Abstract
Postpartum depression (PPD) is a common complication following childbirth experienced by one in every five new mothers. Pregnancy stress enhances vulnerability to PPD and has also been shown to increase depressive-like behavior in postpartum rats. Thus, gestational stress may be an important translational risk factor that can be used to investigate the neurobiological mechanisms underlying PPD. Here we examined the effects of gestational stress on depressive-like behavior during the early/mid and late postpartum periods and evaluated whether this was accompanied by altered structural plasticity in the nucleus accumbens (NAc), a brain region that has been linked to PPD. We show that early/mid (PD8) postpartum female rats exhibited more depressive-like behavior in the forced swim test as compared to late postpartum females (PD22). However, two weeks of restraint stress during pregnancy increased depressive-like behavior regardless of postpartum timepoint. In addition, dendritic length, branching, and spine density on medium spiny neurons in the NAc shell were diminished in postpartum rats that experienced gestational stress although stress-induced reductions in spine density were evident only in early/mid postpartum females. In the NAc core, structural plasticity was not affected by gestational stress but late postpartum females exhibited lower spine density and reduced dendritic length. Overall, these data not only demonstrate structural changes in the NAc across the postpartum period, they also show that postpartum depressive-like behavior following exposure to gestational stress is associated with compromised structural plasticity in the NAc and thus may provide insight into the neural changes that could contribute to PPD.
Keywords: postpartum depression, ventral striatum, plasticity, dendritic spines, animal model
Introduction
Postpartum depression (PPD) is a common complication following childbirth experienced by approximately 15-20% of all new mothers (O'Hara & McCabe, 2013; Wisner et al., 2013). Despite the prevalence and potentially detrimental consequences of PPD for both mother and child (Grace et al., 2003; Letourneau et al., 2012), little is known about the neural changes associated with this disorder. Although there are numerous risk factors that may increase the risk of PPD in mothers (Bloch et al., 2000; O'Hara &McCabe, 2013), one of the strongest predictors for the emergence of PPD is exposure to chronic stress during pregnancy (Robertson et al., 2004; O'Hara & Wisner, 2014). Similar to humans, gestational stress increases depressive-like behavior in the postpartum rat (Smith et al., 2004; O'Mahony et al., 2006; Leuner et al., 2014). Thus, gestational stress may be a useful and important translational risk factor to investigate the neural mechanisms underlying vulnerability to depression during the postpartum period (Hillerer et al., 2012; Perani & Slattery, 2014).
Several brain regions including the hippocampus, amygdala, and prefrontal cortex have been implicated in mood disorders, including animal models of PPD (Suda et al., 2008; Brummelte & Galea, 2010; Furuta et al., 2013; Workman et al., 2013; Leuner et al., 2014). Increasing evidence suggests that depression is also accompanied by disruptions in the brain reward and motivation system comprised mainly of mesolimbic dopaminergic projections from the ventral tegmental area (VTA) to the nucleus accumbens (NAc) (Nauczyciel et al., 2013; Russo & Nestler, 2013). Likewise, neuroimaging studies in mothers with PPD have demonstrated abnormal activity of the ventral striatum which is characterized by reduced activation in response to rewarding stimuli (Moses-Kolko et al., 2011) as well as a more specific attenuation in response to hearing their own infant cry (Laurent & Ablow, 2012).
Within the NAc, emerging research has linked altered structural plasticity to depression (Russo & Nestler, 2013). In the NAc of depressed humans, there is evidence for reduced expression of genes involved in synaptic remodeling (Golden et al., 2013) while in rodent stress models, depressive-like behavior and reward related deficits have been correlated with functional and morphological changes within the NAc (Morales-Medina et al., 2009; Christoffel et al., 2011; Christoffel et al., 2012; Bessa et al., 2013). Whether structural modifications in the NAc accompany PPD has not been investigated. Thus, in the present study we employed gestational stress to induce depressive-like behavior in postpartum rats and assessed whether this was associated with altered structural plasticity in the NAc by measuring dendritic length, branching and spine density of medium spiny neurons (MSNs), the principal neuron type of the NAc. Given differences in their connectivity and functions (Zahm, 2000; Saddoris et al. 2014), we analyzed the shell and core sub-regions of the NAc separately. Moreover, we examined females during both the early/mid and late postpartum periods to evaluate the persistence of any observed changes in depressive-like behavior and/or NAc structural plasticity.
Materials and Methods
All experiments were approved by The Ohio State University Institutional Animal Care and Use Committee (Protocol No. 2011A00000005) and were performed in compliance with the rules and regulations set forth by the PHS Policy on Humane Care and Use of Laboratory Animals and the National Institutes of Health Guide for the Care and Use of Laboratory Animals.
Animals
Timed pregnant female Sprague-Dawley rats (Taconic; Albany, NY, USA) arrived at our facility on gestation day 4 (GD4). Rats were individually housed in clear Plexiglas cages, provided with food and water ad libitum, and were maintained on 12h/12h light-dark cycle (lights on at 6AM). The day of pup delivery was designated as postpartum day 0 (PD0) and on PD1 litters were culled to 8-10 pups (4-5 males, 4-5 females). To minimize the possibility that any observed differences between stressed and unstressed mothers was indirectly due to the effects of gestational stress on the pups, litters were combined at the time of culling and pups randomly assigned to a postpartum female. Rats were weighed daily throughout pregnancy and both mothers and litters were weighed daily throughout the postpartum period.
Gestational stress protocol
Pregnant females were randomly assigned to the stressed group or served as unstressed controls. Unstressed controls were handled daily for 5 min. Stressed rats were restrained twice daily for 30 min from GD7 to GD20. The two stress sessions took place between 10AM and 4PM with a 4 h interval between sessions. Restraint stress was selected because it has been used extensively to model stress-induced mood disorders and investigate their structural correlates (McEwen, 2000; Buynitsky & Mostofsky, 2009). Moreover, previous studies have shown that restraint during gestation induces depressive-like behavior during the postpartum period (Smith et al., 2004; O'Mahony et al., 2006; Hillerer et al., 2011; Leuner et al., 2014).
Forced swim test
The forced swim test (FST) was used to assess depressive-like behavior in separate groups of early/mid (stress n=8; no stress n=8) and late (stress n=9; no stress n=11) postpartum females. Briefly, Plexiglas cylinders (diameter: 30.5 cm, height: 49 cm) were filled to a depth of 30 cm with 25 ± 0.5°C water. On PD7 (early/mid) or PD21 (late), postpartum females were individually placed into the FST cylinders for 15 min, towel-dried, and returned to their home cage. 24 h later, rats were returned to the same apparatus for 5 min and the session digitally recorded. The percentage of time spent immobile [(time spent floating in the water only making movements necessary to maintain the head above water/total test time) × 100] was later measured blind by a trained observer using BEST analysis software (Education Consulting Inc.; Hobe Sound, FL, USA).
Golgi staining
24 h following the FST, postpartum females (early/mid: PD9; late: PD23) were deeply anesthetized with Euthasol, rapidly decapitated, and brains removed for Golgi impregnation using the FD Rapid Golgi Stain kit (FD Neurotechnologies; Ellicot City, MD, USA). Briefly, small blocks of tissue containing the NAc were placed in plastic scintillation vials containing 10 ml of a potassium dichromate, mercuric chloride, and potassium chromate solution (Solution A+B). Following a two week incubation period in the dark at room temperature, brains were then transferred to solution C and stored in the dark at 4°C for 2 d. Next, 200 μm coronal sections were cut on a Vibratome, mounted onto gelatin-coated slides, and dried at room temperature in the dark. Slides were then rinsed, developed in solutions D + E for 10 min, dehydrated, cleared with xylene, and coverslipped with Permount (Thermo Fisher Scientific; Fair Lawn, NJ, USA). During the staining procedure, two brains were lost from the no stress late timepoint and one was lost from the stress early timepoint.
Microscopic analyses
All analyses were done blind to experimental conditions. MSNs located approximately between 1.7mm and 1mm anterior to bregma in both the shell and core sub-regions of the NAc were analyzed (Paxinos & Watson, 1998; Fig. 4a). The anterior commissure and the ventricles were used as landmarks to identify and differentiate the shell and core subregions. Only MSNs within these regions that were fully impregnated, not obscured by neighboring neurons, and had no obviously truncated dendrites were chosen for analysis. For each animal, five randomly chosen, representative neurons in each sub-region were completely traced at 20X using NIS elements software and a Nikon 90i microscope (Nikon Instruments; Melville, NY, USA). From these traced neurons, total dendritic length and number of branch points (every point of bifurcation along dendritic branches) were measured. On these neurons, dendritic spines were then counted at 100X on five dendritic segments 20 μm in length located at least 50 μm away from the cell body. Every effort was made to ensure segments were in the same plane of focus and spines were counted only if they made a continuous connection with the dendritic shaft. Spine density was calculated by dividing the number of spines on a segment by the segment length and expressed as the numbers of dendritic spines per 10 μm. For dendritic length and branching, values for each of the five cells per animal were averaged to obtain an animal mean. For spine density, the numbers of spines on five segments of a cell were averaged for a cell mean, and the five cells from each animal were then averaged for an animal mean.
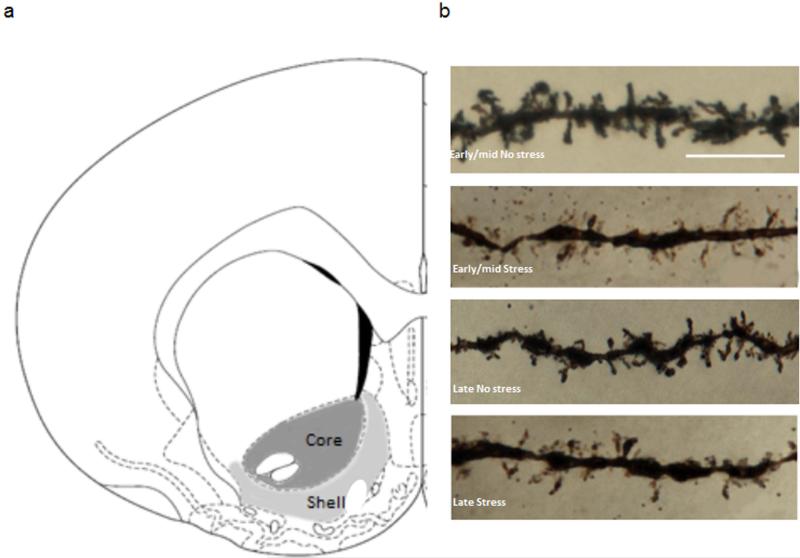
Figure 4.
NAc shell and core subregions and representative dendritic segments from MSNs within the NAc shell. Coronal plate depicting the location of the NAc shell and core subregions from which MSNs were sampled for morphological analysis (a). Representative images of dendritic segments from MSNs within the shell subregion (b). Scale bar = 10 μm.
Statistical analyses
Group data are reported as the mean ± SEM. All body weight and litter weight parameters as well as percent immobility in the FST were analyzed using two-way ANOVA with timepoint (early/mid vs. late) and stress condition (stress vs. unstressed) as independent variables. Total dendritic length, dendritic branching, and spine density data were analyzed separately for the shell and core subregions using two-way ANOVA again using timepoint (early/mid vs. late) and stress condition (stress vs. unstressed) as independent variables. Bonferroni post-hoc tests were applied when necessary. All analyses were conducted using GraphPad Prism 5.0 software (La Jolla, CA, USA) with significance set at p < 0.05.
Results
Gestational stress reduces weight gain during pregnancy
Two-way ANOVA revealed a significant main effect of stress [F(1,32) = 12.26, p < 0.005] on percent body weight gain during pregnancy (Table 1) such that pregnant females who were stressed gained less weight regardless of timepoint. However, there was no effect of gestational stress on percent postpartum weight gain (Table 1) (p's > 0.05). In addition, there were no changes in litter size (early/mid no stress: 11.88 ± 0.85 pups; early/mid stress: 11.50 ± 1.52 pups; late no stress: 12.00 ± 0.68 pups; late stress: 12.38 ± 1.79 pups), litter weight on PD1 (Table 1), or percent litter weight gain (Table 1) as a result of gestational stress (p's > 0.05). There was no main effect of timepoint and no stress × timepoint interaction for any of the above measures (p's > 0.05).
Table 1.
Effects of gestational stress on % weight gain during pregnancy and the postpartum period. Also shown is litter weight on PD1 and % litter weight gain.
| Group | % gestational weight gain | % postpartum weight gain | Litter weight on PD1 (g) | % litter weight gain |
|---|---|---|---|---|
| Early/mid No Stress | 47.82 ± 4.312 | 8.727 ± 1.528 | 85.73 ± 3.03 | 106.5 ± 14.80 |
| Early/mid Stress | 30.87 ± 3.127* | 10.41 ± 3.09 | 83.22 ± 6.593 | 85.41 ± 12.60 |
| Late No Stress | 39.01 ± 1.084 | 7.499 ± 1.11 | 86.88 ± 6.754 | 175.5 ± 4.83 |
| Late Stress | 32.19 ± 3.025* | 6.454 ± 1.183 | 88.75 ± 12.54 | 184.6 ± 14.16 |
p < 0.01, main effect of stress.
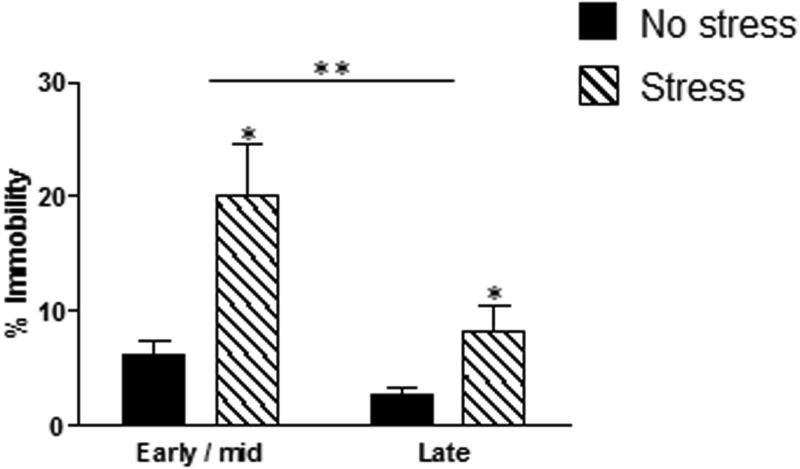
Gestational stress induces depressive-like behavior during the early/mid and late postpartum periods
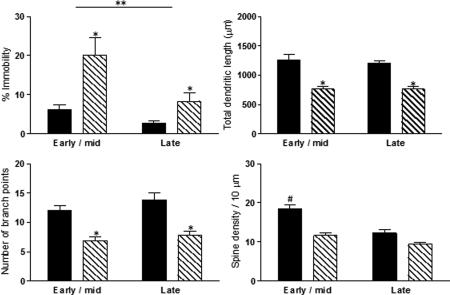
In the FST (Fig.1), there was a significant main effect of stress [F(1,32) = 16.96, p < 0.0005] such that stressed mothers spent more time immobile indicative of increased depressive-like behavior. There was also a significant main effect of timepoint [F(1,32) = 10.23, p < 0.005] with mothers during the early/mid postpartum period displaying more immobility than late postpartum females. The interaction between stress and timepoint on the percent time spent immobile in the FST was not significant [F(1,32) = 3.17, p > 0.05].
Figure 1.
Gestational stress increases depressive-like behavior during the postpartum period. Gestational stress significantly increased the percentage of time spent immobile in the FST during both the early/mid and late postpartum periods. In addition, percent immobility was overall significantly higher during the early postpartum period. Bars represent mean ± SEM, *p < 0.0005, main effect of stress; **p < 0.005, main effect of timepoint.
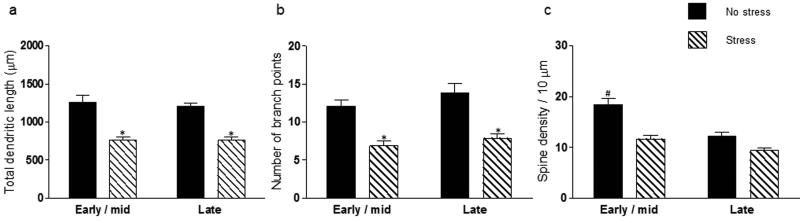
Gestational stress reduces structural plasticity within the shell, but not core, of the NAc
In the NAc shell (Fig. 2a, b), there was a main effect of stress on total dendritic length [F(1,29) = 70.55, p < 0.0001] and branch points [F(1,29) = 34.59, p < 0.0001] such that stressed mothers had shorter dendrites and fewer branch points. There was no main effect of timepoint and no stress × timepoint interaction on dendritic length or branching (p's > 0.05). For NAc shell dendritic spine density (Figs. 2c, 4b), there was a main effect of stress [F(1,29) = 29.39, p < 0.0001], a main effect of timepoint [F(1,29) = 22.14, p < 0.0001], and a significant stress × timepoint interaction [F(1,29) = 4.77, p < 0.05]. Bonferroni post-hoc analysis revealed that early/mid postpartum females who were unstressed had a greater density of dendritic spines as compared to early/mid postpartum females who were stressed (p < 0.05) as well as both groups of late postpartum females (p's < 0.05) which did not differ from one another (p's > 0.05).
Figure 2.
Gestational stress induces structural changes within the postpartum NAc shell. Gestational stress significantly reduced total dendritic length (a) and number of branch points (b) during the early/mid and late postpartum periods. Dendritic spine density was highest in early/mid postpartum females who were unstressed as compared to early/mid postpartum females who were stressed and both groups of late postpartum mothers which did not differ from one another (c). Bars represent mean ± SEM, *p < 0.0001, main effect of stress, #p < 0.05, early/mid no stress vs. all other groups.
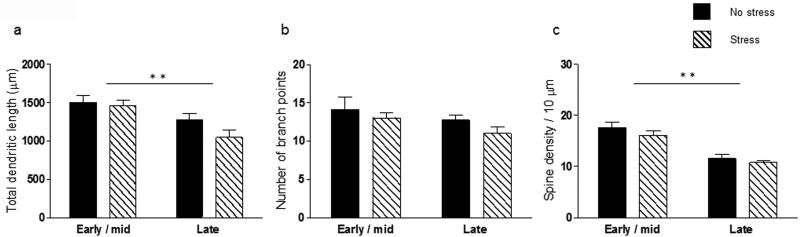
In the NAc core (Fig. 3), there was a main effect of timepoint on total dendritic length [F(1,29) = 14.10, p < 0.001] and spine density [F(1,29) = 41.67, p < 0.0001] both of which were reduced during the late postpartum period. There was no main effect of stress and no stress × timepoint interaction for dendritic length or spine density (p's > 0.05). Furthermore, there were no significant main effects of timepoint or stress and no stress x timepoint interaction for branch points in the NAc core (p's > 0.05).
Figure 3.
Gestational stress does not alter structural plasticity in the postpartum NAc core. Gestational stress did not alter dendritic length, branching or spine density in the NAc core. However, total dendritic length and spine density were significantly reduced during the late postpartum period as compared to early/mid postpartum. Bars represent mean ± SEM, **p < 0.001, main effect of timepoint.
Discussion
Here we show that increased postpartum depressive-like behavior in mothers exposed to chronic gestational stress is associated with structural changes in the NAc shell including reduced dendritic length, branching, and spine density. In contrast, structural plasticity in the NAc core was not affected by gestational stress although late postpartum females exhibited lower spine density and reduced dendritic length as compared to mothers during the early/mid postpartum period. Overall these data not only demonstrate structural changes in the NAc across the postpartum period, they also show that postpartum depressive-like behavior following exposure to gestational stress is associated with compromised structural plasticity in the NAc and thus may provide insight into the neural changes that could contribute to PPD.
In this study, gestational stress reduced percent body weight gain during pregnancy thereby confirming the efficacy of our stress procedure. This finding is consistent with evidence in humans linking high levels of stress during pregnancy to insufficient gestational weight gain (Orr et al., 1996; Brawarsky et al., 2005) as well as other rodent studies showing that gestational stress (Baker et al., 2008; Hillerer et al., 2011; Leuner et al., 2014) or glucocorticoid administration during pregnancy (Brummelte & Galea, 2010) reduces weight gain. However, in contrast to other reports (Hillerer et al., 2011; Leuner et al., 2014), we did not detect differences in postpartum weight gain as result of gestational stress nor did we find that gestational stress impacted litter weight gain. Although these discrepancies may be related to differences in stress protocols, it appears that a variety of gestational stress paradigms increase immobility in the FST during the postpartum period including the restraint procedure used here (Smith et al., 2004; O'Mahony et al., 2006; Hillerer et al., 2011; Leuner et al., 2014). It is important to note that concerns about the validity of restraint have been raised (Carini et al., 2013) and thus additional stress models of PPD are needed to gain a complete understanding of PPD. In this regard, unpublished work from our lab suggests that chronic mild stress, a depression model with high validity (Hill et al., 2012), yields the same behavioral and physiological symptoms in postpartum rats noted here including increased immobility in the FST and reduced gestational weight gain. It will also be critical to investigate whether gestational stress impacts other core symptoms of depressive behavior such as anhedonia. Such a consequence is likely given that behavioral despair in the FST and anhedonia in the sucrose preference test are often strongly correlated measures of mood (Strekalova et al., 2004; Bessa et al., 2009).
It is notable that overall, early/mid postpartum females exhibited more depressive-like behavior than late postpartum females. This effect is likely driven by the high levels of immobility in the early/mid mothers exposed to gestational stress which could reflect locomotor acclimation engendered by the repeated restraint procedure. Although we cannot eliminate this possibility, our data and others (O'Mahony et al., 2006) show that gestational stress also increases immobility during the late postpartum period when acclimation to restraint is less likely to be an issue. It is also possible that increased immobility in early postpartum females that experienced gestational stress is a lingering response to withdrawal from ovarian hormones. Indeed, findings from several studies in humans and rodents suggest that the rapid and robust decline in estradiol and progesterone levels following parturition induce postpartum mood alterations (Bloch et al., 2000; Galea et al., 2001; Stoffel & Craft, 2004; Green et al., 2009; Navarre et al., 2010; Schiller et al., 2013). Thus, hormonal withdrawal may precipitate depressive-like behavior in early/mid postpartum females and exposure to gestational stress may exacerbate this effect.
Our data reveal for the first time that gestational stress also leads to robust (approximately 35% change) and persistent morphological modifications on MSNs in the shell of the NAc. Specifically, at both the early/mid and late timepoints, mothers exposed to gestational stress had shorter dendrites and fewer branch points. However, two issues must be addressed in future studies in order to better understand the cause of these changes. First, because we did not examine late pregnant and/or newly parturient females, we are unable to determine if the effects we observed were a direct consequence of gestational stress or if they arose a result of changes in mother-offspring interactions which are known to occur following gestational stress (Smith et al., 2004; Champagne et al., 2006; Baker et al., 2008; Leuner et al., 2014). Second, we did not include a group of virgin females which were reported in a previous study to also have reduced dendritic complexity in the ventral striatum as compared to postpartum females (Shams et al., 2012). Thus, although our data suggest that gestational stress diminishes structural plasticity in the NAc shell, the possibility remains that gestational stress prevented the enhancement in structural plasticity that normally occurs postpartum.
In the NAc shell, spine density was also reduced in response to gestational stress but only at the early/mid postpartum timepoint. Also at this early/mid timepoint, unstressed mothers had the highest density of dendritic spines. Increased spine density early/mid postpartum may be necessary to enhance pup salience and motivation to engage in maternal care both of which are known to be greatest during the early/mid postpartum period and which are mediated by the NAc shell (Li & Fleming, 2003; Wansaw et al., 2008). Thus, the differential effect of gestational stress in early/mid versus late postpartum females may be related to differences in baseline spine density in unstressed mothers across the postpartum period. Like the other aspects of NAc shell morphology that were affected by gestational stress, it will be necessary to determine if gestational stress leads to a loss of preexisting spines or if it suppresses a potential postpartum growth of new dendritic spines and whether these effects are related to a stress-induced change in maternal behavior.
Gestational stress did not affect structural plasticity in the NAc core which is consistent with the greater sensitivity of the NAc shell to stress (Kalivas & Duffy, 1995; Wang et al., 2012). However, as compared to the early/mid postpartum period, total dendritic length and spine density were reduced in the NAc core during the late postpartum period. Like other brain regions (e.g. hippocampus) which show temporal changes in dendritic architecture across the postpartum period, the structural differences in the NAc core in early/mid versus late postpartum females may be mediated by pup exposure and postpartum hormonal fluctuations (Leuner et al., 2010; Workman et al., 2012).
Previous work in male rodents has demonstrated changes in NAc dendritic morphology and spine density in response to stress or corticosterone administration. Similar to our results with postpartum females, chronic administration of corticosterone to male rats was shown to reduce total dendritic length and spine density in the NAc shell (Morales-Medina et al., 2009). These data are consistent with human postmortem studies reporting reduced expression of genes involved in synaptic remodeling in the NAc of depressed subjects (Golden et al., 2013). However, our findings differ from other work showing increased spine density (Christoffel et al., 2011; Christoffel et al., 2012) and total dendritic length (Bessa et al., 2013) in the NAc of male rats and mice following chronic stress exposure. Although different stressors were used, it may nonetheless seem paradoxical that males and postpartum females exhibit opposite morphological responses to chronic stress and yet depressive-like behavior is increased in both (Christoffel et al., 2012). However, other aspects of synaptic function are not captured by our morphological measures. For example, reduced spine density in postpartum females exposed to chronic gestational stress may be compensated for by a change in synaptic efficacy of existing synapses ultimately leading to a similar behavior phenotype to that seen in males. It is also important to consider that the effects of stress on structural plasticity within the NAc of virgin females have not been examined although there are reported sex differences in NAc synaptic connectivity and structural complexity (Wissman et al., 2011; Wissman et al., 2012). Thus, it is possible that males and females exhibit different responses to stress and in females that response may be further modified by gonadal hormones and maternal experience. Because depression is more prevalent in women than men (Kessler, 2003; Noble, 2005), particularly during periods of dramatic hormonal fluctuations (Steiner et al., 2003; Soares & Zitek, 2008), sex differences in the effects of stress on neuronal morphology in mood regulating areas such as the NAc could account for sex differences in depression prevalence and the interaction between hormones and changes in vulnerability across women's lifespan. Minimally, these data highlight the need to better understand the impact of stress on NAc structural plasticity in males vs. females and in females across reproductive conditions.
Altered morphology of MSNs in the NAc shell as a consequence of gestational stress could involve several structural plasticity mediators that have also been implicated in depression. For example, brain derived neurotrophic trophic factor has been linked to PPD (Gazal et al., 2012) and is known to regulate stress-induced dendritic and synaptic plasticity in the NAc (Christoffel et al., 2011; Russo & Nestler, 2013). Another likely candidate is dopamine given that the NAc receives extensive dopaminergic input from the VTA (Baik, 2013). Since accumbal neuronal morphology is positively regulated by dopamine (Meredith et al., 1995), reduced spine density and neuronal complexity in the NAc shell of stressed mothers may indicate less dopamine input. Consistent with this possibility, dopaminergic system dysregulation has been observed in women with PPD (Moses-Kolko et al., 2012) and although not measured here, other animal models of PPD have reported reduced dopamine levels in the NAc during mother-pup interactions (Lavi-Avnon et al., 2008). It is important to note that while the vast majority of MSNs in the NAc are GABAergic, they have different projection pathways and are dichotomous in their expression of either D1 or D2 dopamine receptors (Smith et al., 2013). These two MSN subtypes also have different intracellular responses to dopamine (Albin et al., 1989; Surmeier et al., 2007) that might contribute to stress-induced morphological changes in the NAc thus emphasizing the need for future studies to investigate whether the effects of gestational stress are cell type specific. In addition to DA, MSNs in the NAc are also a target of convergent glutamatergic input from the mPFC, hippocampus, and basolateral amygdala (Russo & Nestler, 2013). As afferent excitatory input regulates dendritic structure (Fiala et al., 2002; Wong & Ghosh, 2002; Redmond, 2008), stress-induced alterations in excitatory innervation and signaling in the NAc from one or more of these regions (Campioni et al., 2009; Marsden, 2011; Besheer et al., 2014) may also contribute to postpartum structural modifications and would be consistent with recent studies showing that perturbations of the glutamatergic system are at least partially involved in the synaptic abnormalities found in mood disorders (Jun et al., 2014).
Similar to the NAc shell, two weeks of gestational stress is sufficient to attenuate spine density on pyramidal neurons in the mPFC during the postpartum period (Leuner et al., 2014). As noted above, the mPFC sends glutamatergic projections to the NAc and like the NAc receives dopaminergic projections from the VTA thereby forming the mesocortical dopamine system (Tzschentke, 2000; Russo & Nestler, 2013). Both the mPFC and NAc represent critical components of the neural circuitry regulating emotion (Puglisi-Allegra & Ventura, 2012; Volman et al., 2013) and altered structural plasticity in these regions has been linked to depressive behavior in rodents and humans (Pittenger & Duman, 2008; Russo & Neslter, 2013). These regions also play a major role in regulating rewarding, motivated behaviors (Tzschentke & Schmidt, 2000) including maternal care (Li & Fleming, 2003; Afonso et al., 2007) which is impaired in mothers with PPD (Lovejoy et al., 2000; Wan & Green, 2009) as well as postpartum rodents exhibiting depressive-like behavior (Smith et al., 2004; Lavi-Avnon et al., 2005; Leuner et al., 2014). Thus, compromised structural plasticity in the mesocortical dopamine system following gestational stress could not only underlie postpartum depressive-like behavior but may also interfere with reward and motivational processes including those that at are necessary for maternal responsiveness.
The negative consequences of gestational stress on the cognitive, emotional and social development of the offspring are well documented (Wehmer et al., 1970; Laplante et al., 2004; Van den hove et al., 2006; Weinstock, 2008). As such, treatment of depressed mothers is critical and commonly achieved with administration of selective serotonin reuptake inhibitor (SSRI) antidepressant medications (Logsdon et al., 2011). Other than one report showing increased neurogenesis in the hippocampus of gestationally stressed mothers following chronic postpartum fluoxetine administration (Pawluski et al., 2012), the ability of SSRI treatment to reverse stress-induced structural and behavioral changes in postpartum females hasn't been assessed. Since the NAc receives serotonergic input from the dorsal raphe (Van Bockstaele et al., 1993), such a consequence is likely and may at least partially underlie the amelioration of depressed mood in mothers with PPD.
Compared to the offspring, the impact of gestational stress on the mother has received much less attention. Here we show that increased depressive-like behavior in postpartum females exposed to chronic gestational stress is accompanied by reduced structural complexity of MSNs in the NAc shell thus demonstrating that gestational stress not only significantly impacts structural plasticity in the NAc of the offspring (Muhammad et al., 2012), but also the mother. Given evidence linking the ventral striatum to PPD (Moses-Kolko et al., 2011; Laurent & Ablow, 2012), our results may provide insights into the cellular underpinnings of PPD for which little is currently known.
Acknowledgements
We thank Peter J. Fredericks, Christopher Albin-Brooks, and Orin Hemminger for technical assistance. This work was funded by a grant from the National Institute of Health (R0084148) to B.L.
Abbreviations
- FST
forced swim test
- mPFC
medial prefrontal cortex
- MSN
medium spiny neuron
- NAc
nucleus accumbens
- PPD
postpartum depression
- VTA
ventral tegmental area
References
- Afonso VM, Sison M, Lovic V, Fleming AS. Medial prefrontal cortex lesions in the female rat affect sexual and maternal behavior and their sequential organization. Behav. Neurosci. 2007;121:515–526. doi: 10.1037/0735-7044.121.3.515. [DOI] [PubMed] [Google Scholar]
- Albin RL, Young AB, Penney JB. The functional anatomy of basal ganglia disorders. Trends Neurosci. 1989;12:366–375. doi: 10.1016/0166-2236(89)90074-x. [DOI] [PubMed] [Google Scholar]
- Baik JH. Dopamine signaling in reward related behaviors. Front. Neural Circuits. 2013;7:152. doi: 10.3389/fncir.2013.00152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker S, Chebli M, Rees S, LeMarec N, Godbout R, Bielajew C. Effects of gestational stress: 1. evaluation of maternal and juvenile offspring behavior. Brain Res. 2008;12:98–110. doi: 10.1016/j.brainres.2008.03.035. [DOI] [PubMed] [Google Scholar]
- Besheer J, Fisher KR, Jaramillo AA, Frisbee S, Cannady R. Stress hormone exposure reduces mGluR5 expression in the nucleus accumbens: functional implications for interceptive sensitivity to alcohol. Neuropsychopharmacology. 2014 doi: 10.1038/npp.2014.85. doi: 10.1038/npp.2014.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bessa JM, Mesquita RA, Oliveira M, Pego JM, Cerqueira JJ, Palha JA, Almeida OF, Sousa N. A trans-dimensional approach to the behavioral aspects of depression. Front. Behav. Neurosci. 2009;3:1. doi: 10.3389/neuro.08.001.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bessa JM, Morais M, Marques F, Pinto L, Palha JA, Almeida OF, Sousa N. Stress-induced anhedonia is associated with hypertrophy of medium spiny neurons of the nucleus accumbens. Transl. Psychiatry. 2013;3:e266. doi: 10.1038/tp.2013.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bloch M, Schmidt PJ, Danaceau M, Murphy J, Neiman L, Rubinow D. Effects of gonadal steroids in women with a history of postpartum depression. Am. J. Psychiatry. 2000;157:924–930. doi: 10.1176/appi.ajp.157.6.924. [DOI] [PubMed] [Google Scholar]
- Brawarsky P, Stotland NE, Jackson RA, Fuentes-Afflick E, Escobar GJ, Rubashkin N, Haas JS. Pre-pregnancy and pregnancy-related factors and the risk of excessive or inadequate gestational weight gain. Int. J. Gynaecol. Obstet. 2005;91:125–131. doi: 10.1016/j.ijgo.2005.08.008. [DOI] [PubMed] [Google Scholar]
- Brummelte S, Galea LAM. Chronic corticosterone during pregnancy and postpartum affects maternal care, cell proliferation and depressive-like behavior in the dam. Horm. Behav. 2010;58:769–779. doi: 10.1016/j.yhbeh.2010.07.012. [DOI] [PubMed] [Google Scholar]
- Buynitsky T, Mostofsky DI. Restraint stress in biobehavioral research: recent developments. Neurosci. Biobehav. Rev. 2009;33:1089–1098. doi: 10.1016/j.neubiorev.2009.05.004. [DOI] [PubMed] [Google Scholar]
- Campioni MR, Xu M, McGehee DS. Stress-induced changes in nucleus accumbens glutamate synaptic plasticity. J. Neurophysiol. 2009;101:3192–3198. doi: 10.1152/jn.91111.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carini LM, Murgatroyd CA, Nephew BC. Using chronic social stress to model postpartum depression in lactating rodents. J. Vis. Exp. 2013;76:e50324. doi: 10.3791/50324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Champagne FA, Meaney MJ. Stress during gestation alters postpartum maternal care and the development of the offspring in a rodent model. Biol. Psychiatry. 2006;59:1227–1235. doi: 10.1016/j.biopsych.2005.10.016. [DOI] [PubMed] [Google Scholar]
- Christoffel DJ, Golden SA, Dumitriu D, Robinson AJ, Janssen WG, Ahn HF, Krishnan V, Reyes CM, Han MH, Ables JL, Eisch AJ, Dietz DM, Ferguson D, Neve RL, Greengard P, Kim Y, Morrison JH, Russo SJ. IkB kinase regulates social defeat-induced synaptic and behavioral plasticity. J. Neurosci. 2011;31:314–321. doi: 10.1523/JNEUROSCI.4763-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christoffel DJ, Golden SA, Heshmati M, Graham A, Birnbaum S, Neve RL, Hodes GE, Russo SJ. Effects of inhibitor of κB kinase activity in the nucleus accumbens on emotional behavior. Neuropsychopharmacology. 2012;37:2615–2623. doi: 10.1038/npp.2012.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiala JC, Spacek J, Harris KM. Dendritic spine pathology: cause or consequence of neurological disorders? Brain Res. Brain Res. Rev. 2002;39:29–54. doi: 10.1016/s0165-0173(02)00158-3. [DOI] [PubMed] [Google Scholar]
- Furuta M, Numakawa T, Chiba S, Ninomiya M, Kajiyama Y, Adachi N, Akema T, Kunugi H. Estrogen, predominantly via estrogen receptor α, attenuates postpartum-induced anxiety- and depression-like behaviors in female rats. Endocrinology. 2013;154:3807–3816. doi: 10.1210/en.2012-2136. [DOI] [PubMed] [Google Scholar]
- Galea LA, Wide JD, Barr AM. Estradiol alleviates depressive-like symptoms in a novel animal model of post-partum depression. Behav. Brain Res. 2001;122:1–9. doi: 10.1016/s0166-4328(01)00170-x. [DOI] [PubMed] [Google Scholar]
- Gazal M, Motta LS, Wiener CD, Fernandes JC, Quevedo LA, Jansen K, Pinheiro KA, Giovenardi M, Souza DO, Silva RA, Pinheiro RT, Portela LV, Oses JP. Brain-derived neurotropic factor in post-partum depressive mothers. Neurochem. Res. 2012;37:583–587. doi: 10.1007/s11064-011-0647-3. [DOI] [PubMed] [Google Scholar]
- Golden SA, Christoffel DJ, Heshmati M, Hodes GE, Magida J, Davis K, Cahill ME, Dias C, Ribeiro E, Ables JL, Kennedy PJ, Robinson AJ, Gonzalez-Maeso J, Neve RL, Turecki G, Ghose S, Tamminga CA, Russo SJ. Epigenetic regulation of RAC1 induces synaptic remodeling in stress disorders and depression. Nat. Med. 2013;19:337–344. doi: 10.1038/nm.3090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grace SL, Evindar A, Stewart DE. The effect of postpartum depression on child cognitive development and behavior: a review and critical analysis of the literature. Arch. Womens Ment. Health. 2003;6:263–274. doi: 10.1007/s00737-003-0024-6. [DOI] [PubMed] [Google Scholar]
- Green AD, Barr AM, Galea LA. Role of estradiol withdrawal in ‘anhedonic’ sucrose consumption: a model of postpartum depression. Physiol. Behav. 2009;97:259–265. doi: 10.1016/j.physbeh.2009.02.020. [DOI] [PubMed] [Google Scholar]
- Hill MN, Hellemans KG, Verma P, Gorzalka BB, Weinberg L. Neurobiology of chronic mild stress: parallels to major depression. Neurosci. Biobehav. Rev. 2012;36:2085–2117. doi: 10.1016/j.neubiorev.2012.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hillerer KM, Reber SO, Neumann ID, Slattery DA. Exposure to chronic pregnancy stress reverses peripartum-associated adaptations: implications for postpartum anxiety and mood disorders. Endocrinology. 2011;152:3930–3940. doi: 10.1210/en.2011-1091. [DOI] [PubMed] [Google Scholar]
- Hillerer KM, Neumann ID, Slattery DA. From stress to postpartum mood and anxiety disorders: how chronic peripartum stress can impair maternal adaptations. Neuroendocrinology. 2012;95:22–38. doi: 10.1159/000330445. [DOI] [PubMed] [Google Scholar]
- Jun C, Choi Y, Lim SM, Bae S, Hong YS, Kim JE, Lyoo IK. Disturbance of the glutamatergic system in mood disorders. Exp. Neurobiol. 2014;23:28–35. doi: 10.5607/en.2014.23.1.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalivas PW, Duffy P. Selective activation of dopamine transmission in the shell of the nucleus accumbens by stress. Brain Res. 1995;675:325–328. doi: 10.1016/0006-8993(95)00013-g. [DOI] [PubMed] [Google Scholar]
- Kessler RC. Epidemiology of women and depression. J. Affect. Disord. 2003;74:5–13. doi: 10.1016/s0165-0327(02)00426-3. [DOI] [PubMed] [Google Scholar]
- Laplante DP, Barr RG, Brune A, Galbaud Du Fort G, Meaney ML, Saucier JF, Zelazo PR, King S. Stress during pregnancy affects general intellectual and language functioning in human toddlers. Pediatr. Res. 2004;56:400–410. doi: 10.1203/01.PDR.0000136281.34035.44. [DOI] [PubMed] [Google Scholar]
- Laurent HK, Ablow JC. A cry in the dark: depressed mothers show reduced neural activation to their own infants cry. Soc. Cog. Affect. Neurosci. 2012;2:125–134. doi: 10.1093/scan/nsq091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavi-Avnon Y, Shayit M, Yadid G, Overstreet HD, Weller A. Immobility in the swim test and observations of maternal behavior in lactating flinders sensitive line rats. Behav. Brain Res. 2005;161:155–163. doi: 10.1016/j.bbr.2005.02.002. [DOI] [PubMed] [Google Scholar]
- Lavi-Avnon Y, Weller A, Finberg JP, Gispan-Herman I, Kinor N, Stern Y, Schroeder M, Gelber V, Bergman SY, Overstreet DH, Yadid G. The reward system and maternal behavior in an animal model of depression: a microdialysis study. Psychopharmacology. 2008;196:281–291. doi: 10.1007/s00213-007-0961-2. [DOI] [PubMed] [Google Scholar]
- Letourneau NL, Dennis CL, Benzies K, Duffett-Leger L, Stewart M, Tryphonopoulos PD, Este D, Watson W. Postpartum depression is a family affair: Addressing the impact on mothers, fathers, and children. Issues Ment. Health Nurs. 2012;33:445–457. doi: 10.3109/01612840.2012.673054. [DOI] [PubMed] [Google Scholar]
- Leuner B, Glasper ER, Gould E. Parenting and plasticity. Trends Neurosci. 2010;33:465–473. doi: 10.1016/j.tins.2010.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leuner B, Fredericks PJ, Nealer C, Albin-Brooks C. Chronic gestational stress leads to depressive-like behavior and compromises medial prefrontal cortex structure and function during the postpartum period. PLoS One. 2014;9:e89912. doi: 10.1371/journal.pone.0089912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li M, Fleming AS. The nucleus accumbens shell is critical for normal expression of pup retrieval in postpartum rats. Behav. Brain Res. 2003;145:99–111. doi: 10.1016/s0166-4328(03)00135-9. [DOI] [PubMed] [Google Scholar]
- Logsdon MC, Wisner K, Sit D, Luther JF, Wisniewski SR. Depression treatment and maternal functioning. Depress. Anxiety. 2011;28:1020–1026. doi: 10.1002/da.20892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovejoy MC, Graczyk PA, O'Hare E, Neuman G. Maternal depression and parenting behavior: a meta-analytic review. Clin. Psychol. Rev. 2000;20:561–592. doi: 10.1016/s0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- Marsden WN. Stressor-induced NMDAR dysfunction as a unifying hypothesis for the aetiology, pathogenesis and comorbidity of clinical depression. Med. Hypotheses. 2011;77:508–528. doi: 10.1016/j.mehy.2011.06.021. [DOI] [PubMed] [Google Scholar]
- McEwen BS. Effects of adverse experience for brain structure and function. Biol. Psychiatry. 2000;48:721–731. doi: 10.1016/s0006-3223(00)00964-1. [DOI] [PubMed] [Google Scholar]
- Meredith GE, Ypma P, Zahm DS. Effects of dopamine depletion on the morphology of medium spiny neurons in the shell and core of the rat nucleus accumbens. J. Neurosci. 1995;15:3808–3820. doi: 10.1523/JNEUROSCI.15-05-03808.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morales-Medina JC, Sanchez F, Flores G, Dumont Y, Quirion R. Morphological reorganization after repeated corticosterone administration in the hippocampus, nucleus accumbens and amygdala in the rat. J. Chem. Neuroanat. 2009;38:266–272. doi: 10.1016/j.jchemneu.2009.05.009. [DOI] [PubMed] [Google Scholar]
- Moses-Kolko EL, Fraser D, Wisner KL, James JA, Saul T, Fiez JA, Phillips ML. Rapid habituation of ventral striatal response to reward receipt in postpartum depression. Biol. Psychiatry. 2011;71:395–399. doi: 10.1016/j.biopsych.2011.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moses-Kolko EL, Price JC, Wisner KL, Hanusa BH, Meltzer CC, Berga SL, Grace AA, di Scalea TL, Kaye WH, Becker C, Drevets WC. Postpartum and depression status are associated with lower [11C]raclopride BP(ND) in reproductive-age women. Neuropsychopharmacology. 2012;37:1422–1432. doi: 10.1038/npp.2011.328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muhammad A, Carroll C, Kolb B. Stress during development alters dendritic morphology in the nucleus accumbens and prefrontal cortex. Neuroscience. 2012;216:103–109. doi: 10.1016/j.neuroscience.2012.04.041. [DOI] [PubMed] [Google Scholar]
- Nauczyciel C, Robic S, Dondaine T, Verin M, Robert G, Drapier D, Naudet F, Millet B. The nucleus accumbens: a target for deep brain stimulation in resistant major depressive disorder. J. Molec. Psychiatry. 2013;1:17. doi: 10.1186/2049-9256-1-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Navarre MB, Laggart JD, Craft RM. Anhedonia in postpartum rats. Physiol. Behav. 2010;99:59–66. doi: 10.1016/j.physbeh.2009.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noble RE. Depression in women. Metabolism. 2005;54:49–52. doi: 10.1016/j.metabol.2005.01.014. [DOI] [PubMed] [Google Scholar]
- O'Hara MW, McCabe JE. Postpartum depression: current status and future directions. Annu. Rev. Clin. Psychol. 2013;9:379–407. doi: 10.1146/annurev-clinpsy-050212-185612. [DOI] [PubMed] [Google Scholar]
- O'Hara MW, Wisner KL. Perinatal mental illness: definition, description and aetiology. Best Pract. Res. Clin. Obstet. Gynaecol. 2014;28:3–12. doi: 10.1016/j.bpobgyn.2013.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Mahony SM, Myint AM, van den Hove D, Desbonnet L, Steinbusch H, Leonard BE. Gestational stress leads to depressive-like behavioural and immunological changes in the rat. Neuroimmunomodulation. 2006;13:82–88. doi: 10.1159/000096090. [DOI] [PubMed] [Google Scholar]
- Orr ST, James SA, Miller CA, Barakat B, Daikoku N, Pupkin M, Engstrom K, Huggins G. Psychosocial stressors and low birthweight in an urban population. Am. J. Prev. Med. 1996;12:459–466. [PubMed] [Google Scholar]
- Pawluski JL, Charlier TD, Fillet M, Houbart V, Crispin HT, Steinbusch HW, Van den Hove DL. Chronic fluoxetine treatment and maternal adversity differentially alter neurobehavioral outcomes in the rat dam. Behav. Brain Res. 2012;228:159–168. doi: 10.1016/j.bbr.2011.11.043. [DOI] [PubMed] [Google Scholar]
- Paxinos G, Watson C. The rat brain in stereotaxic coordinates. Academic Press; San-Diego, CA.: 1998. [Google Scholar]
- Perani CV, Slattery DA. Using animal models to study postpartum psychiatric disorders. Br. J. Pharmacol. 2014 doi: 10.1111/bph.12640. doi: 10.1111/bph.12640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pittenger C, Duman RS. Stress, depression, and neuroplasticity: a convergence of mechanisms. Neuropsychopharmacology. 2008;33:88–109. doi: 10.1038/sj.npp.1301574. [DOI] [PubMed] [Google Scholar]
- Puglisi-Allegra S, Ventura R. Prefrontal/accumbal catecholamine system processes emotionally driven attribution of motivational salience. Rev. Neurosci. 2012;23:509–526. doi: 10.1515/revneuro-2012-0076. [DOI] [PubMed] [Google Scholar]
- Redmond L. Translating neuronal activity into dendrite elaboration: signaling to the nucleus. Neurosignals. 2008;16:194–208. doi: 10.1159/000111563. [DOI] [PubMed] [Google Scholar]
- Robertson E, Grace S, Wallington T, Stewart DE. Antenatal risk factors for postpartum depression: a synthesis of recent literature. Gen. Hosp. Psychiatry. 2004;26:289–295. doi: 10.1016/j.genhosppsych.2004.02.006. [DOI] [PubMed] [Google Scholar]
- Russo SJ, Nestler EJ. The brain reward circuitry in mood disorders. Nat. Rev. Neurosci. 2013;14:609–625. doi: 10.1038/nrn3381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saddoris MP, Sugam JA, Cacciapaglia F, Carelli RM. Rapid dopamine dynamics in the accumbens core and shell: learning and action. Front. Biosci. 2014;5:273–288. doi: 10.2741/e615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schiller EC, O'Hara MW, Rubinow DR, Johnson AK. Estradiol modulates anhedonia and behavioral despair in rats and negative affect in subgroup of women with high risk for postpartum depression. Physiol. Behav. 2013;119:137–144. doi: 10.1016/j.physbeh.2013.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shams S, Pawluski JL, Chatterjee-Chakraborty M, Oatley H, Mastroianni A, Fleming AS. Dendritic morphology in the striatum and hypothalamus differentially exhibits experience-dependent changes in response to maternal care and early social isolation. Behav. Brain Res. 2012;233:79–89. doi: 10.1016/j.bbr.2012.04.048. [DOI] [PubMed] [Google Scholar]
- Smith JW, Seckl JR, Evans AT, Costall B, Smythe JW. Gestational stress induces post-partum depression-like behavior and alters maternal care in rats. Psychoneuroendocrinology. 2004;29:227–244. doi: 10.1016/s0306-4530(03)00025-8. [DOI] [PubMed] [Google Scholar]
- Smith RJ, Lobo MK, Spencer S, Kalivas PW. Cocaine-induced adaptations in D1 and D2 accumbens projection neurons (a dichotomy not necessarily synonymous with direct and indirect pathways). Curr. Opin. Neurobiol. 2013;23:546–552. doi: 10.1016/j.conb.2013.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soares CN, Zitek B. Reproductive hormone sensitivity and risk for depression across the female life cycle: A continuum of vulnerability? J. Psychiatry Neurosci. 2008;33:331–343. [PMC free article] [PubMed] [Google Scholar]
- Steiner M, Dunn E, Born L. Hormones and mood: from menarche to menopause and beyond. J. Affect. Disord. 2003;74:67–83. doi: 10.1016/s0165-0327(02)00432-9. [DOI] [PubMed] [Google Scholar]
- Strekalova T, Spanagel R, Bartsch D, Henn FA, Gass P. Stress-induced anhedonia in mice is associated with deficits in forced swim test and exploration. Neuropsychopharmacology. 2004;29:2007–2017. doi: 10.1038/sj.npp.1300532. [DOI] [PubMed] [Google Scholar]
- Stoffel EC, Craft RM. Ovarian hormone withdrawal-induced “depression” in female rats. Physiol. Behav. 2004;83:505–513. doi: 10.1016/j.physbeh.2004.08.033. [DOI] [PubMed] [Google Scholar]
- Suda S, Segi-Nishida E, Newton SS, Duman RS. A postpartum model in rat: behavioral and gene expression changes induced by ovarian steroid deprivation. Biol. Psychiatry. 2008;64:311–319. doi: 10.1016/j.biopsych.2008.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surmeier DJ, Ding J, Day M, Wang Z, Shen W. D1 and D2 dopamine-receptor modulation of striatal glutamatergic signaling in striatal medium spiny neurons. Trends Neurosci. 2007;30:228–235. doi: 10.1016/j.tins.2007.03.008. [DOI] [PubMed] [Google Scholar]
- Tzschentke TM. The medial prefrontal cortex as a part of the brain reward system. Amino Acids. 2000;19:211–219. doi: 10.1007/s007260070051. [DOI] [PubMed] [Google Scholar]
- Tzschentke TM, Schmidt WJ. Functional relationship among medial prefrontal cortex, nucleus accumbens, and ventral tegmental area in locomotion and reward. Crit. Rev. Neurobiol. 2000;14:131–142. [PubMed] [Google Scholar]
- Van Bockstaele EJ, Biswas A, Pickel VM. Topography of serotonin neurons in the dorsal raphe nucleus that send axon collaterals to the rat prefrontal cortex and nucleus accumbens. Brain Res. 1993;624:188–198. doi: 10.1016/0006-8993(93)90077-z. [DOI] [PubMed] [Google Scholar]
- Van den Hove DL, Steinbusch HW, Scheepens A, Van de Berg WD, Kooiman LA, Boosten BJ, Prickaerts J, Blanco CE. Prenatal stress and neonatal rat brain development. Neuroscience. 2006;137:145–155. doi: 10.1016/j.neuroscience.2005.08.060. [DOI] [PubMed] [Google Scholar]
- Volman SF, Lammel S, Margolis EB, Kim Y, Richard JM, Roitman MF, Lobo MK. New insights into the specificity and plasticity of reward and aversion encoding in the mesolimbic system. J. Neurosci. 2013;33:17569–17576. doi: 10.1523/JNEUROSCI.3250-13.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wan MW, Green J. The impact of maternal psychopathology on child-mother attachment. Arch. Womens Ment. Health. 2009;12:123–134. doi: 10.1007/s00737-009-0066-5. [DOI] [PubMed] [Google Scholar]
- Wang YC, Ho UC, Ko MC, Liao CC, Lee LJ. Differential neuronal changes in medial prefrontal cortex, basolateral amygdala and nucleus accumbens after postweaning social isolation. Brain Struct. Funct. 2012;217:337–351. doi: 10.1007/s00429-011-0355-4. [DOI] [PubMed] [Google Scholar]
- Wansaw MP, Pereira M, Morrell JI. Characterization of maternal motivation in lactating rat: contrasts between early and late postpartum responses. Horm. Behav. 2008;54:294–301. doi: 10.1016/j.yhbeh.2008.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wehmer F, Porter RH, Scales B. Pre-mating and pregnancy stress in rats affects behavior of grandpups. Nature. 1970;227:622. doi: 10.1038/227622a0. [DOI] [PubMed] [Google Scholar]
- Weinstock M. The long-term behavioural consequences of prenatal stress. Neurosci. Biobehav. Rev. 2008;32:1073–1086. doi: 10.1016/j.neubiorev.2008.03.002. [DOI] [PubMed] [Google Scholar]
- Wisner KL, Sit DK, McShea MC, Rizzo DM, Zoretich RA, Hughes CL, Eng HF, Luther JF, Wisniewski SR, Costantino ML, Confer AL, Moses-Kolko EL, Famy CS, Hanusa BH. Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. JAMA Psychiatry. 2013;70:490–498. doi: 10.1001/jamapsychiatry.2013.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wissman AM, McCollum AF, Huang GZ, Nikrodhanond AA, Woolley CS. Sex differences and effects of cocaine on excitatory synapses in the nucleus accumbens. Neuropharmacology. 2011;61:217–227. doi: 10.1016/j.neuropharm.2011.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wissman AM, May RM, Woolley CS. Ultrastructural analysis of sex differences in nucleus accumbens synaptic connectivity. Brain Struct. Funct. 2012;217:181–190. doi: 10.1007/s00429-011-0353-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong RO, Ghosh A. Activity-dependent regulation of dendritic growth and patterning. Nat. Rev. Neurosci. 2002;3:803–812. doi: 10.1038/nrn941. [DOI] [PubMed] [Google Scholar]
- Workman JL, Barha CK, Galea LA. Endocrine substrates of cognitive and affective changes during pregnancy and postpartum. Behav. Neurosci. 2012;126:54–72. doi: 10.1037/a0025538. [DOI] [PubMed] [Google Scholar]
- Workman JL, Brummelte S, Galea LA. Postpartum corticosterone administration reduces dendritic complexity and increases the density of mushroom spines of hippocampal CA3 arbours in dams. J. Neuroendocrinol. 2013;25:119–130. doi: 10.1111/j.1365-2826.2012.02380.x. [DOI] [PubMed] [Google Scholar]
- Zahm DS. An integrative neuroanatomical perspective on some subcortical substrates of adaptive responding with emphasis on the nucleus accumbens. Neurosci. Biobehav. Rev. 2000;24:85–105. doi: 10.1016/s0149-7634(99)00065-2. [DOI] [PubMed] [Google Scholar]