Abstract
The use of nanoparticulate pharmaceutical drug delivery systems (NDDSs) to enhance the in vivo effectiveness of drugs is now well established. The development of multifunctional and stimulus-sensitive NDDSs is an active area of current research. Such NDDSs can have long circulation times, target the site of the disease and enhance the intracellular delivery of a drug. This type of NDDS can also respond to local stimuli that are characteristic of the pathological site by, for example, releasing an entrapped drug or shedding a protective coating, thus facilitating the interaction between drug-loaded nanocarriers and target cells or tissues. In addition, imaging contrast moieties can be attached to these carriers to track their real-time biodistribution and accumulation in target cells or tissues. Here, I highlight recent developments with multifunctional and stimuli-sensitive NDDSs and their therapeutic potential for diseases including cancer, cardiovascular diseases and infectious diseases.
Nanoparticulate pharmaceutical drug delivery systems (NDDSs) are widely used in pharmaceutical research and in clinical settings to enhance the effectiveness of diagnostic agents and drugs, including anticancer, antimicrobial and antiviral drugs1,2. The types of nano-carriers that exist are diverse and include the following: liposomes; polymeric nanoparticles; polymeric micelles; silica, gold, silver and other metal nanoparticles; carbon nanotubes; solid lipid nanoparticles; niosomes; and dendrimers. The use of NDDSs can overcome several problems that are associated with traditional drugs, such as poor aqueous solubility, low bioavailability and nonspecific distribution in the body.
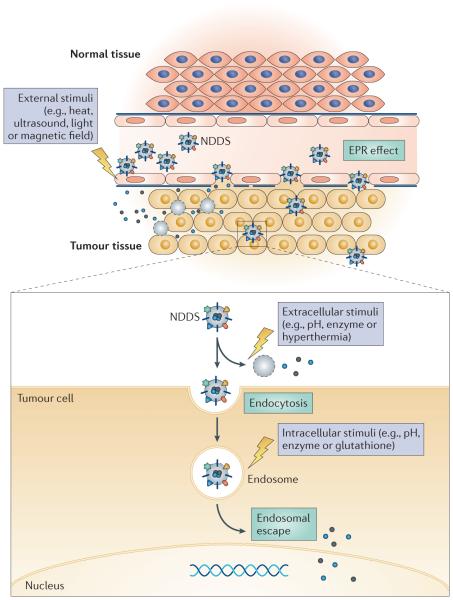
The first generation of NDDSs mainly aimed to address single challenges, such as the need to increase drug stability in vivo and the circulation time in the blood, or the need to target a drug to a specific tissue or pathology. Now, research has led to the development of NDDSs that can perform two or more functions (either simultaneously or sequentially) to overcome multiple physiological barriers to optimize delivery and deliver their loads (which can be single or multiple) to the required target sites (such as organs, tissues, cells) or specific pathologies in the body3 (FIG. 1). The properties of multifunctional NDDSs include the ability to bear a sufficient load of a drug or DNA-related material, have increased circulation times (through the use of soluble polymers) and target the intended site of action both nonspecifically (for example, via the enhanced permea-bility and retention (EPR) effect) and specifically (via the attachment of target-specific ligands). In addition, multifunctional NDDSs can respond to several stimuli that are characteristic of the pathological site, which is achieved through the inclusion of components that react to abnormal pH, temperature and redox conditions, and to the overexpression of certain biological molecules. Multifunctional NDDSs can also respond to stimuli from outside the body, such as magnetic or ultrasound fields, and can be supplemented with an imaging contrast moiety to enable their biodistribution, target accumulation or the efficacy of the therapy to be monitored.
Figure 1. Schematic of a drug-loaded, multifunctional, stimuli-sensitive NDDS.
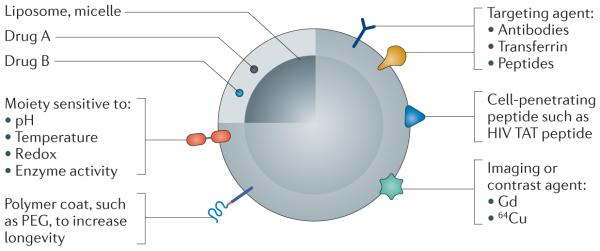
Drugs (Drug A and Drug B) can be loaded into a pharmaceutical nanocarrier, such as a liposome or polymeric micelle. Depending on the purpose of the nanoparticulate pharmaceutical drug delivery system (NDDS), various agents can be added to the nanoparticle to target the NDDS to a particular tissue, to increase cell penetration, to enable imaging or to release the drugs in response to a given stimulus.
PEG, poly(ethylene glycol).
Although as yet there is no broadly recognized and accepted single classification system for multifunctional NDDSs, they can generally be divided into three groups. The first group consists of drug-loaded NDDSs that com-bine at least two different functions, such as longevity, targetability, stimuli-sensitivity or cell penetration. The second group of NDDSs, in addition to the previously described properties, are loaded with more than one drug and/or gene therapy-related material, such as antisense oligonucleotides or small interfering RNAs (siRNAs). The third group consists of so-called theranostic NDDSs, which have an additional diagnostic label for use with current clinical imaging modalities.
Research in the area of multifunctional NDDSs4,5 is very active, but substantial work remains to make them a clinical reality. Here, I highlight recent developments relating to multifunctional NDDSs. The majority of the currently available data relate to cancer, although there are some examples with other diseases.
NDDS longevity and targeting
One of the most common uses of NDDSs is to combine prolonged circulation times with targetabilty. Such NDDSs are particularly useful for tumour targeting because tumours (as well as other inflammation zones) usually have increased vascular permeability as well as poor lymphatic drainage6,7. This enables long-circulating NDDSs to accumulate in tumours through the EPR effect, which forms the basis for passive targeting8 . Nevertheless, EPR-based drug delivery strategies face several challenges. First, tumours — especially large, solid tumours — are pathophysiologically heterogeneous. Some parts of such tumours are not vascularized, do not exhibit the EPR effect, may have sizeable necrotic areas9,10 and have varied microvascular permeability10. In addition, the increased interstitial pressure that exists within tumours may limit the EPR-mediated accumulation of NDDSs even if the vasculature is leaky11.
NDDSs that are used for passive targeting and/or spontaneous accumulation must have long circulation times to ensure that sufficient drug is delivered to the target tissue. The usual approach to obtain long-circulating NDDSs is to coat them with hydrophilic and flexible polymers, such as poly(ethylene glycol) (PEG), as was first suggested for liposomes12. The pegylation of NDDSs prevents their interaction with opsonins and impedes their capture and clearance by the mononuclear phagocyte system. However, pegylated NDDSs can induce the production of antibodies that can accelerate the blood clearance of nanoparticles (as was demonstrated for clinically used pegylated liposomes), particularly after repetitive administration; this is the so-called accelerated blood clearance phenomenon13,14.
Although PEG is still the gold-standard polymer that is used to prepare long-circulating NDDSs, other hydrophilic polymers that are used include poly[N-(2-hydroxypropyl) methacrylamide]15, poly(acryloyl morpholine), poly-N-vinylpyrrolidones16 and polyvinyl alcohol17. In general, the concept of pegylation, as well as the use of alternative polymers for longevity, is well established and reviewed; thus, in the next section only some of the key developments in this area are briefly mentioned. Importantly, the shape of NDDSs can also influence their pharmacokinetics and biodistribution18,19.
Liposomal long-circulating NDDSs are the most frequently studied type of NDDS; however, synthetic amphiphilic polymers have also been used to sterically stabilize several other types of NDDS to alter their bio-distribution. For example, pegylation of gold nanoparticles reduced their uptake by the mononuclear phagocyte system and their subsequent clearance from the body20. One potential application of pegylated gold nanoparticles is their use in photothermal tumour therapy (known as ablation) following their accumulation in the tumour21. Pegylated methotrexate-conjugated poly-l-lysine dendrimers also accumulated efficiently in solid tumours in rats and mice via the EPR affect22, and pegylation reduced the toxicity of positive charge-bearing dendrimers in cell-culture experiments23. Quantum dots can also be modified by pegylation. In mice, pegylated quantum dots had prolonged circulation times, which were attrib-utable to their decreased uptake in organs (such as the spleen and liver) in which the mononuclear phagocyte system is active24.
Active targeting of NDDSs can be achieved by attaching targeting ligands, such as monoclonal antibodies, transferrin, various peptides, folate, aptamers (single-stranded oligonucleotides) or certain sugar moieties, onto their surface25,26. To prevent steric hindrance between the targeting moiety and the protective polymer (such as PEG), the targeting ligand is usually attached to the chemically activated distal end of the NDDS-grafted polymeric chain27. An example of such active targeting of NDDSs is pegylated doxorubicin-loaded liposomes that have human epidermal receptor 2 (HER2; also known as ERBB2)-specific antibodies attached; these were suc-cessfully used to target HER2-overexpressing SK-BR3 cells in mice28. A nucleosome-specific monoclonal antibody (mAb 2C5) that recognized multiple types of tumour cells via tumour cell-surface-bound nucleosomes improved the targeting of doxorubicin-loaded liposomes to tumour cells and increased cancer cell cytotoxicity in in vitro and in vivo models29 , including nude mice xeno-grafted with the U-87 cell line, which was derived from a human glioblastoma30. In another example of active targeting, pegylated gold nanoparticles conjugated to monoclonal F19 antibodies were used as targeted label-ling agents for human pancreatic carcinoma tissues31. Lactoferrin-conjugated PEG–polylactic-acid nanoparticles improved the delivery of the conjugated particles to the brain in an experimental murine model32.
An interesting approach to increase targeting centres on self-assembling polyalkylcyanoacrylate-based nanoparticles. These types of nanoparticles could serve as pharmaceutical carriers for various drugs and could be produced in pegylated and ‘activated’ forms, enabling various ligands to be easily attached33. Polyisohexyl-cyanoacrylate nanoparticles loaded with doxorubicin produced by BioAlliance Pharma as Livatag (doxorubicin Transdrug) are currently in a Phase III trial in Europe and in the United States as a second-line treatment of hepatocellular carcinoma after sorafenib, at a stage with no available approved treatment (Livatag press release; see Further information).
Aptamers that impart affinity and specificity by electrostatic, hydrogen or hydrophobic bonding, but not via the base pairing, have also been used as stable and efficient targeting moieties for NDDSs. For example, liposomal NDDSs modified with specific aptamers have been used to target leukaemia cells34.
Targetability can also be applied to stimuli-sensitive NDDSs. Gemcitabine-loaded pegylated pH-sensitive liposomes modified with an epidermal growth factor receptor (EGFR)-specific antibody efficiently inhibited tumour growth in mice35. Micellar NDDSs that were composed of amphiphilic conjugates of PEG and a co-polymer of poly(ε-caprolactone) and poly(malic acid) loaded with doxorubicin conjugated to poly(malic acid) via a pH-sensitive bond were modified with folate for enhanced cellular uptake36. This preparation provided an enhanced release of doxorubicin at lowered pH values inside cancer cells36. NDDSs with similar properties based on pH-sensitive polymethacrylate (PMA)-grafted poly(amidoamine) nanocarriers and additionally pegylated and modified with a folate moiety efficiently delivered paclitaxel to tumours and inhibited tumour growth in mice37.
Clearly, the separation of long-circulating NDDSs into those that achieve active targeting and passive targeting is conditional. That is, both phenomena are closely connected because NDDSs will accumulate in the target area via the EPR effect (passive targeting) before ligand-mediated interaction with target cells (active targeting) occurs.
Another interesting issue is associated with the use of targeting ligands that are also naturally present (in their free form) in the circulation, such as folate, transferrin or certain peptides. Although one may expect competition between the ligands attached to NDDSs and the native ligands for the binding sites, the success of folate-and transferrin-targeted NDDSs (see below) demonstrates that this potential problem can be overcome. This is probably achieved through multipoint interactions of ligand-modified NDDSs with the target and/or because of the rapid recirculation of the cognate receptors, which provides sufficient opportunities for an interaction of the NDDS with the receptor.
Disease applications for NDDS-based therapies
Cardiovascular diseases
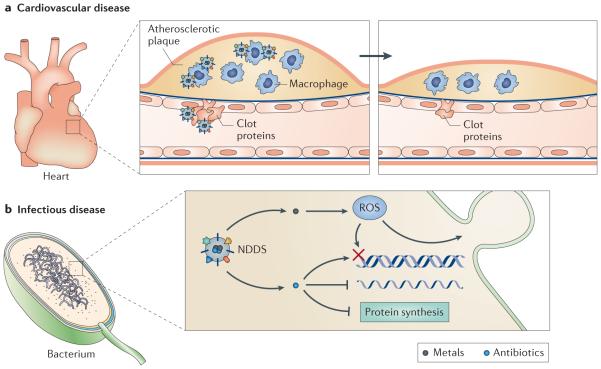
NDDSs hold promise as therapeutic, diagnostic and theranostic agents for cardio-vascular diseases38, particularly atherosclerosis39 (FIG. 2). Multifunctional micellar NDDSs that combined a targeting pentapeptide, a fluorophore and a drug targeting atherosclerotic plaques by specifically binding to clotted plasma proteins were used to visualize atherosclerotic lesions in a mouse model. This preparation was shown to increase the amount of the anticoagulant agent biva-lirudin that was delivered to the lesion40. Because the increased uptake of low-density lipoproteins (LDLs) by resident macrophages in plaques is associated with the progression of atherosclerosis, targeting plaque-associated macrophages could be a method of inhibiting LDL uptake41. Indeed, targeted polymeric NDDSs loaded with pravastatin specifically and dramatically inhibited the phagocytic activity of macrophages without affecting non-target cells42.
Figure 2. Multifunctional and stimuli-sensitive NDDSs in cardiovascular pathologies and infectious diseases.
a | Nanoparticulate pharmaceutical drug delivery systems (NDDSs) can be engineered to target activated macrophages in atherosclerotic plaques or proteins present in a clot. These nanoparticles can thereby reduce plaque size through these two distinct mechanisms. b | NDDSs can be used to deliver metals to bacteria, where they can generate reactive oxygen species (ROS) to induce membrane blebbing and DNA damage. Antibiotics can also be delivered intracellularly using NDDSs.
Multimodal diagnostic micellar NDDSs that were fluorescent and paramagnetic and targeted to macrophage scavenger receptors using specific antibodies have been used to visualize lesions in the abdominal aortas of mice with atherosclerosis43. Furthermore, polymeric NDDSs made of polyketals that were used to deliver small-molecule drugs, such as the p38 mitogen-activated protein kinase (MAPK) inhibitor SB239063, and anti-oxidant proteins, such as superoxide dismutase, to the area of the myocardial infarction in a rat model significantly improved cardiac function44.
Liposome-based systems have also been frequently used to study the potential use of NDDSs in cardiovascular diseases45. For example, liposomes loaded with ATP or co-enzyme Q accumulated well in the infarcted areas of the myocardium and improved cardiac parameters in rat and rabbit models of myocardial infarct46,47. In a rat model of heart transplant, organ rejection was simultaneously imaged and treated using multifunctional polymeric NDDSs co-loaded with superparamagnetic iron oxide nanoparticles (SPIONs) and plasmid DNA48. The SPION acted as a magnetic resonance imaging (MRI) contrast agent, whereas the plasmid DNA suppressed the local immune response48. NDDSs for targeted thrombolytic therapy were developed by conjugating a thrombolytic agent (recombinant tissue plasminogen activator) to dextran-coated iron oxide nanoparticles, which were additionally modified with a thrombus-targeted peptide that was sensitive to activated factor XIII49. These NDDSs had increased binding to the margins of intravascular thrombi and good thrombolytic activity in a mouse model of pulmonary embolism.
The translation of these NDDSs and others identified in similar studies into clinical practice remains the primary challenge to advancing the field and will be addressed in the closing section of this article.
Infectious diseases
NDDSs have a growing role in combatting infectious diseases50. Of particular interest here are multicomponent NDDSs that contain metals, which can facilitate the formation of reactive oxygen species to eliminate pathogenic bacteria (FIG. 2). For example, NDDSs that combined iodinated chitosan and silver nanoparticles bound to and killed bacteria better than either component alone51. Hydrogel and glass-based nanoparticles capable of releasing nitric oxide facilitated the cleaning and healing of open wounds in mice52. NDDSs can be used to deliver antibiotics inside cells; murine salmonellosis was successfully treated (with a greater than tenfold decrease in the level of pathogen in the liver and spleen of experimental mice) using gentamicin in silica xerogel-based NDDSs53. The bacteria-mediated degradation of a polyphosphoester core of antibiotic-loaded NDDSs by bacterial enzymes54 provided an interesting example of a targeted, responsive NDDS. Nevertheless, this area is in early stages of development and more animal-based studies will be required to reveal its full potential.
Cancer
The majority of preclinical research with NDDSs relates to cancer. Based on one of the most popular pharmaceutical nanocarriers — liposomes — several anticancer NDDSs are available at different stages of development (see TABLE 1 for a selected list).
Table 1.
Liposome-based drugs for cancer therapy
| Drug formulation | Indication | Status* | Refs |
|---|---|---|---|
| Liposomal doxorubicin (Doxil, also known as Caelyx; Janssen) |
AIDS-related Kaposi’s sarcoma, recurrent ovarian cancer, metastatic breast cancer and multiple myeloma |
Approved | 165 |
|
| |||
| Non-pegylated liposomal doxorubicin (Myocet; Sopherion Therapeutics) |
Metastatic breast cancer | Approved | 168,169 |
|
| |||
| Liposomal doxorubicin (LipoDox; Sun Pharma Global FZE) |
Kaposi’s sarcoma, breast and ovarian cancer |
Approved | 170,171 |
|
| |||
| Thermally sensitive liposomal doxorubicin (Thermodox; Celsion ) |
Hepatocellular carcinoma | Phase III, active: NCT00617981 | 182 – 184 |
|
| |||
| Breast cancer | Phase I/II, recruiting: NCT00826085 | ||
|
| |||
| Hepatocellular carcinoma | Phase III, recruiting: NCT02112656 | ||
|
| |||
| Liposomal paclitaxel (Lipusu; Luye Pharma) |
Solid tumours | Approved in China | 166 |
|
| |||
| Liposomal paclitaxel (EndoTAG-1; Medigene) |
Breast cancer | Phase II, completed: NCT01537536, NCT00448305 |
175,176 |
|
| |||
| Pancreatic cancer | Phase II, completed: NCT00377936 | ||
|
| |||
| Liver cancer | Phase II, completed: NCT00542048 | ||
|
| |||
| Liposomal paclitaxel (LEP-ETU; NeoPharm) |
Breast cancer | Phase II, completed: NCT01190982 | 202 |
|
| |||
| Liposomal daunorubicin (DaunoXome; Galen) |
Kaposi’s sarcoma | Approved | 167 |
|
| |||
| Liposomal vincristine (Marqibo; Talon Therapeutics) |
Acute lymphoblastic leukaemia | Approved | 172 – 174 |
|
| |||
| Liposomal cisplatin (LiPlaCis; LiPlasome Pharma) |
Advanced or refractory solid tumours | Phase I, recruiting: NCT01861496 | 203 |
|
| |||
| Liposomal cisplatin (Lipoplatin; Regulon) | Pancreatic cancer, non-small-cell lung cancer, head and neck cancer and breast cancers |
Phase I/II/III |
175, 177–179 |
|
| |||
| Liposomal cisplatin (SPI-077; Azla Corporation) |
Ovarian cancer | Phase II, completed: NCT00004083 |
175,180, 181 |
|
| |||
| Liposomal formulation of SN-38, the active metabolite of irinotecan (LE-SN38; NeoPharm) |
Colorectal carcinoma | Phase II, completed: NCT00311610 | 175,185 |
|
| |||
| Liposomal irinotecan HCl: floxuridine mixture (CPX-1; Celator Pharmaceuticals) |
Colorectal cancer | Phase II, completed: NCT00361842 | 182 |
|
| |||
| Liposomal irinotecan (MM-398; Merrimack Pharmaceuticals) |
Metastatic pancreatic cancer | Phase III, active: NCT01494506 | 204 |
|
| |||
| Liposomal L-annamycin | Acute lymphocytic leukaemia, doxorubicin-resistant blood cancer |
Phase I/II | 186,187 |
|
| |||
| Liposomal vinorelbine, INX-0125 (AlocrestTM; Hana Biosciences) |
Hodgkin’s disease, non-Hodgkin’s lymphoma | Phase I, active: NCT00364676 | 188 |
ClinicalTrials.gov identifiers provided where appropriate.
The next step in the development of anticancer NDDSs is to target them to tumours. Cancer cells contain several targets discussed below that can be used by NDDSs. Each of these targets could be specific for a certain type or types of cancer. Although it is possible that there will be overlapping expression of a target in cancer cells and normal cells, the level of expression is usually much higher in cancer cells; this characteristic is a prerequisite for an NDDS-targeting ligand.
Folate has been used as a targeting ligand in preclinical studies of NDDSs, owing to its easy conjugation to nanocarriers, high affinity for folate receptors and the lower expression of folate receptors in normal cells then in cancer cells and activated macrophages that are typical of inflammatory diseases55. Numerous folate-targeted liposomal systems for cancer have been described (reviewed in REFS 56,57). For example, liposomes modified with folate via a PEG spacer efficiently delivered their cargo intracellularly through receptor-mediated endocytosis (which could bypass multidrug resistance), and doxorubicin-mediated cytotoxicity against cancer cells expressing folate receptors was 85-fold higher with drug-loaded targeted liposomes than with unmodified liposomes58. In addition, when glutathione-conjugated folate was coupled to a PEG–distearoylphosphatidyl-ethanolamine (PEG–DSPE) polymer and incorporated into the liposomal membrane, there was increased activity of the liposomal vincristine and favourable pharmaco-kinetics in mice59. Folate-based modified NDDSs loaded with paclitaxel60 or carboplatin61 had high antitumour activity in mouse models. Liposome targeting to folate receptors has also been used to improve gene delivery of the herpes simplex virus type 1 thymidine kinase suicide gene; the liposome preparation inhibited tumour growth in a mouse model of oral cancer62.
Transferrin, an 80 kDa serum glycoprotein, binds to the transferrin receptor and is taken into cells via receptor-mediated endocytosis. Compared with normal cells, the expression of transferrin receptor in certain cancer cells is much higher because of their increased demand for iron. Consequently, transferrin-receptor-targeted NDDSs could be used for anticancer therapy. Indeed, this was demonstrated with doxorubicin-loaded long-circulating transferrin-modified liposomes in a rat model of liver cancer63. Other examples of the anticancer effects of transferrin-targeted liposomes in mouse models include those loaded with boron compounds64,65 and with ceramide66.
EGFRs are frequently overexpressed in solid tumours67,68 and are therefore popular targets for NDDSs. HER2, which is overexpressed in approximately 20% of breast cancers68 and some other cancers, is also a popular target for NDDSs. For example, there was greater accumulation of HER2-targeted pegylated liposomes loaded with doxorubicin than of non-targeted liposomes in HER2-overexpressing breast cancer cells69 and in ascitic lymphoma cells70.
The tumour vasculature is also an attractive target; destruction of the vasculature inhibits tumour growth and metastasis, it is not tumour type-specific and, importantly, NDDSs do not need to diffuse into the tumour mass to reach this target71. Targets that have been the focus of most studies include vascular endothelial growth factor (VEGF; especially for anti-angiogenic therapy), vascular cell adhesion molecule (VCAM), matrix metalloproteinases (MMPs) and integrins72,73. For example, peptides that bind specifically to the tumour vasculature coupled to liposomes loaded with doxorubicin improved drug efficacy against several human cancers in severe combined immunodeficient mice74. Pegylated VCAM-targeted immunoliposomes bound selectively to activated endothelial cells in vitro and accumulated in tumour vessels in vivo75. MMPs are overexpressed on the newly formed vessels and tumour tissues, and are involved in tissue remodelling, tumour invasiveness, resistance to apoptosis and metastasis. An antigen-binding fragment of the antibody against MMP that was conjugated to doxorubicin-loaded liposomes via a PEG spacer showed enhanced tumoural uptake and inhibited tumour growth in a mouse model76.
Considerations for NDDS receptor targeting
The success of receptor-mediated targeting depends strongly on the target affinity and the density of the receptors that are present on the cell surface. In addition, with pegylated NDDSs, the surface-attached PEG could prevent or hinder the interaction between the targeting ligand and its receptor. In a sense, this limits the opportunities of targeting because not all potential targets are expressed at sufficient levels. It is also important to consider, on a case by case basis, whether spontaneous targeting (passive accumula-tion; based on the EPR effect) or ligand-mediated specific targeting (which clearly requires more synthetic effort) is preferable. In general, if good accumulation of a drug in the pathological tissue is the primary goal, then EPR-mediated accumulation may suffice. However, if the presence of the drug inside the cell is needed then ligands that can be internalized may be required.
Stimuli-sensitive NDDSs
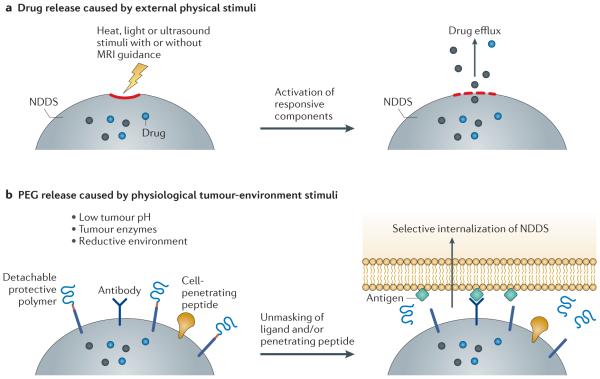
The use of NDDSs that respond to different types of stimuli to control the properties and behaviour of the NDDS is an important and growing area of research77 (FIG. 3; TABLE 2). The stimuli can be internal and intrinsic to the target tissue (such as changes in pH, temperature, redox condition or the activity of certain enzymes) or external and artificially applied (such as a magnetic field, ultrasound and various types of irradiation) (FIG. 4).
Figure 3. Penetration of NDDSs into pathological tissue and interaction with target cells.
Moieties attached to nanoparticulate pharmaceutical drug delivery systems (NDDSs) can enhance their penetration into the target tissue or cell. Externally applied stimuli (such as heat) or intrinsic stimuli (such as a change in pH in the target tissue) can cause the NDDS to release its cargo in the vicinity of the target tissue (such as a tumour). Intracellular proteins specific to the target tissue can be used to ensure cargo release in the correct cell type. EPR, enhanced permeability and retention.
Table 2.
Stimuli that can control the behaviour and/or properties of NDDSs
| Stimulus | Mechanistic basis | Key studies | Refs |
|---|---|---|---|
| pH | Low pH occurs in pathological areas such as tumours, infarcts and sites of inflammation, because of hypoxia (owing to increased glycolysis) and massive cell death; low pH also occurs in endosomes and the cytoplasm |
pH-responsive complexes were achieved by engineering prefunctionalized polymers; these complexes successfully co-delivered doxorubicin and siRNA into cancer cells |
189 |
|
| |||
| Redox conditions |
There is an increased concentration of glutathione inside many pathological cells |
Bioreducible compounds containing disulphide bonds, such as poly(disulphide amine) and disulphide-based poly(amidoamine) polymers and dendrimers, increased the efficiency of intracellular gene delivery |
190 – 192 |
|
| |||
| An NDDS comprised of an siRNA–lipid conjugate (composed of a GFP-targeted siRNA conjugated to lipids via a disulphide bond) incorporated into polymeric micelles (made of a PEG2000–PE conjugate) protected siRNA from degradation; siRNA was released in reducing glutathione-rich surroundings, and downregulated the GFP-encoding gene 30-fold more effectively than did free siRNA |
193 | ||
|
| |||
| Enzyme activity |
Certain enzymes are upregulated in pathological areas; for example, MMPs are upregulated in tumours |
100 nm nanoparticles composed of a gelatin (an MMP substrate) core and amino-PEG quantum dots conjugated to the core surface were degraded by MMPs in a mouse tumour model; the MMP degradation caused release of the quantum dots, which penetrated further into the tumour mass |
194 |
|
| |||
| Multifunctional liposomes containing an MMP2-responsive moiety (maleimide– PEG-cleavable peptide–DOPE) increased tumour targeting and internalization of the nanocarrier by tumour cells |
105 | ||
|
| |||
| Temperature | Inflammation-induced hyperthermia |
The temperature difference between normal and diseased tissues is not usually high enough for most thermosensitive NDDSs, so an external heating source (such as a water bath, electromagnet, laser or high-intensity focused ultrasound to control the local temperature) is required |
103,195, 196 |
|
| |||
| Grafting a co-polymer of vinylpyrrolidinone and N-isopropylacryamide onto PE enhanced the accumulation of the now-thermosensitive conjugate in hyperthermia (42 °C)-treated tumours in a mouse model; there was a tenfold increase in DNA deposition in heated tumours compared with non-heated tumours |
89 | ||
|
| |||
| Magnetic nanoparticles (15 nm) introduced directly into a tumour in a mouse model and then heated using an alternating high frequency magnetic field were able to irreparably damage tumour cells or sensitize the tumour cells for additional chemo- or radiotherapy |
98 | ||
|
| |||
| Ultrasound | Local ultrasound increases temperature and microconvection in target tissues, resulting in a temporary or permanent destruction of cell membranes |
Locally applied ultrasound led to the tumour-specific release of ~70% of loaded cisplatin from liposomes (compared with <3% release without ultrasound); this inhibited the growth of lymphoma and colon tumours in mouse models |
197 |
|
| |||
| Liposomes co-loaded with inert gases or perfluorated hydrocarbon and drugs could be used as contrast agents or for local drug release; this approach may work better on superficial tumours |
198 | ||
|
| |||
| Magnetic field | A magnetic field can concentrate magnetically sensitive NDDSs in specific areas |
Conjugation of paclitaxel to PEG–SPION via a pH-sensitive ester bond resulted in NDDSs with high anticancer activity in vitro and in a mouse H22 tumour model |
97,199 |
|
| |||
| Methotrexate- and glutamic acid-complexed iron oxide co-loaded into liposomes caused a fivefold increase in drug accumulation in the target tissue of experimental mice when an external magnetic field was applied compared with a magnetically insensitive preparation |
200 | ||
|
| |||
| Light | Light-sensitive components can be incorporated into NDDSs; light induces photo-triggered structural changes in the NDDSs, leading to their direct interaction with the target cells. This interaction occurs via membrane fusion, photoisomerism, photofragmentation or photopolymerization, and/or drug leakage from NDDSs |
A photosensitive, amphiphilic, dendritic conjugate based on the near-infrared- sensitive diazonaphthoquinone assembled into a photosensitive micellular nanocarrier loaded with doxorubicin enabled rapid drug release in vitro |
201 |
DOPE, dioleoylphosphatidylethanolamine; GFP, green fluorescent protein; MMP, matrix metalloproteinase; NDDS, nanoparticulate pharmaceutical drug delivery system; PE, phosphatidyl ethanolamine; PEG, poly(ethylene glycol); siRNA, small interfering RNA; SPION, superparamagnetic iron oxide nanoparticles.
Figure 4. Methods for targeted drug release.
Various external stimuli can be applied to facilitate intracellular delivery (part a), and various local stimuli, such as enzymes present in the tumour environment, can be used to eliminate the protective poly(ethylene glycol) (PEG) layer from a nanoparticulate pharmaceutical drug delivery system (NDDS) to facilitate its interaction with target cells (part b). MRI, magnetic resonance imaging.
pH-triggered drug delivery
The acidic environment of tumours78,79 and endosomes can be harnessed in the design of stimuli-sensitive NDDSs. For example, an NDDS can contain pH-sensitive components that protonate at lowered pH, resulting in the destabilization of the carrier and release of the drug. Pegylated poly l-histidine can form fairly stable polymeric micelles, but at pH values of approximately 6.5 and lower, histidine residues in the polyhistidine block become protonated, which results in an increase in the critical micelle concentration and micelle destabilization. As a result, the micelle-incorporated drug is released80; the high resultant drug concentration in the tumour interstitium or in the cytoplasm of the cancer cell may overcome drug efflux and other mechanisms of drug resistance81,82.
To avoid the premature degradation of drugs in lysosomes, pH-sensitive components (such as dioleoylphosphatidylethanolamine (DOPE)) that are capable of destabilizing the endosomal membrane or rupturing endosomes are used to modify NDDSs (such as liposomal NDDSs). This facilitates the fusion of the NDDS with the endovacuolar membrane after endocytosis and the subsequent release of the contents of the NDDS into the cytoplasm in response to the lowered endosomal pH83. Lipid conjugates of polyethyleneimine, such as DOPE-modified low-molecular-mass polyethyl-eneimine (PEI; 1,800 Da), were used to prepare nanoparticles to improve the PEI-mediated intracellular delivery of DNA84 and siRNA85 for various therapeutic purposes. Such conjugates have the combined advantages of positive charge, buffering capacity, fusogenicity and lowered toxicity.
The stimulus sensitivity of PEG coatings can enable the preparation of NDDSs with functions that are unveiled and activated only after the PEG molecules are detached. The use of ester and hydrazone moieties between the PEG moieties and NDDSs (which are stable at a neutral pH, such as in the blood, but hydrolyse at a pH of 6 or below) eliminates the protective effect of PEG during internalization by the target cell but also enables prolonged circulation in the blood. PEG is then removed once the NDDS is inside the acidified targets. PEG was detached from pH-sensitive PEG–hydrazone– phosphatidylethanolamine-based micelles and liposomes at lowered pH values, resulting in a cellular uptake that was similar to that of PEG-free NDDSs86.
Temperature-triggered drug delivery
Many pathological areas, such as tumours and inflamed areas, are hyperthermic68, which could be used as a possible trigger for stimuli-sensitive NDDSs. Alternatively, the tumour site could be heated from the outside to increase the size of pores within the microvasculature and increase blood flow, which results in an increased extravasation of drug-loaded NDDSs. Lipids with a suitable gel-to-liquid phase-transition temperature are usually used to prepare thermosensitive liposomes, such as dipalmitoylphosphatidylcholine or lysolipids. Indeed, temperature-sensitive lysolipid doxorubicin-loaded liposomes (named ThermoDox) have improved efficacy for liver cancer-targeted drug delivery in mice87,88 and have also been tested in human patients. Celsion, which developed Thermodox, recently reported a 57% improvement in overall survival when heat-activated liposomal doxorubicin in combination with radio-frequency ablation (RFA) was used in Phase III clinical trials to treat primary liver cancer (Celsion press release; see Further information). Temperature-sensitive NDDSs can also be prepared by incorporating polymers that have a lower physiological critical solution temperature (such as poly(N-isopropylacrylamide)) into the NDDS. In mice, it was shown that at temperatures above the low critical solution temperature, the polymer precipitates and causes disruption of the NDDSs to release the drug89.
Redox-triggered drug delivery
The difference in redox potential between normal and tumour tissues, and between the intracellular and extracellular environment, can also be exploited for drug delivery in cancer. For example, the concentration of glutathione in cancer cells is 100-to 1,000-fold higher than in the blood, and in a tumour mass the glutathione concentration is also markedly (100-fold) higher than the extracellular level of glutathione in normal tissue5. Reduction-sensitive liposomes that have two forms of disulphide-conjugated multifunctional lipids on their surface have been tested in a breast cancer cell line90. The cleavage of the disulphide bond resulted in the removal of the hydrophilic head group of the conjugate, membrane re-organization and the release of encapsulated calcein90. The disulphide bond has been widely used as the cleavable and/or reversible linker in NDDSs to confer redox sensitivity.
Enzyme-sensitive systems
The increased expression of certain local enzymes in cancer, such as MMPs, could be considered as a biomarker for disease diagnosis and prognosis, as well as a means for the delivery of pharmaceuticals via an enzyme-triggered mechanism91,92 (FIG. 2). Several substrates that are sensitive to MMPs have been designed for the delivery of drugs and as imaging agents. Cancer-associated proteases are another set of enzymes that are upregulated in tumours and can be used to develop enzyme-sensitive NDDSs. For instance, conjugates composed of cholesterol, peptide and poly-acrylic acid were cleaved by a cancer-associated protease (urokinase) and induced rapid drug release in an in vitro model93.
Magnetically sensitive systems
NDDSs that can be magnetized either by incorporating magnetite or prepared by direct modification of magnetized metal particles with biocompatible polymers could be used for specific targeting under an external magnetic field. Unlike ferromagnetic materials, magnetite or ferromagnetic particles that are less than 10 nm in diameter have a lower intensity of stray magnetic field, which reduces the potential health risks caused by magnetic fields94. These particles are referred to as SPIONs and can be surface-modified with various biocompatible compounds, such as dextran, to reduce their aggregation and increase their biocompatibility95.
SPIONs can be loaded into nanocarriers such as liposomes94, micelles96,97 or solid nanoparticles98,99 together with drugs and can increase drug localization in tumours under the exposure to a magnetic field. For example, liposomes co-loaded with methotrexate and SPION94 localized to tumours in mice. NDDSs containing SPIONs and a taxane drug could be additionally modified with PEG for longevity or with antibodies for tumour targeting96.
Control of NDDS functionalities with stimulus-sensitive moieties for enhanced targeting
Multifunctional NDDSs that combine stimulus-sensitive properties with another drug delivery approach could improve the therapeutic outcome in animal models and, hopefully, in future clinical applications86,94,100–103. The combined use of two different stimulus-sensitive approaches could be beneficial, as was shown for co-polymeric micelles that were sensitive to both pH and redox potential. For example, doxorubicin delivery to HepG2 tumour cells by these dual-sensitive NDDSs was more effective than with single-stimulus-sensitive control NDDSs104. Thermosensitive and magnetically sensitive liposomes loaded with methotrexate had more favourable drug pharmacokinetic properties (that is, better drug accumulation in skeletal muscle tissue in the tested animal model) than single-stimulus-sensitive delivery systems94. In addition, a multifunctional liposomal nanocarrier modified simultaneously with an antitumour monoclonal antibody (which actively targeted the tumour), a cell-penetrating peptide (which enabled intracellular delivery) and an MMP2-sensitive PEG–lipid conjugate (which facilitated MMP2-triggered PEG detachment from the lipid anchor) enhanced tumour targeting in vitro105.
Of all the stimuli considered above, pH and temperature (which can also be controlled by external factors) are the easiest to use among the intrinsic stimuli, whereas magnetic field and ultrasound — which are likely to be used clinically in the near future — are the external stimuli that are easiest to use. The use of redox condi-tions or local enzymatic activity still requires substantial synthetic efforts, whereas light-based approaches could be restricted primarily to superficial lesions unless fibre optics or near-infrared irradiation can be used.
Intracellular delivery and organelle targeting
After reaching the target, NDDSs may still need to cross the barrier of the cell membrane to deliver their drug load into specific organelles within the cytoplasm. Several strategies to prevent lysosomal degradation following the cellular internalization of NDDSs have been described106, including the use of targeting and cell-penetrating moieties as well as agents that can destabilize the lysosomal membrane, such as fusogenic lipids and pore-forming proteins107.
Cell-penetrating peptides are able to internalize nanosized particles, including liposomes, into cells108–110. Complexes of HIV TAT peptide (TATp)–liposomes and a plasmid encoding green fluorescence protein (pGFP) were used for successful in vitro transfection of several tumour and normal cells, as well as for the in vivo transfection of Lewis lung carcinoma tumour cells in mice111. Octa-arginine-modified, bleomycin- or doxorubicin-loaded liposomes demonstrated good intracellular penetration and strong inhibition of tumour growth in murine models112,113.
To provide intracellular drug delivery, the cell-penetrating function should be shielded — for example, under a PEG coating — until the NDDS is inside the target cell (where PEG is cleaved by local conditions)5,86. NDDSs such as targeted long-circulating pegylated liposomes and PEG–phosphatidylethanolamine-based micelles that possess several functionalities86,114 have been described. A pegylated TATp-modified pGFP-loaded liposomal preparation that had a PEG coating that detached at a lowered pH provided highly efficient transfection of tumour cells in vivo115. The potential therapeutic use of this approach was demonstrated in mice bearing ovarian cancer xenografts using a liposomal system that exposed a hidden cell-penetrating peptide (TATp) upon removal of PEG by the lower pH environment inside the tumour116,117.
Other micellar-based NDDSs were constructed using degradable ε-caprolactone-based co-polymers; the func-tional group on the co-polymer was used to incorporate siRNA against multidrug resistance protein 1 (MDR1; also known as ABCB1) or doxorubicin118. These micelles were also modified with the integrin-specific RGD4C peptide for cancer targeting and with the cell-penetrating TATp. Fluorescently labelled micelles were effectively taken up by cells and they improved drug delivery into cell nuclei, resulting in enhanced cytotoxicity in a mouse tumour model118.
However, delivering drugs or drug-loaded NDDSs inside cells may not be sufficient to achieve the maximum therapeutic response, and can even result in increased off-target effects. As such, the delivery of drug-loaded NDDSs directly to the organelle of interest could maximize the intended effect. This requires developing NDDSs that combine longevity, targetability and organelle recognition.
As mitochondrial dysfunction has been linked to many diseases, including cancer119, several strategies including the incorporation of the lipophilic cation rhodamine 123 to target NDDSs to mitochondria have been described120. Cell lysosomes have been targeted with NDDSs modified with octadecyl-rhodamine B121. Cytotoxic ceramides have been delivered to lysosomes of cancer cells using transferrin-modified liposomes, which resulted in reduced tumour growth in mice bearing an ovarian carcinoma xenograft66. Rhodamine B-modified fusogenic liposomes have also been used to deliver glucocerebrosidase into the mitochondria of Gaucher’s-type cells with low glucocerebrosidase activity122. Glucocerebrosidase is an enzyme that is deficient in patients with Gaucher’s disease, and so this type of NDDS is of particular interest for the treatment of lysosomal storage diseases122.
NDDSs for multimodal imaging and theranostics
Currently used medical imaging modalities include γ-scintigraphy, MRI, computed tomography and ultra-sonography, together with some modifications of these methods. Because each modality has its own advantages and limitations, it is highly desirable to have more than one type of reporter group associated with the same NDDS. Multifunctional NDDSs have been constructed for multimodal imaging, which could overcome various problems associated with individual imaging modalities, such as insufficient sensitivity or resolution123. With this in mind, several NDDSs that combine optical imaging with computed tomography or positron emission tomography (PET), or combine PET with computed tomography have been developed; these systems enable higher resolution and can be based on traditional NDDSs, such as liposomes or polymeric micelles, or they can use template nanoparticles with intrinsic contrast properties (such as gold or iron oxide nanoparticles, or quantum dots), which could be additionally modified with contrast moieties for other imaging modalities.
Thus, iron-oxide-based nanoparticles have been modified using click chemistry with a near-infrared dye to yield a dual MRI–near-infrared contrast agent124. Pegylated liposomes co-loaded with iohexol (a computed tomography imaging agent) and gadoteridol (a Gd-containing agent for MRI) had a long circulation lifetime and enabled simultaneous enhancement of computed tomography and magnetic resonance signals in mice and rabbits125. Dual-mode computed tomography–MRI imaging in rats and mice was achieved using multifunctional Gd-loaded dendrimer-entrapped gold nanoparticles126. Simultaneous optical imaging, computed tomography imaging and MRI was made possible using liposomes labelled with a fluorophore tracer, 99mTc, 111In or 64Cu and Gd127,128 in mouse models. Moreover, the addition of a radionuclide129 enables the imaging system to become a therapeutic. The use of polychelating amphiphilic polymers, which enable the attachment of many reporter metal atoms and can be incorporated or absorbed onto the nanocarrier, enabled a marked increase in the number of bound reporter metal atoms per particle and image-signal intensity130. In mouse models, such preparations can be targeted to tumours with a cancer-specific mAb with rapid and specific tumour accumulation and could serve as effective contrast agents for MRI of tumours131.
A relatively novel development in the area of multi-functional NDDSs is the use of so-called theranostics; that is, the simultaneous use of pharmaceutical NDDSs for diagnostic and/or imaging purposes together with therapeutic use. Through the use of contrast reporter moieties, theranostics enable real-time monitoring of the biodistribution and target accumulation of NDDSs. Theranostics often use liposomes, polymeric micelles, dendrimers and iron oxide nanoparticles as the carrier component of NDDSs, and heavy metal atoms (such as 111 In, 99m Tc, Mn and Gd) as contrast moieties for γ-scintigraphy and MRI132,133. For example, liposomes co-loaded with quantum dots and the dopamine agonist apomorphine had increased uptake into the brains of mice (apomorphine accumulation in the brain was increased by 2.4-fold) and enabled fluorescent brain imaging134. Multifunctional receptor-targeted nano-complexes containing a neurotensin-targeting peptide, DNA, a fluorophore and Gd have been used for brain imaging combined with DNA delivery in rats135.
Multifunctional core-shell polymeric nanoparticles composed of a poly(lactic-co-glycolic acid) core and a positively charged glycol-chitosan shell and co-loaded with DNA and quantum dots enabled transdermal DNA delivery and transfection of epidermal Langerhans cells in mice, and allowed the migration of target cells to be monitored136. Long-circulating pegylated liposomes loaded with doxorubicin and additionally decorated with a tumour-specific antibody and contrast moieties137,138 had increased therapeutic activity in vivo, and their target accumulation could be easily followed by γ-scintigraphy or MRI.
Iron-oxide-based NDDSs, which combine magnetic drug targeting and MRI, have attracted attention in recent years. SPIONs (which are popular MRI imaging agents) are frequently combined with therapeutic agents139 and PEG for longevity. For example, chlorotoxin-conjugated iron oxide nanoparticles delivered therapeutic methotrexate and an MRI contrast agent to 9L glioma xenografts in mice140. Magnetic particles modified with a recombinant peptide containing the amino-terminal fragment of urokinase-type plasminogen activator (uPA) can target tumours overexpressing uPA receptors, which enabled enhanced imaging and delivery in mice141. A targeted theranostic NDDS was prepared by covalent attachment of a near-infrared imaging agent and a translocation peptide to magnetic nanoparticles co-loaded with siRNA and was used for multimodal tumour imaging and to monitor the silencing activity of siRNA in tumour models142,143. Furthermore, hydrophobic photosensitizers (such as protoporphyrin IX) were loaded into pH-sensitive PEG–poly(β-amino ester)block co-polymer micelles for simultaneous tumour imaging and photodynamic therapy in mice144. A pegylated, siRNA-containing, magnetic-resonance-contrast liposome-based NDDS that contained fluorescent labels for histology downregulated the expression of survivin and inhibited tumour growth in xenografted tumours in mice145. In addition, pegylated liposomes that were loaded with Gd(III) for MRI, siRNA against survivin for tumour therapy, and additionally labelled with rhodamine–PE (phosphatidylethanolamine) for fluorescent detection have been studied in mice145.
Targeting of theranostic NDDSs provides an additional advantage, as was shown for the co-delivery of Gd and doxorubicin in liposomes targeted with a peptide specific for a neural cell adhesion molecule, which resulted in higher drug concentration in tumour tissues, increased inhibition of tumour growth and enhanced MRI visualization of Kaposi’s tumours in mice146. Antibody-mediated targeting of liposomes co-loaded with iron oxide and doxorubicin to pancreatic tumours in mice enhanced both the antitumour activity and the tumour magnetic resonance signal compared with untargeted liposomes147. The combination of a chemotherapeutic drug and a contrast agent on the same NDDS facilitates the development of personalized nanotherapeutic approaches because the efficiency of nanocarrier accumulation in the tumour (which is determined by the leakiness of the blood vessels and traced by a technique that uses contrast, such as mammography) can assist in the determination of the correct dose of the therapeutic agent for the treatment of each individual tumour148,149.
NDDSs for combination therapy
Drug combinations that can be delivered by NDDSs may be useful to combat drug resistance in patients with cancer150. A targeted liposome-polycation-hyaluronic acid NDDS that co-delivered three different siRNAs and one miRNA (to downregulate proliferation pathways, angio-genesis and the cellular defence against apoptosis) into tumours resulted in an 80% decrease in tumour size in a mouse model of melanoma151. Pegylated liposomes modified with trilysinoyl oleyamide have been used to co-deliver myeloid cell leukaemia 1 (MCL1)-specific siRNA and the histone deacetylase inhibitor suberoxy-lanilide hydroxamic acid into tumours, which resulted in a greater inhibition of tumour growth in mice bearing KB (human cervical cancer) xenografts152.
Similarly, liposomes co-loaded with doxorubicin and DNA encoding a dominant mutant form of survivin and targeted to tumours had enhanced antitumour activity in a murine model of Lewis lung carcinoma153,154. Peptide-targeted liposomes loaded with doxorubicin or cisplatin together with oligonucleotides against the molecules involved in two main drug resistance mechanisms, B cell lymphoma 2 (BCL-2) and MDR1 (multidrug-resistance protein 1), had high efficacy in human ovarian cancer xenografts155. Moreover, a combination of the colorectal cancer drug irinotecan and 5-fluoroorotic acid in pegylated liposomes (at a 5:1 ratio) had synergistic effects and had higher therapeutic efficacy than did the free drug mixtures in animal models, including KB-tumour-bearing mice156,157. For example, in a Phase I clinical trial, liposomes loaded with irinotecan and floxuridine liposomes (in a 1:1 molar ratio) were well tolerated and had antitumour activity in patients with advanced colorectal cancer, whereby 13 out of 15 patients responded to therapy158. The drug is currently in Phase II (TABLE 1).
Challenges in developing multifunctional NDDSs
When developing multifunctional and stimuli-sensitive NDDSs, one has to keep in mind that the different NDDS-attached functions may affect the biological activity of those NDDSs differently. Thus, although targeted ligands can result in improved cellular uptake, the surface properties, size and shape of the NDDSs will define their pharmacokinetics and biodistribution. Interestingly, some studies159,160 have demonstrated that the use of targeting ligands (that is, antibodies) does not necessarily increase the accumulation of NDDSs in the target area (with tumours as an example) when compared with EPR-mediated accumulation. Instead, the targeting ligand may enhance intracellular drug delivery in situations in which an internalizable ligand was used159,160, which could be beneficial for drugs that act intracellularly. It is also important to bear in mind that many surface-attached functions (most notably targeting moieties) could compromise the increased longevity of NDDSs that is imparted by pegylation; the surface density of such ligands should be closely monitored to provide a desirable targeting effect without overly compromising longevity.
I have mainly considered findings from early preclinical studies in this Review. The question then arises as to why, with so many interesting and impressive data, there still seems to be a long and arduous journey to bring these promising preclinical results into clinical practice? Potential answers to this question have been analysed in several recent publications161–164. Based on these discussions, one can first of all note that many data obtained in animal models cannot be easily translated into humans. This is particularly important in cancer research, in which subcutaneous tumour xenografts still represent the most frequently used model for targeted cancer therapy. Effective tumour targeting requires a sufficient number of productive contacts to be made between the targeted NDDSs and the target cells, which, in turn, requires effective preliminary accumulation of these NDDSs in the tumour via the EPR effect. In humans, this process is much more heterogeneous than in animal models because of a high heterogeneity in tumour blood flow. It is particularly problematic for animal models of subcutaneous tumours, in which the access of the blood to the tumour interstitium is greater than it is in solid tumours in patients. Unfortunately, the situation is even less clear with models of other non-cancer diseases.
In addition, there is ongoing discussion as to whether passive or active targeting will be more beneficial for various potential therapeutic indications. Nevertheless, the current thinking suggests that passive spontaneous accumulation of long-circulating NDDSs in tumours should be sufficient for drug delivery into the tumour mass, whereas intracellular drug delivery could be more effective if NDDSs are supplemented with specific targeting moieties that recognize cell-surface ligands to promote the internalization of drug-loaded NDDSs. Moreover, many experimental models of various human diseases are not uniformly standardized, which often makes the comparison of results difficult. From a technological point of view, many of the effective and experimentally elegant NDDSs are difficult to reproducibly scale up in the industrial setting to produce NDDSs on a commercial scale because of their complexity, which will also add substantially to the final price of the product.
Assuming the problems described above are eventu-ally resolved, the translation of the current knowledge into clinical applications will require the active involvement of pharmaceutical and biotechnology companies and an increased understanding of the benefits of NDDSs by the broad clinical community. Once more clinical data become available, multifunctional, stimuli-sensitive and theranostic NDDSs will continue to be developed and improved. To become a successful product, such NDDSs should be reasonably simple. That is, their preparation should not require complex multistep processes, should not include uncommon or expensive constituents, and they should preferably be made of components that are generally recognized as safe. In the future, the scalability of NDDSs should not represent a problem and be preferably based on known and accepted processes and protocols. The final product should also be sufficiently stable under normal storage conditions and easy to use; that is, it should not require complex administration protocols or regimens. If these requirements are met, multifunctional, stimuli-sensitive and theranostic NDDSs could become an important component of personalized therapy in the near future.
Acknowledgements
The author acknowledges US National Institutes of Health grant U54CA151881 and tremendous help by T. Levchenko.
Glossary
- Enhanced permeability and retention (EPR) effect
The property through which macromolecules (such as nanoparticles) accumulate in areas of inflammation including tumours, owing to the increased vascular permeability or abnormal blood vessel architecture.
- Passive targeting
The mechanism through which nanoparticulate pharmaceutical drug delivery systems tend to accumulate in tumours, probably through the enhanced permeability and retention effect.
- Quantum dots
Nanometre-scale particles of semiconductor materials that have quantum mechanical properties.
- Active targeting
The mechanism through which specific moieties attached to nanoparticulate pharmaceutical drug delivery systems force them to interact with a specific type of cell or tissue.
- HIV TAT peptide
An amino acid sequence within the HIV transactivator of transcription (TAT) protein. This peptide promotes cell entry as it is a key part of a protein transduction domain.
- Theranostics
The simultaneous use of nanoparticulate pharmaceutical drug delivery systems for therapeutic as well as diagnostic and/or imaging purposes.
Footnotes
Competing interests statement
The author declares no competing interests.
References
- 1.Torchilin VP, editor. Nanoparticulates as Drug Carriers. Imperial College Press; 2006. [Google Scholar]
- 2.Thassu D, Deleers M. In: Nanoparticulate Drug Delivery Systems. Pathak Y, editor. Informa Healthcare USA; 2007. [Google Scholar]
- 3.Ferrari M. Cancer nanotechnology: opportunities and challenges. Nature Rev. Cancer. 2005;5:161–171. doi: 10.1038/nrc1566. [DOI] [PubMed] [Google Scholar]
- 4.van Vlerken LE, Amiji MM. Multi-functional polymeric nanoparticles for tumour-targeted drug delivery. Expert Opin. Drug Deliv. 2006;3:205–216. doi: 10.1517/17425247.3.2.205. [DOI] [PubMed] [Google Scholar]
- 5.Torchilin V. Multifunctional and stimuli-sensitive pharmaceutical nanocarriers. Eur. J. Pharm. Biopharm. 2009;71:431–444. doi: 10.1016/j.ejpb.2008.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hobbs SK, et al. Regulation of transport pathways in tumor vessels: role of tumor type and microenvironment. Proc. Natl Acad. Sci. USA. 1998;95:4607–4612. doi: 10.1073/pnas.95.8.4607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jain RK. Transport of molecules, particles, and cells in solid tumors. Annu. Rev. Biomed. Eng. 1999;1:241–263. doi: 10.1146/annurev.bioeng.1.1.241. [DOI] [PubMed] [Google Scholar]
- 8.Maeda H. Tumor-selective delivery of macromolecular drugs via the EPR effect: background and future prospects. Bioconjugate Chem. 2010;21:797–802. doi: 10.1021/bc100070g. [DOI] [PubMed] [Google Scholar]
- 9.Nagamitsu A, Greish K, Maeda H. Elevating blood pressure as a strategy to increase tumor-targeted delivery of macromolecular drug SMANCS: cases of advanced solid tumors. Jpn J. Clin. Oncol. 2009;39:756–766. doi: 10.1093/jjco/hyp074. [DOI] [PubMed] [Google Scholar]
- 10.Monsky WL, et al. Augmentation of transvascular transport of macromolecules and nanoparticles in tumors using vascular endothelial growth factor. Cancer Res. 1999;59:4129–4135. [PubMed] [Google Scholar]
- 11.Jain RK, Stylianopoulos T. Delivering nano-medicine to solid tumors. Nature Rev. Clin. Oncol. 2010;7:653–664. doi: 10.1038/nrclinonc.2010.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Klibanov AL, Maruyama K, Torchilin VP, Huang L. Amphipathic polyethyleneglycols effectively prolong the circulation time of liposomes. FEBS Lett. 1990;268:235–237. doi: 10.1016/0014-5793(90)81016-h. [DOI] [PubMed] [Google Scholar]
- 13.Ishida T, et al. Injection of PEGylated liposomes in rats elicits PEG-specific IgM, which is responsible for rapid elimination of a second dose of PEGylated liposomes. J. Control Release. 2006;112:15–25. doi: 10.1016/j.jconrel.2006.01.005. [DOI] [PubMed] [Google Scholar]
- 14.Ishida T, Atobe K, Wang X, Kiwada H. Accelerated blood clearance of PEGylated liposomes upon repeated injections: effect of doxorubicin-encapsulation and high-dose first injection. J. Control Release. 2006;115:251–258. doi: 10.1016/j.jconrel.2006.08.017. [DOI] [PubMed] [Google Scholar]
- 15.Whiteman KR, Subr V, Ulbrich K, Torchilin VP. Poly(HPMA)-coated liposomes demonstrate prolonged circulation in mice. J. Liposome Res. 2001;11:153–164. doi: 10.1081/LPR-100108459. [DOI] [PubMed] [Google Scholar]
- 16.Torchilin VP, et al. Amphiphilic poly-N-vinyl-pyrrolidones: synthesis, properties and liposome surface modification. Biomaterials. 2001;22:3035–3044. doi: 10.1016/s0142-9612(01)00050-3. [DOI] [PubMed] [Google Scholar]
- 17.Takeuchi H, Kojima H, Yamamoto H, Kawashima Y. Evaluation of circulation profiles of liposomes coated with hydrophilic polymers having different molecular weights in rats. J. Control Release. 2001;75:83–91. doi: 10.1016/s0168-3659(01)00368-6. [DOI] [PubMed] [Google Scholar]
- 18.Geng Y, et al. Shape effects of filaments versus spherical particles in flow and drug delivery. Nature Nanotechnol. 2007;2:249–255. doi: 10.1038/nnano.2007.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Maksimenko A, et al. A unique squalenoylated and nonpegylated doxorubicin nanomedicine with systemic long-circulating properties and anticancer activity. Proc. Natl Acad. Sci. USA. 2014;111:E217–E226. doi: 10.1073/pnas.1313459110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Niidome T, et al. PEG-modified gold nanorods with a stealth character for in vivo applications. J. Control. Release. 2006;114:343–347. doi: 10.1016/j.jconrel.2006.06.017. [DOI] [PubMed] [Google Scholar]
- 21.von Maltzahn G, et al. Computationally guided photothermal tumor therapy using long-circulating gold nanorod antennas. Cancer Res. 2009;69:3892–3900. doi: 10.1158/0008-5472.CAN-08-4242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kaminskas LM, et al. Pharmacokinetics and tumor disposition of PEGylated, methotrexate conjugated poly-l-lysine dendrimers. Mol. Pharm. 2009;6:1190–1204. doi: 10.1021/mp900049a. [DOI] [PubMed] [Google Scholar]
- 23.Wang W, et al. The decrease of PAMAM dendrimer-induced cytotoxicity by PEGylation via attenuation of oxidative stress. Nanotechnology. 2009;20:105103. doi: 10.1088/0957-4484/20/10/105103. [DOI] [PubMed] [Google Scholar]
- 24.Schipper ML, et al. Particle size, surface coating, and PEGylation influence the biodistribution of quantum dots in living mice. Small. 2009;5:126–134. doi: 10.1002/smll.200800003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sawant RR, Torchilin VP. Challenges in development of targeted liposomal therapeutics. AAPS J. 2012;14:303–315. doi: 10.1208/s12248-012-9330-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Trapani G, Denora N, Trapani A, Laquintana V. Recent advances in ligand targeted therapy. J. Drug Target. 2012;20:1–22. doi: 10.3109/1061186X.2011.611518. [DOI] [PubMed] [Google Scholar]
- 27.Torchilin VP, et al. p-nitrophenylcarbonyl-PEG-PE-liposomes: fast and simple attachment of specific ligands, including monoclonal antibodies, to distal ends of PEG chains via p-nitrophenylcarbonyl groups. Biochim. Biophys. Acta. 2001;1511:397–411. doi: 10.1016/s0005-2728(01)00165-7. [DOI] [PubMed] [Google Scholar]
- 28.Gao J, et al. Tumor-targeted PE38KDEL delivery via PEGylated anti-HER2 immunoliposomes. Int. J. Pharm. 2009;374:145–152. doi: 10.1016/j.ijpharm.2009.03.018. [DOI] [PubMed] [Google Scholar]
- 29.Elbayoumi TA, Torchilin VP. Tumor-specific anti-nucleosome antibody improves therapeutic efficacy of doxorubicin-loaded long-circulating liposomes against primary and metastatic tumor in mice. Mol. Pharm. 2009;6:246–254. doi: 10.1021/mp8001528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gupta B, Torchilin VP. Monoclonal antibody 2C5-modified doxorubicin-loaded liposomes with significantly enhanced therapeutic activity against intracranial human brain U-87 MG tumor xenografts in nude mice. Cancer Immunol. Immunother. 2007;56:1215–1223. doi: 10.1007/s00262-006-0273-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Eck W, et al. PEGylated gold nanoparticles conjugated to monoclonal F19 antibodies as targeted labeling agents for human pancreatic carcinoma tissue. ACS Nano. 2008;2:2263–2272. doi: 10.1021/nn800429d. [DOI] [PubMed] [Google Scholar]
- 32.Hu K, et al. Lactoferrin-conjugated PEG-PLA nanoparticles with improved brain delivery: in vitro and in vivo evaluations. J. Control. Release. 2009;134:55–61. doi: 10.1016/j.jconrel.2008.10.016. [DOI] [PubMed] [Google Scholar]
- 33.Le Droumaguet B, et al. Versatile and efficient targeting using a single nanoparticulate platform: application to cancer and Alzheimer’s disease. ACS Nano. 2012;6:5866–5879. doi: 10.1021/nn3004372. [DOI] [PubMed] [Google Scholar]
- 34.Kang H, O’Donoghue MB, Liu H, Tan W. A liposome-based nanostructure for aptamer directed delivery. Chem. Commun. 2010;46:249–251. doi: 10.1039/b916911c. [DOI] [PubMed] [Google Scholar]
- 35.Kim IY, et al. Antitumor activity of EGFR targeted pH-sensitive immunoliposomes encapsulating gemcitabine in A549 xenograft nude mice. J. Control. Release. 2009;140:55–60. doi: 10.1016/j.jconrel.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 36.Yang X, Grailer JJ, Pilla S, Steeber DA, Gong S. Tumor-targeting, pH-responsive, and stable unimolecular micelles as drug nanocarriers for targeted cancer therapy. Bioconjug. Chem. 2010;21:296–504. doi: 10.1021/bc900422j. [DOI] [PubMed] [Google Scholar]
- 37.Shen M, et al. Multifunctional drug delivery system for targeting tumor and its acidic microenvironment. J. Control. Release. 2012;161:884–892. doi: 10.1016/j.jconrel.2012.05.013. [DOI] [PubMed] [Google Scholar]
- 38.Binsalamah ZM, Paul A, Prakash S, Shum-Tim D. Nanomedicine in cardiovascular therapy: recent advancements. Expert Rev. Cardiovasc. Ther. 2012;10:805–815. doi: 10.1586/erc.12.41. [DOI] [PubMed] [Google Scholar]
- 39.Psarros C, Lee R, Margaritis M, Antoniades C. Nanomedicine for the prevention, treatment and imaging of atherosclerosis. Nanomedicine. 2012;8(Suppl. 1):59–68. doi: 10.1016/j.nano.2012.05.006. [DOI] [PubMed] [Google Scholar]
- 40.Peters D, et al. Targeting atherosclerosis by using modular, multifunctional micelles. Proc. Natl Acad. Sci. USA. 2009;106:9815–9819. doi: 10.1073/pnas.0903369106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Iverson NM, Sparks SM, Demirdirek B, Uhrich KE, Moghe PV. Controllable inhibition of cellular uptake of oxidized low-density lipoprotein: structure-function relationships for nanoscale amphiphilic polymers. Acta Biomater. 2010;6:3081–3091. doi: 10.1016/j.actbio.2010.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Broz P, et al. Inhibition of macrophage phagocytotic activity by a receptor-targeted polymer vesicle-based drug delivery formulation of pravastatin. J. Cardiovasc. Pharmacol. 2008;51:246–252. doi: 10.1097/FJC.0b013e3181624aed. [DOI] [PubMed] [Google Scholar]
- 43.Mulder WJ, et al. Molecular imaging of macrophages in atherosclerotic plaques using bimodal PEG-micelles. Magn. Reson. Med. 2007;58:1164–1170. doi: 10.1002/mrm.21315. [DOI] [PubMed] [Google Scholar]
- 44.Sy JC, Davis ME. Delivering regenerative cues to the heart: cardiac drug delivery by microspheres and peptide nanofibers. J. Cardiovasc. Transl. Res. 2010;3:461–468. doi: 10.1007/s12265-010-9210-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bowey K, Tanguay JF, Tabrizian M. Liposome technology for cardiovascular disease treatment and diagnosis. Expert Opin. Drug Deliv. 2012;9:249–265. doi: 10.1517/17425247.2012.647908. [DOI] [PubMed] [Google Scholar]
- 46.Levchenko TS, Hartner WC, Verma DD, Bernstein EA, Torchilin VP. ATP-loaded liposomes for targeted treatment in models of myocardial ischemia. Methods Mol. Biol. 2010;605:361–375. doi: 10.1007/978-1-60327-360-2_25. [DOI] [PubMed] [Google Scholar]
- 47.Verma DD, Hartner WC, Thakkar V, Levchenko TS, Torchilin VP. Protective effect of coenzyme Q10-loaded liposomes on the myocardium in rabbits with an acute experimental myocardial infarction. Pharm. Res. 2007;24:2131–2137. doi: 10.1007/s11095-007-9334-0. [DOI] [PubMed] [Google Scholar]
- 48.Guo Y, et al. Simultaneous diagnosis and gene therapy of immuno-rejection in rat allogeneic heart transplantation model using a T-cell-targeted theranostic nanosystem. ACS Nano. 2012;6:10646–10657. doi: 10.1021/nn3037573. [DOI] [PubMed] [Google Scholar]
- 49.McCarthy JR, et al. Multifunctional nanoagent for thrombus-targeted fibrinolytic therapy. Nanomed. 2012;7:1017–1028. doi: 10.2217/nnm.11.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mehendale R, Joshi M, Patravale VB. Nanomedicines for treatment of viral diseases. Crit. Rev. Ther. Drug Carrier Syst. 2013;30:1–49. doi: 10.1615/critrevtherdrugcarriersyst.2013005469. [DOI] [PubMed] [Google Scholar]
- 51.Banerjee M, Mallick S, Paul A, Chattopadhyay A, Ghosh SS. Heightened reactive oxygen species generation in the antimicrobial activity of a three component iodinated chitosan-silver nanoparticle composite. Langmuir. 2010;26:5901–5908. doi: 10.1021/la9038528. [DOI] [PubMed] [Google Scholar]
- 52.Mihu MR, et al. The use of nitric oxide releasing nanoparticles as a treatment against Acinetobacter baumannii in wound infections. Virulence. 2010;1:62–67. doi: 10.4161/viru.1.2.10038. [DOI] [PubMed] [Google Scholar]
- 53.Seleem MN, et al. Silica-antibiotic hybrid nanoparticles for targeting intracellular pathogens. Antimicrob. Agents Chemother. 2009;53:4270–4274. doi: 10.1128/AAC.00815-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Xiong MH, et al. Bacteria-responsive multifunctional nanogel for targeted antibiotic delivery. Adv. Mater. 2012;24:6175–6180. doi: 10.1002/adma.201202847. [DOI] [PubMed] [Google Scholar]
- 55.Low PS, Henne WA, Doorneweerd DD. Discovery and development of folic-acid-based receptor targeting for imaging and therapy of cancer and inflammatory diseases. Acc. Chem. Res. 2008;41:120–129. doi: 10.1021/ar7000815. [DOI] [PubMed] [Google Scholar]
- 56.Lu Y, Low PS. Folate-mediated delivery of macromolecular anticancer therapeutic agents. Adv. Drug Deliv. Rev. 2002;54:675–693. doi: 10.1016/s0169-409x(02)00042-x. [DOI] [PubMed] [Google Scholar]
- 57.Gabizon A, Shmeeda H, Horowitz AT, Zalipsky S. Tumor cell targeting of liposome-entrapped drugs with phospholipid-anchored folic acid-PEG conjugates. Adv. Drug Deliv. Rev. 2004;56:1177–1192. doi: 10.1016/j.addr.2004.01.011. [DOI] [PubMed] [Google Scholar]
- 58.Lee RJ, Low PS. Folate-mediated tumor cell targeting of liposome-entrapped doxorubicin in vitro. Biochim. Biophys. Acta. 1995;1233:134–144. doi: 10.1016/0005-2736(94)00235-h. [DOI] [PubMed] [Google Scholar]
- 59.Liu Y, et al. Synthesis and evaluation of a novel lipophilic folate receptor targeting ligand. Anticancer Res. 2011;31:1521–1525. [PubMed] [Google Scholar]
- 60.Niu R, et al. Preparation, characterization, and antitumor activity of paclitaxel-loaded folic acid modified and TAT peptide conjugated PEGylated polymeric liposomes. J. Drug Target. 2011;19:373–381. doi: 10.3109/1061186X.2010.504266. [DOI] [PubMed] [Google Scholar]
- 61.Chaudhury A, Das S, Bunte RM, Chiu GN. Potent therapeutic activity of folate receptor-targeted liposomal carboplatin in the localized treatment of intraperitoneally grown human ovarian tumor xenograft. Int. J. Nanomed. 2012;7:739–751. doi: 10.2147/IJN.S26172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Duarte S, Faneca H, Lima MC. Folate-associated lipoplexes mediate efficient gene delivery and potent antitumoral activity in vitro and in vivo. Int. J. Pharm. 2012;423:365–377. doi: 10.1016/j.ijpharm.2011.12.035. [DOI] [PubMed] [Google Scholar]
- 63.Li X, Ding L, Xu Y, Wang Y, Ping Q. Targeted delivery of doxorubicin using stealth liposomes modified with transferrin. Int. J. Pharm. 2009;373:116–123. doi: 10.1016/j.ijpharm.2009.01.023. [DOI] [PubMed] [Google Scholar]
- 64.Cheng KT, Wang PC, Shan L. Alexa Fluor 680-labeled transferrin-cationic (NBD-labeled DOPE-DOTAP) liposome-encapsulated gadopentetate dimeglumine complex. MICAD. 2007 [online], http://www.ncbi.nlm.nih.gov/books/NBK23470/ [PubMed]
- 65.Ito Y, et al. Disposition of TF-PEG-Liposome-BSH in tumor-bearing mice. Appl. Radiat. Isot. 2009;67:S109–110. doi: 10.1016/j.apradiso.2009.03.018. [DOI] [PubMed] [Google Scholar]
- 66.Koshkaryev A, Piroyan A, Torchilin VP. Increased apoptosis in cancer cells in vitro and in vivo by ceramides in transferrin-modified liposomes. Cancer Biol. Ther. 2012;13:50–60. doi: 10.4161/cbt.13.1.18871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kim SK, Huang L. Nanoparticle delivery of a peptide targeting EGFR signaling. J. Control. Release. 2012;157:279–286. doi: 10.1016/j.jconrel.2011.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Danhier F, Feron O, Preat V. To exploit the tumor microenvironment: passive and active tumor targeting of nanocarriers for anti-cancer drug delivery. J. Control. Release. 2010;148:135–146. doi: 10.1016/j.jconrel.2010.08.027. [DOI] [PubMed] [Google Scholar]
- 69.Chiu GNC, et al. Modulation of cancer cell survival pathways using multivalent liposomal therapeutic antibody constructs. Mol. Cancer Ther. 2007;6:844–855. doi: 10.1158/1535-7163.MCT-06-0159. [DOI] [PubMed] [Google Scholar]
- 70.Gabizon A, et al. Improved therapeutic activity of folate-targeted liposomal doxorubicin in folate receptor-expressing tumor models. Cancer Chemother. Pharmacol. 2010;66:43–52. doi: 10.1007/s00280-009-1132-4. [DOI] [PubMed] [Google Scholar]
- 71.Byrne JD, Betancourt T, Brannon-Peppas L. Active targeting schemes for nanoparticle systems in cancer therapeutics. Adv. Drug Deliv. Rev. 2008;60:1615–1626. doi: 10.1016/j.addr.2008.08.005. [DOI] [PubMed] [Google Scholar]
- 72.Wicki A, et al. Targeting tumor-associated endothelial cells: anti-VEGFR2 immunoliposomes mediate tumor vessel disruption and inhibit tumor growth. Clin. Cancer Res. 2012;18:454–464. doi: 10.1158/1078-0432.CCR-11-1102. [DOI] [PubMed] [Google Scholar]
- 73.Li SD, Chono S, Huang L. Efficient oncogene silencing and metastasis inhibition via systemic delivery of siRNA. Mol. Ther. 2008;16:942–946. doi: 10.1038/mt.2008.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Chang DK, et al. Antiangiogenic targeting liposomes increase therapeutic efficacy for solid tumors. J. Biol. Chem. 2009;284:12905–12916. doi: 10.1074/jbc.M900280200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Gosk S, Moos T, Gottstein C, Bendas G. VCAM-1 directed immunoliposomes selectively target tumor vasculature in vivo. Biochim. Biophys. Acta. 2008;1778:854–863. doi: 10.1016/j.bbamem.2007.12.021. [DOI] [PubMed] [Google Scholar]
- 76.Hatakeyama H, et al. Tumor targeting of doxorubicin by anti-MT1-MMP antibody-modified PEG liposomes. Int. J. Pharm. 2007;342:194–200. doi: 10.1016/j.ijpharm.2007.04.037. [DOI] [PubMed] [Google Scholar]
- 77.Mura S, Nicolas J, Couvreur P. Stimuli-responsive nanocarriers for drug delivery. Nature Mater. 2013;12:991–1003. doi: 10.1038/nmat3776. [DOI] [PubMed] [Google Scholar]
- 78.Helmlinger G, Sckell A, Dellian M, Forbes NS, Jain RK. Acid production in glycolysis-impaired tumors provides new insights into tumor metabolism. Clin. Cancer Res. 2002;8:1284–1291. [PubMed] [Google Scholar]
- 79.Wojtkowiak JW, Verduzco D, Schramm KJ, Gillies RJ. Drug resistance and cellular adaptation to tumor acidic pH microenvironment. Mol. Pharm. 2011;8:2032–2038. doi: 10.1021/mp200292c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lee ES, Shin HJ, Na K, Bae YH. Poly(L-histidine)-PEG block copolymer micelles and pH-induced destabilization. J. Control. Release. 2003;90:363–374. doi: 10.1016/s0168-3659(03)00205-0. [DOI] [PubMed] [Google Scholar]
- 81.Kim D, Lee ES, Oh KT, Gao ZG, Bae YH. Doxorubicin-loaded polymeric micelle overcomes multidrug resistance of cancer by double-targeting folate receptor and early endosomal pH. Small. 2008;4:2043–2050. doi: 10.1002/smll.200701275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kim D, Gao ZG, Lee ES, Bae YH. In vivo evaluation of doxorubicin-loaded polymeric micelles targeting folate receptors and early endosomal pH in drug-resistant ovarian cancer. Mol. Pharm. 2009;6:1353–1362. doi: 10.1021/mp900021q. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Farhood H, Serbina N, Huang L. The role of dioleoyl phosphatidylethanolamine in cationic liposome mediated gene transfer. Biochim. Biophys. Acta. 1995;1235:289–295. doi: 10.1016/0005-2736(95)80016-9. [DOI] [PubMed] [Google Scholar]
- 84.Sawant RR, et al. Polyethyleneimine-lipid conjugate-based pH-sensitive micellar carrier for gene delivery. Biomaterials. 2012;33:3942–3951. doi: 10.1016/j.biomaterials.2011.11.088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Navarro G, et al. P-glycoprotein silencing with siRNA delivered by DOPE-modified PEI overcomes doxorubicin resistance in breast cancer cells. Nanomed. 2012;7:65–78. doi: 10.2217/nnm.11.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Sawant RM, et al. “SMART” drug delivery systems: double-targeted pH-responsive pharmaceutical nanocarriers. Bioconjug Chem. 2006;17:943–949. doi: 10.1021/bc060080h. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Needham D, Park JY, Wright AM, Tong J. Materials characterization of the low temperature sensitive liposome (LTSL): effects of the lipid composition (lysolipid and DSPE-PEG2000) on the thermal transition and release of doxorubicin. Faraday Discuss. 2013;161:515–534. doi: 10.1039/c2fd20111a. discussion 563–589. [DOI] [PubMed] [Google Scholar]
- 88.Chen KJ, et al. Hyperthermia-mediated local drug delivery by a bubble-generating liposomal system for tumor-specific chemotherapy. ACS Nano. 2014;8:5105–5115. doi: 10.1021/nn501162x. [DOI] [PubMed] [Google Scholar]
- 89.Schwerdt A, et al. Hyperthermia-induced targeting of thermosensitive gene carriers to tumors. Hum. Gene Ther. 2008;19:1283–1292. doi: 10.1089/hum.2008.064. [DOI] [PubMed] [Google Scholar]
- 90.Goldenbogen B, et al. Reduction-sensitive liposomes from a multifunctional lipid conjugate and natural phospholipids: reduction and release kinetics and cellular uptake. Langmuir. 2011;27:10820–10829. doi: 10.1021/la201160y. [DOI] [PubMed] [Google Scholar]
- 91.Meers P. Enzyme-activated targeting of liposomes. Adv. Drug Deliv. Rev. 2001;53:265–272. doi: 10.1016/s0169-409x(01)00205-8. [DOI] [PubMed] [Google Scholar]
- 92.Gialeli C, Theocharis AD, Karamanos NK. Roles of matrix metalloproteinases in cancer progression and their pharmacological targeting. FEBS J. 2011;278:16–27. doi: 10.1111/j.1742-4658.2010.07919.x. [DOI] [PubMed] [Google Scholar]
- 93.Basel MT, Shrestha TB, Troyer DL, Bossmann SH. Protease-sensitive, polymer-caged liposomes: a method for making highly targeted liposomes using triggered release. ACS Nano. 2011;5:2162–2175. doi: 10.1021/nn103362n. [DOI] [PubMed] [Google Scholar]
- 94.Zhu L, et al. Targeted delivery of methotrexate to skeletal muscular tissue by thermosensitive magnetoliposomes. Int. J. Pharm. 2009;370:136–143. doi: 10.1016/j.ijpharm.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 95.Wang FH, et al. Diffusion and clearance of superparamagnetic iron oxide nanoparticles infused into the rat striatum studied by MRI and histochemical techniques. Nanotechnology. 2011;22:015103. doi: 10.1088/0957-4484/22/1/015103. [DOI] [PubMed] [Google Scholar]
- 96.Sawant RM, et al. Nanosized cancer cell-targeted polymeric immunomicelles loaded with superparamagnetic iron oxide nanoparticles. J. Nanoparticle Res. 2009;11:1777–1785. [Google Scholar]
- 97.Liao C, Sun Q, Liang B, Shen J, Shuai X. Targeting EGFR-overexpressing tumor cells using cetuximab-immunomicelles loaded with doxorubicin and superparamagnetic iron oxide. Eur. J. Radiol. 2011;80:699–705. doi: 10.1016/j.ejrad.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 98.Lee JH, et al. Exchange-coupled magnetic nanoparticles for efficient heat induction. Nature Nanotechnol. 2011;6:418–422. doi: 10.1038/nnano.2011.95. [DOI] [PubMed] [Google Scholar]
- 99.Xie J, Liu G, Eden HS, Ai H, Chen X. Surface- engineered magnetic nanoparticle platforms for cancer imaging and therapy. Acc. Chem. Res. 2011;44:883–892. doi: 10.1021/ar200044b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Zhu L, Ye Z, Cheng K, Miller DD, Mahato RI. Site-specific delivery of oligonucleotides to hepatocytes after systemic administration. Bioconjug. Chem. 2008;19:290–298. doi: 10.1021/bc070126m. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Zhu L, Mahato RI. Targeted delivery of siRNA to hepatocytes and hepatic stellate cells by bioconjugation. Bioconjug Chem. 2010;21:2119–2127. doi: 10.1021/bc100346n. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Yudina A, et al. Ultrasound-mediated intracellular drug delivery using microbubbles and temperature- sensitive liposomes. J. Control. Release. 2011;155:442–448. doi: 10.1016/j.jconrel.2011.06.006. [DOI] [PubMed] [Google Scholar]
- 103.Kang H, et al. Near-infrared light-responsive core-shell nanogels for targeted drug delivery. ACS Nano. 2011;5:5094–5099. doi: 10.1021/nn201171r. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Chen J, et al. pH and reduction dual-sensitive copolymeric micelles for intracellular doxorubicin delivery. Biomacromolecules. 2011;12:3601–3611. doi: 10.1021/bm200804j. [DOI] [PubMed] [Google Scholar]
- 105.Zhu L, Kate P, Torchilin VP. Matrix metalloprotease 2-responsive multifunctional liposomal nanocarrier for enhanced tumor targeting. ACS Nano. 2012;6:3491–3498. doi: 10.1021/nn300524f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Wang T, Upponi JR, Torchilin VP. Design of multifunctional non-viral gene vectors to overcome physiological barriers: dilemmas and strategies. Int. J. Pharm. 2012;427:3–20. doi: 10.1016/j.ijpharm.2011.07.013. [DOI] [PubMed] [Google Scholar]
- 107.Sasaki K, et al. An artificial virus-like nano carrier system: enhanced endosomal escape of nanoparticles via synergistic action of pH-sensitive fusogenic peptide derivatives. Anal. Bioanal Chem. 2008;391:2717–2727. doi: 10.1007/s00216-008-2012-1. [DOI] [PubMed] [Google Scholar]
- 108.Josephson L, Tung CH, Moore A, Weissleder R. High-efficiency intracellular magnetic labeling with novel superparamagnetic-Tat peptide conjugates. Bioconjug. Chem. 1999;10:186–191. doi: 10.1021/bc980125h. [DOI] [PubMed] [Google Scholar]
- 109.Torchilin VP, Rammohan R, Weissig V, Levchenko TS. TAT peptide on the surface of liposomes affords their efficient intracellular delivery even at low temperature and in the presence of metabolic inhibitors. Proc. Natl Acad. Sci. USA. 2001;98:8786–8791. doi: 10.1073/pnas.151247498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Tseng YL, Liu JJ, Hong RL. Translocation of liposomes into cancer cells by cell-penetrating peptides penetratin and tat: a kinetic and efficacy study. Mol. Pharmacol. 2002;62:864–872. doi: 10.1124/mol.62.4.864. [DOI] [PubMed] [Google Scholar]
- 111.Torchilin VP, et al. Cell transfection in vitro and in vivo with nontoxic TAT peptide-liposome-DNA complexes. Proc. Natl Acad. Sci. USA. 2003;100:1972–1977. doi: 10.1073/pnas.0435906100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Koshkaryev A, Piroyan A, Torchilin VP. Bleomycin in octaarginine-modified fusogenic liposomes results in improved tumor growth inhibition. Cancer Lett. 2013;334:293–301. doi: 10.1016/j.canlet.2012.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Biswas S, Dodwadkar NS, Deshpande PP, Parab S, Torchilin VP. Surface functionalization of doxorubicin-loaded liposomes with octa-arginine for enhanced anticancer activity. Eur. J. Pharm. Biopharm. 2013;84:517–525. doi: 10.1016/j.ejpb.2012.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Kale AA, Torchilin VP. Design, synthesis, and characterization of pH-sensitive PEG-PE conjugates for stimuli-sensitive pharmaceutical nanocarriers: the effect of substitutes at the hydrazone linkage on the ph stability of PEG-PE conjugates. Bioconjug. Chem. 2007;18:363–370. doi: 10.1021/bc060228x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Kale AA, Torchilin VP. Enhanced transfection of tumor cells in vivo using “smart” pH-sensitive TAT- modified pegylated liposomes. J. Drug Target. 2007;15:538–545. doi: 10.1080/10611860701498203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Koren E, Apte A, Jani A, Torchilin VP. Multifunctional PEGylated 2C5-immunoliposomes containing pH-sensitive bonds and TAT peptide for enhanced tumor cell internalization and cytotoxicity. J. Control. Release. 2012;160:264–273. doi: 10.1016/j.jconrel.2011.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Apte A, Koren E, Koshkaryev A, Torchilin VP. Doxorubicin in TAT peptide-modified multifunctional immunoliposomes demonstrates increased activity against both drug-sensitive and drug-resistant ovarian cancer models. Cancer Biol. Ther. 2013;15:69–80. doi: 10.4161/cbt.26609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Xiong XB, Lavasanifar A. Traceable multifunctional micellar nanocarriers for cancer-targeted co-delivery of MDR-1 siRNA and doxorubicin. ACS Nano. 2011;5:5202–5213. doi: 10.1021/nn2013707. [DOI] [PubMed] [Google Scholar]
- 119.Galluzzi L, et al. Mitochondrial gateways to cancer. Mol. Aspects Med. 2010;31:1–20. doi: 10.1016/j.mam.2009.08.002. [DOI] [PubMed] [Google Scholar]
- 120.Biswas S, Dodwadkar NS, Sawant RR, Koshkaryev A, Torchilin VP. Surface modification of liposomes with rhodamine-123-conjugated polymer results in enhanced mitochondrial targeting. J. Drug Target. 2011;19:552–561. doi: 10.3109/1061186X.2010.536983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Koshkaryev A, Thekkedath R, Pagano C, Meerovich I, Torchilin VP. Targeting of lysosomes by liposomes modified with octadecyl-rhodamine B. J. Drug Target. 2011;19:606–614. doi: 10.3109/1061186X.2010.550921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Thekkedath R, Koshkaryev A, Torchilin VP. Lysosome-targeted octadecyl-rhodamine B-liposomes enhance lysosomal accumulation of glucocerebrosidase in Gaucher’s cells in vitro. Nanomed. 2013;8:1055–1065. doi: 10.2217/nnm.12.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Willmann JK, van Bruggen N, Dinkelborg LM, Gambhir SS. Molecular imaging in drug development. Nature Rev. Drug Discov. 2008;7:591–607. doi: 10.1038/nrd2290. [DOI] [PubMed] [Google Scholar]
- 124.Liu J, et al. Bifunctional nanoparticles with fluorescence and magnetism via surface-initiated AGET ATRP mediated by an iron catalyst. Langmuir. 2011;27:12684–12692. doi: 10.1021/la202749v. [DOI] [PubMed] [Google Scholar]
- 125.Zheng J, Liu J, Dunne M, Jaffray DA, Allen C. In vivo performance of a liposomal vascular contrast agent for CT and MR-based image guidance applications. Pharm. Res. 2007;24:1193–1201. doi: 10.1007/s11095-006-9220-1. [DOI] [PubMed] [Google Scholar]
- 126.Wen S, et al. Multifunctional dendrimer-entrapped gold nanoparticles for dual mode CT/MR imaging applications. Biomaterials. 2013;34:1570–1580. doi: 10.1016/j.biomaterials.2012.11.010. [DOI] [PubMed] [Google Scholar]
- 127.Li S, Goins B, Zhang L, Bao A. Novel multifunctional theranostic liposome drug delivery system: construction, characterization and multimodality MR, near-infrared fluorescent and nuclear imaging. Bioconj. Chem. 2012;23:1322–1332. doi: 10.1021/bc300175d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Mitchell N, et al. Incorporation of paramagnetic, fluorescent and PET/SPECT contrast agents into liposomes for multimodal imaging. Biomaterials. 2013;34:1179–1192. doi: 10.1016/j.biomaterials.2012.09.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Mitra A, Nan A, Line BR, Ghandehari H. Nanocarriers for nuclear imaging and radiotherapy of cancer. Curr. Pharm. Des. 2006;12:4729–4749. doi: 10.2174/138161206779026317. [DOI] [PubMed] [Google Scholar]
- 130.Trubetskoy VS, Cannillo JA, Milshtein A, Wolf GL, Torchilin VP. Controlled delivery of Gd-containing liposomes to lymph nodes: surface modification may enhance MRI contrast properties. Magn. Reson. Imag. 1995;13:31–37. doi: 10.1016/0730-725x(94)00083-f. [DOI] [PubMed] [Google Scholar]
- 131.Erdogan S, Medarova ZO, Roby A, Moore A, Torchilin VP. Enhanced tumor MR imaging with gadolinium-loaded polychelating polymer-containing tumor-targeted liposomes. J. Magn. Reson. Imag. 2008;27:574–580. doi: 10.1002/jmri.21202. [DOI] [PubMed] [Google Scholar]
- 132.Torchilin VP. Surface-modified liposomes in gamma- and MR-imaging. Adv. Drug Deliv. Rev. 1997;24:301–313. [Google Scholar]
- 133.Glogard C, Stensrud G, Hovland R, Fossheim SL, Klaveness J. Liposomes as carriers of amphiphilic gadolinium chelates: the effect of membrane composition on incorporation efficacy and in vitro relaxivity. Int. J. Pharm. 2002;233:131–140. doi: 10.1016/s0378-5173(01)00935-8. [DOI] [PubMed] [Google Scholar]
- 134.Wen CJ, Zhang LW, Al-Suwayeh SA, Yen TC, Fang JY. Theranostic liposomes loaded with quantum dots and apomorphine for brain targeting and bioimaging. Int. J. Nanomed. 2012;7:1599–1611. doi: 10.2147/IJN.S29369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Kenny GD, et al. Multifunctional receptor-targeted nanocomplexes for the delivery of therapeutic nucleic acids to the brain. Biomaterials. 2013;34:9190–9200. doi: 10.1016/j.biomaterials.2013.07.081. [DOI] [PubMed] [Google Scholar]
- 136.Lee PW, et al. Multifunctional core-shell polymeric nanoparticles for transdermal DNA delivery and epidermal Langerhans cells tracking. Biomaterials. 2010;31:2425–2434. doi: 10.1016/j.biomaterials.2009.11.100. [DOI] [PubMed] [Google Scholar]
- 137.Elbayoumi TA, Torchilin VP. Enhanced accumulation of long-circulating liposomes modified with the nucleosome-specific monoclonal antibody 2C5 in various tumours in mice: gamma-imaging studies. Eur. J. Nucl. Med. Mol. Imag. 2006;33:1196–1205. doi: 10.1007/s00259-006-0139-x. [DOI] [PubMed] [Google Scholar]
- 138.Elbayoumi TA, Torchilin VP. Enhanced cytotoxicity of monoclonal anticancer antibody 2C5-modified doxorubicin-loaded PEGylated liposomes against various tumor cell lines. Eur. J. Pharm. Sci. 2007;32:159–168. doi: 10.1016/j.ejps.2007.05.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Thomas R, Park IK, Jeong YY. Magnetic iron oxide nanoparticles for multimodal imaging and therapy of cancer. Int. J. Mol. Sci. 2013;14:15910–15930. doi: 10.3390/ijms140815910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Sun C, et al. Tumor-targeted drug delivery and MRI contrast enhancement by chlorotoxin-conjugated iron oxide nanoparticles. Nanomed. 2008;3:495–505. doi: 10.2217/17435889.3.4.495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Yang L, et al. Receptor-targeted nanoparticles for in vivo imaging of breast cancer. Clin. Cancer Res. 2009;15:4722–4732. doi: 10.1158/1078-0432.CCR-08-3289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Kumar M, Yigit M, Dai G, Moore A, Medarova Z. Image-guided breast tumor therapy using a small interfering RNA nanodrug. Cancer Res. 2010;70:7553–7561. doi: 10.1158/0008-5472.CAN-10-2070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Medarova Z, Pham W, Farrar C, Petkova V, Moore A. In vivo imaging of siRNA delivery and silencing in tumors. Nature Med. 2007;13:372–377. doi: 10.1038/nm1486. [DOI] [PubMed] [Google Scholar]
- 144.Koo H, et al. In vivo tumor diagnosis and photodynamic therapy via tumoral pH-responsive polymeric micelles. Chem. Commun. 2010;46:5668–5670. doi: 10.1039/c0cc01413c. [DOI] [PubMed] [Google Scholar]
- 145.Kenny GD, et al. Novel multifunctional nanoparticle mediates siRNA tumour delivery, visualisation and therapeutic tumour reduction in vivo. J. Control. Release. 2011;149:111–116. doi: 10.1016/j.jconrel.2010.09.020. [DOI] [PubMed] [Google Scholar]
- 146.Grange C, et al. Combined delivery and magnetic resonance imaging of neural cell adhesion molecule- targeted doxorubicin-containing liposomes in experimentally induced Kaposi’s sarcoma. Cancer Res. 2010;70:2180–2190. doi: 10.1158/0008-5472.CAN-09-2821. [DOI] [PubMed] [Google Scholar]
- 147.Deng L, et al. A MSLN-targeted multifunctional nanoimmunoliposome for MRI and targeting therapy in pancreatic cancer. Int. J. Nanomed. 2012;7:5053–5065. doi: 10.2147/IJN.S34801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Koning GA, Krijger GC. Targeted multifunctional lipid-based nanocarriers for image-guided drug delivery. Anticancer Agents Med. Chem. 2007;7:425–440. doi: 10.2174/187152007781058613. [DOI] [PubMed] [Google Scholar]
- 149.Sajja HK, et al. Development of multifunctional nanoparticles for targeted drug delivery and noninvasive imaging of therapeutic effect. Curr. Drug Discov. Technol. 2009;6:43–51. doi: 10.2174/157016309787581066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Parhi P, Mohanty C, Sahoo SK. Nanotechnology- based combinational drug delivery: an emerging approach for cancer therapy. Drug Discov. Today. 2012;17:1044–1052. doi: 10.1016/j.drudis.2012.05.010. [DOI] [PubMed] [Google Scholar]
- 151.Chen Y, Zhu X, Zhang X, Liu B, Huang L. Nanoparticles modified with tumor-targeting scFv deliver siRNA and miRNA for cancer therapy. Mol. Ther. 2010;18:1650–1656. doi: 10.1038/mt.2010.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Shim G, et al. Trilysinoyl oleylamide-based cationic liposomes for systemic co-delivery of siRNA and an anticancer drug. J. Control. Release. 2011;155:60–66. doi: 10.1016/j.jconrel.2010.10.017. [DOI] [PubMed] [Google Scholar]
- 153.Xiao W, et al. Co-delivery of doxorubicin and plasmid by a novel FGFR-mediated cationic liposome. Int. J. Pharm. 2010;393:119–126. doi: 10.1016/j.ijpharm.2010.04.018. [DOI] [PubMed] [Google Scholar]
- 154.Grossman D, Kim PJ, Schechner JS, Altieri DC. Inhibition of melanoma tumor growth in vivo by survivin targeting. Proc. Natl Acad. Sci. USA. 2001;98:635–640. doi: 10.1073/pnas.230450097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Zhang Y, et al. Incorporation of a selective sigma-2 receptor ligand enhances uptake of liposomes by multiple cancer cells. Int. J. Nanomed. 2012;7:4473–4485. doi: 10.2147/IJN.S31981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Riviere K, Huang Z, Jerger K, Macaraeg N, Szoka FC., Jr. Antitumor effect of folate-targeted liposomal doxorubicin in KB tumor-bearing mice after intravenous administration. J. Drug Target. 2011;19:14–24. doi: 10.3109/10611861003733953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Adrian JE, et al. Targeted SAINT-O-Somes for improved intracellular delivery of siRNA and cytotoxic drugs into endothelial cells. J. Control. Release. 2010;144:341–349. doi: 10.1016/j.jconrel.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 158.Batist G, et al. Safety, pharmacokinetics, and efficacy of CPX-1 liposome injection in patients with advanced solid tumors. Clin. Cancer Res. 2009;15:692–700. doi: 10.1158/1078-0432.CCR-08-0515. [DOI] [PubMed] [Google Scholar]
- 159.Bartlett DW, Su H, Hildebrandt IJ, Weber WA, Davis ME. Impact of tumor-specific targeting on the biodistribution and efficacy of siRNA nanoparticles measured by multimodality in vivo imaging. Proc. Natl Acad. Sci. USA. 2007;104:15549–15554. doi: 10.1073/pnas.0707461104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Kirpotin DB, et al. Antibody targeting of long-circulating lipidic nanoparticles does not increase tumor localization but does increase internalization in animal models. Cancer Res. 2006;66:6732–6740. doi: 10.1158/0008-5472.CAN-05-4199. [DOI] [PubMed] [Google Scholar]
- 161.Bae YH, Park K. Targeted drug delivery to tumors: myths, reality and possibility. J. Control. Release. 2011;153:198–205. doi: 10.1016/j.jconrel.2011.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Venditto VJ, Szoka FC., Jr. Cancer nanomedicines: so many papers and so few drugs. Adv. Drug Deliv. Rev. 2013;65:80–88. doi: 10.1016/j.addr.2012.09.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Wei A, Mehtala JG, Patri AK. Challenges and opportunities in the advancement of nanomedicines. J. Control. Release. 2012;164:236–246. doi: 10.1016/j.jconrel.2012.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Crommelin DJ, Florence AT. Towards more effective advanced drug delivery systems. Int. J. Pharm. 2013;454:496–511. doi: 10.1016/j.ijpharm.2013.02.020. [DOI] [PubMed] [Google Scholar]
- 165.Barenholz Y. Doxil® — the first FDA-approved nano-drug: lessons learned. J. Control. Release. 2012;160:117–134. doi: 10.1016/j.jconrel.2012.03.020. [DOI] [PubMed] [Google Scholar]
- 166.Zhang Q, Huang XE, Gao LL. A clinical study on the premedication of paclitaxel liposome in the treatment of solid tumors. Biomed. Pharmacother. 2009;63:603–607. doi: 10.1016/j.biopha.2008.10.001. [DOI] [PubMed] [Google Scholar]
- 167.Petre CE, Dittmer DP. Liposomal daunorubicin as treatment for Kaposi’s sarcoma. Int. J. Nanomed. 2007;2:277–288. [PMC free article] [PubMed] [Google Scholar]
- 168.Park J. Liposome-based drug delivery in breast cancer treatment. Breast Cancer Res. 2002;4:95–99. doi: 10.1186/bcr432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Batist G, et al. Reduced cardiotoxicity and preserved antitumor efficacy of liposome-encapsulated doxorubicin and cyclophosphamide compared with conventional doxorubicin and cyclophosphamide in a randomized, multicenter trial of metastatic breast cancer. J. Clin. Oncol. 2001;19:1444–1454. doi: 10.1200/JCO.2001.19.5.1444. [DOI] [PubMed] [Google Scholar]
- 170.Ayen WY, Kumar N. In vivo evaluation of doxorubicin-loaded (PEG)3-PLA nanopolymersomes (PolyDoxSome) using DMBA-induced mammary carcinoma rat model and comparison with marketed LipoDox™. Pharm. Res. 2012;29:2522–2533. doi: 10.1007/s11095-012-0783-8. [DOI] [PubMed] [Google Scholar]
- 171.Taiwanese Gynecologic Oncology Group et al. Pegylated liposomal doxorubicin (Lipo-Dox) for platinum-resistant or refractory epithelial ovarian carcinoma: a Taiwanese gynecologic oncology group study with long-term follow-up. Gynecol. Oncol. 2006;101:423–428. doi: 10.1016/j.ygyno.2005.10.027. [DOI] [PubMed] [Google Scholar]
- 172.Silverman JA, Deitcher SR. Marqibo® (vincristine sulfate liposome injection) improves the pharmacokinetics and pharmacodynamics of vincristine. Cancer Chemother. Pharmacol. 2013;71:555–564. doi: 10.1007/s00280-012-2042-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Rodriguez MA, et al. Vincristine sulfate liposomes injection (Marqibo) in heavily pretreated patients with refractory aggressive non-Hodgkin lymphoma: report of the pivotal phase 2 study. Cancer. 2009;115:3475–3482. doi: 10.1002/cncr.24359. [DOI] [PubMed] [Google Scholar]
- 174.Sarris AH, et al. Liposomal vincristine in relapsed non-Hodgkin’s lymphomas: early results of an ongoing phase II trial. Ann. Oncol. 2000;11:69–72. doi: 10.1023/a:1008348010437. [DOI] [PubMed] [Google Scholar]
- 175.Immordino ML, Dosio F, Cattel L. Stealth liposomes: review of the basic science, rationale, and clinical applications, existing and potential. Int. J. Nanomed. 2006;1:297–315. [PMC free article] [PubMed] [Google Scholar]
- 176.Fasol U, et al. Vascular and pharmacokinetic effects of EndoTAG-1 in patients with advanced cancer and liver metastasis. Ann. Oncol. 2012;23:1030–1036. doi: 10.1093/annonc/mdr300. [DOI] [PubMed] [Google Scholar]
- 177.Fantini M, et al. Lipoplatin treatment in lung and breast cancer. Chemother. Res. Pract. 2011;2011:125192. doi: 10.1155/2011/125192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Stathopoulos GP, et al. Comparison of liposomal cisplatin versus cisplatin in non-squamous cell non- small-cell lung cancer. Cancer Chemother. Pharmacol. 2011;68:945–950. doi: 10.1007/s00280-011-1572-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Stathopoulos GP, Boulikas T. Lipoplatin formulation review article. J. Drug Deliv. 2012;2012:581363. doi: 10.1155/2012/581363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Newman MS, Colbern GT, Working PK, Engbers C, Amantea MA. Comparative pharmacokinetics, tissue distribution, and therapeutic effectiveness of cisplatin encapsulated in long- circulating, pegylated liposomes (SPI-077) in tumor- bearing mice. Cancer Chemother. Pharmacol. 1999;43:1–7. doi: 10.1007/s002800050855. [DOI] [PubMed] [Google Scholar]
- 181.Seetharamu N, Kim E, Hochster H, Martin F, Muggia F. Phase II study of liposomal cisplatin (SPI-77) in platinum-sensitive recurrences of ovarian cancer. Anticancer Res. 2010;30:541–545. [PubMed] [Google Scholar]
- 182.Dicko A, Mayer LD, Tardi PG. Use of nanoscale delivery systems to maintain synergistic drug ratios in vivo. Expert Opin. Drug Deliv. 2010;7:1329–1341. doi: 10.1517/17425247.2010.538678. [DOI] [PubMed] [Google Scholar]
- 183.Poon RTP, Borys N. Lyso-thermosensitive liposomal doxorubicin: an adjuvant to increase the cure rate of radiofrequency ablation in liver cancer. Future Oncol. 2011;7:937–945. doi: 10.2217/fon.11.73. [DOI] [PubMed] [Google Scholar]
- 184.Staruch R, Chopra R, Hynynen K. Localised drug release using MRI-controlled focused ultrasound hyperthermia. Int. J. Hyperthermia. 2011;27:156–171. doi: 10.3109/02656736.2010.518198. [DOI] [PubMed] [Google Scholar]
- 185.Pal A, et al. Preclinical safety, pharmacokinetics and antitumor efficacy profile of liposome-entrapped SN-38 formulation. Anticancer Res. 2005;25:331–341. [PubMed] [Google Scholar]
- 186.Booser DJ, et al. Phase II study of liposomal annamycin in the treatment of doxorubicin-resistant breast cancer. Cancer Chemother. Pharmacol. 2002;50:6–8. doi: 10.1007/s00280-002-0464-0. [DOI] [PubMed] [Google Scholar]
- 187.Apostolidou E, Swords R, Alvarado Y, Giles FJ. Treatment of acute lymphoblastic leukaemia: a new era. Drugs. 2007;67:2153–2171. doi: 10.2165/00003495-200767150-00004. [DOI] [PubMed] [Google Scholar]
- 188.Semple SC, et al. Optimization and characterization of a sphingomyelin/cholesterol liposome formulation of vinorelbine with promising antitumor activity. J. Pharm. Sci. 2005;94:1024–1038. doi: 10.1002/jps.20332. [DOI] [PubMed] [Google Scholar]
- 189.Dong DW, et al. pH-responsive complexes using prefunctionalized polymers for synchronous delivery of doxorubicin and siRNA to cancer cells. Biomaterials. 2013;34:4849–4859. doi: 10.1016/j.biomaterials.2013.03.018. [DOI] [PubMed] [Google Scholar]
- 190.Kim SH, Jeong JH, Kim TI, Kim SW, Bull DA. VEGF siRNA delivery system using arginine-grafted bioreducible poly(disulfide amine) Mol. Pharm. 2009;6:718–726. doi: 10.1021/mp800161e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Vader P, van der Aa LJ, Engbersen JF, Storm G, Schiffelers RM. Disulfide-based poly(amido amine)s for siRNA delivery: effects of structure on siRNA complexation, cellular uptake, gene silencing and toxicity. Pharm. Res. 2011;28:1013–1022. doi: 10.1007/s11095-010-0344-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Kurtoglu YE, et al. Poly(amidoamine) dendrimer drug conjugates with disulfide linkages for intracellular drug delivery. Biomaterials. 2009;30:2112–2121. doi: 10.1016/j.biomaterials.2008.12.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Musacchio T, Vaze O, D’Souza G, Torchilin VP. Effective stabilization and delivery of siRNA: reversible siRNA-phospholipid conjugate in nanosized mixed polymeric micelles. Bioconjug. Chem. 2010;21:1530–1536. doi: 10.1021/bc100199c. [DOI] [PubMed] [Google Scholar]
- 194.Wong C, et al. Multistage nanoparticle delivery system for deep penetration into tumor tissue. Proc. Natl Acad. Sci. USA. 2011;108:2426–2431. doi: 10.1073/pnas.1018382108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Pradhan P, et al. Targeted temperature sensitive magnetic liposomes for thermo-chemotherapy. J. Control Release. 2010;142:108–121. doi: 10.1016/j.jconrel.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 196.Sherlock SP, Tabakman SM, Xie L, Dai H. Photothermally enhanced drug delivery by ultrasmall multifunctional FeCo/graphitic shell nanocrystals. ACS Nano. 2011;5:1505–1512. doi: 10.1021/nn103415x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Schroeder A, et al. Ultrasound triggered release of cisplatin from liposomes in murine tumors. J. Control. Release. 2009;137:63–68. doi: 10.1016/j.jconrel.2009.03.007. [DOI] [PubMed] [Google Scholar]
- 198.Ibsen S, et al. A novel nested liposome drug delivery vehicle capable of ultrasound triggered release of its payload. J. Control. Release. 2011;155:358–366. doi: 10.1016/j.jconrel.2011.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Liu D, et al. Conjugation of paclitaxel to iron oxide nanoparticles for tumor imaging and therapy. Nanoscale. 2012;4:2306–2310. doi: 10.1039/c2nr11918h. [DOI] [PubMed] [Google Scholar]
- 200.Zhu L, Torchilin VP. Stimulus-responsive nanopreparations for tumor targeting. Integr. Biol. 2013;5:96–107. doi: 10.1039/c2ib20135f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Sun L, Yang Y, Dong CM, Wei Y. Two-photon- sensitive and sugar-targeted nanocarriers from degradable and dendritic amphiphiles. Small. 2011;7:401–406. doi: 10.1002/smll.201001729. [DOI] [PubMed] [Google Scholar]
- 202.Slingerland M, et al. Bioequivalence of Liposome-Entrapped Paclitaxel Easy-To-Use (LEP-ETU) formulation and paclitaxel in polyethoxylated castor oil: a randomized, two-period crossover study in patients with advanced cancer. Clin Ther. 2013;35:1946–1954. doi: 10.1016/j.clinthera.2013.10.009. [DOI] [PubMed] [Google Scholar]
- 203.de Jonge MJ, et al. Early cessation of the clinical development of LiPlaCis, a liposomal cisplatin formulation. Eur. J.Cancer. 2010;46:3016–3021. doi: 10.1016/j.ejca.2010.07.015. [DOI] [PubMed] [Google Scholar]
- 204.Saif MW. MM-398 achieves primary endpoint of overall survival in phase III study in patients with gemcitabine refractory metastatic pancreatic cancer. JOP. 2014;15:278–279. doi: 10.6092/1590-8577/2507. [DOI] [PubMed] [Google Scholar]