Abstract
Purpose
To identify patient and physician factors related to enrollment onto Gynecologic Oncology Group (GOG) trials.
Methods
Prospective study of women with primary or recurrent cancer of the uterus or cervix treated at a GOG institution from July 2010 to January 2012. Logistic regression examined probability of availability, eligibility and enrollment in a GOG trial. Odds ratios (OR) and 95% confidence intervals (CI) for significant (p<0.05) results reported.
Results
Sixty institutions, 781 patients, and 150 physicians participated, 300/780 (38%) had a trial available, 290/300 had known participation status. Of these, 150 women enrolled (59.5%), 102 eligible did not enroll (35%), 38 (13%) were ineligible. Ethnicity and specialty of physician, practice type, data management availability, and patient age were significantly associated with trial availability. Patients with ≥ 4 comorbidities (OR 4.5; CI 1.7-11.8) had higher odds of trial ineligibility. Non-White patients (OR 7.9; CI 1.3-46.2) and patients of Black physicians had greater odds of enrolling (OR 56.5; CI 1.1- 999.9) in a therapeutic trial. Significant patient therapeutic trial enrollment factors: belief trial may help (OR 76.9; CI 4.9->1000), concern about care if not on trial (OR12.1; CI 2.1-71.4), pressure to enroll (OR .27; CI 0.12-.64), caregiving without pay (OR 0.13; CI.02-.84). Significant physician beliefs were: patients would not do well on standard therapy (OR 3.6; CI 1.6-8.4), and trial would not be time consuming (OR 3.3; CI 1.3-8.1).
Conclusions
Trial availability, patient and physician beliefs were factors identified that if modified could improve enrollment in cancer cooperative group clinical trials.
INTRODUCTION
It is reported that 80% of clinical trials struggle to meet their set accrual targets. [1] Cheng et al reported that of more than 500 NCI Cancer Therapy Evaluation Program (CTEP) trials, 40 % failed to achieve minimum patient enrollment, and more than three of five phase III trials failed to do so [1]. Enrollment in cancer trials has, for decades been low for all groups, with racial and ethnic minorities, women, and the elderly reported to be less likely to enroll in cooperative group cancer trials than whites, men, and younger patients, respectively. Arising from concern of the ability of cooperative groups to conduct timely, large-scale, innovative clinical trials needed to improve patient care, a recent Institute of Medicine report recommended changes to the clinical cooperative group system to enhance efficiency and participation of patients and physicians in clinical trial research. [2,3]
For patients who have access to clinical trials, through their treating physician, it is recognized that patient accrual is influenced by a number of factors. In 2007, Howerton and colleagues reviewed 18 studies examining recruitment of under-represented populations to cancer clinical trials and determined that patient accrual was significantly influenced by provider attitudes. [4]. Other factors influencing enrollment include: awareness and individual level influences, interpersonal level factors, institutional and clinical practice level influences, and community and public policy level influences [5-10]. Few studies have included both the patient and provider perspective when examining factors influencing trial enrollment in the setting of real time decision-making.
In 2010, the Gynecologic Oncology Group (GOG), a multi-disciplinary cooperative group dedicated to clinical research in gynecologic cancers consisted of nearly 200 institutions across the country. Over the course of a decade, the GOG recruited more than 41,000 women onto clinical trials [11]. No prior published studies have examined trial availability, eligibility and enrollment in women with gynecologic cancer.
Given that multiple factors influence participation in clinical trials and the paucity of literature in gynecologic cancers, we sought to identify modifiable factors associated with clinical trial availability, eligibility, and enrollment for patients with cancer of the cervix and endometrium in order to inform future interventions.
METHODS
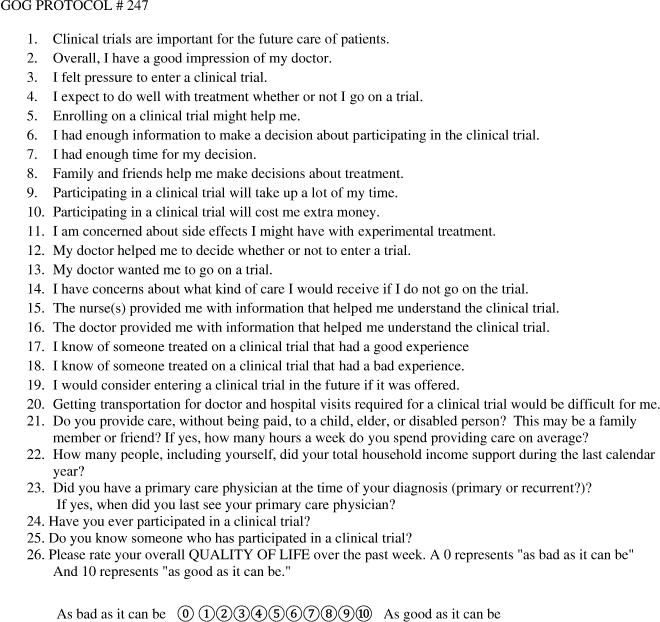
GOG Protocol 247 was a prospective multi-institutional observational study of women with newly diagnosed primary or recurrent cancer of the uterine corpus or cervix under the care of a GOG participating gynecologic oncologist, medical oncologist, or radiation oncologist at a GOG member or affiliate institution during the period 7/19/10- 1/17/12. The project received local Institutional Review Board review for participating sites. Each primary GOG physician completed a registration form indicating; year of birth, race, ethnicity, specialty, years of experience, institutional affiliation, practice type and the type of staff dedicated to research. Each patient completed the patient registration form indicating; race, ethnicity, income, and then completed the patient quality of life questionnaire (Figure 1). All participants signed an institutionally approved informed consent to participate in the current study, including Health Insurance Portability and Accountability Act (HIPAA) authorization. Consistent with institutional and physician practices, patients with a trial available and who were eligible were invited to enroll in a therapeutic trial.
Figure 1.
Questionnaire
Once a decision was made to enroll or not enroll the patient in a GOG clinical trial, the GOG physician completed the Physician Follow-up Questionnaire.
Logistic regression was applied to examine the effect of patient and physician factors on the probabilities of availability, eligibility, and enrollment on a GOG trial. Adjusted Odds ratios (OR) and 95% confidence intervals (CI) were reported for statistically significant results (p<0.05) for the final selected logistic regression model.
Questionnaire variables ranging from strongly disagree to strongly agree were recoded into two categories (usually agree or disagree) to provide cell counts large enough for univariate Chi Square tests to be valid. Similarly, other categorical variable codes were collapsed as needed to allow a valid univariate Chi-square test for associations with each outcome. Variables with invalid Chi Square tests were deleted from further consideration. Univariate tests of association of outcomes with continuous predictors were performed using t-tests or Mann-Whitney U- Tests as appropriate.
Each variable found to be significantly associated with univariate tests was included in initial logistic regression models and backward selection was used to reduce the model to include significant (p<0.05) variables and any other variables that, if deleted would result in the deletion of a previously significant variable. At each step, the factor with the largest p-value was deleted, unless its deletion resulted in another variable that had been significant becoming non-significant. In this case, the deleted variable was added back into the model and the variable with the next largest p-value was deleted. The final models contained only significant factors or non-significant factors that, when deleted, resulted in a loss of significance.
The results include the final models resulting from the backward selection strategy, along with follow-up pairwise comparison to describe significant effects. Adjusted OR's and 95% confidence intervals were used to make the pairwise comparisons.
RESULTS
During the study period, 781 women from 60 sites and their physicians completed the GOG 247 registration and questionnaire. Patients and their physicians participated from 28 states across the continental US. Twenty-four of the participating sites were primary GOG sites and the remaining sites were affiliates and nearly 1/3 of the patients were enrolled from CCOP sites.
Patient and physician ethnicity, race and age distributions of the patients and physicians participating in GOG 247 are presented in Table 1. Gynecologic oncologists enrolled 91% of the patients, and radiation and medical oncologists enrolled the remaining 9% of women. Forty seven percent of physicians practiced in an academic center, 21% a hospital-based practice, 28% private practice, and 4% were in other practice settings.
Table 1.
Race and ethnicity of patients and physicians enrolled in this study (Gynecologic Oncology Group Study Number GOG 247)
| Patient and Physician Demographics | Patient n = 781 (%) | Physician n = 150 (%) |
|---|---|---|
| Age | ||
| 20-29 | 8(1) | 0 |
| 30-39 | 51(6.5) | 25(16.7) |
| 40-49 | 88(11.3) | 53(35.3) |
| 50-59 | 205(26.2) | 45(30) |
| 60-69 | 259(33.2) | 22(14.7) |
| 70-79 | 129(16.5) | 4(2.7) |
| 80-89 | 37(4.7) | 1(.7) |
| >=90 | 4(.5) | 0 |
| Ethnicity | ||
| Hispanic | 24 (3.1) | 7 (4.7) |
| Non-Hispanic | 755(96.7) | 136(90.6) |
| Unknown | 2 (0.2) | 7 (4.7) |
| Race | ||
| Asian | 23 (2.9) | 18(12) |
| Black | 63 (8.0) | 6 (4) |
| American Indian | 20 (2.6) | 0 |
| White | 665(85.1) | 123(82) |
| Native Hawaiian/Pacific Islander | 2 (0.2) | 0 |
| Unknown | 8 (1.0) | 3 (2) |
A GOG treatment trial was available at the institution for 300 (38%) of the participating women. Ten of these were deemed eligible by their physician but it was not reported whether they participated in a GOG treatment trial or not. Of the 290 patients with a trial available and known participation status, 102 (35%) were eligible but did not enroll, 38 (13%) were not eligible and 150 (52%) enrolled in a treatment trial. Those enrolled represented 150/252 (59.5%) of patients who enrolled or were eligible for a trial and did not enroll. The distributions of these 290 patients with a trial available into these eligibility/enrollment categories are presented by race and overall in Table 2.
Table 2.
Eligibility/Enrollment Outcome Distribution of patients with a Trial Available (n=290), by Race and Overall
| Patient Race | Eligible, Not Enrolled | Enrolled | Not Eligible | Race of Women with a Trial Available |
|---|---|---|---|---|
| (%) Among patients with a Trial Available | (%)(Among patients with a Trial Available | (%)Among patients with a Trial Available | (%) | |
| White | 94 (40) | 107 (45) | 33 (14) | 234 (81) |
| Black | 2 (7) | 24 (83) | 3 (10) | 29 (10) |
| Asian/Asian/White | 2 (14.2) | 11 (78.6) | 1 (7) | 14(4.8) |
| Native American | 1 (12.5) | 6 (75) | 1 (12.5) | 8 (2.7) |
| Hawaiian/PI | 1 (100) | 0 | 0 | 1 (0.03) |
| Unknown | 2 (50) | 2 (50) | 0 | 4 (1.3) |
| Overall Total (%) | 102 (35) | 150 (52) | 38 (13) | 290 (100) |
During the study period 15 cervix cancer trials, 16 endometrial cancer trials and 4 uterine sarcoma trials were open in the GOG. The mean number of studies open at each site was 4.3 with a median of 3 and a range of 0-26.
Physician and practice characteristics and trial availability
Patients of physicians with Hispanic/Latino ethnicity had lower odds of having a trial available than those of non-Hispanic/Latino physicians (OR 0.25; CI 0.8, 0.75, p=0.0135). There were no differences in trial availability for patients among physicians of different racial groups. A description race and ethnicity of physicians, and the availability, eligibility and enrollment of patients onto a clinical trial is found in Supplemental Table 1 (on line).
Physician subspecialty was related to trial availability. Gynecologic oncologists (OR; CI 2.1, 20.3; p=0.0014) and medical oncologists (OR 5.0; CI 1.4, 18.6; p=0.0156) had higher odds of having trials available for patients with cervical or uterine cancer compared to radiation oncologists.
Physicians in academic practice (OR 8.56; CI 2.57, 28.6, p=0.0005), hospital based practice (OR 9.63; CI 3.89-23.78, p<0.0001) and other practice settings (OR 16.48; CI 5.27, 51.5, p<0.0001) were more likely to have trials available than those in private practice.
Dedicated personnel resources were important in determining trial availability. Institutions with no data management staff dedicated to GOG were less likely to have a trial available for their patients (OR 0.25; CI 0.1, 0.55, p=0.0006) than institutions with GOG data management staff. In summary, ethnicity, specialty and practice type of physician, and availability and adequacy of data management infrastructure were significantly associated with trial availability.
Patient characteristics and trial availability
Overall, trials were available for 33% of Black patients, 37.8% of White patients and 48% of Asian patients, (p=0.1680). Trials were available for just 7% of Hispanic/Latina women compared with 43% of Non Hispanic/Latina women (p=0.0001). We determined that there were also differences in the percentage of patients with available trials by age. Patients over the age of 71 were less likely to have trials available when compared with patients under the age of 41 (OR 0.4; 0.2, 0.8, p=0. 0097), 41-50 (OR 0.51; 0.28, .93, p=0.0267), and 51-60 (OR 0.55; 0.34, 0.88. p=0.0120). A description race and ethnicity of patients, trial availability, eligibility and enrollment of patients is found in supplemental Table 2 (on line).
Trials were available for 50% or more of women with Stage IV disease (on line Table 3).
Treatment recommended by physicians who participated in this study
Of the 780 patients enrolled in this study who could be included in any of our analyses (complete data was not available for one patient), in 29% (n=224) the physician offered no further treatment, in 18% (n=143) the physician planned treatment on a GOG trial (4 of these 143, however, did not enroll in a GOG treatment trial), in 1.4% (n=11) participation in a pharmaceutical study was planned (1 of these 11, however, enrolled in a GOG treatment trial), in 6.3% (n=49) an institutional protocol was planned (1 of these, however, enrolled in a GOG treatment trial), and in 45.3% (n=353) treatment off protocol was planned (9 of these 353 women, however, enrolled in a GOG trial).
Physician race and ethnicity and trial eligibility
The percentage of eligible patients did not vary significantly by race of the physician however, patients of Hispanic/Latino physicians had higher odds of being ineligible for a trial (OR 28.87; 2.33-358.86, p=0.009) (Table 4).
Table 4.
Logistic regression analysis: variables associated with trial eligibility/ineligibility among patients with a trial available (n=290)
| P-value | Odds Ratio | Lower Bound of the 95% CI | Upper Bound of the 95% CI | |
|---|---|---|---|---|
| Ethnicity of Physician non Hispanic | 0.009 | 28.87 | 2.32 | 358.86 |
| I have concerns about what type of care I would receive If I don't go on the trial | 0.0322 | 5.56 | 1.16 | 29.4 |
| Comorbidity <4 vs. ≥4 | 0.0019 | 4.50 | 1.74 | 11.76 |
Patient eligibility for GOG clinical trial (n=300 patients with a trial available)
For the 300 patients for whom a trial was available there were no significant differences in percent eligible by race of the patient. Supplemental Table 3 (on line) displays eligibility and Supplemental Table 4 (on line) displays enrollment of women by stage of disease and tumor type.
Multiple comorbid illnesses were negatively associated with eligibility for a clinical trial. Eighty six percent of women (240/276) with 4 or fewer comorbidities were eligible for a trial when one was available and 15/24 or 62% of women with more than 4 comorbidities were eligible for a trial when one was available (p=0.0019), Table 4.
Physician characteristics and trial enrollment of eligible or presumed eligible patients with known enrollment outcome (n=290)
Physician attitudes associated with higher odds of enrollment included believing their patient would not respond well to standard treatment (OR 3.07; CI 1.56-8.26, p=0.0027). In addition, if the physician believed that the trial would not be time consuming for the patient, (OR 3.27; CI 1.31-8.13), the odds of patient enrollment were higher than if they believed the trial would take up a lot of the patient's time. Black physicians had higher odds of enrolling patients on a trial (OR 56.5; 1.06->999.999) compared to White or Asian physicians (Table 5).
Table 5.
Logistic regression analysis: variables associated with trial enrollment
| P-value | Odds Ratio | Lower Bound of the 95% CI | Upper Bound of the 95% CI | |
|---|---|---|---|---|
| Race Doctor Asian v White | 0.0004 | 0.03 | 0.005 | 0.22 |
| Race Doctor Black vs. White | 0.0465 | 56.50 | 1.06 | >999.999 |
| Patient race non white vs. white | 0.0219 | 7.893 | 1.35 | 46.19 |
| I felt pressure to enter a trial (agree vs. disagree) | 0.0016 | 0.27 | 0.12 | 0.64 |
| Enrolling in a clinical trial might help me (agree vs. disagree) | 0.0020 | 76.9 | 4.80 | >1000 |
| Participating in a trial will take up a lot of time (agree vs. disagree) | 0.0355 | 0.18 | 0.034 | 0.89 |
| My doctor wanted me to go on trial (agree vs. disagree) | 0.0016 | 13.80 | 2.717 | 71.42 |
| I have concerns about the type of care I would receive if I do not go on trial (agree vs. disagree) | 0.0058 | 12.12 | 2.057 | 71.36 |
| I would consider entering a clinical trial in the future if it was offered (agree vs. disagree) | 0.0022 | 40.00 | 3.780 | 500 |
| Getting transportation for doctor and hospitals visits required for a clinical trial would be difficult for me (agree vs. disagree) | 0.0059 | 0.109 | 0.022 | 0.527 |
| Do you provide care without being paid to a child, elder or disabled person? This may be a family member or friend (yes vs. no) | 0.0323 | 0.125 | 0.019 | 0.84 |
To examine whether the differences in enrollment seen among physicians of different racial groups were uniform across patients of all races, or if they were patient-race specific, a logistic regression model that included the race of the physician by race of patient interaction was performed. This analysis revealed that Black physicians had high rates of enrollment of patients uniform across all races but the low enrollment rate of patients with Asian physicians was specific to White patients..
Patient characteristics associated with clinical trial enrollment
Patient factors associated with higher odds of enrollment were: Non white patient race (OR 7.89,1.35-46.19), the patient believing the clinical trial might help them (OR 76.9; 4.8->1000), believing their doctor wanted them to go on a trial (OR 13.8; 2.72-71.42), or concern about the care they might receive if they were not on a clinical trial (OR12.12; 2.06-71.36). Patients who felt pressured to enter a trial (OR 0.27; 0.12-0.64) or thought participating in a trial would take up a lot of time (OR 0.18. 0.034-0.89) had lower odds of enrolling. Performing duties as a caregiver to a friend or family member without pay was also associated with lower odds of enrollment (0.125; 0.019-0.84). (Table 5) Supplemental on line tables 5 through 7 display additional patient variables associated with availability, eligibility and enrollment.
DISCUSSION
This study represents a unique prospective examination of patient and physician factors associated with entry onto a Gynecologic Oncology Group trial. This is one of the first such studies conducted documenting patient and physician perspectives in real time as the decisions about enrolling in a therapeutic trial were being made. Strengths of this study include: the prospective and multi-institutional nature, the inclusion of the perspectives of physicians and patients, and the analysis of trial availability, patient eligibility, and enrollment outcomes. Limitations of this study include the fact that approximately 1/3 of GOG centers opened this trial and it is not possible to know who was screened and who did not enroll. The findings are provocative and bring new information about what factors influence clinical trial enrollment in women with cervical and uterine cancer in the cooperative group setting.
Overall, clinical trials were available for just 37% of patients. Trials were more likely to be available in hospital based or academic settings with dedicated infrastructure and data management support. A high level of sustained dedicated support for the conduct of clinical trials in community settings is vital for community oncologists to be able to participate in clinical trial networks and for results of clinical trials to be adopted in community settings. This point was emphasized in a 2010 Institute of Medicine report, that noted that uptake of evidence-based practices are slow when practitioners are not engaged in the research that supports the changes. [12]
Overall, 13% of women in this study for whom a trial was available and whose enrollment outcome was known, were not eligible for a GOG clinical trial. Given that the number of individuals screened for trials is not routinely captured and reported, it is uncertain if this percentage is modifiable, however, clinical trial eligibility represents one of the few accrual factors directly controlled by the lead study investigator. Although calls have been made to simplify and provide rationale for study inclusion and exclusion criteria, it is not clear that a common exclusion such as a prior cancer diagnosis interferes with study outcomes in all cases. [13] Exclusions for comorbidity potentially represent a modifiable factor in order for study populations to more accurately reflect the population affected by the condition of interest. [14-17]
Traditionally, time constraints and logistical barriers such as transportation and the necessity of caring for others without pay have not been factored into research infrastructure considerations or feasibility of enrollment. However, given these factors were associated with enrollment in this study, they warrant pro-active consideration and are potentially modifiable with navigator and social service support. [18,19].
The race of the patient and the race of the doctor were associated with the likelihood of clinical trial enrollment. Overall, Black physicians had high rates of enrollment of patients uniform across all races. The enrollment rate of patients with Asian physicians was specific to White patients. Stated differently, this interaction is the result of a difference in the enrollment of White patients when the race of the physician was White, Asian or Black In the group of women that were eligible for a trial, 45% of White women enrolled in a trial in comparison with 83% of Black women, 78% of Asian women, and 75% of Native American Women. We determined that White women enrolled at a lower rate relative to the fraction they represented in the study and Non White women enrolled at a rate higher than the fraction of the population they represented in the study. Restated, White women represented 81% of the 290 women in this study who had a trial available for whom enrollment status was known and 71% of the 150 women who subsequently enrolled in a GOG uterine or cervical cancer trial. Black women represented 10% of 290 and 16% of the 150 who subsequently enrolled in a GOG uterine or cervical trial, Asian women comprised 4.8% of the 290 and 7.3% of those who enrolled. This study had a 5 to 8 fold higher percentage of Native American women in comparison with previously conducted GOG studies. They represented 2.7% (8/290) of this study population and 4% (6/150) of the women in this study that enrolled in a GOG trial. These findings bring a different dimension to the influence of race and cultural perspective in medical and clinical trial settings. [21,22] The relatively high percentage of enrollment among Black women in our study is consistent with a report by Wendler et al., however given our findings documenting the patient perspective on factors influencing enrollment, this should not be interpreted as evidence that barriers to non-white enrollment no longer exist and can be ignored. [23] It is likely there are culturally influenced issues of perceived benefit or risk of harm playing a role in a patient's decision to enter both this study and, more generally, clinical trials. [24,25] The very high enrollment rates (~80%) among minority women may reflect women who were concerned about their treatment if they did not go on a study. There continues to be a great opportunity to address enrollment onto research trials through investigator training that includes acknowledgement of the role of cultural perspectives. [26]. Patients of Hispanic/Latino physicians in this study were less likely to be eligible for GOG studies. Hispanic/Latina women participated at a rate of 3% and no Hispanic/Latina women in this study enrolled in a GOG trial. While the precise reasons for these findings are unknown, these findings are of concern and represent a significant opportunity to address the needs of this growing demographic group. [27-29].
The patient's perception of being helped by the trial and, the perception of the care they might receive if they were not on trial was positively associated with clinical trial enrollment. Conversely, odds of enrollment were lower if the patient felt pressure to enter a trial. From the physician's perspective, if the doctor felt the trial would benefit the patient compared with standard of care the odds of enrollment were higher.
Approaching patients regarding clinical trials requires a delicate balance. It is possible that true pressure existed, or that enthusiasm was interpreted as pressure. This is a reminder of the importance of frankly acknowledging that it is simply not known which treatment is better when comparing an experimental treatment to a standard treatment. Given historical missteps in informed consent, which remain a barrier to participation in research, our findings reveal an opportunity to enhance training of the research team with specific focus on ethical considerations in research and in building trust [30-34]. Cultural appropriateness and sensitivity, and involvement of minority physicians are noted to be important strategies for increasing enrollment of minority patients in research. Possible approaches include implementation of cultural competency training programs accompanied by evaluation and metrics along with tailored, recruitment processes focused on recruitment of minority physicians into research [6,35]. This is particularly relevant given that it is stated that by 2045, people of non-white race and Hispanic/Latino ethnicity are projected to account for the majority of the U.S. population [36]. Currently, just 13.5% percent of practicing physicians identify as Black, American Indian or Alaska Native, or Hispanic/Latino. [37] In our study, 4% of physicians were Black, 4% were Hispanic. None of the physicians were American Indian or Alaska Native, Hawaiian or Pacific Islander. Active intervention will be required to address this important modifiable factor highlighted by our findings.
In summary, we determined there are modifiable infrastructure factors associated with availability of clinical trials and potentially modifiable patient and physician factors associated with patient eligibility for clinical trials. We also determined that variations of enrollment based on the race or ethnicity of the doctor or patient, are potentially modifiable factors that relate to the doctor/patient interaction. Health systems and practices should appreciate that in addition to investigators, patients and a minimum level of dedicated infrastructure, a formalized process to address cultural competence training will promote effective enrollment of patients in clinical trials . Such training can include education aimed at increasing sensitivity and awareness; the provision of relevant multicultural knowledge, health and demographic information; and skills building in bicultural and bilingual interviewing and patient assessment. Assessment of patient satisfaction and correlation of recruitment the burden of disease in the catchment area of interest would add additional dimensions of understanding to local challenges influencing recruitment to clinical trials. [38]
The newly consolidated cooperative group structure (NRG Oncology) and its committees that specifically focus on clinical trial accrual have the potential to draw on best practices from each of the legacy groups and create new processes and programs that will enhance training of investigators, foster development of a diversified workforce and develop recruitment strategies designed to meet the needs of increasingly diverse populations,. These steps would facilitate the goal of comprehensive inclusion of participants in clinical trials to assure expeditious completion and generalizability of clinical trial results [38-40].
Supplementary Material
Highlights.
Ethnicity and specialty of the physician, practice type, data management availability, and patient age were significantly associated with trial availability.
Patient factors associated with enrollment: belief trial might help, concern about care if not on trial, feeling pressure to enroll.
Physician factors associated with enrollment: Patient would not do well on standard therapy and trial would not be time consuming
Table 3.
Trial availability percentage by Stage of disease and by tumor type
| Cervix Trial Available A/B (%) | Uterine Trial Available C/D (%) | |
|---|---|---|
| Stage of Disease/status | ||
| Stage I | 8/63 (12.7) | 100/356 (28) |
| Stage II | 5/32 (15.6) | 31/64 (48) |
| Stage III | 5/27 (18.5) | 76/112 (68) |
| Stage IV | 8/16 (50) | 20/33 (60) |
| Persistent | 4/4(100) | 1/4 (25) |
| Recurrent | 13/18 (72) | 29/51 (57) |
A=number of cervical patients with trial available
B=number of cervical patients
C=number of uterine patients with trial available
D=number of uterine patients
(n= 780, data unavailable for 1 patient)
ACKNOWLEDGMENTS
We would like to thank Linda Gedeon of the NRG Oncology/Gynecologic Oncology Group for her assistance and management of the data on GOG Protocol 247.
The following GOG member institutions participated in this protocol: Roswell Park Cancer Institute; Duke University Medical Center; Abington Memorial Hospital; University of Mississippi; University of Cincinnati Medical Center; University of North Carolina; University of California Medical Center at Irvine; State University of New York Downstate Medical Center; State University of New York at Stony Brook; Cooper Hospital University Medical Center; Columbus Cancer Council/Ohio State University; Women's Cancer Center of Nevada; University of Oklahoma; Case Western Reserve University; Yale University; University of Wisconsin Hospital and Clinics; University of Texas – Galveston; Women and Infants Hospital; The Hospital of Central Connecticut and the Community Clinical Oncology Program.
Research Support: This study was supported by National Cancer Institute grants CA 27469 (Gynecologic Oncology Group) and CA 37517 (Gynecologic Oncology Group Statistical and Data Center).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Previous Presentations: Abstract presented at the 45th Annual Meeting of The Society of Gynecologic Oncology held in Tampa, Florida on March 22-25, 2014.
Registration number at ClinicalTrials.gov: NCT01098630
CONFLICT OF INTEREST
The authors wish to disclose that there are no conflicts of interest with the exception of Dr. Randy Carter who reports that he receives grant funding from the NRG Oncology Group.
REFERENCES
- 1.Cheng SK, Dietrich MS, Ditts DM. Predicting accrual achievement: monitoring accrual milestones of NCI-CTEP–sponsored clinical trials. Clin Cancer Res. 2011;17:1947–55. doi: 10.1158/1078-0432.CCR-10-1730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Murthy VH, Krumholz HM, Gross CP. Participation in cancer clinical trials: Race-, sex-, and age-based disparities. JAMA. 2004;291:2720–2726. doi: 10.1001/jama.291.22.2720. [DOI] [PubMed] [Google Scholar]
- 3.Institute of Medicine (US) Committee on Cancer Clinical Trials and the NCI Cooperative Group Program; Nass SJ, Moses HL, Mendelsohn J, editors. A National Cancer Clinical Trials System for the 21st Century: Reinvigorating the NCI Cooperative Group Program. National Academies Press (US); Washington (DC): 2010. PubMed PMID: 25032387. [PubMed] [Google Scholar]
- 4.Howerton MW, Gibbons MC, Baffi CR, et al. Provider Roles in the recruitment of underrepresented populations to clinical trials. Cancer. 2007;109:465–76. doi: 10.1002/cncr.22436. [DOI] [PubMed] [Google Scholar]
- 5.Joffe S, Cook EF, Cleary PD, Clark JW, Weeks JC. Quality of informed consent in cancer clinical trials: a cross-sectional survey. Lancet. 2001;24:1772–77. doi: 10.1016/S0140-6736(01)06805-2. [DOI] [PubMed] [Google Scholar]
- 6.Ulrich CM1, James JL, Walker EM, Stine SH, Gore E, Prestidge B, et al. RTOG physician and research associate attitudes, beliefs and practices regarding clinical trials: implications for improving patient recruitment. Contemp Clin Trials. 2010;31:221–8. doi: 10.1016/j.cct.2010.03.002. [DOI] [PubMed] [Google Scholar]
- 7.Christian MC, Trimble EL. Increasing participation of physicians and patients from underrepresented racial and ethnic groups in National Cancer Institute-sponsored clinical trials. Cancer Epidem Biomar. 2003;12:S277–S283. [PubMed] [Google Scholar]
- 8.Baquet CR, Ellison GL, Mishra SI. Analysis of Maryland cancer patient participation in national cancer institute-supported cancer treatment clinical trials. J Clin Oncol. 2008;26:3380–86. doi: 10.1200/JCO.2007.14.6027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lara PN, Jr, Higdon R, Lim N, Kwan K, Tanaka M, Lau DH, et al. Prospective evaluation of cancer clinical trial accrual patterns: identifying potential barriers to enrollment. J Clin Oncol. 2001;19:1728–33. doi: 10.1200/JCO.2001.19.6.1728. [DOI] [PubMed] [Google Scholar]
- 10.Baquet CR, Commiskey P, Daniel Mullins C, et al. Recruitment and participation in clinical trials: socio-demographic, rural/urban, and health care access predictors. Cancer Detect Prev. 2006;30:24–33. doi: 10.1016/j.cdp.2005.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.DiSaia PJ. [1/23/15];GOG White Paper 3/4/11. http://www.gog.org/TheGOGWhitePaper.pdf.
- 12.English R, Lebovitz Y, Griffin R. Institute of Medicine (US) Forum on Drug Discovery, Development, and Translation. Transforming Clinical Research in the United States: Challenges and Opportunities: Workshop Summary. National Academies Press (US); Washington (DC): PubMed PMID: 21210556. [PubMed] [Google Scholar]
- 13.Lara PN, Jr1, Higdon R, Lim N, Kwan K, Tanaka M, Lau DH, et al. Prospective evaluation of cancer clinical trial accrual patterns: identifying potential barriers to enrollment. J Clin Oncol. 2001;19:1728–33. doi: 10.1200/JCO.2001.19.6.1728. [DOI] [PubMed] [Google Scholar]
- 14.Brooks SE, Chen TT, Baquet CR, et al. Association of age, race, and co morbid illness with resource utilization for patients undergoing hysterectomy with or without lymph node dissection for endometrial cancer. Gynecol Oncol. 2002;85:242–49. doi: 10.1006/gyno.2002.6591. [DOI] [PubMed] [Google Scholar]
- 15.Brooks SE, Zhan M, Cote T, et al. Surveillance, epidemiology, and end results analysis of 2677 cases of uterine sarcoma 1989-1999. Gynecol Oncol. 2004;93:204–08. doi: 10.1016/j.ygyno.2003.12.029. [DOI] [PubMed] [Google Scholar]
- 16.Townsley CA, Selby R, Siu LL. Systematic review of barriers to the recruitment of older patients with cancer onto clinical trials. J Clin Oncol. 2005;23:3112–24. doi: 10.1200/JCO.2005.00.141. [DOI] [PubMed] [Google Scholar]
- 17.George SL. Reducing patient eligibility criteria in cancer clinical trials. J Clin Oncol. 1996;14:1364–70. doi: 10.1200/JCO.1996.14.4.1364. [DOI] [PubMed] [Google Scholar]
- 18.Holmes DR, Lyonga MJ, Alleyne RS, et al. Increasing minority patient participation in cancer clinical trials using oncology nurse navigation. Am J Surg. 2011;203:415–22. doi: 10.1016/j.amjsurg.2011.02.005. [DOI] [PubMed] [Google Scholar]
- 19.Brown DR, Fouad MN, Basen-Engquist K, et al. Recruitment and retention of minority women in cancer screening, prevention, and treatment trials. Ann Epidemiol. 2000;10(8, Supplement 1):S13–S21. doi: 10.1016/s1047-2797(00)00197-6. [DOI] [PubMed] [Google Scholar]
- 20.Springfield S. Racial and ethnic minorities accrual to NCI clinical trials. Center to Reduce Cancer Health Disparities, National Cancer Institute, NIH; Bethesda, MD: 2010. http://www.nmqf.org/presentations/10SpringfieldSAJCP2.pdf. [Google Scholar]
- 21.Vicini F, Nancarrow-Tull J, Shah C, et al. Increasing accrual in cancer clinical trials with a focus on minority enrollment: The William Beaumont Hospital Community Clinical Oncology Program Experience. Cancer. 2011;117:4764–71. doi: 10.1002/cncr.26094. doi: 10.1002/cncr.26094. [DOI] [PubMed] [Google Scholar]
- 22.Wendler D, Kington R, Madans J, Wye GV, Christ-Schmidt H, et al. Are racial and ethnic minorities less willing to participate in Health Research? PLoS Med. 2006;3(2):e19. doi: 10.1371/journal.pmed.0030019. doi:10.1371/journal.pmed.0030019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Quinn GP, McIntyre J, Gonzalez LE, et al. Improving awareness of cancer clinical trials among Hispanic patients and families: audience segmentation decisions for a media intervention. J Health Commun. 2013 doi: 10.1080/10810730.2013.768723. DOI: 10.1080/10810730.2013.768723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Byrne MM, Tannenbaum SL, Glück S, et al. Participation in cancer clinical trials: why are patients not participating? Med Decis Making. 2013;34:116–26. doi: 10.1177/0272989X13497264. [DOI] [PubMed] [Google Scholar]
- 25.Braunstein JB, Sherber NS, Schulman SP, et al. Race, medical researcher distrust, perceived harm, and willingness to participate in cardiovascular prevention trials. Medicine (Baltimore) 2008;87:1–9. doi: 10.1097/MD.0b013e3181625d78. [DOI] [PubMed] [Google Scholar]
- 26.Schapira MM, Mackenzie ER, Lam R, et al. Breast cancer survivors willingness to participate in an acupuncture clinical trial: a qualitative study. Support Care Cancer. 2013 Dec 21; doi: 10.1007/s00520-013-2073-3. 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. [2/10/15]; http://www.census.gov/prod/cen2010/briefs/c2010br-04.pdf.
- 28. [2/10/15]; http://seer.cancer.gov/csr/1975_2011/results_merged/topic_race_ethnicity.pdf.
- 29.Hawk ET, Habermann EB, Ford JG, et al. Five National Cancer Institute-designated cancer centers' data collection on racial/ethnic minority participation in therapeutic trials: A current view and opportunities for improvement. Cancer. 2014 Apr 1;120(Suppl 7):1113–21. doi: 10.1002/cncr.28571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fouad MN, Partridge E, Green BL, et al. Minority recruitment in clinical trials: a conference at Tuskegee, researchers and the community. Ann Epidemiol. 2000;10(8 Suppl):S35–S40. doi: 10.1016/s1047-2797(00)00199-x. [DOI] [PubMed] [Google Scholar]
- 31. http://www.nbcnews.com/health/nih-finally-makes-good-henrietta-lacks-family-its-about-time-6C10867941.
- 32. [1/23/15]; http://www.nih.gov/news/health/aug2013/nih-07.htm.
- 33.Ford ME, Siminoff LA, Pickelsimer E, et al. Unequal burden of disease, unequal participation in clinical trials: Solutions from African American and Latino community members. Health Soc Work. 2013;38:29–38. doi: 10.1093/hsw/hlt001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fouad MN, Partridge E, Wynn T, et al. Statewide Tuskegee Alliance for clinical trials. A community coalition to enhance minority participation in medical research. Cancer. 2001;91(1 Suppl):237–241. doi: 10.1002/1097-0142(20010101)91:1+<237::aid-cncr11>3.3.co;2-l. [DOI] [PubMed] [Google Scholar]
- 35.Hudson SV1, Harris-Haywood S, Stange KC, Orzano AJ, Crabtree BF. Recruiting minority primary care practices into practice-based research. Med Care. 2006;44:696–700. doi: 10.1097/01.mlr.0000215818.38729.81. [DOI] [PubMed] [Google Scholar]
- 36. [2/10/15]; http://www.census.gov/population/projections/data/national/2014.html.
- 37. [2/10/15]; http://aamcdiversityfactsandfigures.org/section-ii-current-status-of-us-physician-workforce/
- 38. [3/5/15]; [[ http://minorityhealth.hhs.gov/assets/pdf/checked/part%202.pdf.
- 39.Cottler LB, McCloskey DJ, Aguilar-Gaxiola S, et al. Community needs, concerns and perceptions about health research: Findings from the clinical and translational science award sentinel network. Am J Public Health. 2013;103:1685–92. doi: 10.2105/AJPH.2012.300941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Symonds RP, Lord K, Mitchell AJ, et al. Recruitment of ethnic minorities into cancer clinical trials: experience from the front lines. Br J Cancer. 2012;107:1017–21. doi: 10.1038/bjc.2012.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.