Abstract
Dementia is a clinical diagnosis requiring new functional dependence on the basis of progressive cognitive decline. It is estimated that 1.3% of the entire UK population, or 7.1% of those aged 65 or over, have dementia. Applying these to 2013 population estimates gives an estimated number of 19,765 people living with dementia in Northern Ireland. The clinical syndrome of dementia can be due to a variety of underlying pathophysiological processes. The most common of these is Alzheimer's disease (50-75%) followed by vascular dementia (20%), dementia with Lewy bodies (5%) and frontotemporal lobar dementia (5%). The clinical symptoms and pathophysiological processes of these diseases overlap significantly. Biomarkers to aid diagnosis and prognosis are emerging. Acetylcholinesterase inhibitors and memantine are the only medications currently licensed for the treatment of dementia. The nature of symptoms mean people with dementia are more dependent and vulnerable, both socially and in terms of physical and mental health, presenting evolving challenges to society and to our healthcare systems.
INTRODUCTION
Dementia is a clinical diagnosis requiring new functional dependence on the basis of progressive cognitive decline and representing, as its Latin origins suggest, a departure from previous mental functioning.
The incidence of dementia rises with age making it an increasingly common phenomenon within our aging population. The nature of symptoms mean people with dementia are more dependent and vulnerable, both socially and in terms of physical and mental health, presenting evolving challenges to society and to our healthcare systems. Despite the seemingly simple premise, the clinical diagnosis of dementia can be difficult with de novo functional impairment often obscured by physical frailty, comorbid psychiatric symptoms such as depression and a subtle but steady assuming of household responsibilities by spouses and family. Clinical and pathological criteria for the main dementia-causing diseases overlap significantly. The emergence of symptoms decades into the pathophysiological process hamper targeted disease therapy. A great number of research initiatives are underway to identify potential biomarkers of disease processes earlier. The association of both overt cognitive decline and underlying pathophysiological processes with normal aging complicate the process of identifying disease processes early within the spectrum of normal aging.
Once the diagnosis is established, prognostic measures are required, and are still lacking, as disease trajectories between individuals can vary greatly. Globally, governments are recognising these challenges. Investment and research infrastructure are beginning to reflect the scale of the need. Drugs conferring symptomatic benefit are available and memory service structures exist to diagnose dementias and guide management. The personal impact of dementia on patients and families is also being increasingly recognised, with discussion in the media surrounding famous sufferers and dramatisations in literature and film. Herein we attempt to describe the current landscape of dementia.
EPIDEMIOLOGY AND SOCIO-ECONOMIC IMPLICATIONS
Dementia is often arbitrarily considered early (< 65yrs) or late-onset (> 65yrs), with the vast majority (>97%) of cases being of late-onset1. Table 1 shows the most recent age-related prevalence estimates for dementia in the UK, which equate to 1.3% of the entire UK population or 7.1% of those aged 65 or over2. Applying these to 2013 population estimates gives an estimated number of 19,765 people living with dementia in Northern Ireland2. This compares to the 12,811 people registered with the Quality and Outcomes Framework for Northern Ireland (NI) with a diagnosis of dementia in 2013-2014 (http://www.dhsspsni.gov.uk/index/statistics/qof/qof-achievement/qof-lcg-13-14.htm).
Table 1.
Gender specific age-related prevalence (%) of dementia in the UK (estimates from Dementia UK 2014)
| Age in years | Female | Male | Total |
|---|---|---|---|
| 60 – 64 | 0.9 | 0.9 | 0.9 |
| 65 – 69 | 1.8 | 1.5 | 1.7 |
| 70 – 74 | 3.0 | 3.1 | 3.0 |
| 75 – 79 | 6.6 | 5.3 | 6.0 |
| 80 – 84 | 11.7 | 10.3 | 11.1 |
| 85 – 89 | 20.2 | 15.1 | 18.3 |
| 90 – 94 | 33.0 | 22.6 | 29.9 |
| 95+ | 44.2 | 28.8 | 41.1 |
The age-related incidence of dementia in the UK is falling, presumably as a result of better public health measures3, meaning the increasing absolute numbers of people with dementia are based on the shifting population demographic, the aging population. Global estimates of a doubling in the dementia population every 20 years giving an estimated 115 million people with dementia by 2050 were revised further upwards in 2013, to take account of the likely further increases in lower and middle income countries4.
Prognosis at the time of dementia diagnosis varies, with evidence that age at diagnosis, gender, comorbidities and disease severity can all affect life expectancy5. Whilst methodological variations limit the usefulness of the data available, median life expectancy from the time of diagnosis has been shown to range from 3.2 to 6.6 years, and from 3.3 to 11.7 years from dementia onset 5. Local research has suggested a median survival of 5.9 years from diagnosis (unpublished data).
Transition into residential care as a result of the functional impairments of dementia is a prospect that worries many patients and a reality that many families face. It was estimated last year that 69% of all those living in residential care within the UK suffer from dementia2.
It is perhaps no surprise then that dementia is expensive. The updated estimated cost to the UK economy of £26.3 billion per year published last year2 took account of the role played by unpaid carers (£11.6 billion), social care costs were estimated at £10.3 billion and healthcare costs at £4.3 billion in comparison.
CLINICAL DIAGNOSIS
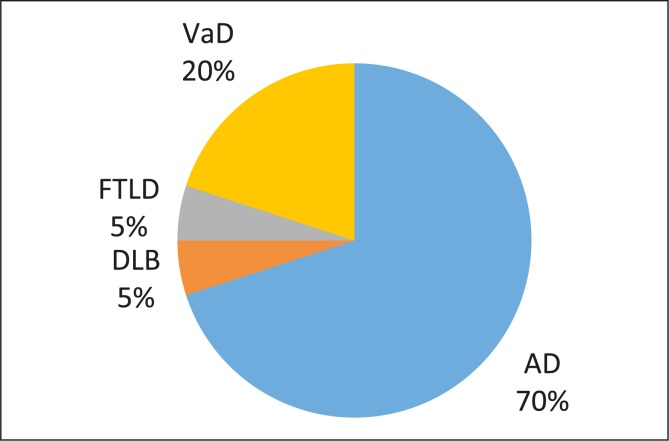
The clinical syndrome of dementia, characterised by new functional dependence on the basis of progressive cognitive decline, can be due to a variety of underlying pathophysiological processes. The most common of these is Alzheimer's disease (AD; 50-75%) followed by vascular dementia (VaD; 20%), dementia with Lewy bodies (DLB; 5%) and frontotemporal lobar dementia (FTLD; 5%) (Figure 1). The significant clinical and pathological overlap between these processes mean their relative frequencies are estimates at best1, 6. Less common causes (3%) include Huntingdon's disease, Creutzfeldt-Jakob disease, HIV/AIDS and multiple sclerosis. We will first consider the clinical and then the pathological properties of these diseases.
Fig 1.
Pie chart showing estimated frequencies of dementiacausing disease processes
Cognitive impairments central to the diagnosis of dementia can be categorised into five main domains: memory; executive function; language; visuospatial abilities; personality and behaviour. As dementia, of any cause, progresses, cognitive impairments will broaden, involving more domains, and deepen, causing increased functional impairment. It can thus be difficult to distinguish dementias of different aetiologies in the later stages. In the early stages however the pattern of prominent symptoms can help identify the most likely underlying disease process. Clinical criteria exist for all the main dementia sub-types, the main features of which are outlined in Table 2 7–11. All criteria require a diagnosis of dementia and include the caveats that there should not be a symptom pattern more in keeping with another of the dementias and that cognitive impairments should not be better explained by a psychiatric illness. Neuropsychiatric symptoms should be sought. Depression can be a cause or effect of cognitive impairments and often features such as hallucinations and delusions will not be volunteered unless specific enquiries are made.
Table 2.
Clinical diagnostic criteria for dementias
| Disease | ADD | DLB | Behavioural variant FTLD | Primary progressive aphasia (FTLD) | VaD |
|---|---|---|---|---|---|
| Authors (year) | McKhann et al (2011) | McKeith et al (2005) | Rascovsky et al (2011) | Gorno-Tempini et al (2011) | Gorelick et al (2011) |
| Required symptoms | (Typical ADD) Memory deficits + deficits in at least one other cognitive domain | (Central features) Attentional deficits Executive dysfuction Visuospatial deficits (Core features, 2/3) Fluctuating cognition Visual hallucinations Parkinsonism (Suggestive features) REM sleep behavior disorder Neuroleptic sensitivity Positive DAT scan |
Behavioural disinhibition Apathy or inertia Loss of sympathy or empathy Perseverative, stereotyped or compulsive/ritualistic behavior Hyperorality and dietary changes Executive dysfunction with relative sparing of episodic memory and visuospatial skills (3/6 required) |
Language deficit most prominent symptom and accounts for functional decline No prominent memory, visuospatial or behavioural problems |
Clear temporal relationship between vascular event and onset of cognitive deficits Cognitive deficits independent of motor/ sensory sequelae of vascular event |
AD, the most common cause of dementia, typically presents with short-term memory deficits, manifesting for example as repetitive questioning. Impairment in at least one other cognitive domain is required for a diagnosis of probable dementia due to AD (ADD). Atypical presentations of ADD include behavioural or language deficits suggesting frontal variants or prominent early visuospatial problems suggesting posterior cortical atrophy. The most relevant feature of a presentation of VaD is the temporal association of cognitive deficits with stroke and evidence of cerebrovascular disease on examination and imaging. The Lewy body diseases comprise DLB and Parkinson's disease (PD). Patients with DLB may go on to develop Parkinsonism. As a rule of thumb, if the emergence of dementia and physical PD symptoms are within one year the diagnosis is PD dementia (PDD), if cognitive symptoms predate physical symptoms and signs by more than one year the diagnosis is considered to be DLB. Early language or behavioural symptoms raise the prospect of FTLD. In the younger age groups, ie less than 65, the incidence of FTLD and ADD are almost equal, in contrast to the vastly lower incidence of FTLD in older age groups. The early symptoms of behavioural variant FTLD often raise the possibility of primary functional psychiatric diagnosis, complicating diagnosis.
It is relatively common to be presented with clinical scenarios that do not wholly and exclusively fulfil a single diagnostic criteria. Reflecting the concurrent accumulation of pathophysiological processes within the brain, symptoms can represent overlapping disease processes and mixed pictures can be said to occur, this is most commonly the case with ADD and VaD.
Many people present with objective cognitive symptoms that fall short of the requirements for a diagnosis of dementia. Criteria exist then for the diagnosis of mild cognitive impairment (MCI)12, 13. Creation of this diagnostic category has facilitated focused follow up demonstrating that 5-10% per year of those with MCI will progress to fulfill the diagnostic requirements of a dementia14. Such symptoms can also be due to psychiatric illness, drugs known to be deleterious to cognition or may be transient and regress spontaneously. As the use of biomarkers, outlined below, evolves, identification of those more likely to be in the prodromal stages of a dementia is improving, with some arguing that patients should be identified at the MCI stage as either prodromal dementia or not15. For now the diagnostic bracket of MCI, whilst disputed, remains.
Other diagnostic criteria exist. In addition to the criteria set out by McKhann et al in 20117 an International Working Group has proposed diagnostic criteria for ADD intended for use primarily in research15. The older Hachinski16 and NINDS-AIREN17 scales are still used to define VaD. The 5th edition of the Diagnostic and Statistical Manual of Mental Disorders published in 2013 by the American Psychiatric Association18 has introduced the terms major and mild neurocognitive disorders, which equate to dementia and MCI. Their criteria for the various subtypes equate broadly with the pre-existing clinical criteria.
Diagnosis and differentiation of dementias requires careful history taking and examination. Both patient and collateral histories are needed to establish a new functional dependence and to explore the progressive cognitive impairments as well as neuropsychiatric symptoms. Physical examination is required to examine for focal neurological or extrapyramidal signs. Cognition will be assessed informally during the course of the consultation but formal testing is required, and facilitates longitudinal monitoring. A suggested framework for assessment of patients presenting with cognitive complaints is outlined in Table 3.
Table 3.
Suggested foci of assessment of patients with cognitive symptoms
| History | History from patient and informant Change from baseline Functional decline Past medical history Drug history Current home circumstances Alcohol and smoking Driving Family history |
Some specific examples: repetitive questioning; inability to navigate journeys and less familiar environments eg shopping centres, own children's home; difficulty recognising previously familiar people; difficulty using new equipment eg new oven; word-finding difficulties; tendency to participate less in group conversations; less attention to personal hygiene/appearance; new short-temperedness with family Progressing to: agitation in the evening; not recognising home as own Specific safety concerns: problems in the kitchen; problems with cigarette disposal; wandering; handling of money |
| Physical examination | Extrapyramidal signs Focal neurological deficit(s) Ability to follow instructions Pulse Chest auscultation |
|
| Cognitive examination and associated scales (52,53) | Formal cognitive testing (eg MMSE/ACEIII) Geriatric Depression Scale (or alternative) Activities of Daily Living Scale Neuropsychiatric Inventory |
Neuropsychiatric Inventory includes delusions, hallucinations, agitation/aggression, apathy, disinhibition, sleep and appetite |
| Investigation | Bloods CT brain (or MRI if appropriate) ECG |
Probably the most widely recognised formal cognitive test is the Mini Mental State Examination (MMSE), first proposed in 197519. Whilst assertions of copyright have impacted on its use in recent years the MMSE has become well and widely established, and provides a common language for those fluent in its use. The Montreal Cognitive Assessment, originally developed as a test for MCI, and also marked out of 30, has expanded into the space created by MMSE apprehension (www.mocatest.org). The Addenbrooke's Cognitive Examination-III (ACE-III) provides a more thorough assessment and marks are calculated for each domain, then tallied to give a total, out of 100 (http://www.neura.edu.au/frontier/research/test-downloads/). A growing variety of scales exist, none of which is perfect. Inter and intra-rater reliability can limit use and all scales are reliant on premorbid educational abilities. The important thing is to become familiar with a scale, ensure its consistent use within a service, and use it to monitor progression.
PATHOPHYSIOLOGY/PATHOLOGICAL FEATURES
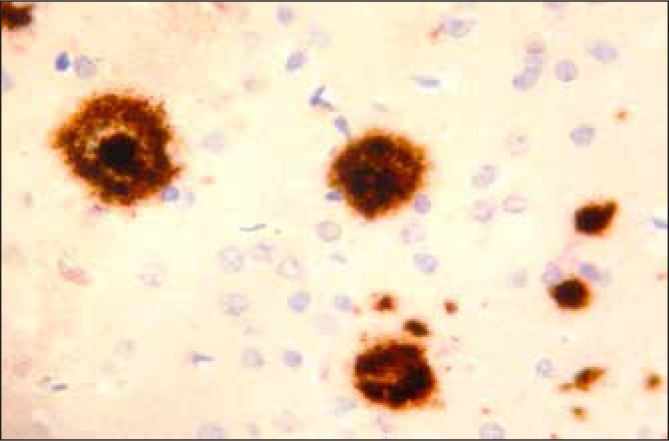
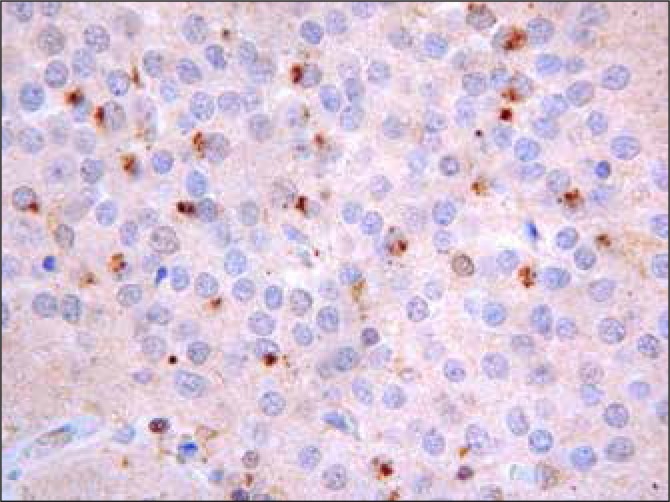
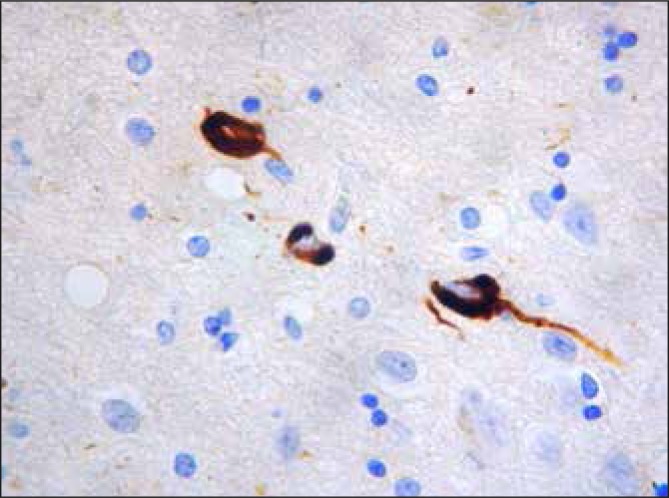
The disease processes underlying dementia are yet to be fully understood. With the (probable) exception of VaD, all involve a pathological accumulation of a native protein: in the case of AD it is the extracellular plaques of amyloid and the intracellular tangles of hyperphosphorylated tau; in DLB it is alpha-synuclein in the form of Lewy bodes; in FTLD several culprits have been identified including TDP-43 and the hallmark proteins of AD and DLB in a frontotemporal distribution. Examples of these lesions can be seen in Figures 2–5. It is important to remember that evidence of these processes is also found post-mortem in people who did not exhibit cognitive impairments prior to death, and that these patterns are not mutually exclusive, existing concurrently as they often do20.
Fig 2.
An immunohistochemical section taken through the cortex in a case of ADD. An antibody to Beta A4 amyloid is applied to the tissue and detects this antigen which in turn stains the antigen brown. This shows a dense deposition of amyloid throughout the cortex as dense core (DC) and diffuse (D) plaques.
Fig 5.
A section from the hippocampal dentate fascia showing dot like deposition of ubiquitin. This is characteristic of Frontotemporal Lobar Dementia with Ubiquitinised inclusions (now called TDP).
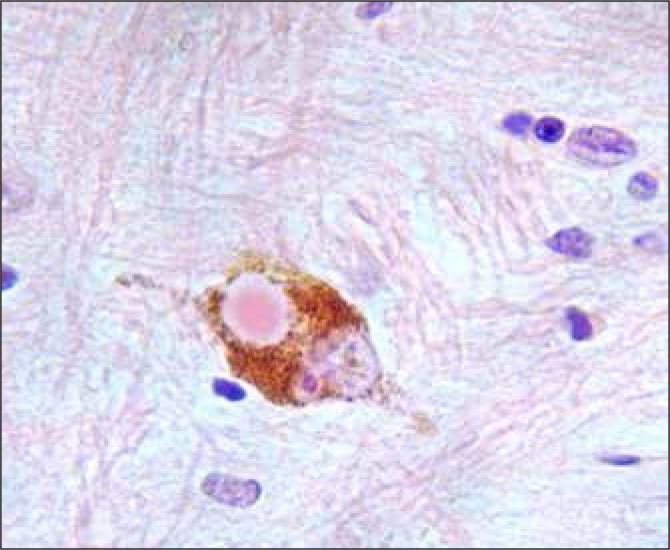
Fig 3.
Neuronal tangles stained with an antibody to Tau (T)
Fig 4.
A pigmented neuron from the substantia nigra. A single Lewy Body is present. This patient also had diffuse cortical Lewy bodies characteristic of Pure Lewy Body Dementia
These pathological accumulations are associated with synapse and neuronal loss and atrophy which also demonstrate patterns in terms of distribution. Hippocampal atrophy within the medial temporal lobe for instance is associated with AD, in keeping with the early amnestic symptoms21
Genetic studies have contributed greatly to our knowledge of these disease processes. The observation that people with Down's syndrome (trisomy 21) almost invariably develop AD, led to the discovery of the first of three autosomal dominant genes associated with early-onset ADD22. Study of these genes, responsible for amyloid cleavage, have been integral to the understanding of pathological amyloid production. In contrast to the aberrant production of amyloid proteins implicated in early onset ADD, late-onset ADD (LOAD) is thought to be more to do with faulty clearance of amyloid from the brain. Apolipoprotein E23 and, more recently, TREM-224, 25 alleles have been identified as risk factors for LOAD. Their pathophysiological roles remain unclear: they are implicated in amyloid processing and neuroinflammation amongst other pathways. Neither are sufficient or requisite for LOAD and are therefore not tested for in routine clinical practice. Genome wide association studies in recent years have consistently identified several genes with significant but modest associations with LOAD26 and examination of their relevant pathways, including immune response and inflammation, cell migration and lipid transport, have enhanced the evolving understanding of the ADD disease process.
These methods are being applied across the dementia spectrum and similar pathways are implicated in DLB, FTLD and VaD27, 28. FTLD in particular has myriad of increasingly recognized heritable components.
Animal models, often based on these predisposing genetic mutations, continue to provide basic science research opportunities. Improving chemistry techniques, such as proteomics and metabolomics are also being used to study the disease using human-derived samples such as blood and cerebrospinal fluids.
BIOMARKERS
The search for biomarkers further informs our understanding of these disease processes and offers the opportunity to identify them prior to symptom emergence. A biomarker has been defined as a ‘characteristic that is objectively measured and evaluated as an indicator of normal biological processes, pathogenic processes, or pharmacologic responses to a therapeutic intervention29. Research into ADD is currently the main focus and biomarkers are generally considered as representing the underlying AD process (evidence of amyloid and tau accumulation) or neurodegeneration (markers of synapse/neuronal loss or atrophy)7, 15.
Low amyloid beta and high tau in cerebrospinal fluid (CSF) and high levels of intracerebral amyloid as measured by positron emission tomography (PET) scanning predict the subsequent development of ADD30. The downstream markers of neurodegeneration - hippocampal atrophy on MRI and decreased uptake of a radiolabelled glucose tracer (18-fluorodeoxyglucose, FDG) as measured using PET scanning (FDG-PET) have also been shown to increase diagnostic accuracy when used to supplement clinical measures30.
The occurrence of these pathophysiological processes in cognitively normal people, especially with increasing age, complicates the interpretation of these biomarkers. Several studies of cognitively normal patients are ongoing and a recently published cross sectional study of 985 participants showed that over the age of 85 more people had biomarker changes in keeping with ADD than did not31. There are significant variations in neuroimaging techniques across centres and also in the sampling, handling and analysis of CSF21, 32, 33. Worldwide research collaborations, such as the Alzheimer's Disease Neuroimaging Initiative (ADNI), are in place to try and accelerate our understanding of the pathophysiological processes underlying dementia, and hence the interpretation of biomarker findings, in both cognitively normal and impaired participants. Global standardisation initiatives are also ongoing with regard to MRI and PET imaging and CSF amyloid and tau. Biomarkers are beginning to be used in clinical practice34 but the likelihood, and benefit, of more widespread adoption is dependent on these issues being resolved.
INVESTIGATION
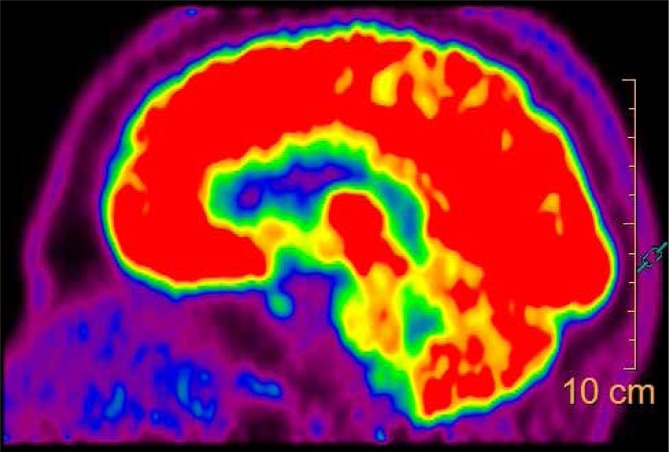
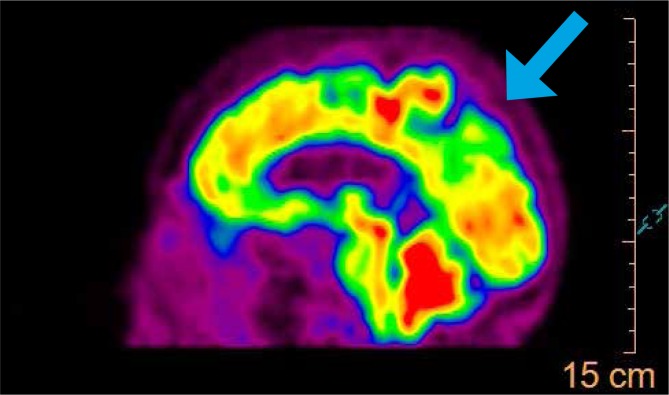
Initial investigation of patients presenting with cognitive impairment centres on the exclusion of reversible causes of cognitive impairment. The National Institute of Clinical Excellence (NICE) recommends blood tests (full blood picture, urea and electrolytes, calcium, glucose, liver function tests, thyroid function tests and vitamin B12 and folate) and structural brain imaging (preferably MRI but CT will suffice)35. In addition to ruling out tumours, subdural haematomas, stroke and normal pressure hydrocephalus, CT, and to a greater extent MRI, can also provide information regarding chronic ischaemia, infarcts and focal atrophy. Functional imaging, such as single-photon emission computed tomography (SPECT) and FDG-PET are recommended to help differentiate between the dementia sub-types where appropriate. Figure 6&7 show normal compared to reduced uptake in keeping with ADD on FDG-PET. Dopamine transporter (DAT) scanning has shown high sensitivity and specificity for DLB and is the investigation of choice when trying to differentiate between DLB and other dementias36.
Fig 6.
Figures 6 and 7 show normal and reduced uptake on FDG-PET scanning respectively. The decreased uptake in the temporoparietal and precuneus (arrow) regions, typical of ADD, can be seen.
Fig 7.
Figures 6 and 7 show normal and reduced uptake on FDG-PET scanning respectively. The decreased uptake in the temporoparietal and precuneus (arrow) regions, typical of ADD, can be seen.
RISK FACTORS
In tandem with the laboratory science methods outlined above, observational studies have informed our understanding of the risk factors for dementia, as well as the natural history and prognosis of the diseases. Age is the main risk factor for dementia. Established modifiable risk factors for dementia include: depression, diabetes, (midlife) hypertension, (midlife) obesity, smoking, alcohol abuse, high cholesterol, coronary heart disease, renal dysfunction, low unsaturated fat intake and inflammation37. It has been argued that the decrease in age-related dementia incidence seen in the UK is due to better public health measures and thus amelioration of these factors3. There is in addition increased focus on recognised protective factors such as: cognitive activity, physical activity, healthy dietary pattern and low/moderate alcohol intake37.
MANAGEMENT – NON-PHARMACOLOGICAL
Management will be guided by the nature and severity of the symptoms and any safety concerns. Vascular risk factors should be addressed. Patients and relatives should be offered information and explanations. The Public Health Agency (www.publichealth.hscni.net) have developed a booklet ‘Communicating effectively with a person living with dementia’ available via their website. The Alzheimer's Society have local offices and provide information and support (www.alzheimers.org.uk). Patients and carers should be referred to a social worker if a carer's assessment is felt appropriate and to facilitate access to services such as Day Centres and social services care provision. As a result of the NI Dementia Strategy a navigation service for all those diagnosed with dementia is being established in all Trusts; this will ensure patients and carers have a consistent contact point throughout their journey. Moderate physical exercise should be encouraged where possible. No formal cognitive training services are currently being offered consistently though supportive evidence is emerging and may translate into service provision. Where appropriate patients can be referred to community mental health teams. Transition into residential care is influenced by social circumstances, dementia severity and the behavioural and psychological symptoms of dementia (BPSD) eg aggression. Non-pharmacological measures are recommended as first line therapy for BPSD but there is as yet no consensus regarding the most effective measures. All patients should be advised to inform the Driver & Vehicle Agency and their insurer of a diagnosis of dementia. If there are concerns regarding a patient's ability to drive they should be advised to stop driving. Where patients lack capacity to manage their own affairs and assets a referral to the Office of Care and Protection (www.courtsni.govuk/en-GB/Services/OCP/) may be warranted. A draft Mental Capacity Bill (NI) (working title) is due to be introduced to the NI Assembly this year having already been consulted upon. It is likely this will have significant impact on how healthcare decisions are made for people who lack capacity.
People with dementia are frequently admitted acutely to hospital, most commonly following a fall, and it is estimated that up to one quarter of in patients in UK hospitals, at any one time, have dementia38. This is important as caring for patients with dementia requires modification of communication, diagnostic and, at times, management approaches. Patients may have difficulties articulating symptoms. Constipation and acute urinary retention for example should be actively sought out. Disorientation and agitation may develop and both environmental (eg clear signage and clocks) and attitudinal (eg repeated reassurance, clear explanations, good lighting, involvement of families) approaches can ameliorate this. Dysphagia is a common occurrence as dementia progresses and patients may require dietary modification and assistance at meal times. Dyspraxia can hinder personal care, with considerate assistance required. Patients with dementia are more likely to develop delirium which can further complicate care needs39. Rehabilitation attempts can be hampered by cognitive impairments but dementia should not be a contraindication to rehabilitation as evidence for benefit exists. Discharge planning is required, often with inclusion of families. More than one third of patients with dementia admitted to hospital from their own homes will be discharged to an institutional setting38. A scheme has been introduced to increase the understanding, and identification, of dementia within hospital settings (http://butterflyscheme.org.uk).
MANAGEMENT – PHARMACOLOGICAL
Offending medications, in particular those with anticholinergic properties should be reconsidered and stopped where possible. It is important to note that even over the counter medications can affect cognition40. An association with benzodiazepines has been suggested by observational work and these too should be reconsidered41.
Acetylcholinesterase inhibitors and memantine, an NMDA receptor antagonist, (Table 4) are the only medications currently licensed for the treatment of dementia. All three acetylcholinesterase inhibitors (AChEi) have a license and are recommended by NICE for the treatment of ADD with rivastigmine additionally approved for the treatment of PDD42, 43. Memantine is approved for the treatment of moderate ADD where AChEi are contraindicated or not tolerated and as an adjunct to AChEi therapy in severe disease43. Evidence exists to suggest a moderate improvement in cognitive function with these drugs44, 45. These drugs are not licensed for use in VaD. In clinical practice it can be difficult to distinguish whether there is an ADD component and these medications are often offered as a therapeutic trial. There is no evidence to support the use of AChEi or memantine in FTLD;46, 47 AChEi usually make symptoms of FTLD worse as the underlying pathological process is different to that of ADD.
Table 4.
Acetylcholinesterase inhibitors and memantine
| Generic name | Brand name | Dosing schedule |
|---|---|---|
| Donepezil | Aricept | 5mg od, titrated up to 10mg od after 4 weeks if tolerated |
| Galantamine | Reminyl | XL preparation available for od administration, 8mg daily initially, titrating up by 8mg after 4 weeks if tolerated to maximum of 24mg od |
| Rivastigmine Rivastigmine patch | Exelon | 1.5mg bd titrating up by 1.5mg bd at intervals of at least 2 weeks; usual range 3-6mg bd 4.6mg/24 hours titrating up to 9.5mg/24 hours after 4 weeks if tolerated |
| Memantine | Ebixa | 5mg od, titrated up by 5mg per week to maximum dose 20mg od |
Mild, moderate and severe disease severity categories are often used but are arbitrary by nature. As a rule of thumb NICE considers corresponding cut-offs by MMSE of 21-26, 10-20 and less than 1035 but in practice this is only a single facet of the assessment outlined in Table 3.
AChEi therapy exerts its benefit by raising pathologically low levels of the neurotransmitter acetylcholine. Potential adverse events include risk of bradycardia and syncope, potential worsening of obstructive airways disease and gastrointestinal disturbance. Assessment should therefore include an ECG and chest auscultation, with severe sinus bradycardia or evidence of a significant cardiac conduction defect or significant audible wheeze all contraindications to AChEi therapy. The possibility of reduction in the dose of beta-blocker or ratelimiting calcium channel blocker could be considered prior to initiation of an AChEi. An anti-emetic, usually domperidone, can be prescribed on an as required basis for the first few weeks to alleviate nausea. The British National Formulary recommends nocte administration of donepezil but it is acceptable to take it in the morning. The decision to continue or terminate drug therapy, in the setting of inevitable cognitive decline, can be difficult. The DOMINO-AD48 study showed that continuation of donepezil therapy, even in severe disease, was associated with significant cognitive benefit.
Souvenaid is a food for special medical purposes with evidence for improved memory function in early ADD49. It is not available on prescription and requires a recommendation from a healthcare professional.
BPSD is an umbrella term for a variety of symptoms including apathy, agitation, disinhibition and sleep disturbance. These can be particularly distressing for carers and often precipitate admission to institutional care. Atypical antipsychotics are sometimes employed to combat BPSD but are associated with significant side effects including an increase in mortality and so should be carefully considered50. Only risperidone has a license for the treatment of BPSD and short-term treatment (<6 weeks) is recommended42. Depression is a common symptom (see the upcoming review in this Journal regarding diagnosis and treatment of depression).
Many pharmacological avenues are being explored in an effort to find new effective, safe drugs for dementia. Efforts are hampered by the as yet incomplete understanding of the pathophysiological processes being targeted. Drugs targeting amyloid production and amyloid plaque clearance have failed on safety and efficacy grounds. Anti-tau agents are currently being studied. Apart from Souvenaid the much vaunted dietary supplements have yet to be supported by consistent evidence. Safety concerns are being addressed, and emerging pathophysiological insights exploited, by attempts to reposition existing drugs within the dementia field, for example metformin51.
CONCLUSION
Significant advances have been made in our understanding of dementia in recent decades. Dementia presents laboratory, clinical, societal and economic challenges. Diagnosis remains clinical, supplemented by improving biomarkers. Dementia causing diseases overlap in their pathophysiology and phenotypes. The only licensed drugs to date provide symptomatic benefit. Disease-modifying drug development is reliant on early identification of disease processes prior to symptom emergence, where it is currently felt best therapeutic window exists. Both biomarker and drug development depend on better understanding of underlying pathophysiological processes. The wide-reaching benefits of improved public health measures have yielded a decrease in age-related incidence but the ongoing demographic shift means efforts on all fronts must be redoubled if we are to diagnose, treat, understand and care for those of us who develop dementia. The importance of dementia as a global priority is recognised in the declarations of the G8 Dementia Summit in 2013, committing the G8 nations to the improvement in the quality of life for people with dementia and their carers and identification of disease-modifying therapies by way of a co-ordinated and funded international research framework.
ACKNOWLEDGEMENTS
Dr William Murphy, Consultant Radiologist, provided the FDGPETCT images. Drs Shane Gallagher and Brenda Campbell, General Practitioners, reviewed the article and provided advice. Patients and relatives have donated tissue over the years to further the study and understanding of dementia.
CONFLICTS OF INTEREST
ELC has received a contribution towards conference fees from Lundbeck
BMcG has received honoraria and assistance with travel from Nutricia
BH has nothing to declare
APP has received honoraria and assistance with travel from Pfizer/Eisai, Shire, J&J, Novartis, Lundbeck and Nutricia
REFERENCES
- 1.Knapp M, Prince M. Dementia UK: full report. London: Alzheimer's Society; 2007. [Google Scholar]
- 2.Prince M, Knapp M, Guerchet M, McCrone P, Prina M, Comas-Herrera A. Dementia UK: Update. London: Alzheimer's Society; 2014. [Google Scholar]
- 3.Matthews FE, Arthur A, Barnes LE, Bond J, Jagger C, Robinson L, et al. A two-decade comparison of prevalence of dementia in individuals aged 65 years and older from three geographical areas of England: results of the Cognitive Function and Ageing Study I and II. Lancet. 2013;382(9902):1405–12. doi: 10.1016/S0140-6736(13)61570-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Prince M, Guerchet M, Prina M. Policy Brief for Heads of Government: The Global Impact of Dementia 2013 - 2050; London: Alzheimer's Disease International; 2013. [Google Scholar]
- 5.Todd S, Barr S, Roberts M, Passmore AP. Survival in dementia and predictors of mortality: a review. Int J Geriatr Psychiatry. 2013;28(11):1109–24. doi: 10.1002/gps.3946. [DOI] [PubMed] [Google Scholar]
- 6.Prince M, Jackson J. World Alzheimer Report 2009. London: Alzheimer's Disease International; 2009. [Google Scholar]
- 7.McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR, Jr, Kawas CH, et al. The diagnosis of dementia due to Alzheimer's disease: Recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Demen. 2011;7(3):263–9. doi: 10.1016/j.jalz.2011.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McKeith IG, Dickson DW, Lowe J, Emre M, O'Brien JT, Feldman H, et al. Diagnosis and management of dementia with Lewy bodies: third report of the DLB Consortium. Neurology. 2005;65(12):1863–72. doi: 10.1212/01.wnl.0000187889.17253.b1. [DOI] [PubMed] [Google Scholar]
- 9.Rascovsky K, Hodges JR, Knopman D, Mendez MF, Kramer JH, Neuhaus J, et al. Sensitivity of revised diagnostic criteria for the behavioural variant of frontotemporal dementia. Brain. 2011;134(Pt 9):2456–77. doi: 10.1093/brain/awr179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gorno-Tempini ML, Hillis AE, Weintraub S, Kertesz A, Mendez M, Cappa SF, et al. Classification of primary progressive aphasia and its variants. Neurology. 2011;76(11):1006–14. doi: 10.1212/WNL.0b013e31821103e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gorelick PB, Scuteri AC, Black SE, DeCarli C, Greenberg SM, Iadecola C, et al. Vascular contributions to cognitive impairment and dementia: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42(9):2672–13. doi: 10.1161/STR.0b013e3182299496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Petersen RC MJ. Mild cognitive impairment as a clinical entity and treatment target. Arch Neurol. 2005;62(7):1160–3. doi: 10.1001/archneur.62.7.1160. [DOI] [PubMed] [Google Scholar]
- 13.Albert MS, DeKosky ST, Dickson D, Dubois B, Feldman HH, Fox NC, et al. The diagnosis of mild cognitive impairment due to Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Demen. 2011;7(3):270–9. doi: 10.1016/j.jalz.2011.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mitchell AJ, Shiri-Feshki M. Rate of progression of mild cognitive impairment to dementia – meta-analysis of 41 robust inception cohort studies. Acta Psychiatr Scand. 2009;119(4):252–65. doi: 10.1111/j.1600-0447.2008.01326.x. [DOI] [PubMed] [Google Scholar]
- 15.Dubois B, Feldman HH, Jacova C, Hampel H, Molinuevo JL, Blennow K, et al. Advancing research diagnostic criteria for Alzheimer's disease: the IWG-2 criteria. Lancet Neurology. 2014;13(6):614–29. doi: 10.1016/S1474-4422(14)70090-0. [DOI] [PubMed] [Google Scholar]
- 16.Hachinski VC, Iliff LD, Zilhka E, Du Boulay GH, McAllister VL, Marshall J, et al. Cerebral blood flow in dementia. Arch Neurol. 1975;32(9):632–7. doi: 10.1001/archneur.1975.00490510088009. [DOI] [PubMed] [Google Scholar]
- 17.Roman GC, Tatemichi TK, Erkinjuntti T, Cummings JL, Masdeu JC, Garcia JH, et al. Vascular dementia: diagnostic criteria for research studies. Report of the NINDS-AIREN International Workshop. Neurology. 1993;43(2):250–60. doi: 10.1212/wnl.43.2.250. [DOI] [PubMed] [Google Scholar]
- 18.DSM-5 Task Force. 5th ed. Washington, DC: American Psychiatric Association; 2013. Diagnostic and statistical manual of mental disorders. [Google Scholar]
- 19.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 20.Wharton SB, Brayne C, Savva GM, Matthews FE, Forster G, Simpson J, et al. Epidemiological neuropathology: the MRC Cognitive Function and Aging Study experience. J Alzheimers Dis. 2011;25(2):359–72. doi: 10.3233/JAD-2011-091402. [DOI] [PubMed] [Google Scholar]
- 21.Frisoni GB, Jack CR, Jr, Bocchetta M, Bauer C, Frederiksen KS, Liu Y, et al. The EADC-ADNI Harmonized Protocol for manual hippocampal segmentation on magnetic resonance: Evidence of validity. Alzheimers Dement. 2015;11(2):111–25. doi: 10.1016/j.jalz.2014.05.1756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chouraki V, Seshadri S. Genetics of Alzheimer's Disease. Adv Genet. 2014;87:245–94. doi: 10.1016/B978-0-12-800149-3.00005-6. [DOI] [PubMed] [Google Scholar]
- 23.Verghese PB, Castellano J, Holtzman DM. Apolipoprotein E in Alzheimer's Disease and other neurological disorders. Lancet Neurology. 2011;10(3):241–52. doi: 10.1016/S1474-4422(10)70325-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guerreiro R, Wojtas A, Bras J, Carrasquillo M, Rogaeva E, Majounie E, et al. TREM2 Variants in Alzheimer's Disease. N Engl J Med. 2013;368(2):117–27. doi: 10.1056/NEJMoa1211851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jonsson T, Stefansson H, Steinberg S, Jonsdottir I, Jonsson PV, Snaedal J, et al. Variant of TREM2 Associated with the risk of Alzheimer's disease. N Engl J Med. 2013;368(2):107–16. doi: 10.1056/NEJMoa1211103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lambert J, Ibrahim-Verbaas CA, Harold D, Naj AC, Sims R, Bellenguez C, et al. Meta-analysis of 74,046 individuals identifies 11 new susceptibility loci for Alzheimer's disease. Nat Genet. 2013;45(12):1452–8. doi: 10.1038/ng.2802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Beecham GW, Hamilton K, Naj AC, Martin ER, Huentelman M, Myers AJ, et al. Genome-wide association meta-analysis of neuropathologic features of Alzheimer's disease and related dementias. PLoS Genetics. 2014;10(9):e1004606. doi: 10.1371/journal.pgen.1004606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ferencz B, Gerritsen L. Genetics and Underlying Pathology of Dementia. Neuropsychol Rev. 2015;25(1):113–24. doi: 10.1007/s11065-014-9276-3. [DOI] [PubMed] [Google Scholar]
- 29.Biomarkers Definitions Working Group. Biomarkers and surrogate endpoints: preferred definitions and conceptual framework. Clin Pharmacol Ther. 2001;69(3):89–95. doi: 10.1067/mcp.2001.113989. [DOI] [PubMed] [Google Scholar]
- 30.Vos SJ, Verhey F, Frölich L, Kornhuber J, Wiltfang J, Maier W. Prevalence and prognosis of Alzheimer's disease at the mild cognitive impairment stage. Brain. 2015 Feb 17; doi: 10.1093/brain/awv029. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jack CR, Jr, Wiste HJ, Weigand SD, Rocca WA, Knopman DS, Mielke MM, et al. Age-specific population frequencies of cerebral beta-amyloidosis and neurodegeneration among people with normal cognitive function aged 50-89 years: a cross-sectional study. Lancet Neurol. 2014;13(10):997–1005. doi: 10.1016/S1474-4422(14)70194-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Carrillo MC, Blennow K, Soares H, Lewczuk P, Mattsson N, Oberoi P, et al. Global standardization measurement of cerebral spinal fluid for Alzheimer's disease: an update from the Alzheimer's Association Global Biomarkers Consortium. Alzheimers Dement. 2013;9(2):137–40. doi: 10.1016/j.jalz.2012.11.003. [DOI] [PubMed] [Google Scholar]
- 33.Klunk WE, Koeppe RA, Price JC, Benzinger TL, Devous MD, Sr, Jagust WJ, et al. The Centiloid Project: Standardizing quantitative amyloid plaque estimation by PET. Alzheimers Dement. 2015;11(1):1–15. doi: 10.1016/j.jalz.2014.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bocchetta M, Galluzzi S, Kehoe PG, Aguera E, Bernabei R, Bullock R, et al. The use of biomarkers for the etiologic diagnosis of MCI in Europe: An EADC survey. Alzheimers Dement. 2015;11(2):195–206. doi: 10.1016/j.jalz.2014.06.006. [DOI] [PubMed] [Google Scholar]
- 35.National Collaborating Centre for Mental Health. Leicester: The British Psychological Society and Gaskell. Dementia: The NICE–SCIE Guideline on supporting people with dementia and their carers in health and social care. National Clinical Practice Guideline; 42. 2007 [PubMed] [Google Scholar]
- 36.McCleery J, Morgan S, Bradley K, Noel-Storr A, Ansorge O, Hyde C. Cochrane Database of Systematic Reviews. Dopamine transporter imaging for the diagnosis of dementia with Lewy bodies. 2015(1):010633. doi: 10.1002/14651858.CD010633.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Deckers K, van Boxtel MP, Schiepers OJ, de Vugt M, Muñoz Sánchez JL, Anstey KJ, et al. Target risk factors for dementia prevention: a systematic review and Delphi consensus study on the evidence from observational studies. Int J Geriatr Psychiatry. 2015;30(3):234–46. doi: 10.1002/gps.4245. [DOI] [PubMed] [Google Scholar]
- 38.Lakey L. Counting the cost: Caring for people with dementia on hospital wards. London: Alzheimer's Society; [Google Scholar]
- 39.Inouye SK, Westendorp RG, Saczynski JS. Delirium in elderly people. Lancet. 2014;383(9920):911–22. doi: 10.1016/S0140-6736(13)60688-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gray SL, Anderson ML, Dublin S, Hanlon JT, Hubbard R, Walker R, et al. Cumulative use of strong anticholinergics and incident dementia: A prospective cohort study. JAMA Int Med. 2015;175(3):401–7. doi: 10.1001/jamainternmed.2014.7663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Billioti de Gage S, Moride Y, Ducruet T, Kurth T, Verdoux H, Tournier M. Benzodiazepine use and risk of Alzheimer's disease: casecontrol study. BMJ. 2014 Sep 9;:349. doi: 10.1136/BMJ.G5205. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Joint Formulary Committee. British National Formulary (BNF) 69. London: BMJ Publishing Group and Royal Pharmaceutical Society; 2015. [Google Scholar]
- 43.NICE Clinical Guideline; 42. Dementia: supporting people with dementia and their carers in health and social care. (Incorporating NICE technology appraisal guidance 217; 2011). [Google Scholar]
- 44.London: National Institute for Health and Care Excellence; 2013 [Google Scholar]
- 45.Birks J. Cochrane Database of Systematic Reviews. Cholinesterase inhibitors for Alzheimer's disease. 2006(1):005593. doi: 10.1002/14651858.CD005593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.McShane R, Areosa Sastre A, Minakaran N. Cochrane Database of Systematic Reviews. Memantine for dementia. 2006(2):003154. doi: 10.1002/14651858.CD003154.pub5. [DOI] [PubMed] [Google Scholar]
- 47.Li Y, Hai S, Zhou Y, Dong B. Cholinesterase inhibitors for rarer dementias associated with neurological conditions. Cochrane Database of Systematic Reviews. 2015(3):009444. doi: 10.1002/14651858.CD009444.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Boxer AL, Knopman DS, Kaufer DI, Grossman M, Onyike C, Graf- Radford N, et al. Memantine in patients with frontotemporal lobar degeneration: a multicentre, randomised, double-blind, placebocontrolled trial. Lancet Neurol. 2013;12(2):149–56. doi: 10.1016/S1474-4422(12)70320-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Howard R, McShane R, Lindesay J, Ritchie C, Baldwin A, Barber R, et al. Donepezil and Memantine for moderate-to-severe Alzheimer's disease. N Engl J Med. 2012;366(10):893–903. doi: 10.1056/NEJMoa1106668. [DOI] [PubMed] [Google Scholar]
- 50.Ritchie C, Bajwa J, Coleman G, Hope K, Jones R, Lawton M, et al. Souvenaid®: a new approach to management of early Alzheimer's disease. J Nutr Health Aging. 2014;18(3):291–9. doi: 10.1007/s12603-013-0411-2. [DOI] [PubMed] [Google Scholar]
- 51.Ballard C, Waite J, Birks J. Atypical antipsychotics for aggression and psychosis in Alzheimer's disease. Cochrane Database of Systematic Reviews. 2006(1):003476. doi: 10.1002/14651858.CD003476.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Corbett A, Pickett J, Burns A, Corcoran J, Dunnett SB, Edison P, et al. Drug repositioning for Alzheimer's disease. Nature Rev.Drug Discov. 2012;11(11):833–46. doi: 10.1038/nrd3869. [DOI] [PubMed] [Google Scholar]
- 53.Cummings JL, Mega M, Gray K, Rosenberg-Thompson S, Carusi DA, Gornbein J. The Neuropsychiatric Inventory: comprehensive assessment of psychopathology in dementia. Neurology. 1994;44(12):2308–14. doi: 10.1212/wnl.44.12.2308. [DOI] [PubMed] [Google Scholar]
- 54.Yesavage JA, Sheikh JI. Geriatric Depression Scale (GDS) Clin Gerontol. 1986;5(1-2):165–73. [Google Scholar]