Abstract
Objective
Identify diagnostic risk factors of mania/hypomania in the offspring of parents with bipolar disorder (“high-risk offspring”).
Method
High-risk offspring aged 6-18 years (n=391) and demographically-matched offspring (n=248) of community parents without bipolar disorder were assessed longitudinally with standardized diagnostic instruments by staff blind to parental diagnoses. Follow-up assessments were completed in 91% of the offspring (mean interval 2.5 years; mean duration 6.8 years).
Results
High-risk offspring, as compared to community offspring, had significantly higher rates of subthreshold (hypo)manic (13.3% vs. 1.2%, p<.0001), manic/hypomanic (9.2% vs. 0.8%, p=.0003) and major depressive episodes (32.0% vs. 14.9%, p<.0001). They also had higher rates of attention-deficit hyperactivity (30.7% vs. 18.2%, p=.01), disruptive behavior (27.4% vs. 15.3%, p=.03), anxiety (39.9% vs. 21.8%, p=.0002), and substance use disorders (20.0% vs. 10.1%, p=.008), but not unipolar major depressive disorder (major depression with no bipolarity; 18.9% vs. 13.7%; p=.10). Multivariate Cox regressions in the high-risk offspring showed that subthreshold (hypo)manic episodes (Hazard Ratio 2.29, p=.03), major depressive episodes (Hazard Ratio 1.99, p=.05), and disruptive behavior disorders (Hazard Ratio 2.12, p=.03) were associated with subsequent mania/hypomania. Only subthreshold (hypo)manic episodes (Hazard Ratio 7.57, p<.0001) were associated when analyses were restricted to prospective data.
Conclusions
Subthreshold (hypo)manic episodes were a diagnostic risk factor for the development of mania/hypomania in the offspring of parents with bipolar disorder, and should be a target for clinical assessment and future treatment research. Major depressive episodes and disruptive behavior disorders are also indications for close clinical monitoring of emergent bipolarity in high-risk offspring.
Introduction
Most adults with bipolar disorder recall having mood symptoms prior to age 18 and there is growing evidence that those with childhood or adolescent onset have a worse prospective course of mood symptomatology and higher rates of comorbid psychiatric illness as compared to those with adult-onset.(1-3) Furthermore, there is on average a lag of more than a decade between the onset of impairing mood symptoms and a bipolar diagnosis in bipolar adults with onset during youth.(4) Improved identification of bipolar disorder in childhood and adolescence may increase the opportunity to apply evidence-based treatments in earlier phases of the illness, which in turn has the potential to improve long-term course and outcomes. Given that bipolar disorder runs in families(5) and has a strong genetic basis(6), the offspring of parents with bipolar disorder are an excellent population to examine diagnostic precursors of bipolar disorder.
Most studies of the child and adolescent offspring of bipolar parents show that the offspring have elevated rates of bipolar disorder, major depression, and anxiety disorders compared to control groups.(7, 8) However, results are mixed regarding attention-deficit hyperactivity disorder, oppositional defiant disorder, and conduct disorder.(9-14) There are only a few high-risk studies with longitudinal data, but low numbers of bipolar disorder in the high-risk group limit their ability to identify predictors of developing bipolar disorder. Depression was found to precede manic/hypomanic episodes in nearly all high-risk offspring with bipolar disorder in two longitudinal studies, though the mean age at intake was 16.5 years in both of these studies.(15, 16) Episodic symptoms such as crying, anxiety, hyper-alertness, and decreased sleep in childhood preceded the onset of mania in a small sample of offspring of Amish parents with bipolar disorder, but power limitations precluded formal statistical analyses.(17)
The Pittsburgh Bipolar Offspring Study (BIOS) is the largest study to date of offspring of parents with bipolar disorder. A unique feature of BIOS is that offspring were assessed for subthreshold episodes of manic symptomatology using a priori operationalized criteria from the Course and Outcome of Bipolar Youth (COBY) study.(18) Prior results from the intake assessment demonstrated that the offspring of parents with bipolar disorder had higher rates of anxiety, bipolar-I, and bipolar-spectrum (bipolar-I, II or bipolar disorder not otherwise specified) disorders as compared to control offspring.(12) A diagnosis of a bipolar-spectrum disorder in the high-risk offspring was associated with younger parental age at the child's birth, older offspring age, higher rates of anxiety and disruptive behavior disorders in the offspring, and both parents having a bipolar diagnosis.(19)
The primary aims of this article are: (1) to confirm and extend the findings regarding diagnostic differences between the offspring of parents with bipolar disorder (subsequently referred to as “high-risk offspring”) vs. offspring of community control parents now that longitudinal data are included and the mean age of the sample is 18 years old; and (2) to describe the developmental trajectory of mood episodes and identify diagnostic precursors of full threshold bipolar disorder (defined as the presence of manic, mixed, or hypomanic episodes, subsequently referred to as mania/hypomania) in the offspring of parents with bipolar disorder. Based on the studies noted above, we hypothesized that subthreshold (hypo)mania, depression, anxiety, and disruptive behavior disorders would be associated with future mania/hypomania.
Methods
The methods of BIOS have been described in detail in prior reports.(12) The study was approved by the University of Pittsburgh Institutional Review Board prior to the start of the study.
Sample
The sample was recruited via the parent probands. Parents with bipolar disorder were recruited via advertisement (53%), other research studies (31%), and outpatient clinics (16%). Parents with bipolar disorder had to meet DSM-IV criteria for bipolar-I or bipolar-II disorders and live within 200 miles of Pittsburgh. Exclusion criteria were a lifetime diagnosis of schizophrenia, mental retardation, a mood disorder secondary to medical illness, or substance or medication use. Control parents were recruited from the community using random digit dialing and were group matched to the bipolar parents by age, sex, and neighborhood. Control parents could not have a parent or sibling with bipolar disorder, and the biological co-parent could not have bipolar disorder. The study included all offspring of the parent probands who were aged 6 to 18 years (including siblings and half-siblings), unless the child had mental retardation.
Procedures
Study procedures were initiated after obtaining informed consent from the parents and assent from the children.(12) Parent probands and participating biological co-parents (31%) were assessed for DSM-IV disorders by direct interview using the Structured Clinical Interview for DSM-IV (SCID) and the attention-deficit hyperactivity disorder, oppositional defiant disorder, conduct disorder, and separation anxiety disorder sections of the Schedule for Affective Disorders and Schizophrenia for School Age Children-Present and Lifetime Version (KSADS-P/L). The psychiatric history of non-participating biological co-parents was obtained from the parent proband using the Family-History Research Diagnostic Criteria method (20) plus attention-deficit hyperactivity disorder, oppositional defiant disorder, conduct disorder, and separation anxiety items from the KSADS P/L.
At intake, parents were interviewed about their child offspring and the children were directly interviewed using the KSADS P/L for non-mood disorders and the K-SADS Mania Rating Scale and the depression items from the KSADS-Present Version. Symptoms that are criteria for more than one diagnosis (e.g. distractibility) were not rated as fulfilling criteria for a mood disorder unless it had its onset or significantly intensified during a period of abnormal mood. Subthreshold (hypo)mania was diagnosed using the bipolar disorder not otherwise specified criteria from the COBY study (18) and was defined by distinct periods of abnormally elevated, expansive, or irritable mood that met the following four criteria: (1) at least two DSM-IV manic symptoms (three if the mood is irritable only) that were clearly associated with the onset of abnormal mood; (2) a clear change in functioning associated with the onset of these affective symptoms; (3) the presence of the elated and/or irritable mood and manic symptoms for a significant part of the day (a minimum of four hours, though this did not necessarily need to be expressed consecutively); (4) a minimum of four days (not necessarily consecutive) meeting criteria 1-3 over the subject's lifetime.
Socioeconomic status was determined using the Hollingshead scale. (21)
Follow-up evaluations were performed approximately every two years using the same diagnostic instruments cited above for parents and child offspring younger than age 19. Offspring aged 19 and older were assessed using the SCID for non-mood disorders and the KSADS-Mania Rating Scale and depression items from the KSADS-Present Version. If a participant was not able to complete an interview at the two year interval, attempts to schedule and complete the evaluation would continue unless the participant or parent/guardian asked to withdraw from the study. Follow-up evaluations focused on assessment of the time interval since the prior interview.
Assessments were performed by interviewers with Bachelors or Masters Degrees who had intensive training with the diagnostic instruments and were required to achieve 80% agreement with a certified rater. Interviewers who assessed offspring were blind to the diagnosis of the parents, as different interviewers were used to assess the parents. All information was presented to a child psychiatrist, who reviewed the data to confirm diagnoses. Psychiatrists were blind to parental diagnoses. As per KSADS instructions, all available data were used to assign summary symptom and diagnostic scores, and discrepant information was discussed at case conference with the psychiatrist.
Diagnostic reliability was assessed using audiotapes of 44 actual BIOS assessments which were rated by 2 to 8 BIOS interviewers (mean 5.4). The κ statistic for diagnostic reliability was 0.86 for bipolar-spectrum disorders, 0.77 for bipolar-I/II vs. bipolar disorder not otherwise specified vs. no bipolar disorder, 0.64 for major depressive episode, 0.71 for any depressive episode, 0.86 for attention-deficit hyperactivity disorder, 0.78 for anxiety disorders, 0.84 for oppositional defiant disorder and/or conduct disorder, and 1.0 for substance use disorders.
Age of onset of specific disorders and mood episodes was set to the estimated age that the participant met full DSM-IV criteria. In order to be consistent with other longitudinal high-risk studies, the onset of full threshold bipolar disorder in the offspring was when they first met DSM-IV criteria for a manic, mixed, or hypomanic episode. The age of onset of bipolar spectrum disorder was set to be the age of the first time the participant met criteria for subthreshold (hypo)mania or full threshold bipolar disorder.
Statistical Analyses
Comparisons of demographic and clinical characteristics were evaluated between parent and biological co-parent groups using t, and χ2 tests. Comparisons between offspring groups used mixed logistic regression models in order to control for within family correlation. Demographic variables that showed group differences at a level of p<0.2 were included as potential covariates in subsequent models comparing diagnostic differences between the high-risk and control offspring. Potential covariates were entered in a forward stepwise approach (criterion p<0.2 for entry and p<0.1 for retention used for all stepwise models). Mixed regression models controlling for parental psychopathology were also used to compare diagnostic differences among the offspring of bipolar parents and three different control offspring groups: (1) all control offspring; (2) the offspring of control parent probands who had a lifetime diagnosis of an Axis I disorder; and (3) the offspring of healthy control parent probands. Potential covariates were entered in a forward stepwise approach and included the demographic variables from the prior analyses, as well as parental proband and co-parent non-bipolar diagnoses. Offspring groups were compared on the cumulative risk of developing mania/hypomania, and any bipolar spectrum disorder (bipolar I, II or not otherwise specified) using Kaplan-Meier survival analyses.
Diagnostic precursors of mania/hypomania were evaluated in the high-risk offspring using Cox Regression Models that included family membership as a random effect. Diagnostic factors that were associated with hazard of developing mania/hypomania at a level of p<0.2 in univariate models were included in a stepwise multivariate Cox regression with retention criteria of p<0.1. Since mania/hypomania would only be diagnosed in an offspring with a prior substance use disorder if there was clear and convincing evidence that the two disorders were independent, the temporal association between the two conditions may have been distorted. Therefore, we did not include substance use disorders in the multivariate models. Potential confounding factors were then evaluated by adding to them to the model one at a time, and were retained if they significantly affected results (defined as > 15% change in the hazard ratio of diagnostic factors retained in the model). Potential confounding factors were as follows: offspring age at intake; offspring age at last assessment; year of intake; number of assessments; duration of follow-up; whether the first follow-up assessment occurred within 3 years of intake; whether the second follow-up assessment occurred within 5 years of intake; offspring sex; offspring race; socioeconomic status; parent proband sex; parent proband age at onset of their own bipolar disorder; and parent probands bipolar subtype (I or II). Sensitivity analyses repeating the Cox regressions using the same methodology were performed in the subset of high-risk offspring, with follow-up on those who did not have a history of mania/hypomania at intake. In order to minimize the influence of recall bias, mood episodes and diagnoses were only considered to precede the onset of mania/hypomania in the sensitivity analyses if they were diagnosed at an assessment prior to the assessment at which mania/hypomania was identified.
Results
Participants
There were 391 offspring of 236 parents with bipolar disorder (bipolar-I = 170; bipolar-II = 66) and 248 offspring of 141 community control parents. Two community control parents developed bipolar disorder over follow-up and were reassigned to the bipolar disorder group. One additional bipolar disorder family was entered into the study after the initial analyses, and one child of a parent with bipolar disorder was determined to have mental retardation and was removed from the study.
At least one follow-up visit was completed in 90.9% of the offspring, and follow-up rates did not differ between offspring groups (Table 1). The initial follow-up assessment was completed “on-time” (within three years of intake) in 78.6% of offspring, with no difference between offspring groups. Though not statistically significant, the rates of second follow-up assessments that were on-time (within five years of intake) were lower in the high-risk offspring versus the community offspring (63.4% vs. 71.8%). There were no differences between the high-risk offspring and control offspring in the mean (± standard deviation) number of follow-up assessments (2.7 ± 1.3 vs. 2.7 ± 1.2; F=0.28, p=0.6), duration of follow-up (6.8 ± 2.2 vs. 6.9 ± 2.0 years; F=0.01, p=0.9), or duration between assessments (2.5 ± 1.1 vs. 2.4 ± 0.8 years; F=1.75, p=0.2).
Table 1. Offspring Demographic Factors.
| All Offspring | ||||
|---|---|---|---|---|
| High-risk offspring (n=391) |
Community Control Offspring (n=248) |
Statistic (F)† |
p-value | |
| % | ||||
| Sex (Female) | 48.9% | 54.0% | 1.63 | .20 |
| Race (White) | 81.1% | 74.2% | 3.33 | .07 |
| Living Status (with both biological parents) | 41.7% | 62.1% | 13.4 | .0003 |
| Had at least 1 follow-up assessment | 91.3% | 90.3% | 0.01 | 0.9 |
| 1st follow-up assessment completed within 3 years of intake date | 78.5% | 78.6% | 0.72 | .40 |
| 2nd follow-up assessment completed within 5 years of intake date | 63.4% | 71.8% | 2.74 | .10 |
| mean ± standard deviation | ||||
| Age at Intake | 11.9 ± 3.7 | 11.8 ± 3.6 | 0.06 | .8 |
| Age at Last Assessment | 18.1 ± 4.8 | 18.0 ± 4.5 | 0.00 | 1 |
| Mother's age at offspring's birth | 26.7 ± 5.8 | 28.3 ± 5.6 | 4.67 | .03 |
| Father's age at offspring's birth | 29.5 ± 7.6 | 30.4 ± 7.0 | 1.02 | .31 |
Models adjusted for within family correlation
At intake, offspring with follow-up were more likely to be White, living with both biological parents, and have a lifetime diagnosis of a major depressive episode, anxiety disorder and substance use disorder as compared to those with no follow-up. The groups did not differ in sex or rates of bipolar-spectrum disorders, attention-deficit hyperactivity disorder, oppositional defiant disorder, or conduct disorder (eTable1). Offspring with follow-up had higher SES, and older age of their mothers and fathers at the birth of the offspring.
Offspring Demographics
High-risk offspring were less likely to be living with both biological parents and their mother's age at the offspring's birth was significantly younger as compared to community control offspring (Table 1).
Parent Factors
As compared to the control parents, the parents with bipolar disorder were more likely to be White, less likely to be married, were younger, and were of lower SES (eTable 2). Parents with bipolar disorder were more likely to have a history of a major depressive episode, and of a non-mood Axis I disorder, including anxiety, attention-deficit hyperactivity, disruptive behavior (oppositional defiant/conduct disorders), and substance use disorders. These factors were eligible for inclusion in final multivariate models comparing offspring groups.
The biological co-parents of the high-risk offspring were more likely to have an Axis I diagnosis, depression, and substance use disorder (eTable3). There was no difference between offspring groups in the proportion of co-parents who were assessed using the SCID vs. family history methodology.
Offspring Lifetime Diagnoses and Mood Episodes at Last Assessment
The high-risk offspring as compared to the offspring of control parents had significantly higher lifetime rates of nearly all of the disorders and mood episodes examined except for obsessive-compulsive disorder, post-traumatic stress disorder, conduct disorder, and unipolar major and minor depressive disorders (Table 2). When adjusting for parent and co-parent lifetime Axis I diagnoses (Table 3), there was little change in the results, except that unipolar major depressive disorder was significantly higher in the high-risk offspring. When the comparison was limited to high-risk offspring versus offspring of control parent probands who had a lifetime Axis I disorder, unipolar depression, attention-deficit hyperactivity disorder, and disruptive behavior disorders did not differ between groups.
Table 2. Offspring Lifetime Diagnoses at Last Assessment.
| Offspring of parents with bipolar disorder (n=391) |
Offspring of community control parents (n=248) |
Stat (F)† |
p-value (adjusted for demographics) |
|
|---|---|---|---|---|
| Any axis I disorder | 74.2% | 48.4% | 29.9 | <.0001 |
| Any mood disorder | 48.3% | 22.6% | 30.2 | <.0001 |
| Any bipolar spectrum disorder | 19.2% | 2.0% | 31.5 | <.0001 |
| Bipolar-I disorder | 3.8% | 0.4% | 6.84 | .009 |
| Bipolar-II disorder | 4.6% | 0.4% | 9.39 | .002 |
| Bipolar disorder not otherwise specified | 10.7% | 1.2% | 18.2 | <.0001 |
| Any unipolar depressive disorder | 29.2% | 20.6% | 4.40 | .04 |
| Major depressive disorder | 18.9% | 13.7% | 2.68 | .10 |
| Minor depressive disorder* | 10.2% | 6.9% | 0.94 | .33 |
| Mood episodes | ||||
| Manic, mixed, or hypomanic | 9.2% | 0.8% | 13.2 | .0003 |
| Subthreshold hypo/manic‡ | 13.3% | 1.2% | 23.5 | <.0001 |
| Any depressive episode | 46.3% | 21.8% | 29.5 | <.0001 |
| Major depressive | 32.0% | 14.9% | 20.3 | <.0001 |
| Minor depressive | 27.6% | 10.1% | 26.0 | <.0001 |
| Any non-mood Axis I disorder | 67.3% | 42.7% | 26.2 | <.0001 |
| Any anxiety disorder | 39.9% | 21.8% | 20.2 | <.0001 |
| Generalized anxiety disorder | 20.5% | 6.9% | 25.8 | <.0001 |
| Social phobia | 12.5% | 6.9% | 5.48 | .02 |
| Separation anxiety disorder | 17.1% | 6.9% | 11.6 | .001 |
| Panic disorder | 6.9% | 2.4% | 5.02 | 0.03 |
| Obsessive compulsive disorder | 5.4% | 2.4% | 2.79 | .10 |
| Posttraumatic stress disorder | 8.4% | 5.6% | 0.75 | .39 |
| Attention-deficit hyperactivity disorder | 30.7% | 18.1% | 6.06 | .01 |
| Disruptive Behavior Disorder | 27.4% | 15.3% | 4.85 | .03 |
| Oppositional Defiant Disorder | 25.3% | 12.9% | 5.87 | .02 |
| Conduct Disorder | 9.5% | 5.7% | 0.91 | .34 |
| Substance Use Disorder | 19.9% | 10.1% | 10.1 | .002 |
Forward stepwise models adjusted for family membership and the following pool of potential covariates (p<0.2 for entry, p<0.1 for retention): race, living with both biological parents, mother's age at child's birth, proband age at intake, 2nd follow-up assessment completed within 5 years of intake date, and socioeconomic status.
Dysthymia or depressive disorder not otherwise specified
Subthreshold (hypo)manic episodes not diagnosed after onset of manic, mixed or hypomanic episodes
Table 3. Adjusted odds ratios comparing diagnostic rates between high-risk offspring and control offspring groups.
| High-risk offspring (n=391) vs. offspring of all control parents (n=248)† | High-risk offspring (n=391) vs. offspring of community control parents who had a lifetime Axis I disorder (n=149)† | High-risk offspring (n=391) vs. offspring of healthy community control parents (n=99)‡ | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Hazard Ratio | 95% Confidence Interval | p-value | Hazard Ratio | 95% Confidence Interval | p-value | Hazard Ratio | 95% Confidence Interval | p-value | |
| Any Axis I disorder | 2.15 | 1.39, 3.34 | 0.0006 | 2.13 | 1.31, 3.44 | 0.002 | 3.94 | 2.30, 6.74 | <0.0001 |
| Any mood disorder | 2.68 | 1.64, 4.37 | <0.0001 | 2.60 | 1.53, 4.42 | 0.0004 | 4.13 | 2.15, 7.93 | <0.0001 |
| Bipolar spectrum disorders | 10.58 | 4.15, 26.93 | <0.0001 | 10.94 | 3.34, 35.81 | <0.0001 | 10.03 | 2.37, 42.46 | 0.002 |
| Bipolar I / II disorders | 11.34 | 2.69, 47.82 | 0.001 | 13.64 | 1.84, 101.05 | 0.01 | 9.03 | 1.22, 67.14 | 0.03 |
| Unipolar depressive disorders | 1.47 | 0.9, 2.40 | 0.1 | 1.38 | 0.82, 2.32 | 0.2 | 2.22 | 1.17, 4.23 | 0.02 |
| Unipolar major depressive disorder | 1.70 | 1.05, 2.77 | 0.03 | 1.53 | 0.89, 2.65 | 0.1 | 1.79 | 0.87, 3.69 | 0.1 |
| Any anxiety disorder | 1.67 | 1.02, 2.72 | 0.04 | 1.83 | 1.07, 3.14 | 0.03 | 2.69 | 1.45, 4.97 | 0.002 |
| Social phobia, separation anxiety and/or generalized anxiety disorders | 2.03 | 1.23, 3.33 | 0.005 | 2.18 | 1.25, 3.81 | 0.006 | 2.80 | 1.49, 5.25 | 0.002 |
| Attention-deficit hyperactivity disorder | 1.63 | 1.08, 2.47 | 0.02 | 1.25 | 0.79, 1.97 | 0.3 | 3.68 | 1.75, 7.72 | 0.0006 |
| Disruptive behavior disorders | 1.90 | 1.11, 3.25 | 0.02 | 1.73 | 0.93, 3.20 | 0.08 | 2.50 | 1.11, 5.60 | 0.03 |
| Oppositional defiant disorder | 2.20 | 1.25, 3.86 | 0.006 | 1.79 | 0.95, 3.35 | 0.07 | 3.86 | 1.47, 10.10 | 0.006 |
| Conduct disorder | 1.75 | 0.68, 4.52 | 0.2 | 1.34 | 0.55, 3.25 | 0.5 | 0.82 | 0.33, 2.00 | 0.7 |
| Substance use disorders | 4.49 | 1.86, 10.81 | 0.0009 | 4.36 | 1.74, 10.92 | 0.002 | 2.13 | 0.88, 5.17 | 0.09 |
Forward stepwise models adjusted for family membership and the following pool of potential covariates (p<0.2 for entry, p<0.1 for retention): race, sex, living with both biological parents, mother's age at child's birth, proband age at intake, proband marital status, 2nd follow-up assessment completed within 5 years of intake date, socioeconomic status, proband parent diagnoses of major depression, anxiety disorder, attention-deficit hyperactivity disorder, disruptive behavior disorder, and substance use disorders, and biological co-parent diagnoses of depressive disorder, disruptive behavior disorder and substance use disorder.
Forward stepwise models as above excluding proband parent diagnostic variables.
Onset of Bipolar Disorder
The high-risk offspring had a substantially higher likelihood of having a bipolar-spectrum disorder (Figure 1a) and mania/hypomania (Figure 1b) as compared to the offspring of controls. The cumulative rate of bipolar spectrum disorders at age 21 estimated by the Kaplan-Meier analysis was 23.0% in the offspring of the parents with bipolar disorder and 3.2% in the offspring of controls. The estimated cumulative rate of mania/hypomania at age 21 was 12.7% in the high-risk offspring and 1.5% in the control offspring.
Figure 1.
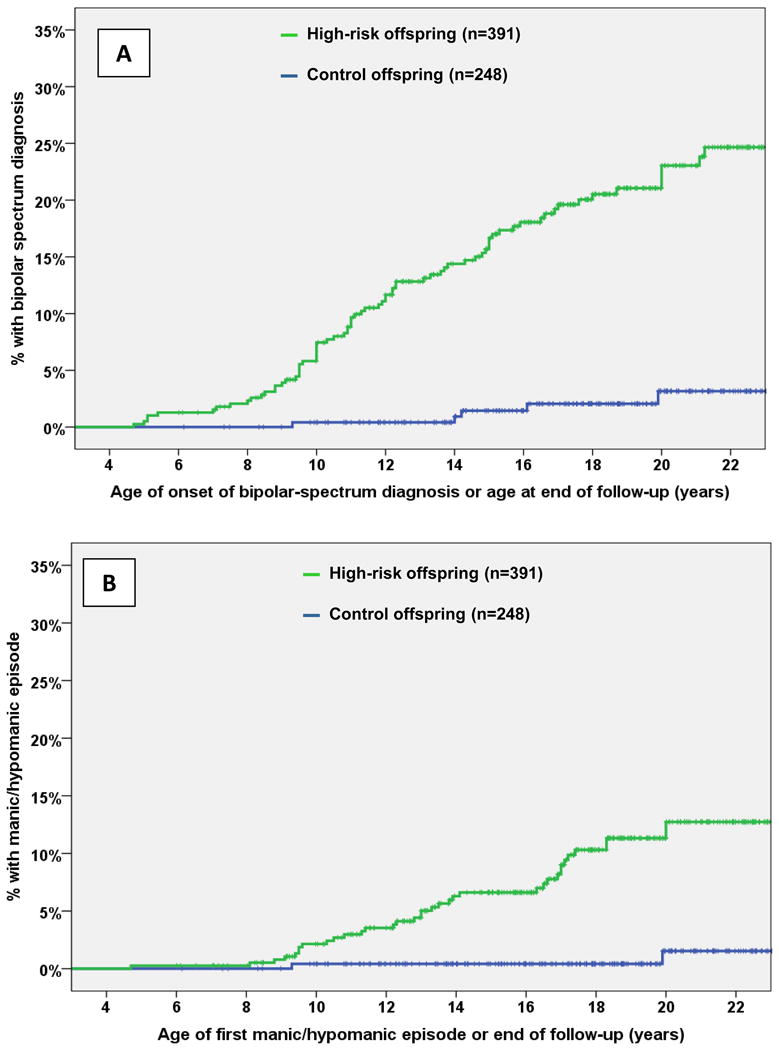
Cumulative rates by age of onset of bipolar spectrum disorders* (A) and mania/hypomania (B)
*Includes bipolar-I and II disorders and bipolar disorder not otherwise specified
Figure 1A: High-risk offspring > Control offspring; Log-Rank χ2 = 40.2; p = 2.3 × 10-10
Figure 1B: High-risk offspring > Control offspring; Log-Rank χ2 = 19.2; p = 1.2 × 10-5 *Includes bipolar-I and II disorders and bipolar disorder not otherwise specified
In the offspring of parents with bipolar disorder, the mean age of onset of mania/hypomania was 13.4 ± 3.8 years and the first onset of bipolar spectrum disorder was 12.1 ± 4.0 years. The mean age of onset of the first major depressive episode was 13.7 ± 4.0 years and the first onset of any depressive episode (major depressive episode or minor depression) was 12.5 ± 4.6 years. Of the 15 high-risk offspring who had a manic episode, 5 (33%) had the first episode prior to age 10 and 8 (53%) had it prior to age 12, with the earliest at age 8.1.
Diagnoses preceding first manic or hypomanic episode in offspring of parents with bipolar disorder
Of the 391 offspring of parents with bipolar disorder, 36 had a lifetime history of a manic/hypomanic episode. Of these 36, 25 (69.4%) had a depressive episode and 20 (55.6%) had a major depressive episode prior to the onset of mania/hypomania. A subthreshold (hypo)manic episode preceded the onset of mania/hypomania in 13 (36.1%) of those with a lifetime history of mania/hypomania (Table 4).
Table 4. Association of prior mood episodes and diagnoses with hazard to develop subsequent manic/hypomanic episodes in high-risk offspring.
| Lifetime mania/hypomania (n=36) |
No mania / hypomania (n=355) |
Hazard Ratio† | 95% Confidence Interval | χ2 | p-value | ||
|---|---|---|---|---|---|---|---|
| % onset prior to manic / hypomanic episode | % lifetime at last assessment | % lifetime at last assessment | |||||
| Any mood episode | 77.8% | 100% | 43.1% | 3.56 | (1.62, 7.81) | 10.02 | .002 |
| Any depressive episode | 69.4% | 91.7% | 41.7% | 2.49 | (1.23, 5.07) | 6.37 | 0.01 |
| Major depressive episode | 55.6% | 80.6% | 27.0% | 2.58 | (1.34, 4.98) | 7.96 | 0.005 |
| Subthreshold (hypo)manic episode | 36.1% | * | 11.0% | 3.76 | (1.90, 7.44) | 14.47 | 0.0001 |
| Any non-mood disorder | 80.6% | 97.2% | 64.2% | 2.30 | (1.01, 5.26) | 3.92 | 0.05 |
| Attention-deficit hyperactivity disorder | 41.7% | 44.4% | 28.7% | 2.04 | (1.05, 3.98) | 4.42 | 0.04 |
| Disruptive behavior disorder | 47.2% | 61.1% | 23.9% | 2.88 | (1.49, 5.59) | 9.84 | 0.002 |
| Anxiety disorder | 52.8% | 72.2% | 36.6% | 1.86 | (0.97, 3.59) | 3.47 | 0.06 |
| Substance use disorder | 5.6% | 44.4% | 17.5% | 0.20 | (0.05, 0.83) | 4.90 | 0.03 |
Cox regression models controlling for within family correlation
Subthreshold (hypo)manic episodes not systematically assessed after onset of mania/hypomania.
Cox regressions showed that any depressive episode, major depressive episode, subthreshold (hypo)manic episode, attention-deficit hyperactivity disorder, and disruptive behavior disorder were associated with an elevated hazard of developing mania/hypomania, while substance use disorders were associated with a reduced hazard (Table 4). The associations between potential confounding variables and risk of developing mania/hypomania are listed in eTable 4. The multivariate Cox model retained three clinical diagnostic factors: subthreshold (hypo)manic episode (Hazard Ratio 2.29; 95% Confidence Interval (CI) 1.10-4.78, p = 0.03); disruptive behavior disorders (Hazard Ratio 2.12; 95% CI 1.09-4.14, p=0.03); and major depressive episode (Hazard Ratio = 1.99; 95% CI 0.99-3.97, p=0.05). It also included one confounder covariate that met criteria for significant impact: proband age at intake assessment (Hazard Ratio 0.94; 95% CI 0.89-0.99, p=0.02).
We also examined the association of two comorbid conditions (e.g. subthreshold (hypo)mania and attention deficit hyperactivity disorder) with onset of manic/hypomania (eTable 5). No comorbid pair of diagnoses was more significantly associated with onset of mania/hypomania than one of the diagnoses alone.
Sensitivity Analyses: Diagnoses preceding prospectively observed mania/hypomania in offspring of parents with bipolar disorder
When the sample was restricted to the 344 high-risk offspring who had prospective follow-up and did not have a history of mania/hypomania at intake, 21 (6.1%) had a new onset of mania/hypomania over follow-up; 8 had a manic episode and 13 had hypomanic episodes only. Of these 21, 12 (57.1%) were diagnosed with a subthreshold (hypo)manic episode at an assessment prior to the assessment when mania /hypomania was first diagnosed, while 66.7% had a prior depressive episode, 52.4% had a prior major depressive episode, 42.9% had a prior diagnosis of attention-deficit hyperactivity disorder, 38.1% had a prior disruptive behavior disorders, 42.9% had a prior anxiety disorder and 9.5% had a prior substance use disorder. Multivariate models showed that only subthreshold (hypo)manic episodes were associated with prospectively observed onset of mania/hypomania (Hazard Ratio 7.57; 95% CI 3.09-18.6, p<.0001), with proband age at bipolar disorder onset retained as a confounder covariate (Hazard Ratio 0.95; 95% CI 0.89-1.02, p=0.1).
Discussion
This study demonstrates that bipolar-spectrum disorders, including bipolar-I, bipolar-II, and bipolar disorder not otherwise specified, are significantly more prevalent in high-risk offspring as compared to community controls, even when the offspring have not reached young adulthood. The high-risk offspring had much higher rates of depressive episodes compared to controls, but the rate of unipolar depressive disorders (depression without a history of manic, hypomanic, or subthreshold (hypo)manic episodes) was only marginally higher. Nearly all non-mood Axis I disorders were more prevalent in the high-risk offspring vs. community parents. Mania/hypomania in the high-risk offspring was almost always preceded by identifiable mood episodes and non-mood disorders. Distinct subthreshold episodes of (hypo)mania were highly specific to the high-risk offspring and were the strongest predictor of progression to full threshold mania/hypomania in the high-risk cohort. Identifiable depressive episodes preceded the onset of mania/hypomania in about 2/3 of the cases, but only major depressive episodes specifically predicted the onset of mania/hypomania above and beyond subthreshold (hypo)manic episodes and the presence of a disruptive behavior disorders. Sensitivity analyses using only prospective data, where the effects of recall bias were minimized, showed that only subthreshold (hypo)manic episodes were associated with prospectively observed mania/hypomania.
When examining the higher rates of non-mood Axis I disorders in the high-risk offspring, controlling for parental non-bipolar Axis I disorders did not substantially change the results. However, when the comparison group was limited to offspring of community control parents who had a lifetime Axis I disorder, attention deficit hyperactivity and disruptive behavior disorders no longer differed between groups. Given that the rates of attention-deficit hyperactivity and disruptive behavior disorders were significantly higher in the high-risk offspring as compared to all community control offspring when parental non-bipolar Axis I diagnoses were included in the model, these results need to be taken with caution.
Before considering the implications of these findings, it is important to consider the study's limitations. Though this is a prospective study, all diagnoses and estimates of age of onset are made retrospectively for the interval of time between assessments. Offspring were recruited across a broad age range (6-18 years, so that most offspring were not through the age of risk for onset of bipolar illness; only 29% were older than age 21 at their last assessment. Although this is the largest longitudinal study of offspring of parents with bipolar disorder, only 36 offspring were diagnosed with full threshold mania/hypomania. Only a small proportion of the biological co-parents had direct diagnostic interviews. Lastly, the bipolar parents were not systematically recruited from clinical or epidemiological populations so it is unclear whether these findings apply to the offspring of all bipolar parents.
The unexpected finding that substance use disorders were associated with a lower risk of developing mania/hypomania was likely caused by the conservative procedure used for diagnosing mania/hypomania in the presence of a substance use disorder. It may not be a valid result, particularly in light of the higher rate of lifetime substance use disorder in high-risk offspring who developed mania/hypomania compared to those who did not (44% vs. 17.5%).
The lifetime prevalence of any Axis I disorder was substantial in both the high-risk offspring (74.2%) and the community controls (48.4%). However, the prevalence of disorders in the controls is similar to that of other community studies of adolescents and young adults. It is nearly identical to that of the National Comorbidity Survey Adolescent Supplement study (49.5%), which was a large cross-sectional study of adolescents in the community.(22) The lifetime prevalence in the community controls also matches the cumulative rate of psychiatric disorders at age 21 (49.2%) in the Great Smoky Mountains Study which, like BIOS, had multiple assessments over time.(23) The lifetime prevalence rates in the high-risk offspring are very similar to the Dutch longitudinal high-risk study (72%) and that of Duffy et al. (76%).(15, 24)
The rate of bipolar-I (3.8%) in the BIOS high-risk sample was comparable to that found in other longitudinal offspring studies (range 3-7%), while the rate of either bipolar-I or II (8.4% vs. 10.1-18.8%) was slightly lower. (15-17, 25) This may be due the younger age at last assessment in BIOS, as the overall rates of bipolar-I/II in BIOS continue to climb after age 18. A recent meta-analysis of epidemiologic studies of adolescents found the rates of bipolar-I (1.2%) and bipolar spectrum disorders (1.8%)were similar to that in the BIOS offspring of community controls (bipolar-I 0.4%; bipolar-spectrum disorders 2.0%). (26)
The results from BIOS differ substantially from other longitudinal offspring studies in three ways. First, the mean age of onset of manic/hypomanic episodes was considerably younger in BIOS (13.4 vs. 17-19), with manic episodes occurring before age 12 in half of the BIOS bipolar-I offspring as compared to none reported in other studies. Second, a major depressive episode preceded the onset of mania/hypomania only about 50% of the time in BIOS, as compared to nearly all cases in other studies. Third, the BIOS offspring had significantly higher rates of psychopathology meeting criteria for one or more non-mood DSM-IV disorders prior to the onset of full threshold bipolar illness. Age at first assessment may be a contributing factor for the first issue; BIOS offspring were 11.9 years old on average as compared to 16.5 in the two largest longitudinal studies. The mean age of onset of first manic/hypomanic episode was significantly earlier in the offspring who were younger than age 12 at intake (n=16, 11.3 ± 3.3) than those who were 12-18 at intake (n=20, 15.0 ± 3.3) (t=-3.3; p=.002). The age of onset of first manic/hypomanic episode was about 12 in the National Comorbidity Survey Adolescent Supplement study, so BIOS is not unique in finding onset of mania and hypomania before adolescence.(27) However, there was no difference between the younger and older age groups at intake and rate of major depressive (50% vs. 60%), subthreshold (hypo)manic episodes (38% vs. 35%), or non-mood Axis I disorders (81% vs. 80%) preceding the onset of mania/hypomania in the BIOS offspring, so the reason for these findings are not clear.
The finding that subthreshold (hypo)manic episodes often precede manic/hypomanic episodes has been found in one other longitudinal offspring study. Duffy and colleagues noted in their cohort that 48% of offspring with bipolar disorder would have met criteria for bipolar disorder not otherwise specified prior to the onset of mania/hypomania.(16) BIOS demonstrates that this is not a result of recall bias, as prospectively observed manic/hypomanic episodes were preceded in 55% of the cases by subthreshold episodes identified at prior assessments. The prognostic significance of subthreshold (hypo)manic episodes has also been demonstrated in a pediatric clinical population. Youth diagnosed with bipolar disorder not otherwise specified at intake in the COBY study developed full threshold bipolar-I or bipolar-II at a rate of 45% over an average of 5 years of follow-up.(28) Those with a family history of bipolar disorder had a significantly higher rate of diagnostic progression compared to those who did not (56% vs. 33%). The prognostic significance of subthreshold (hypo)mania may not be limited to youth, as subthreshold symptoms of hypomania were predictive of future conversion to bipolar disorder in adults diagnosed with unipolar depression.(29)
Anxiety disorders were present at significantly higher rates in the high-risk offspring compared to controls in BIOS and have been associated with the presence of mood disorders in high-risk offspring in other studies (14, 30). However, they were not associated with future onset of mania/hypomania in BIOS, though it was close to statistical significance in the univariate analysis. The lack of association of anxiety disorder with risk of future bipolar disorder is consistent with what was found by Duffy and colleagues. (31) Anxiety was not associated in multivariate models, likely because of their high comorbidity with depression and subthreshold (hypo)mania.
In summary, these results indicate that in the offspring of parents with bipolar disorder, mania and hypomania does not come “out of the blue” but instead is almost always preceded by identifiable mood episodes and non-mood disorders. However, major depression is the index episode only half of the time and subthreshold episodes of (hypo)mania are the only specific diagnostic antecedent to mania and hypomania when using prospectively obtained data. Clinicians should carefully assess for subthreshold (hypo)manic episodes and differentiate them from symptoms of depression and other disorders in the offspring of parents with bipolar disorder, as they carry prognostic significance for the future development of full threshold bipolar illness. It also may provide an opportunity for early intervention to improve the course of illness. For instance, a recent study demonstrated benefits from a family-focused approach for symptomatic youth who had a first degree relative with bipolar disorder.(32) Given the clear prognostic significance of subthreshold (hypo)mania in youth at familial risk for bipolar disorder, we need additional treatment research for these youth. As both major depressive episodes and disruptive behavior disorders also indicate risk of future bipolarity, they are indications for close clinical monitoring in high-risk offspring. Given the high prevalence of both mood and non-mood disorders in the high-risk offspring and the difficulty differentiating subthreshold (hypo)mania from other disorders, it would be worthwhile for clinicians who treat bipolar adults to encourage them to have their children evaluated by specialty pediatric mental health services if the parent is concerned about their child's mood or behavior.
Supplementary Material
eTable 1 Comparison of Intake Factors for Offspring with and without Follow-Up Assessments†
eTable2: Parent Proband Factors
eTable 3: Biological Co-Parent Factors
eTable 4: Association of potential confounding variables with hazard to develop subsequent manic/hypomanic episodes in high-risk offspring†
eTable 5: Association comparing single vs. comorbid prior mood episodes and/or diagnoses in hazard to develop subsequent manic/hypomanic episodes in offspring of parents with bipolar disorder†
References
- 1.Perlis RH, Dennehy EB, Miklowitz DJ, Delbello MP, Ostacher M, Calabrese JR, et al. Retrospective age at onset of bipolar disorder and outcome during two-year follow-up: results from the STEP-BD study. Bipolar Disorders. 2009;11(4):391–400. doi: 10.1111/j.1399-5618.2009.00686.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lish JD, Dime-Meehan S, Whybrow PC, Price RA, Hirschfeld RM. The National Depressive and Manic-Depressive Association (DMDA) Survey of Bipolar Members. Journal of Affective Disorders. 1994;31(4):281–94. doi: 10.1016/0165-0327(94)90104-x. [DOI] [PubMed] [Google Scholar]
- 3.Chengappa KN, Kupfer DJ, Frank E, Houck PR, Grochocinski VJ, Cluss PA, et al. Relationship of birth cohort and early age at onset of illness in a bipolar disorder case registry. American Journal of Psychiatry. 2003;160(9):1636–42. doi: 10.1176/appi.ajp.160.9.1636. [DOI] [PubMed] [Google Scholar]
- 4.Leverich G, Post RM, Keck PE, Altshuler L, Frye MA, Kupka R. The poor prognosis of childhood-onset bipolar disorder. Journal of Pediatrics. 2007;150:485–90. doi: 10.1016/j.jpeds.2006.10.070. [DOI] [PubMed] [Google Scholar]
- 5.Goodwin FK, Jamison KR. Manic-depressive illness: Bipolar Disorders and Recurrent Depression. 2nd. New York: Oxford University Press; 2007. [Google Scholar]
- 6.Barnett JH, Smoller JW. The Genetics of Bipolar Disorder. Neuroscience. 2009;164:331–43. doi: 10.1016/j.neuroscience.2009.03.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.DelBello MP, Geller B. Review of studies of child and adolescent offspring of bipolar parents. Bipolar Disorders. 2001;3(6):325–34. doi: 10.1034/j.1399-5618.2001.30607.x. [DOI] [PubMed] [Google Scholar]
- 8.Lapalme M, Hodgins S, LaRoche C. Children of parents with bipolar disorder: a metaanalysis of risk for mental disorders. Canadian Journal of Psychiatry - Revue Canadienne de Psychiatrie. 1997;42(6):623–31. doi: 10.1177/070674379704200609. [DOI] [PubMed] [Google Scholar]
- 9.Henin A, Biederman J, Mick E, Sachs GS, Hirshfeld-Becker DR, Siegel RS, et al. Psychopathology in the offspring of parents with bipolar disorder: a controlled study. Biological Psychiatry. 2005;58(7):554–61. doi: 10.1016/j.biopsych.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 10.Chang KD, Steiner H, Ketter TA. Psychiatric phenomenology of child and adolescent bipolar offspring. Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39(4):453–60. doi: 10.1097/00004583-200004000-00014. [DOI] [PubMed] [Google Scholar]
- 11.Birmaher B, Axelson D, Goldstein B, Monk K, Kalas C, Obreja M, et al. Psychiatric disorders in preschool offspring of parents with bipolar disorder: the Pittsburgh Bipolar Offspring Study (BIOS) American Journal of Psychiatry. 2010;167(3):321–30. doi: 10.1176/appi.ajp.2009.09070977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Birmaher B, Axelson D, Monk K, Kalas C, Goldstein B, Hickey MB, et al. Lifetime psychiatric disorders in school-aged offspring of parents with bipolar disorder: the Pittsburgh Bipolar Offspring study. Archives of General Psychiatry. 2009;66(3):287–96. doi: 10.1001/archgenpsychiatry.2008.546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vandeleur C, Rothen S, Gholam-Rezaee M, Castelao E, Vidal S, Favre S, et al. Mental disorders in offspring of parents with bipolar and major depressive disorders. Bipolar Disorders. 2012;14(6):641–53. doi: 10.1111/j.1399-5618.2012.01048.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nurnberger JI, Jr, McInnis M, Reich W, Kastelic E, Wilcox HC, Glowinski A, et al. A high-risk study of bipolar disorder. Childhood clinical phenotypes as precursors of major mood disorders. Archives of General Psychiatry. 2011;68(10):1012–20. doi: 10.1001/archgenpsychiatry.2011.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mesman E, Nolen WA, Reichart CG, Wals M, Hillegers MH. The dutch bipolar offspring study: 12-year follow-up. American Journal of Psychiatry. 2013;170(5):542–9. doi: 10.1176/appi.ajp.2012.12030401. [DOI] [PubMed] [Google Scholar]
- 16.Duffy A, Alda M, Hajek T, Sherry SB, Grof P. Early stages in the development of bipolar disorder. Journal of Affective Disorders. 2010;121(1-2):127–35. doi: 10.1016/j.jad.2009.05.022. [DOI] [PubMed] [Google Scholar]
- 17.Egeland JA, Endicott J, Hostetter AM, Allen CR, Pauls DL, Shaw JA. A 16-year prospective study of prodromal features prior to BPI onset in well Amish children. Journal of Affective Disorders. 2012;142(1-3):186–92. doi: 10.1016/j.jad.2012.04.023. [DOI] [PubMed] [Google Scholar]
- 18.Birmaher B, Axelson D, Strober M, Gill MK, Valeri S, Chiappetta L, et al. Clinical course of children and adolescents with bipolar spectrum disorders. Archives of General Psychiatry. 2006;63(2):175–83. doi: 10.1001/archpsyc.63.2.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goldstein BI, Shamseddeen W, Axelson DA, Kalas C, Monk K, Brent DA, et al. Clinical, demographic, and familial correlates of bipolar spectrum disorders among offspring of parents with bipolar disorder. Journal of the American Academy of Child & Adolescent Psychiatry. 2010;49(4):388–96. [PMC free article] [PubMed] [Google Scholar]
- 20.Andreasen NC, Endicott J, Spitzer RL, Winokur G. The family history method using diagnostic criteria. Reliability and validity. Archives of General Psychiatry. 1977;34(10):1229–35. doi: 10.1001/archpsyc.1977.01770220111013. [DOI] [PubMed] [Google Scholar]
- 21.Hollingshead AB. Four-Factor Index of Social Status. New Haven, Connecticut: Yale University Department of Sociology; 1975. [Google Scholar]
- 22.Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui L, et al. Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication--Adolescent Supplement (NCS-A) Journal of the American Academy of Child & Adolescent Psychiatry. 2010;49(10):980–9. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Copeland W, Shanahan L, Costello EJ, Angold A. Cumulative prevalence of psychiatric disorders by young adulthood: a prospective cohort analysis from the Great Smoky Mountains Study. Journal Of The American Academy Of Child And Adolescent Psychiatry. 2011;50(3):252–61. doi: 10.1016/j.jaac.2010.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Duffy A, Alda M, Crawford L, Milin R, Grof P. The early manifestations of bipolar disorder: a longitudinal prospective study of the offspring of bipoalr parents. Bipolar Disorders. 2007;9:828–38. doi: 10.1111/j.1399-5618.2007.00421.x. [DOI] [PubMed] [Google Scholar]
- 25.Meyer SE, Carlson GA, Wiggs EA, Martinez PE, Ronsaville DS, Klimes-Dougan B, et al. A prospective study of the association among impaired executive functioning, childhood attentional problems, and the development of bipolar disorder. Development & Psychopathology. 2004;16(2):461–76. doi: 10.1017/s095457940404461x. [DOI] [PubMed] [Google Scholar]
- 26.Van Meter AR, Moreira ALR, Youngstrom EA. Meta-Analysis of Epidemiological Studies of Pediatric Bipolar Disorder. Journal of Clinical Psychiatry. 2011;72(9):1250–6. doi: 10.4088/JCP.10m06290. [DOI] [PubMed] [Google Scholar]
- 27.Merikangas KR, Cui L, Kattan G, Carlson GA, Youngstrom EA, Angst J. Mania with and without depression in a community sample of US adolescents. Archives of General Psychiatry. 2012;69(9):943–51. doi: 10.1001/archgenpsychiatry.2012.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Axelson DA, Birmaher B, Strober MA, Goldstein BI, Ha W, Gill MK, et al. Course of subthreshold bipolar disorder in youth: diagnostic progression from bipolar disorder not otherwise specified. Journal of the American Academy of Child & Adolescent Psychiatry. 2011;50(10):1001–16. e3. doi: 10.1016/j.jaac.2011.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fiedorowicz JG, Endicott J, Leon AC, Solomon DA, Keller MB, Coryell WH. Subthreshold hypomanic symptoms in progression from unipolar major depression to bipolar disorder. American Journal of Psychiatry. 2011;168(1):40–8. doi: 10.1176/appi.ajp.2010.10030328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Duffy A, Horrocks J, Doucette S, Keown-Stoneman C, McCloskey S, Grof P. The developmental trajectory of bipolar disorder. The British Journal Of Psychiatry: The Journal Of Mental Science. 2014;204(2):122–8. doi: 10.1192/bjp.bp.113.126706. [DOI] [PubMed] [Google Scholar]
- 31.Duffy A, Horrocks J, Doucette S, Keown-Stoneman C, McCloskey S, Grof P. Childhood anxiety: an early predictor of mood disorders in offspring of bipolar parents. Journal Of Affective Disorders. 2013;150(2):363–9. doi: 10.1016/j.jad.2013.04.021. [DOI] [PubMed] [Google Scholar]
- 32.Miklowitz DJ, Schneck CD, Singh MK, Taylor DO, George EL, Cosgrove VE, et al. Early intervention for symptomatic youth at risk for bipolar disorder: a randomized trial of family-focused therapy. Journal of the American Academy of Child and Adolescent Psychiatry. 2013;52(2):121–31. doi: 10.1016/j.jaac.2012.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1 Comparison of Intake Factors for Offspring with and without Follow-Up Assessments†
eTable2: Parent Proband Factors
eTable 3: Biological Co-Parent Factors
eTable 4: Association of potential confounding variables with hazard to develop subsequent manic/hypomanic episodes in high-risk offspring†
eTable 5: Association comparing single vs. comorbid prior mood episodes and/or diagnoses in hazard to develop subsequent manic/hypomanic episodes in offspring of parents with bipolar disorder†


