Abstract
The many improvements in breast cancer therapy in recent years have so lowered rates of recurrence that it is now difficult or impossible to conduct adequately powered adjuvant clinical trials. Given the many new drugs and potential synergistic combinations, the neoadjuvant approach has been used to test benefit of drug combinations in clinical trials of primary breast cancer. A recent FDA-led meta-analysis showed that pathologic complete response (pCR) predicts disease-free survival (DFS) within patients who have specific breast cancer subtypes. This meta-analysis motivated the FDA's draft guidance for using pCR as a surrogate endpoint in accelerated drug approval. Using pCR as a registration endpoint was challenged at ASCO 2014 Annual Meeting with the presentation of ALTTO, an adjuvant trial in HER2-positive breast cancer that showed a nonsignificant reduction in DFS hazard rate for adding lapatinib, a HER-family tyrosine kinase inhibitor, to trastuzumab and chemotherapy. This conclusion seemed to be inconsistent with the results of NeoALTTO, a neoadjuvant trial that found a statistical improvement in pCR rate for the identical lapatinib-containing regimen. We address differences in the two trials that may account for discordant conclusions. However, we use the FDA meta-analysis to show that there is no discordance at all between the observed pCR difference in NeoALTTO and the observed HR in ALTTO. This underscores the importance of appropriately modeling the two endpoints when designing clinical trials. The I-SPY 2/3 neoadjuvant trials exemplify this approach.
Introduction
Over the last 2 decades, there has been an explosion in the development of new drugs for cancer based on mechanistic preclinical research. However, relatively few have successfully improved clinical outcomes and ultimately reached the market. The traditional process of determining which drugs will ultimately benefit patients is long and expensive, with recent reports estimating a cost of over 2 billion dollars and time horizon of 10 to 15 years to get a promising drug to market (1). The greatest opportunity for curing cancer occurs when it is has not metastasized (2, 3). Despite the obvious advantage of focusing phase II and III trials in early disease, clinical drug development has traditionally begun in the metastatic setting. Metastatic benefit does not always predict adjuvant benefit and so there are false positives. Similarly, lack of benefit in metastatic disease may miss a benefit in primary disease and so there are almost certainly false negatives that we do not know about because they failed to pass the metastatic hurdle. The neoadjuvant platform provides what is likely to be a more informative mechanism of adjuvant benefit.
A prototype demonstrating the greater impact of effective drugs when given early is imatinib (Gleevec) in CML (4). The introduction of imatinib led to a dramatic improvement in survival rates when patients were treated in the accelerated phase but not for those treated in blast crisis. Adjuvant therapies offer increased cure rates in numerous disease settings, with effective agents targeting micrometastatic, minimal residual disease.
Despite the obvious potential advantages of early treatment, the adjuvant approach is ill suited for evaluating its benefits. Very little information accrues about the treatment's effect until and if the patient's tumor recurs. The number of events, and not the number of patients, determines the power of a clinical trial. On the other hand, the neoadjuvant approach provides a very clear indication of the treatment's effect by making the posttreatment tumor available at surgery. The eradication of all invasive disease in the breast and lymph nodes, a pathologic complete response (pCR), has been shown in many randomized trials of chemotherapy and targeted therapies to confer a recurrence-free survival benefit (5–8). The FDA meta-analysis quantifies the benefit that experiencing a pCR confers by receptor subtype in women with high-risk primary breast cancer (9). Importantly, the predictive benefit of pCR is even greater when evaluated within subtypes than when all subtypes are combined (7).
The ability of the neoadjuvant setting to predict survival benefits to adjuvant therapy has already been demonstrated within the context of Her2+ breast cancer. In the NOAH trial, trastuzumab, when added to standard anthracycline-based neoadjuvant therapy, significantly improved pCR rates and subsequently improved EFS [HR, 0.59; 95% confidence intervals (CI), 0.38–0.90; P = 0.013; ref. 10]. This subsequently translated to a benefit of trastuzumab in the adjuvant setting that was demonstrated in the combined NSABP B-31/NCCTG 9831 trial analysis, with an absolute improvement in disease-free survival (DFS) of 12% (HR, 0.48; P < 0.0001; ref. 3), establishing a new standard of care for Her2+ nonmetastatic breast cancer.
ALLTO and NeoALTTO Trials in Context
It is within this context that the findings of the ALTTO trial were presented at the American Society of Clinical Oncology 2014 Annual Meeting in Chicago (11). ALTTO showed that the addition of lapatinib to trastuzumab and standard adjuvant chemotherapy was associated with a nonsignificant reduction in DFS in HER2-positive tumors. The HR was 0.84 (97.5% CI, 0.70–1.02) on the basis of about 2,100 patients in each of the two groups. The two-sided P value of 0.048 was not significant because the investigators had added another comparison, the noninferiority of trastuzumab followed by lapatinib versus trastuzumab, both for a total of one year. These results were contrasted with NeoALTTO, a neoadjuvant trial on HER2-positive tumors at higher risk than those in ALTTO. NeoALTTO was reported in 2012 and showed a statistically significant improvement in the rate of pCR (12).
The lack of a statistically significant improvement in DFS in ALTTO despite the significant improvement in pCR in NeoALTTO raised concerns about the validity of using pCR determined in the neoadjuvant setting to predict DFS outcomes when the same therapies are used in the more typical postsurgery adjuvant setting. This presents an important opportunity to analyze the reported results and to determine whether indeed we should back away from pursuing pCR as an efficient and effective way of predicting a therapy's long-term benefits.
There were several differences between the two trials, apart from the timing of surgery. First, to state the obvious, they were different trials. Even if two trials have exactly the same design and are conducted in exactly the same populations, their results can be markedly different. Second, the populations had different risks, with 4-year DFS in NeoALTTO about 75% versus 87% in ALTTO. Risk by itself is not usually a predictor of therapeutic benefit, but it might reflect differences in underlying disease that respond differently to therapy. ALTTO had a greater proportion of node-negative patients, although nodal status is not predictive of the benefits of anti-HER2 therapy. However, ALTTO also had a greater proportion of hormone-receptor positive tumors, and these are less sensitive to anti-HER2 therapy. Third, the order of chemotherapy was different in the two trials, although this probably had little effect. Finally, pCR was assessed in NeoALTTO before the anthracycline-based chemotherapy component of the regimen. Anthracyclines are well known to be effective in HER2-positive disease and this might have served to exaggerate the effects of lapatinib, although the opposite could also have been true.
The ALTTO investigators recognized that the trial was under-powered and they quite appropriately wanted to present whatever information was available to patients as soon as reasonable, despite the lower power. The planned number of DFS events in the two arms in question was 850. The design was modified when the overall event rate was lower than expected, with an announcement of results planned at median follow-up of 4.5 years even if there were fewer than 850 events at that time. The analysis announced at ASCO 2014 had only 555 events. With an additional 295 events, the observed HR of 0.84 or even slightly higher would have been statistically significant; although the additional events would likely have changed the HR, the direction is not clear.
Discussion
The current debate about the relevance of neoadjuvant endpoints in drug development is based on the conclusion, or rather, the assumption, that the results of ALTTO were not consistent with the results of NeoALTTO. Some of the arguments stem from how statistical significance, or lack thereof, is interpreted. Statistical significance does not imply truth and lack of statistical significance does not imply falsity. In this case, reliance on a yes/no interpretation of statistical significance leads to the wrong conclusion. NeoALTTO was considered “statistically significantly positive” for pCR, whereas ALTTO was reported to be “statistically significantly negative” for DFS. The ALTTO and NeoALTTO results show how using these terms, rather than considering the actual results, can lead to erroneous conclusions. In actuality, despite differences in the two trials that might be expected to lead to discordant results, the results of ALTTO are essentially perfectly predicted by NeoALTTO and the FDA meta-analysis (9).
This meta-analysis showed that the EFS HR for HER2-positive breast cancer patients achieving a pCR versus not pCR was 0.39 (95% CI, 0.31–0.50). (The FDA's use of EFS was similar to ALTTO's use of DFS except that ALTTO considered second primary cancers to be events. We will use DFS and EFS interchangeably.) An obvious and quite reasonable concern is that the HR in the meta-analysis may not apply for a particular experimental therapy. For example, adding lapatinib to trastuzumab might change some non-responders to having pCRs but might not prolong those patients' EFS.
What HR would the FDA's meta-analysis have predicted for ALTTO based on the pCR improvement in NeoALTTO? The primary endpoint in NeoALTTO was pCR in the breast, with the combination improving the rate by 22%; the improvement in pCR was 20% (49% for the combination vs. 29%) when pCR included both the breast and axilla. The “pCR” and “No pCR” curves, shown in Fig. 1, are smoothed versions of the EFS curves in the FDA's meta-analysis of patients with HER2-positive tumors (18). The HR of 0.39, as indicated in the figure, is a 61% reduction in the hazard of recurrence. A 20% improvement in pCR would mean moving 1 in 5 patients from the “No pCR” curve to the “pCR” curve. Such a shift would obviously give rise to a reduction in EFS hazard for the combination that is smaller than 61%, although it would not be as small as one-fifth of this quantity. The resulting HR for the treatment comparison as shown in the figure is 0.83, almost exactly the observed value is 0.84 in ALTTO.
Figure 1.
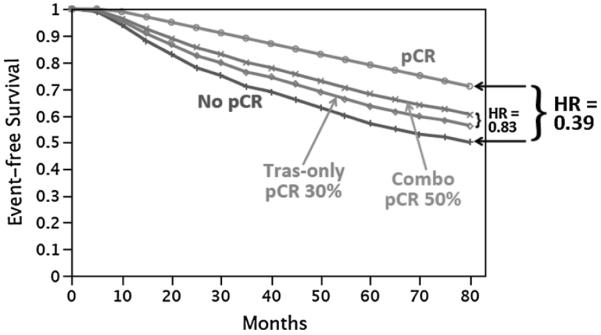
Expected EFS curves for trastuzumab as well as for the combination of trastuzumab and lapatanib are shown based on the NeoALTTO results.
Taking this argument a step further, there are a total of five randomized trials that evaluated trastuzumab ± lapatinib in the neoadjuvant setting (including NeoALTTO), with a total of over 1,200 patients (Table 1). They are quite relevant in predicting ALTTO results. The combined overall pCR advantage of the combination of lapatinib, trastuzumab, and chemotherapy over trastuzumab/chemotherapy alone in these five trials was 13%. On the basis of the FDA meta-analysis, the EFS HR corresponding to a 13% pCR advantage in HER2-positive disease is 0.88. So using all the relevant neoadjuvant data, the results of ALTTO, with its HR of 0.84, are actually somewhat more positive than the FDA's meta-analysis would predict. The difference between the expected 0.88 and the observed 0.84 is easily explained by random variability, but any surprise at the results of ALTTO should be because they were more, not less, positive than expected. In any case, the results of ALTTO support the relationship between pCR and EFS in the FDA's meta-analysis whether using NeoALTTO alone or all five trials in Table 1.
Table 1.
Neoadjuvant trials of lapatinib
Moving forward, trials should be prospectively designed to test the neoadjuvant model. This strategy is being used in the development of neratinib. In contrast with lapatinib, this irreversible small-molecule inhibitor of the HER/ErbB family of receptor-tyrosine kinases provides a different mechanism of action and potentially greater potency than first-generation HER kinase inhibitors such as lapatinib. In preclinical studies, neratinib demonstrated in vitro activity against cancer cell lines of different phenotypes, including HER2-overexpressing as well as non-HER2-overexpressing cells. The potential efficacy of neratinib in the (neo)adjuvant setting was demonstrated in I-SPY 2, in which neratinib was evaluated in patients receiving standard neoadjuvant chemotherapy (paclitaxel qwk × 12, doxorubicin and cyclophosphamide q2–3 wk × 4, T→AC; ref. 13). Patients with HER2-negative tumors were randomized to neratinib plus T→AC chemotherapy (i.e., N+T→AC vs. T→AC). Patients with HER2-positive tumors were randomized to the same experimental regimen (N+T→AC) versus trastuzumab+T→AC, allowing a direct comparison of neratinib with trastuzumab. Neratinib met the predictive probability criterion in the predefined HR−/HER2+signature (where HR stands for hormone receptor), “graduated,” and accrual ceased (115 N patients and 78 concurrently randomized controls). In the HR−/HER2+ signature, the probability of neratinib having a larger pCR rate than control was 95%. On the basis of these results, phase III testing of neratinib in I-SPY 3 is planned. I-SPY 3 has been designed specifically to test the hypothesis that drugs found in a phase II setting such as I-SPY 2 will show success demonstrating a DFS improvement in a phase II trial in specific patient subsets previously identified in I-SPY2. In I-SPY 3, both pCR and EFS are primary endpoints. The sample size is reestimated adaptively in I-SPY 3 based on the pCR results in the experimental and control arms, and on predictions of EFS effect with longer follow-up. The trial uses the modeling from the FDA meta-analysis, but because it is not clear that the meta-analysis applies in the setting of I-SPY 3 and with the treatment regimens in I-SPY 3, that model is updated based on the accumulating information about the relationship between pCR and EFS within those regimens.
The ALTTO results have caused some in the field to call for the abandoning of the neoadjuvant model for drug development in favor of a return to large conventional adjuvant clinical trials. However, as shown above, the statistical ALTTO/NeoALTTO relationship confirms the value of the neoadjuvant setting to identify active new agents that improve outcomes in early breast cancer. The results of ALTTO do not diminish the enthusiasm for testing promising new agents, but rather, provide further impetus to reduce the large size of adjuvant trials by focusing on agents with a higher impact and on patients with higher risk and having a particular biomarker signature.
The neoadjuvant approach presents the opportunity to speed drug development while simultaneously providing real-time benefits to patients who participate in such trials. Women who present with breast cancers that have a 30% or greater risk of developing metastatic disease in the first 5 years after diagnosis are usually advised to receive adjuvant chemotherapy. There is no reason, in the setting where that recommendation is clear, not to offer those patients systemic treatment before surgical resection. Surgical options are improved after neoadjuvant therapy for the vast majority of patients (16). Response to therapy provides prognostic and predictive information and informs decisions about adjuvant radiation treatments. For example, for some women with excellent response to systemic therapy, radiation can even be avoided after mastectomy (17). The neoadjuvant approach, particularly in the context of carefully designed trials, maximizes information garnered and maximizes our ability to correlate early response with EFS outcomes.
However, the ascertainment of residual disease should be rigorous and standardized. The emerging rigorous standards for measuring pCR had not been developed at the start of the NeoALTTO trial. The primary endpoint of NeoALTTO was response in the breast only (not breast and axillary lymph nodes). The latter is the currently accepted standard and it is the basis of the FDA's draft guidance for accelerated drug approval (13). Indeed, it is now critically important to standardize the procedures for pathologic assessment of residual disease across international clinical trial groups, specialty societies, and regulatory bodies, and this should increase the chance of accurate and reproducible results within and across trials.
In summary, pCR is a good predictor of EFS within breast cancer subtypes and should continue to be used as an opportunity to accelerate evaluation of promising agents. The results from ALTTO should not slow this acceleration. Instead, neoadjuvant endpoints should be systematically and carefully incorporated into EFS endpoint trials in the future. These carefully designed studies will continue to improve the neoadjuvant approach and will continue to accelerate drug development. We should take bold steps to compress the timeline to get effective new drugs to market. We owe it to our patients to push the envelope. There is little risk in incorporating neoadjuvant therapy into breast cancer trials. The greater risk lies in avoiding the neoadjuvant approach and being content with huge adjuvant trials and 10 to 15 year time horizons to get new drugs to market.
Translational Relevance.
The recent results of the ALTTO trial are consistent with the predicted benefits from the neoALTTO trial, despite significant differences in the patient populations of the two trials. These results support the neoadjuvant setting as a suitable and important setting for evaluating promising, new targeted agents but highlight the essential requirement for rigorous study design and statistical planning in confirmatory neoadjuvant and adjuvant studies. Future efforts to confirm improvements in pathologic complete response (pCR) should focus on testing neoadjuvant therapies in trials in which event-free survival (EFS) is an important endpoint and in which the relationship between pCR and EFS is an important analysis. This will definitively test the hypothesis that the neoadjuvant strategy can significantly reduce the time, cost, and number of patients to get new drugs approved and demonstrate that early (pCR) and late (EFS) benefits of targeted therapy are highly associated in specific biomarker-defined patient populations.
Acknowledgments
Figure 1 originally appeared in The Cancer Letter (18). The authors thank The Cancer Letter for allowing them to reprint Fig. 1.
Footnotes
Disclosure of Potential Conflicts of Interest D.A. Berry is a founder of and has ownership interest (including patents) in Berry Consultant, LLC. A.D. Elias is a consultant/advisory board member for EMD Serono. C. Isaacs reports receiving speakers bureau honoraria from Genentech. J.W. Park reports receiving speakers bureau honoraria from and has provided expert testimony for Genentech; and has ownership interest in (including patents) and is a consultant/advisory board member for Merrimack Pharma. B.A. Parker reports receiving commercial research grants from GlaxoSmithKline. F. Symmans has ownership interest (including patents) in Nuvera Biosciences, Inc. No potential conflicts of interest were disclosed by the other authors.
Authors' Contributions Conception and design: A. DeMichele, D. Yee, D.A. Berry, K.S. Albain, M. Buxton, T.C. Haddad, C. Isaacs, M. Paoloni, J.W. Park, J. Perlmutter, H. Rugo, D. Tripathy, L.J. van't Veer
Development of methodology: A. DeMichele, D.A. Berry, M. Paoloni, D. Tripathy, L.J. van't Veer, D. Wolf, L.J. Esserman
Acquisition of data (provided animals, acquired and managed patients, provided facilities, etc.): A. DeMichele, J. Boughey, M. Buxton, A.J. Chien, S.Y. Chui, K. Edmiston, B. Haley, P. Haluska, N.M. Hylton, C. Isaacs, H. Kaplan, L. Korde, M.C. Liu, M. Melisko, S.L. Moulder, H. Rugo, D. Tripathy, R.K. Viscusi, A. Wallace
Analysis and interpretation of data (e.g., statistical analysis, biostatistics, computational analysis): A. DeMichele, D.A. Berry, M. Buxton, S.K. Chia, B. Leyland-Jones, M.C. Liu, S.L. Moulder, O.I. Olopade, M. Paoloni, H. Rugo, D. Tripathy, D. Wolf
Writing, review, and/or revision of the manuscript: A. DeMichele, D. Yee, D.A. Berry, K.S. Albain, C.C. Benz, J. Boughey, M. Buxton, S.K. Chia, S.Y. Chui, A. Clark, K. Edmiston, A.D. Elias, A. Forero-Torres, T.C. Haddad, P. Haluska, N.M. Hylton, C. Isaacs, H. Kaplan, L. Korde, B. Leyland-Jones, M.C. Liu, M. Melisko, S.E. Minton, S.L. Moulder, R. Nanda, O.I. Olopade, M. Paoloni, J.W. Park, B.A. Parker, J. Perlmutter, E.F. Petricoin, H. Rugo, F. Symmans, D. Tripathy, L.J. van't Veer, A. Wallace, C. Yau, L.J. Esserman
Administrative, technical, or material support (i.e., reporting or organizing data, constructing databases): A. DeMichele, D.A. Berry, M. Buxton, S.Y. Chui, H. Kaplan, O.I. Olopade, H. Rugo
Study supervision: A. DeMichele, D.A. Berry, M. Buxton, A.J. Chien, S.Y. Chui, H. Kaplan, M.C. Liu, M. Paoloni, A. Wallace
Other (committee participant in discussions leading to the writing and review of this manuscript): C.C. Benz
Other (UAB I SPY 2 Principal Investigator): A. Forero-Torres
References
- 1.LoRusso PM, Anderson AB, Boerner SA, Averbuch SD. Making the investigational oncology pipeline more efficient and effective: are we headed in the right direction? Clin Cancer Res. 2010;16:5956–62. doi: 10.1158/1078-0432.CCR-10-1279. [DOI] [PubMed] [Google Scholar]
- 2.Citron ML, Berry DA, Cirrincione C, Hudis C, Winer EP, Gradishar WJ, et al. Randomized trial of dose-dense versus conventionally scheduled and sequential versus concurrent combination chemotherapy as postoperative adjuvant treatment of node-positive primary breast cancer: first report of Intergroup Trial C9741/Cancer and Leukemia Group B Trial 9741. J Clin Oncol. 2003;21:1431–9. doi: 10.1200/JCO.2003.09.081. [DOI] [PubMed] [Google Scholar]
- 3.Romond EH, Perez EA, Bryant J, Suman VJ, Geyer CE, Davidson NE, et al. Trastuzumab plus adjuvant chemotherapy for operable HER2-positive breast cancer. N Engl J Med. 2005;353:1673–84. doi: 10.1056/NEJMoa052122. [DOI] [PubMed] [Google Scholar]
- 4.Kantarjian HM, Shah NP, Cortes JE, Baccarani M, Agarwal MB, Undurraga MS, et al. Dasatinib or imatinib in newly diagnosed chronic-phase chronic myeloid leukemia: 2-year follow-up from a randomized phase 3 trial (DASISION) Blood. 2012;119:1123–9. doi: 10.1182/blood-2011-08-376087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bear HD, Anderson S, Brown A, Smith R, Mamounas EP, Fisher B, et al. The effect on tumor response of adding sequential preoperative docetaxel to preoperative doxorubicin and cyclophosphamide: preliminary results from national surgical adjuvant breast and bowel project protocol B-27. J Clin Oncol. 2003;21:4165–74. doi: 10.1200/JCO.2003.12.005. [DOI] [PubMed] [Google Scholar]
- 6.von Minckwitz G. Neoadjuvant chemotherapy in breast cancer-insights from the German experience. Breast Cancer. 2012;19:282–8. doi: 10.1007/s12282-012-0393-7. [DOI] [PubMed] [Google Scholar]
- 7.Esserman LJ, Berry DA, DeMichele A, Carey L, Davis SE, Buxton M, et al. Pathologic complete response predicts recurrence-free survival more effectively by cancer subset: results from the I-SPY 1 TRIAL–CALGB 150007/150012, ACRIN 6657. J Clin Oncol. 2012;30:3242–9. doi: 10.1200/JCO.2011.39.2779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Carey LA, Dees EC, Sawyer L, Gatti L, Moore DT, Collichio F, et al. The triple negative paradox: primary tumor chemosensitivity of breast cancer subtypes. Clin Cancer Res. 2007;13:2329–34. doi: 10.1158/1078-0432.CCR-06-1109. [DOI] [PubMed] [Google Scholar]
- 9.Cortazar P, Zhang L, Untch M, Mehta K, Costantino JP, Wolmark N, et al. Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet. 2014;384:164–72. doi: 10.1016/S0140-6736(13)62422-8. [DOI] [PubMed] [Google Scholar]
- 10.Gianni L, Eiermann W, Semiglazov V, Manikhas A, Lluch A, Tjulandin S, et al. Neoadjuvant chemotherapy with trastuzumab followed by adjuvant trastuzumab versus neoadjuvant chemotherapy alone, in patients with HER2-positive locally advanced breast cancer (the NOAH trial): a randomised controlled superiority trial with a parallel HER2-negative cohort. Lancet. 2010;375:377–84. doi: 10.1016/S0140-6736(09)61964-4. [DOI] [PubMed] [Google Scholar]
- 11.Piccart-Gebhart MJ, Holmes AP, Baselga J, Azambuja ED, Dueck AC, Viale G, et al. First results from the phase III ALTTO trial (BIG 2–06; NCCTG [Alliance] N063D) comparing one year of anti-HER2 therapy with lapatinib alone (L), trastuzumab alone (T), their sequence (T→L), or their combination (T+L) in the adjuvant treatment of HER2-positive early breast cancer (EBC) [abstract] J Clin Oncol. 2014;32:LBA4. [Google Scholar]
- 12.Baselga J, Bradbury I, Eidtmann H, Di Cosimo S, de Azambuja E, Aura C, et al. Lapatinib with trastuzumab for HER2-positive early breast cancer (NeoALTTO): a randomised, open-label, multicentre, phase 3 trial. Lancet. 2012;379:633–40. doi: 10.1016/S0140-6736(11)61847-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Berry DA. NeoALTTO & ALTTO Trials, Neoadjuvant Response Predicts Adjuvant. The Cancer Letter [Internet] 2014 Jul; [cited 2014 July 11]; 40- 28:[about 3 p.]. Available from: http://www.cancerletter.com/articles/20140711_2.
- 14.Neratinib Graduates to I-SPY 3. Cancer Discovery. 2014;4:624. doi: 10.1158/2159-8290.CD-NB2014-055. [DOI] [PubMed] [Google Scholar]
- 15.Mukhtar RA, Yau C, Rosen M. Tandon VJI-SPY 1 TRIAL and ACRIN 6657 Investigators Hylton N, et al. Clinically meaningful tumor reduction rates vary by prechemotherapy MRI phenotype and tumor subtype in the I-SPY 1 TRIAL (CALGB 150007/150012; ACRIN 6657) Ann Surg Oncol. 2013;20:3823–30. doi: 10.1245/s10434-013-3038-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mamounas EP, Anderson SJ, Dignam JJ, Bear HD, Julian TB, Geyer CE, Jr, et al. Predictors of locoregional recurrence after neoadjuvant chemotherapy: results from combined analysis of National Surgical Adjuvant Breast and Bowel Project B-18 and B-27. J Clin Oncol. 2012;30:3960–6. doi: 10.1200/JCO.2011.40.8369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Prowell TM, Pazdur R. Pathological Complete Response and Accelerated Drug Approval in Early Breast Cancer. N Engl J Med. 2012;366:2438–41. doi: 10.1056/NEJMp1205737. [DOI] [PubMed] [Google Scholar]
- 18.Carey LA, Berry DA, Ollila D, Harris L, Krop IE, Weckstein D, et al. Clinical and translational results of CALGB 40601: a neoadjuvant phase III trial of weekly paclitaxel and trastuzumab with or without lapatinib for HER2-positive breast cancer [abstract] J Clin Oncol. 2013;31:500. [Google Scholar]
- 19.Guarneri V, Frassoldati A, Bottini A, Cagossi K, Bisagni G, Sarti S, et al. Preoperative chemotherapy plus trastuzumab, lapatinib, or both in human epidermal growth factor receptor 2-positive operable breast cancer: results of the randomized phase II CHER-LOB study. J Clin Oncol. 2012;30:1989–95. doi: 10.1200/JCO.2011.39.0823. [DOI] [PubMed] [Google Scholar]
- 20.Robidoux A, Tang G, Rastogi P, Geyer CE, Azar CA, Atkins JN, et al. Lapatinib as a component of neoadjuvant therapy for HER2-positive operable breast cancer (NSABP protocol B-41): an open-label, randomised phase 3 trial. Lancet Oncol. 2013;14:1183–92. doi: 10.1016/S1470-2045(13)70411-X. [DOI] [PubMed] [Google Scholar]
- 21.Hurvitz SA, Miller JM, Dichmann R, Perez AT, Patel R, Zehngebot LM, et al. Final analysis of a phase II 3-arm randomized trial of neoadjuvant trastuzumab or lapatinib or the combination of trastuzumab and lapatinib, followed by six cycles of docetaxel and carboplatin with trastuzumab and/or lapatinib in patients with HER2+ breast cancer (TRIO-US B07) [abstract] Cancer Res. 2013;73:S1–02. [Google Scholar]


