Abstract
Objective
To describe the incidence of acute kidney injury (AKI) requiring renal replacement therapy (“dialysis-requiring AKI”) and the impact on in-hospital mortality among hospitalized adults with HIV infection.
Design
Longitudinal analysis of a nationally representative administrative database.
Methods
We reviewed the Healthcare Cost and Utilization Project’s Nationwide Inpatient Sample Database, a large, nationally representative sample of inpatient hospital admissions, to identify all adult hospitalizations with an associated diagnosis of HIV infection from 2002–2010. We analyzed temporal trends in the incidence of dialysis-requiring AKI and the associated odds of in-hospital mortality. We also explored potential reasons behind temporal changes.
Results
Among 1830041 hospitalizations with an associated diagnosis of HIV infection, the proportion complicated by dialysis-requiring AKI increased from 0.7% in 2002 to 1.35% in 2010. This temporal rise was completely explained by changes in demographics and increase in concurrent comorbidities and procedure utilization. The adjusted odds of in-hospital mortality associated with dialysis-requiring AKI also increased over the study period, from 1.45 (95% CI 0.97–2.12) in 2002 to 2.64 (95% CI 2.04–3.42) in 2010.
Conclusions
These data suggest that the incidence of dialysis-requiring AKI among hospitalized adults with HIV infection continues to increase, and that severe AKI remains a significant predictor of in-hospital mortality in this population. The increased incidence of dialysis-requiring AKI was largely explained by aging of the HIV population and increasing prevalence of chronic non-AIDS comorbidities, suggesting that these trends will continue.
Keywords: HIV, acute kidney injury, dialysis, mortality
INTRODUCTION
Over the last three decades, HIV/AIDS has emerged as a major public health challenge.[1][2] With dramatic improvements in survival and disease progression in the combination antiretroviral therapy (ART) era, life expectancy approaches that in the general population, and non-AIDS complications have replaced opportunistic infections as the leading causes of death. [3] HIV infection is associated with increased risk for acute kidney injury (AKI) and chronic kidney disease (CKD). [4] AKI was historically secondary to sepsis and volume depletion, but in the ART era, major AKI risk factors in HIV-positive adults are similar to those in the general population. In addition to traditional risk factors, HIV-positive adults may be susceptible to AKI secondary to medications or co-infections.[5] AKI is also associated with adverse outcomes in HIV-positive adults.[6,7] In an analysis of 17,325 HIV-positive US military veterans hospitalized between 1986 and 2006, patients with AKI had significantly higher rates of mortality, end stage renal disease (ESRD), and cardiovascular events over 5.7 years.[7]
Data evaluating temporal trends in AKI incidence among hospitalized HIV-positive adults are limited in the ART era. A previous study of hospitalizations in New York State showed higher incidence of AKI in the ART era, but was based on a single year of data from the pre-ART and ART era.[6] In a large cohort of HIV-positive military veterans followed between 1984 and 2007, there was decrease in overall incidence of AKI following ART introduction, but a corresponding increase in incidence of AKI requiring dialysis.[8] Finally, in a single-center, ART-era cohort study from London, the incidence of AKI remained relatively stable between 1998–2005, with a decrease in incidence among patients engaged in care.[9]
We utilized a large, nationally representative database to estimate the incidence of severe AKI requiring renal replacement therapy (“dialysis-requiring AKI”) among hospitalized HIV-positive adults between 2002 and 2010 and to evaluate the impact of dialysis-requiring AKI on in-hospital mortality.
METHODS
We extracted our study cohort from the Nationwide Inpatient Sample (NIS) of the Healthcare Cost and Utilization Project (HCUP), Agency for Healthcare Research and Quality.[10] We selected the period from 2002–2010 based on complete data availability and approval of current first-line ART. We queried the database using International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) diagnosis codes 042/V08 for HIV infection. We defined AKI by ICD-9-CM code 584.xx. The dialysis procedure was identified by presence of ICD-9-CM procedure code of 39.95 or diagnosis code of v45.11, v56.0 or v56.1. [11] To avoid misclassification of hospitalizations for chronic hemodialysis initiation, we excluded those with procedure codes for arteriovenous access creation or revision.[12] Similarly, we excluded hospitalizations with dialysis codes but no AKI code, assuming that patients were receiving dialysis for ESRD. This approach has been used previously and has sensitivity of 90.4%, specificity of 93.8%, and positive and negative predictive value of 94.0% and 90.0%, respectively. [11]
We calculated the proportion of hospitalizations with a documented diagnosis of dialysis-requiring AKI for each year from 2002–2010. We extracted demographics, concurrent diagnoses, hospital-level characteristics (geographical region, size, and teaching status) and estimated comorbidity burden and mortality risk using the validated All Patient Refined Diagnosis Related Group (APRDRG) mortality score.[13] Specific diagnoses previously associated with increased risk of AKI were identified by ICD-9-CM codes for CKD, diabetes mellitus, hypertension, HCV, liver disease, sepsis, heart failure, cardiac catheterization, and mechanical ventilation. [14–17]
To explore reasons for temporal changes in incidence of dialysis-requiring AKI, we constructed three sequential logistic regression models (Model 1: Calendar year; Model 2: Year + temporal changes in demographics; Model 3: Year + changes in demographics + changes in diagnoses/procedure).
We utilized survey multivariable logistic regression models to estimate impact of dialysis-requiring AKI on in-hospital mortality. We estimated population-level incidence rates of dialysis-requiring AKI using HIV prevalence estimates from CDC.gov; reliable estimates within demographic subgroups were available for 2008–2010.[18] We utilized SAS 9.3 (SAS Institute Inc. Cary, North Carolina) for all analyses and included designated weight values to produce nationally representative estimates. We considered a two-tailed p value ≤ 0.05 as statistically significant.
RESULTS
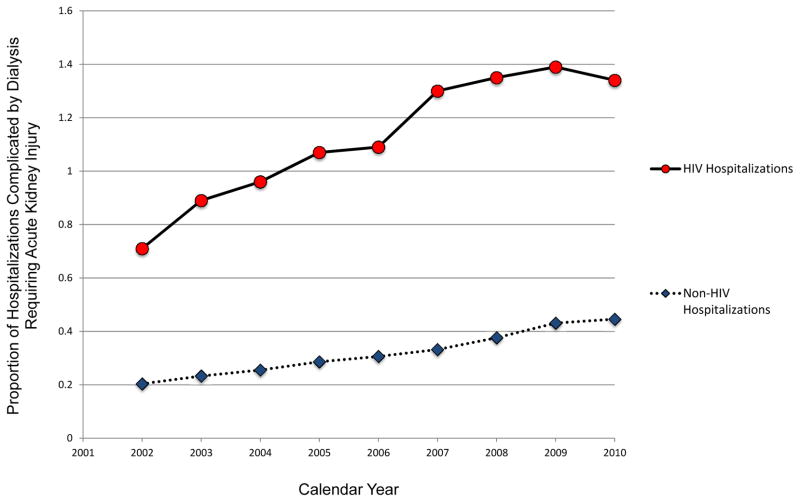
We identified 1,830,041 adult hospitalizations with an associated diagnosis of HIV from 2002–2010. Dialysis-requiring AKI was documented as a complication in 20,695 (1.13%) of these hospitalizations. The proportion of hospitalizations complicated by dialysis-requiring AKI doubled between 2002 and 2010 [1,465/204,121 (0.71%) in 2002 versus 2,830/208,093 (1.36%) in 2010]; however, this proportion was stable between 2007–2010 despite an increase in the absolute number of cases over the same period (Figure 1). For qualitative comparison, similar data are shown for all other adult hospitalizations.
Figure 1.
Temporal Trends in the Incidence of Acute Kidney Injury (AKI) Requiring Renal Replacement Therapy among Hospitalized Adults with and without HIV Infection
Patient characteristics significantly associated with dialysis-requiring AKI (p<0.001) included older age (45.8 vs. 43.5 years in those without AKI); male gender (71.2% vs. 63.8%); African American race (59.5% vs. 44.3%); higher APRDRG risk of mortality score (3.2 vs. 2.3); and chronic comorbidities including diabetes (15.9% vs. 12%), hypertension (38.3% vs. 24.6%), chronic liver disease (15.5% vs. 6.4%), and CKD (18.1% vs. 2.3%). Hospitalizations complicated by dialysis-requiring AKI were more likely to be complicated by mechanical ventilation (51.4% vs. 2.83%) and sepsis (36.9% vs. 5.44%).
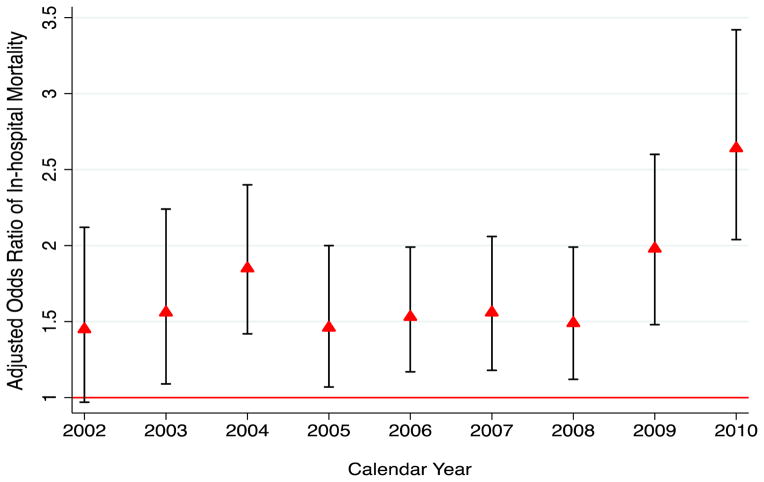
In-hospital mortality in patients with dialysis-requiring AKI increased from 361/1,465 (24.6%) in 2002 to 736/2,830 (26.1%) in 2010. After adjusting for demographics, APRDRG risk of mortality score, acute and chronic comorbidities, and hospital level factors, the adjusted odds ratio increased from 1.45 (95% CI 0.97–2.12) in 2002 to 2.64 (95% CI 2.04–3.42) in 2010 (Figure 2).
Figure 2.
Adjusted Odds of In-Hospital Mortality Associated with Dialysis-requiring Acute Kidney Injury in Hospitalized Adults with HIV infection
In order to explain the observed temporal increase in dialysis-requiring AKI, we constructed a univariable model including only year. This model demonstrated that the odds of dialysis-requiring AKI increased annually by 6% (OR 1.06; 95% CI 1.05–1.07) between 2002 and 2010. Adjustment for patient demographics had minimal effect (adjusted OR 1.05; 95% CI 1.04–1.06.). After adjustment for changes in demographics and concurrent diagnoses (sepsis/myocardial infarction/heart failure) and procedures (cardiac catheterizations/mechanical ventilation) associated with AKI, the impact of year was completely attenuated (adjusted OR 1.003, 95% CI 0.99–1.02; p=0.68).
Using HIV prevalence estimates from CDC.gov, we calculated the population-level incidence rate of dialysis-requiring AKI from 2008–2010 (Supplementary Table 1). The incidence of dialysis-requiring AKI per 1,000 HIV patients was stable over this period. On subgroup analysis, the highest incidence was observed in individuals older than 65 years, in women, and in African-Americans. The estimated population-level incidence increased significantly among HIV-infected African-Americans, from 1.91/1,000 in 2008 to 5.12/1,000 in 2010. There were also significant differences in population-level incidence across geographical regions, with lowest incidence observed in the western United States.
Although our primary objective was to describe temporal trends among hospitalized adults with HIV infection, we also explored the comparison with trends in the general population. As demonstrated in Figure 1, the incidence of dialysis-requiring AKI among hospitalized adults was notably higher in the setting of HIV infection. In unadjusted comparison of demographic and clinical characteristics between HIV-positive and HIV-negative adults with dialysis-requiring AKI (Supplementary Table 2), those with HIV were younger, more likely to be African-American and to have documented HCV infection, and less likely to have diabetes mellitus or hypertension. There were also notable differences in the distribution of concurrent acute diagnoses and procedures, including lower prevalence of acute heart failure, cardiac catheterizations and myocardial infarctions, but higher prevalence of sepsis and mechanical ventilation in HIV-positive cases. (Supplementary Table 2)
DISCUSSION
In a large, nationally representative sample of hospital admissions, we found a two-fold increase in incidence of dialysis-requiring AKI and an accompanying increase in associated inhospital mortality among hospitalized HIV-positive adults between 2002–2010. The increased incidence of dialysis-requiring AKI was largely explained by temporal changes in severity of acute illness and prevalence of chronic comorbidities known to be associated with AKI. This is consistent with reports in the general population, including a recent study demonstrating an increase in the population level incidence of dialysis-requiring AKI from 222 to 533 per million person-years between 2000 and 2009, an increase of 10% per year.[12]
The epidemiology of HIV/AIDS has undergone a substantial shift with ART, with dramatic increase in life expectancy of HIV-positive adults.[19] The age shift in prevalence and incidence of HIV infection has resulted in a growing burden of age-related comorbidities, along with an increase in the use of procedures including cardiac catheterizations and mechanical ventilation. We could account for the increased incidence in dialysis-requiring AKI with temporal changes in demographics, comorbidities, and procedures, suggesting that their increased prevalence accounted for this observed temporal increase. Although we cannot exclude more liberal use of acute dialysis over time,[20] in the general population both dialysis-requiring and laboratory-defined AKI have been increasing in incidence.[21] In addition, the adjusted mortality associated with dialysis-requiring AKI increased over the study period, suggesting that affected patients were sicker.
We also estimated the population-level incidence rate of dialysis-requiring AKI between 2008–2010. As seen in the general population, the highest incidence was in the age group ≥ 65 and among African-Americans, with a significant rise in incidence among African-Americans over this period (Supplementary Table 1) [22,23]. Of note, the mean age of HIV-positive adults with dialysis-requiring AKI was significantly lower than the mean age reported in studies in the general population (45.8 vs. 63.4–75 years) [22,23] and that observed among HIV-negative adults with dialysis-requiring AKI in NIS (64.3 years) This suggests that HIV-positive adults may develop dialysis-requiring AKI at a younger age than the general population. We also observed higher incidence among HIV-positive women. Results in the general population are heterogeneous, suggesting that differences in incidence by sex vary across populations and clinical settings.[22,24] In addition, we observed differences in estimated population-level incidence of dialysis-requiring AKI among HIV-infected adults by geographic region. Regional variation has also been demonstrated in the general population.[25]
To the best of our knowledge, this is the first study to use a nationally representative database to analyze temporal trends in incidence and implications of dialysis-requiring AKI among hospitalized HIV-positive adults in the ART era. The use of a nationally representative sample allowed for accurate estimates, excellent power, and generalizability. We also recognize several limitations, the foremost being the use of administrative data rather than laboratory measurements to define dialysis-requiring AKI. However, dialysis-requiring AKI codes have been found to have excellent validity [11]. Additionally, we could not discriminate between continuous versus intermittent renal replacement therapy and de novo AKI versus acute-on-chronic kidney disease. Because data were de-identified, we could not identify individuals with multiple hospitalizations or recurrent episodes of dialysis-requiring AKI.
In summary, we observed a nearly two-fold increase in incidence of dialysis-requiring AKI among hospitalized HIV-positive adults between 2002–2010. This was largely explained by temporal changes in acute illness severity and prevalence of chronic comorbidities known to be associated with AKI. As in the general population, dialysis-requiring AKI was associated with a significant increase in in-hospital mortality among HIV-positive adults. These findings have important public health implications in an aging HIV population.
Supplementary Material
Acknowledgments
Funding Sources: This work was supported in part by funding from the National Institutes of Health to GNN (T32DK00775716) and CMW (R01 DK100272 and P01DK056492).
Footnotes
Disclosures: All authors report no conflict of interest
- Girish N Nadkarni: Study concept and design; Acquisition of data; Analysis and interpretation of data; Drafting of the manuscript; Critical revision of the manuscript for important intellectual content.
- Achint A Patel: Acquisition of data; Statistical Analysis; Drafting of the manuscript; Critical revision of the manuscript for important intellectual content.
- Rabi Yacoub: Analysis and interpretation of data; Drafting of the manuscript; Statistical analysis
- Alexandre M Benjo: Acquisition of data; Critical revision of the manuscript for important intellectual content; Administrative, technical and material support
- Ioannis Konstantinidis: Acquisition of data; Critical revision of the manuscript for important intellectual content; Technical and material support
- Narender Annapureddy: Drafting of the manuscript; Critical revision of the manuscript for important intellectual content; Technical and material support.
- Shiv Kumar Agarwal: Acquisition of data; Drafting of the manuscript; Administrative and material support.
- Priya K Simoes: Drafting of the manuscript; Critical revision of the manuscript for important intellectual content; Technical and material support.
- Sunil Kamat: Acquisition of data; Critical revision of the manuscript for important intellectual content; Material and administrative support.
- Madhav C Menon: Study concept and design; Analysis and interpretation of data; Critical revision of the manuscript for important intellectual content; Material support.
- Christina Wyatt: Study concept and design; Analysis and interpretation of data; Drafting of the manuscript; Critical revision of the manuscript for important intellectual content; Overall study supervision.
References
- 1.Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Murray CJL, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2197–2223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 3.Selik RM, Byers RH, Dworkin MS. Trends in diseases reported on U.S. death certificates that mentioned HIV infection, 1987–1999. J Acquir Immune Defic Syndr 1999. 2002;29:378–387. doi: 10.1097/00126334-200204010-00009. [DOI] [PubMed] [Google Scholar]
- 4.Balow JE. Nephropathy in the context of HIV infection. Kidney Int. 2005;67:1632–1633. doi: 10.1111/j.1523-1755.2005.00254.x. [DOI] [PubMed] [Google Scholar]
- 5.Rao TK, Friedman EA. Outcome of severe acute renal failure in patients with acquired immunodeficiency syndrome. Am J Kidney Dis Off J Natl Kidney Found. 1995;25:390–398. doi: 10.1016/0272-6386(95)90099-3. [DOI] [PubMed] [Google Scholar]
- 6.Wyatt CM, Arons RR, Klotman PE, Klotman ME. Acute renal failure in hospitalized patients with HIV: risk factors and impact on in-hospital mortality. AIDS Lond Engl. 2006;20:561–565. doi: 10.1097/01.aids.0000210610.52836.07. [DOI] [PubMed] [Google Scholar]
- 7.Choi AI, Li Y, Parikh C, Volberding PA, Shlipak MG. Long-term clinical consequences of acute kidney injury in the HIV-infected. Kidney Int. 2010;78:478–485. doi: 10.1038/ki.2010.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li Y, Shlipak MG, Grunfeld C, Choi AI. Incidence and risk factors for acute kidney injury in HIV Infection. Am J Nephrol. 2012;35:327–334. doi: 10.1159/000337151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Roe J, Campbell LJ, Ibrahim F, Hendry BM, Post FA. HIV care and the incidence of acute renal failure. Clin Infect Dis Off Publ Infect Dis Soc Am. 2008;47:242–249. doi: 10.1086/589296. [DOI] [PubMed] [Google Scholar]
- 10.HCUP Overview. Healthcare Cost and Utilization Project (HCUP); 2009. http://www.HCUP-us.ahrq.gov/overview.jsp. [Google Scholar]
- 11.Waikar SS, Wald R, Chertow GM, Curhan GC, Winkelmayer WC, Liangos O, et al. Validity of International Classification of Diseases, Ninth Revision, Clinical Modification Codes for Acute Renal Failure. J Am Soc Nephrol JASN. 2006;17:1688–1694. doi: 10.1681/ASN.2006010073. [DOI] [PubMed] [Google Scholar]
- 12.Hsu RK, McCulloch CE, Dudley RA, Lo LJ, Hsu C. Temporal changes in incidence of dialysis-requiring AKI. J Am Soc Nephrol JASN. 2013;24:37–42. doi: 10.1681/ASN.2012080800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baram D, Daroowalla F, Garcia R, Zhang G, Chen JJ, Healy E, et al. Use of the All Patient Refined-Diagnosis Related Group (APR-DRG) Risk of Mortality Score as a Severity Adjustor in the Medical ICU. Clin Med Circ Respir Pulm Med. 2008;2:19–25. doi: 10.4137/ccrpm.s544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348:1546–1554. doi: 10.1056/NEJMoa022139. [DOI] [PubMed] [Google Scholar]
- 15.Lee DS, Donovan L, Austin PC, Gong Y, Liu PP, Rouleau JL, et al. Comparison of coding of heart failure and comorbidities in administrative and clinical data for use in outcomes research. Med Care. 2005;43:182–188. doi: 10.1097/00005650-200502000-00012. [DOI] [PubMed] [Google Scholar]
- 16.Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, De Simone G, et al. Executive summary: heart disease and stroke statistics--2010 update: a report from the American Heart Association. Circulation. 2010;121:948–954. doi: 10.1161/CIRCULATIONAHA.109.192666. [DOI] [PubMed] [Google Scholar]
- 17.Wunsch H, Linde-Zwirble WT, Angus DC, Hartman ME, Milbrandt EB, Kahn JM. The epidemiology of mechanical ventilation use in the United States. Crit Care Med. 2010;38:1947–1953. doi: 10.1097/CCM.0b013e3181ef4460. [DOI] [PubMed] [Google Scholar]
- 18.Center for Disease Control.
- 19.Brooks JT, Buchacz K, Gebo KA, Mermin J. HIV infection and older Americans: the public health perspective. Am J Public Health. 2012;102:1516–1526. doi: 10.2105/AJPH.2012.300844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Siew ED, Davenport A. The growth of acute kidney injury: a rising tide or just closer attention to detail? Kidney Int. 2015;87:46–61. doi: 10.1038/ki.2014.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hsu C-Y, McCulloch CE, Fan D, Ordoñez JD, Chertow GM, Go AS. Community-based incidence of acute renal failure. Kidney Int. 2007;72:208–212. doi: 10.1038/sj.ki.5002297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liangos O, Wald R, O’Bell JW, Price L, Pereira BJ, Jaber BL. Epidemiology and outcomes of acute renal failure in hospitalized patients: a national survey. Clin J Am Soc Nephrol CJASN. 2006;1:43–51. doi: 10.2215/CJN.00220605. [DOI] [PubMed] [Google Scholar]
- 23.Xue JL, Daniels F, Star RA, Kimmel PL, Eggers PW, Molitoris BA, et al. Incidence and mortality of acute renal failure in Medicare beneficiaries, 1992 to 2001. J Am Soc Nephrol JASN. 2006;17:1135–1142. doi: 10.1681/ASN.2005060668. [DOI] [PubMed] [Google Scholar]
- 24.Hsu RK, McCulloch CE, Dudley RA, Lo LJ, Hsu C. Temporal changes in incidence of dialysis-requiring AKI. J Am Soc Nephrol JASN. 2013;24:37–42. doi: 10.1681/ASN.2012080800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hsu RK, McCulloch CE, Ku E, Dudley RA, Hsu C-Y. Regional variation in the incidence of dialysis-requiring AKI in the United States. Clin J Am Soc Nephrol CJASN. 2013;8:1476–1481. doi: 10.2215/CJN.12611212. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.