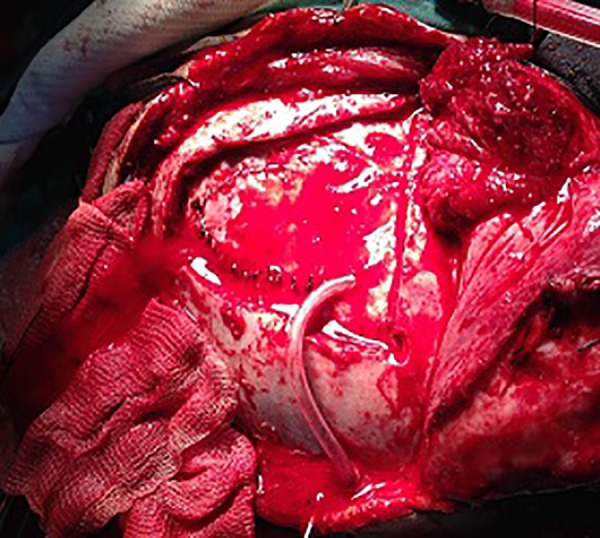
Left parieto-occipital craniotomy and inserted subdural drain.
Treatment
The patient was treated empirically with clindamycin 600 mg two times a day and ceftriaxone 2 g two times a day intravenous. This treatment was changed with ceftriaxone 2 g two times a day intravenous and metronidazole 500 mg four times a day treatment due to the development of intracranial complication at the 24th hour of initial treatment. Ceftriaxone 2 g two times a dayintravenous and metronidazole 500 mg four times a day treatment was continued for 14 days.
Outcome and follow-up
The patient was discharged on the 14th postoperative day. Follow-up assessments 4 and 8 weeks postoperatively were normal.
Discussion
Tooth infections are responsible for 10–12% of unilateral maxillary sinus infections.2 The roots of the maxillary premolar and molar teeth are situated just below the maxillary sinus floor (mean 1.97 mm).3 This close neighbourhood explain how infection of dental origin may be responsible for the development of maxillary sinusitis. Maxillary sinus infections can spread to other paranasal sinuses via the osteomeatal complex. Complications of sinusitis can be life-threatening despite antibiotic treatment. The frontal sinus is important in terms of the intracranial spread of infection. The sinus is directly adjacent to the orbital and intracranial structures and has a narrow ostium. Consequently, inflammatory processes involving the frontal sinus can rapidly spread to adjacent structures. Empyema of the frontal sinusitis can spread intracranially either directly via osteitis and bone erosion or indirectly via thrombophlebitis and local septic emboli. Adolescents are more prone to complications of the frontal sinusitis.4 CT is the gold standard for diagnosing sinusitis,5 although the diagnostic accuracy of MRI is high in patients with suspected intracranial spread of infection. In our case, paranasal sinus CT showed left pansinusitis. The causes of unilateral sinusitis include dental origin, tumours and anatomical malformations. Our patient's left upper premolar tooth was considered to be the cause of the development of the sinus infection. The bacteria most commonly causing uncomplicated paranasal sinus infections are Haemophilus influenzae and Streptococcus pneumoniae.6 The cultures in our patient grew S. viridans, confirming the dental origin of the infection.
Surgical intervention together with antibiotic therapy is often recommended for patients with complications of sinusitis.7 In addition to endoscopic intervention for the paranasal sinuses, an external approach might be preferred to reach the frontal sinus in some cases. In our patient, endoscopic sinus surgery was combined with frontal sinus trephination. To prevent frontal sinus ostium stenosis and reinfection in the early postoperative period, ostia patency was ensured by placing silicone drains.
Empirical therapy antibiotic therapy should cover pathogenic Gram-positive, Gram-negative and anaerobic bacteria. Consequently, our patient was given ceftriaxone and metronidazole, which can enter the cerebrospinal fluid and are effective against oral anaerobic flora.
Learning points.
Tooth infections are responsible for 10–12% of unilateral maxillary sinus infections.
Complications of sinusitis can be life-threatening despite antibiotic treatment.
Surgical intervention including functional endoscopic sinus surgery and a craniotomy is often recommended for patients with complications of sinusitis.
Footnotes
Contributors: SD and MŞ contributed by writing the manuscript and were involved in clinical follow-up of the patient. DBH and LS were involved in clinical follow-up of the patient.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.McIntosh DL, Mahadevan M. Frontal sinus mini-trephination for acute sinusitis complicated by intracranial infection. Int J Pediatr Otorhinolaryngol 2007;71:1573–7. 10.1016/j.ijporl.2007.06.011 [DOI] [PubMed] [Google Scholar]
- 2.Brook I. Sinusitis of odontogenic origin. Otolaryngol Head Neck Surg 2006;135:349–55. 10.1016/j.otohns.2005.10.059 [DOI] [PubMed] [Google Scholar]
- 3.Eberhardt JA, Torabinejad M, Christiansen EL. A computed tomographic study of the distances between the maxillary sinus floor and the apices of the maxillary posterior teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1992;73:345–6. 10.1016/0030-4220(92)90133-B [DOI] [PubMed] [Google Scholar]
- 4.Altman KW, Austin MB, Tom LWC et al. . Complications of frontal sinusitis in adolescents: case presentations and treatment options. Int J Pediatr Otorhinolaryngol 1997;41:9–20. 10.1016/S0165-5876(97)00047-5 [DOI] [PubMed] [Google Scholar]
- 5.Mafee MF, Tran BH, Chapa AR. Imaging of rhinosinusitis and its complications: plain film, CT, and MRI. Clin Rev Allergy Immunol 2006;30:165–86. 10.1385/CRIAI:30:3:165 [DOI] [PubMed] [Google Scholar]
- 6.Antila J, Suonpää J, Lehtonen OP. Bacteriological evaluation of 194 adult patients with acute frontal sinusitis and findings of simultaneous maxillary sinusitis. Acta Otolaryngol Suppl 1997;529:162–4. 10.3109/00016489709124111 [DOI] [PubMed] [Google Scholar]
- 7.Betz CS, Issing W, Matschke J et al. . Complications of acute frontal sinusitis: a retrospective study. Eur Arch Otorhinolaryngol 2008;265:63–72. 10.1007/s00405-007-0411-0 [DOI] [PubMed] [Google Scholar]


