Abstract
Purpose
Programmed death ligand-1 (PD-L1) tumor expression represents a mechanism of immune escape for melanoma cells. Drugs blocking PD-L1 or its receptor have shown unprecedented activity in melanoma, and our purpose was to characterize tumor PD-L1 expression and associated T-cell infiltration in metastatic melanomas.
Experimental Design
We used a tissue microarray (TMA) consisting of two cores from 95 metastatic melanomas characterized for clinical stage, outcome and anatomic site of disease. We assessed PD-L1 expression and tumor infiltrating lymphocytes (TIL) content (total T cells and CD4/CD8 subsets) by quantitative immunofluorescence.
Results
High PD-L1 expression was associated with improved survival (P=0.02) and higher T cell content (P=0.0005). Higher T cell content (total and CD8 cells) were independently associated with improved overall survival; PD-L1 expression was not independently prognostic. High TIL content in extra-cerebral metastases was associated with increased time to developing brain metastases (P=0.03). Cerebral and dermal metastases had slightly lower PD-L1 expression than other sites, not statistically significant. Cerebral metastases had less T cells (P=0.01).
Conclusions
T cell infiltrated melanomas, particularly those with high CD8 T cell content, are more likely to be associated with PD-L1 expression in tumor cells, an improved prognosis, and increased time to development of brain metastases. Studies of T cell content and subsets should be incorporated into trials of PD-1/PD-L1 inhibitors to determine their predictive value. Furthermore, additional studies of anatomic sites with less PD-L1 expression and T cell infiltrate are needed to determine if discordant responses to PD-1/PD-L1 inhibitors are seen at those sites.
Keywords: PD-L1, TILs, brain metastasis, melanoma
INTRODUCTION
Melanoma is considered an “immunogenic” tumor, responsive to immunologic manipulation. Cytokine therapies, including high dose interleukin-2 and interferon-α have been used to treat melanoma for decades, with responses in subsets of patients (1-3). In recent years, immune checkpoint inhibitors, including monoclonal antibodies against CTLA-4, PD-1, PD-L1, LAG-3 and others have been studied. Antibodies that activate co-stimulatory molecules on T cells, such as GITR, CD-137, OX-40, CD-27 and CD-40 have entered clinical trials, as reviewed (4-5).
Ipilimumab, the first anti-CTLA-4 antibody was FDA approved in 2011 based on improvement in overall survival compared with a peptide vaccine (6). Pembrolizumab was the first PD-1 inhibitor to be approved (7-8). Nivolumab, also a PD-1 inhibitor, was approved for patients with metastatic melanoma based on unprecedented activity (9-10), and additional inhibitors of PD-1 and PD-L1 are being evaluated in clinical trials. Notably, response rates to nivolumab and pembrolizumab are approximately 30%, significantly higher than older immune therapies, and responses can be durable.
Attempts have been made to identify predictors of response to PD-1/PD-L1 inhibitors. The overall response rate in a phase I study of nivolumab was 41%, and in patients with available tissue for assessment of PD-L1 levels in tumor cells, there was a relationship between ligand expression and response. None of the PD-L1 negative tumors responded, while 36% of the PD-L1 expressing tumors responded (9). Of note, not all patients had melanoma. A second phase I trial using nivolumab in solid tumors showed a similar result (11). In the phase I study of pembrolizumab in patients with advanced melanoma, the percentage of patients with PD-L1 positive tumors was higher (71%), as reviewed (12). The response rate among patients with PD L1 positive or negative tumors was 49% and 13%, respectively, again indicating an association between PD-L1 positivity and response. When the threshold for positivity was raised to >10% of tumor cells, response rates in PD-L1 positive and negative group rose to 52% and 23%. MPDL3280A is a monoclonal antibody to PD-L1; in a phase I trial of this drug in multiple tumor types, some association was found between treatment response and PD-L1 staining in the tumor microenvironment (but not in tumor cells) (13).
A variety of staining reagents and antibodies were used in these studies, and variable cutpoints for positivity and negativity were employed; some studies used >1% tumor staining as a cutpoint for positivity, while others used >5%. Despite the variability, studies consistently show that although PD-L1 positive tumors are more likely to respond to therapy, not all do, while some of the patients without apparent tumor or tumor microenvironment expression of PDL1 do respond. Additional factors therefore affect activity of this class of agents.
Taube et al. recently studied melanoma specimens from 110 patients (56 metastatic, 54 primary specimens) for presence of T cells and PD-L1 staining patterns (14). They identified four patient groups; 41% had tumors that were both PD-L1 positive and had associated tumor infiltrating lymphocytes (TILs), 1% had PD-L1 positive tumors without TILs, 13% had TILs without PD-L1 positivity and 45% had neither. Tumor inflammation and the type of infitrating cells might affect response to therapy, as secretion of interferon- γ by T cells is known to induce PD-L1 tumor expression (15). This interaction might potentiate activity of PD-1/PD-L1 inhibiting antibodies.
The location of a metastatic tumor might affect the inflammatory process. For example, Hamilton et al studied 26 matched brain and extra-cerebral metastases for gene expression profiling and found differences in pathways associated with T cell activity (16).
Our purpose was to expand on the studies by Taube et al., and further characterize T cell infiltration in PD-L1 positive and negative metastatic melanoma specimens and to determine the association with clinical outcome using a larger cohort of metastatic melanoma specimens, well annotated for clinical outcome. Seeing that melanoma tends to metastasize to the brain frequently, we studied the assciation between PD-L1 positivity and/or T cell infiltrate and time to development of brain metastases. PD-L1 expression and T cell infiltrates were studied in metastatectomy specimens from a number of sites, including brain lesions. To obtain more accurate measures of PD-L1 expression and TILs, we employed a method of quantitative immunofluorescence and characterized TILs by CD-4 versus CD-8 expression, which has been used in a number of prior studies (17-19).
MATERIAL AND METHODS
Cell lines and Western blotting
Early passage melanoma cell cultures and cell lines were grown in OptiMEM media (Invitrogen) supplemented with 10% heat-inactivated FBS (Invitrogen) and antibiotic-antimycotic (penicillin, streptomycin, amphotericin B; Invitrogen). Western blotting was performed by standard methods. β-Actin was utilized to determine sample loading.
Tissue microarray (TMA) construction
We constructed a TMA of metastatic melanoma samples using methods previously described (20-22). This TMA has been previously described (23). Collection of specimens and clinical data was approved by a Yale University Institutional Review Board. Specimens were resected between 2000 and 2011. A pathologist re-examined each case and selected a representative region of invasive tumor for coring. Each tumor was represented by two cores from different areas of the specimen. This cohort included 95 assessable cases.
Clinical characteristics
The cohort included 62% males, 38% females. Age at diagnosis ranged from 20 to 79 (mean-55.4). Follow-up time was up to 187.65 months, mean-31.2 months (23). At diagnosis of stage IV disease, 13% had M1a disease, 29%-M1b and 58%-M1c. LDH was elevated in 31%; BRAF and NRAS mutations were found in 51% and 24%. Time to development of brain metastasis was up to 187.65 months, mean-19.69. 71% received some type of systemic immunotherapy while 29% did not; three patients received PD-1 or PD-L1 inhibitors. Of the patients treated with immune therapy, 42% had sample acquisition after administration of immune therapy (one third received ipilimumab), 58% had sample acquisition before. Specimens included metastases from several sites: lymph nodes (26), skin (11), soft tissue (25) and visceral metastases (53 total, 40 cerebral and 13 extra-cerebral). In 17 cases more than one metastatic site was represented.
To verify antibody specificity, we used control TMAs containing placental and tonsil tissue (known to be positive for PD-L1) and pellets from MEL-624 cell lines, overexpressing or not overexpressing PD-L1, as previously described (14, 17).
Immunofluorescence and Automated Quantitative Analysis (AQUA)
TMAs were heated for 30 minutes at 60°C, deparaffinized and rehydrated through xylene and serial dilutions of ETOH and H2O. Slides were boiled at 100°C for 10 minutes in antigen retrieval buffer (Tris-EDTA-pH9 buffer, DAKO) and incubated in peroxidase blocking reagent (K1500, DAKO) for 5 minutes. For PD-L1 staining, slides were incubated at room temperature for 15 min in ACE blocking buffer. To block endogenous biotin, slides were first incubated in Avidin blocking solution followed by Biotin blocking reagent (Vector Laboratories) for 15 minutes at 37°C. Slides were incubated at 4°C overnight with anti–PD-L1 mouse monoclonal antibody (clone 5H1, generated by Dr. Lieping Chen) diluted at 1:400 in ACE block (24). Simultaneously, slides were incubated overnight with rabbit anti-S100 (1:100, cat#Z0311, DAKO) to localize cell membrane/cytoplasmic compartment and to create a tumor mask. As a negative control, a second TMA slide was incubated overnight in ACE block only. All TMAs were then incubated for 45 minutes at RT with biotynilated anti-mouse IgG (1:500, BA-2001, Vector laboratories), followed by incubation with the ABC kit (Vector Laboratories) for 15 minutes. Slides were covered with amplification reagent (K1500, DAKO) for 4 minutes at RT followed by Streptavidin-HRP (K1500, DAKO) for 15 minutes and then Cyanine-5-tyramide (Perkin Elmer) for target detection. For T cell detection, serial slide cuts were incubated at 4°C overnight with rabbit anti-CD3 (1: 3200, cat# A0452, DAKO) and simultaneously with either mouse anti-CD4 (1:400, cat#M7310, DAKO), mouse anti-CD8 (1:200, cat#M7103, DAKO), mouse anti-FOXP3 (1:200, cat#ab20034, Abcam), or mouse anti-S100 antibodies in 0.3% bovine serum albumin/TBS. Goat anti-rabbit horseradish peroxidase-decorated polymer backbone (Envision, Dako) was utilized to amplify the CD3 signal, visualized with Cyanine-3-tyramide. Slides were incubated twice for 7 minutes with 100mM benzoic hydrazide (Sigma) and 50mM hydrogen peroxide in PBS to quench the HRP. Goat anti-mouse HRP-decorated polymer backbone (Envision, Dako) followed by Cyanine-5-tyramide were used to detect signal for CD4 and CD8. For visualization of S100, a secondary goat IgG conjugated to Alexa 546 (Molecular Probes, Inc.) was utilized. A nuclear mask was created by incubating the slides with 4,6-diamidine-2-phenylindole (DAPI) (Invitrogen, dilution 1:500).
Quantitative Determination of Target Expression
Details of image capturing and algorithms used for quantitative determination of target expression have been previously described (25). PD-L1 signal on cells within the S100 tumor mask was compartmentalized and expressed as average signal intensity within the assayed component (AQUA score), with scores on a scale of 0–255. To assess the degree of tumor-infiltrating lymphocytes (TIL), we used the percentage of either CD3-, CD4- or CD8-positive T-cell area within the histospot.
Statistical Analysis
JMP version 5.0 software was used for analysis (SAS Institute). Associations between continuous AQUA scores and clinical/pathological parameters were assessed by analysis of variance. Cox proportional hazards analysis was used to test the association between expression of PD-L1 and T cell content and survival. Survival curves were constructed using the Kaplan-Meier method.
RESULTS
PD-L1 expression and its association with survival in patients with stage IV metastatic melanoma
Anti-PD-L1 antibody specificity was verified by Western blot on 16 melanoma cell lines, including MEL624 which was non-transfected or transfected to overexpress PD-L1. This antibody was highly specific, since it generated a single dominant band corresponding to the correct molecular weight (Supplementary Figure S1). As expected, PD-L1 was expressed at high levels in MEL624PD-L1+ cells but not the non-transfected cells, and was variably expressed in other melanoma cell lines; five had no detectable PD-L1 levels, six showed moderate-high PDL1 expression, two had low level expression.
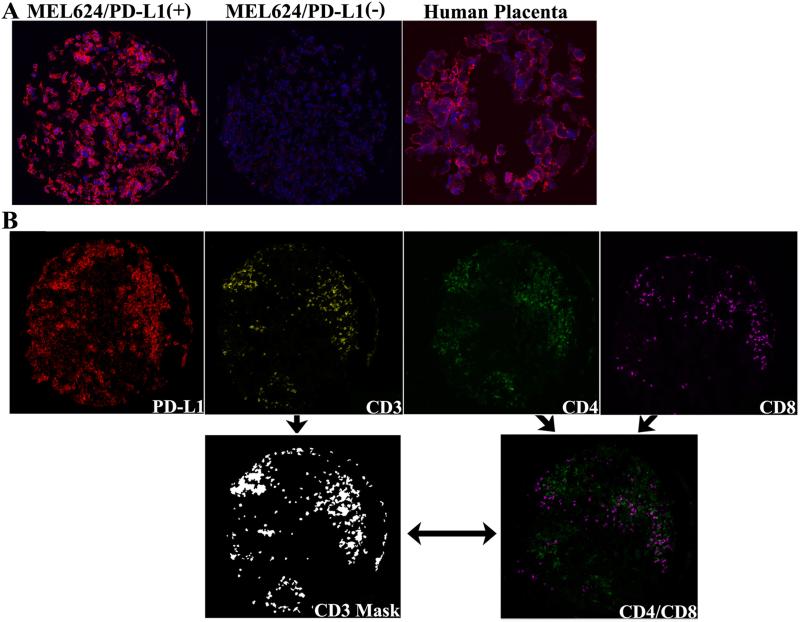
To optimize staining conditions for quantitative immunofluorescence (QIF), we constructed a tissue microarray (TMA) containing positive tissue controls, including human tonsil tissue, human placenta and cores prepared from the MEL624PD-L1+ or MEL624PD-L1− cells. We further confirmed 5H1 antibody specificity by QIF (Figure 1A).
Figure 1.
Quantitative immunofluorescent staining of PD-L1 on tumor cells and quantification of CD3-, CD4- and CD8 TILs. A. Staining is shown in histospots of formalin fixed, paraffin embedded MEL624 cells transfected to overexpress PD-L1 or non-transfected and human placental tissue. DAPI (4,6-diamidine-2-phenylindole) was utilized to identify nuclei and Cy5 to visualize the target. B. Example of a tumor spot showing high PD-L1 expression and high CD3-, CD4- and CD8 lymphocytic content. PD-L1 intensity on tumor cells was calculated on a scale of 1-250. The percentage of either CD3-positive T-cell area or of the CD4- or CD8-positive T-cell subsets within the total tumor area (including stroma) was used to assess the degree of tumor lymphocytic infiltration (TIL density) on a cohort of metastatic melanoma specimens.
To characterize expression of PD-L1 and T cell infiltrates in metastatic melanoma, we utilized an array with 95 cases. Staining for PD-L1 was membranous and present in most cases within the tumor compartment, created by the S100 mask. Figure 1B shows an example of a PDL1 positive case. In some cases PD-L1 was also expressed outside the tumor mask in the tumor microenvironment. Histospots were excluded if tissue was rendered insufficient (<3% of the histospot area) and if there was anomalous staining due to either abundant necrotic tissue or high background of the specimen on the negative control slide due to high endogenous biotin.
Using the Pearson correlation test we compared scores from the two cores for each specimen and found good intra-tumor reproducibility between matching cores for PD-L1 expression; R=0.87 (P<0.0001). Thus average AQUA scores were calculated for each case. The distribution of AQUA scores for PD-L1 ranged from 2.99 to 113.6 (mean-19.54). PD-L1 expression in tumor cells was previously shown to predict better outcome in metastatic melanoma (14). To verify this using our automated method, we analyzed the association between AQUA scores, dichotomized into ‘high’ and ‘low’ by the median score (15.43) and overall survival (OS). By Cox univariate analysis of dichotomized AQUA scores, high PD-L1 expression was associated with longer survival and a 29% risk reduction (HR=0.71; CI (0.52-0.95), P=0.02). To depict the association between high PD-L1 expression and improved survival, we used the Kaplan-Meier method; high PD-L1 is significantly associated with longer OS (Figure 2A) (median 36.06 vs. 20.27 months; Log-Rank P=0.02). On multivariable analysis, PDL1 did not retain independent prognostic value (P=0.23). Other variables included in the model - age, gender, M stage and LDH - were not independently associated with survival.
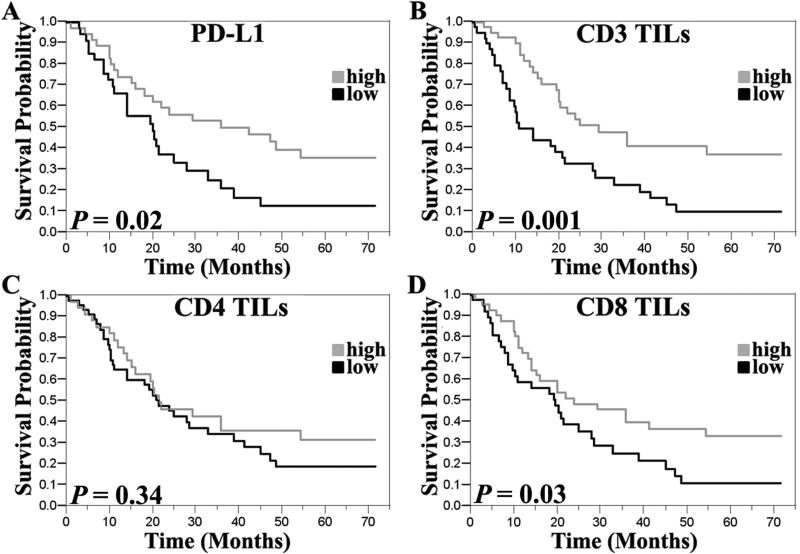
Figure 2.
Kaplan-Meier curves showing the association between PD-L1 expression or TIL density and overall survival. The median PD-L1 intensity score in our cohort was utilized to dichotomize scores into low/high categories while the median CD3 TIL area was used as a threshold for defining high/low TIL density. High PD-L1 expression and high density of either CD3 positive TILs or the CD8 positive subset were significantly associated with longer overall survival.
By analysis of variance, we found no significant association between PD-L1 expression and other clinical variables including age, gender, LDH levels, M stage or presence of B-Raf and N-Ras mutations. 71% of these patients received some type of systemic immunotherapy while 29% did not and three received PD-1/PD-L1 inhibitors. There was no survival difference between the two groups (data not shown), suggesting that the association between PD-L1 expression and improved survival is not dependent on systemic immune therapy in patients who did not receive PD-1/PD-L1 inhibitors.
Quantification of TIL and association with PD-L1 expression
Taube et al. previously showed that the majority of PD-L1 positive tumors also contained TILs (14). To verify this, we used AQUA to quantify the degree of TIL as the percent area of CD3 expressing cells. Quantification was conducted by calculating the percent of TIL out of the total tumor area. We conducted further subset analysis by studying CD4, CD8 expressing TILs. To assess heterogeneity within each case, we used linear regression and found a high degree of correlation between CD3 content in matching cores representing each tumor (R=0.78). Correlation coefficients were somewhat lower for CD4 and CD8 subsets (R=0.52 for CD4 TILs, R=0.65 for CD8 TILs). Approximately half the metastatic melanomas demonstrated presence of intra-tumor immune infiltrates, consistent with findings of Taube et al. (14). Given this reported distribution, we utilized the median value of CD3TIL area as a threshold for defining “high” TIL density versus “low” TIL density melanomas. The area of CD3 TILs ranged from 0%-89.96% (mean-7.53%; median-1.94%). Most cases contained both CD4- and CD8-positive T-cell subsets and only a minority of cases were only CD8 positive; 70% of the high TIL cases (CD3 TIL area above the median) had both high CD4- and CD-8 TIL infiltration.
In the majority of cases, high PD-L1 expression was associated with high TIL densities as measured by the presence of CD3. High PD-L1 was similarly associated with infiltration of both CD4- and CD8 T-cell subsets. Associations measured by Chi-square analysis and by two-sample t test utilizing continuous PD-L1 scores are shown in Table 1 and Supplementary Figure S2. An example of a TIL dense tumor spot demonstrating high CD3-, CD-4- and CD8 lymphocytic infiltrations and high PD-L1 expression is shown in Figure 1B.
Table 1.
Chi-square (χ2) analysis of PD-L1 expression and TIL density
| PD-L1 Expression | CD3 TILs (P =0.0016) | CD4 TILs (P = 0.0002) | CD8 TILs (P< 0.0001) | |||
|---|---|---|---|---|---|---|
| Low Density | High Density | Low Density | High Density | Low Density | High Density | |
| PD-L1 (High) | 12.5% (9/34) | 34.7% (25/34) | 16.9% (12/36) | 33.8% (24/36) | 8.2% (6/35) | 39.7% (29/35) |
| PD-L1 (Low) | 33.3% (24/38) | 19.5% (14/38) | 38% (27/35) | 11.3% (8/35) | 38.4% (28/38) | 13.7% (10/38) |
Given the association between PD-L1 expression and TIL presence, we studied the association between tumor inflammation and overall survival. Utilizing the Cox proportional hazards method, high TIL densities were associated with improved OS. The association was statistically significant when analysing all TILs (by CD3 staining) and the CD8 subset, but not CD4 positive cells (HR=0.65; CI (0.49-0.85), P=0.0022 for CD3 TILs; HR=0.75; CI (0.57-0.98), P=0.04 for CD8 TILs; HR=0.87; CI (0.65-1.14), P=0.32 for CD4 TILs). To visualize the association between TIL density and survival, Kaplan-Meier curves were generated and P-values corresponding to these curves were obtained by the Mantel-Cox log-rank method; Figure 2 (B D) shows significant differences in survival between patients with high versus low CD3 positive TILs and the CD8 positive subset of TILs, but no differences based on CD4 expression. On multivariable analysis, both high density of CD3 cells and the CD8 subset had independent prognostic value (HR=0.57; CI (0.34-0.94), P=0.02 and HR=0.62; CI (0.40-0.99), P=0.05, respectively) (Supplementary Tables S1, S2). PD-L1 expression did not retain its independent prognostic value in these models, likely due to its association with CD3 positive TIL. No significant association was found between TIL density (CD3-postive or CD4- and CD8-positive subsets) and other clinical variables including age, gender, M stage, LDH levels or presence of B-Raf and N-Ras mutations.
To further characterize the TIL population we studied FOXP3 expression. Expression was somewhat variable in replicate histospots from the same patient (R=0.48), and was slightly higher in tumors with high PD-L1 (P=0.07 by χ2 analysis). FOXP3 was not associated with overall survival.
PD-L1 expression and TIL infiltration in melanoma brain metastases compared to extracerebral metastases
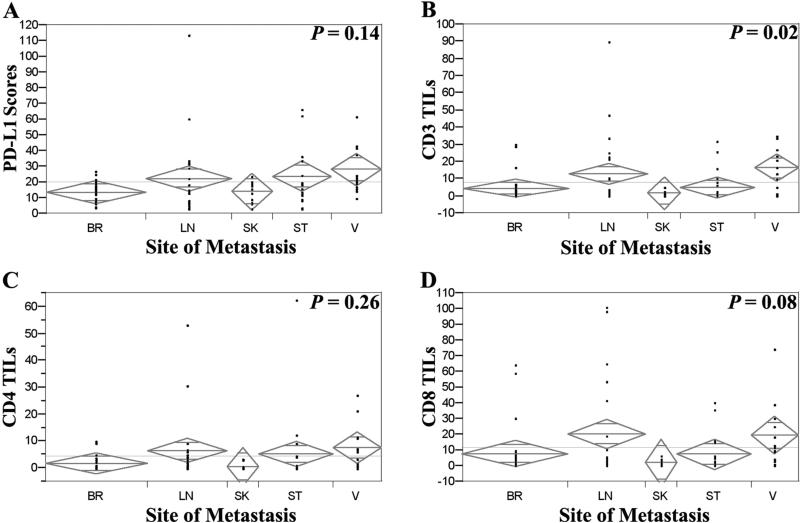
Activity of PD-1/PD-L1 inhibitors is currently being studied in patients with untreated melanoma brain metastases but PD-L1 expression and lymphocytic infiltration have not been studied in cerebral metastases. We therefore analyzed 40 cerebral metastases included in our TMA. The distribution of AQUA scores for PD-L1 in these specimens ranged from 3.74 to 26.7 (mean-13.89). ANOVA of PD-L1 AQUA score distribution across different metastatic sites showed that brain and skin metastases had a trend towards lower PD-L1 expression compared to lymph node, soft tissue and other visceral sites, although differences did not reach statistical significance (P = 0.14, Figure 3A). This difference was not significant by two-way comparison of dichotomized PD-L1 scores comparing cerebral to extra-cerebral sites (P=0.31, Table 2).
Figure 3.
Association between PD-L1 expression or TIL density and tumor characteristics. ANOVA was used to compare PD-L1 expression (continuous intensity scores) or TIL density among specimens of different origin. Brain and skin metastases had the lowest PD-L1 expression and the least TIL infiltration and this association was statistically significant for CD3 TILs. Twenty six specimens were from lymph nodes, 11 from skin, 25 from soft tissue, 40 from the brain and 13 from other (extracerebral) visceral sites.
Table 2.
Chi-square (χ2) analysis of PD-L1 expression and TIL density in melanoma brain metastases
| Site of Metastases | PD-L1 (P = 0.31) | CD3TILs (P = 0.01) | CD4TILs (P = 0.09) | CD8TILs (P = 0.01) | ||||
|---|---|---|---|---|---|---|---|---|
| Low | High | Low Density | High Density | Low Density | High Density | Low Density | High Density | |
| Cerebral | 59.1% (13/22) | 40.9% (9/22) | 70.4% (19/27) | 29.6% (8/27) | 73.1% (19/26) | 26.9% (7/26) | 70.4% (19/27) | 29.6% (8/27) |
| Extra-Cerebral | 46.3% (25/54) | 53.7% (29/54) | 43.3% (26/60) | 56.7% (34/60) | 54.1% (33/61) | 45.9% (28/61) | 41% (25/61) | 59% (36/61) |
The percent area of CD3 positive TILs in brain metastatic specimens was 0-29.75% (mean: 4.6%; median: 1.8%). Comparing across all sites of metastasis by ANOVA, locations with lowest PD-L1 expression (brain and skin metastases) also had the least infiltration of CD3-expressing lymphocytes. The same finding was demonstrated for CD4- and CD8-expressing subsets. The association was statistically significant for CD3 TILs (P=0.02) and trended towards significance for the CD8-expressing TILs (P=0.08) (Figure 3B, D). By chi-square (χ2) analysis comparing high and low T-cell-dense cases, cerebral metastases were more likely to have low T-cell content than extra-cerebral metastases (P=0.01 for CD3TILs). The association trended toward significance for the CD4 subset, and was significant for the CD8 subset (P=0.09 and P=0.01, respectively) (Table 2).
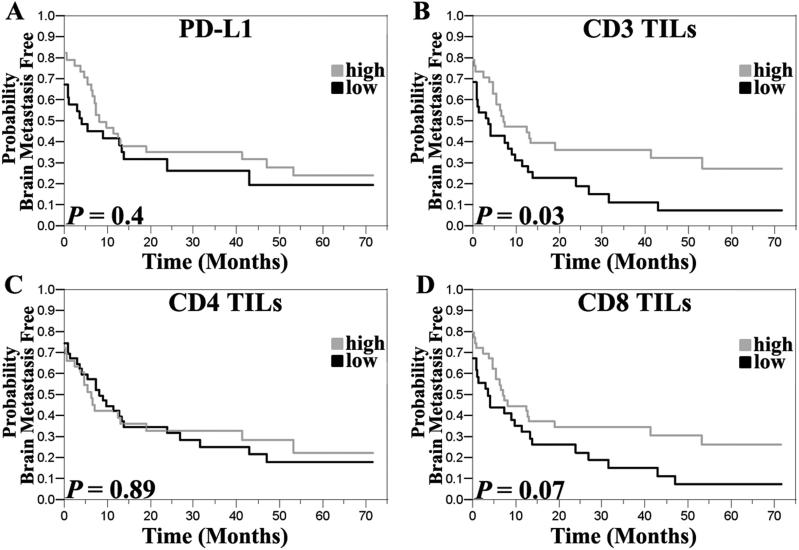
Patients in this cohort were closely followed with serial surveillance MRI of the brain. We studied the association between brain metastasis free survival (BMFS), defined as the interval between diagnosis of metastatic disease and development of brain metastases, and PDL1 expression and lymphocytic infiltration. By Cox proportional hazards, high TIL densities in extra-cerebral sites were associated with increased BMFS. This was statistically significant when analysing all TILs by CD3 staining (HR=0.76; CI (0.58-0.99), P=0.04). There was a trend toward significance for the CD8 subset, but not for PD-L1 and CD4 positive cells (HR=0.8; CI (0.61-1.04), P=0.09 for CD8 TILs; HR=0.89; CI (0.67-1.19), P=0.4; for PD-L1, HR=0.98; CI (0.74-1.28), P=0.9 for CD4 TILs). Kaplan Meier curves with long rank statistics demonstrating these associations are shown in Figure 4. On multivariable analysis, using the Cox proportional hazards model, high TIL density was not an independent predictor of increased BMFS (P>0.05).
Figure 4.
Kaplan-Meier curves showing the association between PD-L1 expression or TIL density and time to development of brain metastases from the time of diagnosis of metastatic melanoma. The median PD-L1 intensity score was utilized to dichotomize scores into low/high while the median CD3 TIL areas was used as thresholds for defining high/low TIL density. High density of CD3 positive TILs was significantly associated with a longer time to development of brain metastasis.
DISCUSSION
With the recent unprecedented success of PD-1/PD-L1 targeting antibodies for treating metastatic melanoma, our purpose was to further characterize PD-L1 expression in metastatic melanoma in the context of T cell infiltrates. High PD-L1 expression was associated with improved OS, but was not independent on multi-variable analysis, likely due to the association with T cell content. The percent area of T cells (using CD3 as a pan-T cell marker) was associated with improved OS on both uni- and multi-variable analysis, and infiltration of the CD8 subset was particularly associated with OS, whereas the CD4 subset was not. PD-L1 expression was lower in cerebral and skin metastases than other sites, and the corresponding T cell infiltration in brain and skin metastases was also less pronounced. High PD-L1 expression and T cell content in extra-cerebral tumors was associated with prolonged time to development of brain metastases.
Our studies confirm those by Taube et al, conducted on a smaller cohort of metastatic melanomas (56 cases) (14). We studied 95 cases using a quantitative method to assess PD-L1 expression and T cell content. Using our automated method, we confirmed the association between PD-L1 expression and TIL content, and the association between high PD-L1 expression and improved survival. PD-L1 expression is up-regulated by T cell secretion of interferon-γ, and therefore patients with T cell dense tumors expressing PD-L1 are likely to have baseline improved immune surveillance (24). In our cohort, the association appears to be independent of systemic immune therapy, although only three patients were treated with inhibitors of PD-1 or PD-L1. Based on preliminary observations among melanoma patients treated with these drugs, the association between PD-L1 expression and TIL content and overall survival is likely to be stronger now that PD-1 inhibitors have been approved for this population (26).
We conducted additional studies of subsets of T cells by analyzing CD4 and CD8 cell content. Both subsets were strongly associated with PD-L1 expression. However, only CD8 infiltrates were associated with improved OS. This is not surprising given the role of memory and effector CD8 cells in the inflammatory response to cytokine secretion and in preventing tumor invasion and metastasis (27-28). Our study was not designed to determine the regulatory versus helper CD4+ cell components, but the former likely explains the lack of association between CD4+ tumor content and improved survival (29). However, our studies support those of Spranger et al who demonstrated co-existence of CD8+ cells and CD4+ suppressive cells, including FOXP3+ regulatory T cells and PD-L1 activated T cells, and suggested that this is due to compensatory mechanisms of tumor immune escape (30). Our findings also support those by Hamilton et al., who found that increased TIL content (both CD3 and CD8) in patients with brain metastases was associated with improved survival (16).
Published predictive correlative studies done on multi-institutional trials have focused primarily on PD-L1 expression. While this clearly correlates with T cell content (total and subsets), the prognostic value of CD3 TILs, in particular the CD8 subset, which is independent of PD-L1 expression, suggests that this should be included in predictive biomarker studies of patients treated with PD-1/PD-L1 inhibitors. This has been done in a small study of multiple tumor types (melanoma, renal cell carcinoma and lung cancer) treated with nivolumab at a single institution (31). Tumor PD-L1 expression remained the strongest predictor of response to nivolumab, however, it is possible that a model incorporating both might best predict response to PD-1/PD-L1 inhibitors.
Our TMA did not include analysis of multiple sites of metastases from individual patients, and did not allow for intra-patient comparison of PD-L1 expression and T cell content. In previous studies in renal cell carcinoma, we showed that in a given patient, PD-L1 expression can vary at different anatomic sites (17). Across all metastatic sites, PD-L1 expression appears to be somewhat lower in brain and skin metastases compared to other sites, although differences were not statistically significant, and the corresponding T cell infiltration analysis in brain and skin metastases indicated that metastases at these sites indeed have less T cell content. This is likely due to variability in factors associated with the tumor microenvironment. For example, higher PD-L1 tumor expression in lymph node metastases might be due to cytokine secretion by surrounding lymphocytes (32). Some organs such as the lungs, have an abundance of dendritic cells and macrophages, cells that secrete interferon-γ (33-34). This might result in increases in tumor PD-L1 in these organs.
Recent studies by Tumeh et al and Taube et al have shown that the location of T cell infiltrate and PD-L1-expressing cells within a tumor sample is of great importance; presence of CD-8 TILs and PD-L1 expressing cells at the invasive margin is associated with a greater likelihood of response to therapy (31, 35). Our study used tissue microarrays that were constructed utilizing tissue from the most central location when possible. Many patients in this cohort did not have full metastatectomies, but rather excisional biopsies, and the invasive margin could not be determined. However, we believe that cores utilized in TMAs are reflective of clinical practice in which core or excisional biopsies are conducted at metastatic sites, often using image-guided techniques to access the center of the tumor, rather than full excisions. For predictive studies, however, given the variability in PD-L1 expression and TIL content within a tumor sample, when possible, metastatectomies should be studied rather than core needle or incisional biopsies.
Studies of the association between PD-L1 expression and response to PD-1/PD-L1 targeting drugs using variable cutpoints and reagents demonstrate that patients whose tumors express PD-L1 are more likely to respond to therapy (12). Using a more quantitative method, we demonstrated variability in the degree of PD-L1 expression at different anatomic sites. We note that we were not able to study multiple sites of metastasis in individual patients, and with the data available to us at present, we cannot determine intra-patient variability in PD-L1 expression at different anatomic sites. Taube et al analyzed some patients with multiple specimens from different anatomic sites (31). They noted some differences in PD-L1 staining and in T-cell infiltrate, but found that the highest scoring sample among multiple biopsies was the most likely to predict response to PD-L1 therapy. Inhibition of the PD-1/PD-L1 interaction at one site might result in increased TIL activity at that site and release of cytokines and circulating effector cells, which can result in anti-tumor T cell activity at distant sites which might be PD-L1 negative. Alternatively, differences in PD-L1 expression and T-cell infiltrate at different anatomic sites might explain discordant responses seen in some patients, who might have shrinkage in one location and growth in another (7-10). The strong correlation between PD-L1 expression and T cell content within the tumor (as represented by the S100 tumor mask) further supports studies by Tumeh et al, who demonstrated close proximity between PD-L1 and PD-1 expressing cells (35). However, a limitation of our method is the inability to distinguish PD-L1 T cell expression from PD-L1 melanocyte expression within the tumor mask and PD-L1 staining on macrophages, monocytes and microglial cells. Methods such as flow cytometry can determine PD-L1 expression within cellular subsets, although flow cytometry cannot be interpreted within the histological context. However, newer in situ methods that involve multiplexing of additional cellular components are being developed and might facilitate measurement of PD-L1 expression in additional cell types, such as macrophages, in the tumor microenvironment. Future studies should incorporate more quantitative measures of PD-L1 expression and T cell content, and when possible, more than one metastatic site should be studied, with a particular focus on the site most requiring treatment, rather than previously resected tumor sites.
Brain metastases pose a particular challenge in the treatment of metastatic melanoma. The incidence of cerebral dissemination in this disease is highest of all malignancies (36). Historically the prognosis has been poor, but with improved methods of local control of brain lesions, the prognosis is improving, and additional studies of this patient population are warranted. Our study shows increased time to brain metastases in PD-L1 positive tumors with high TIL content. However, the numbers in our study are small and validation in additional patient cohorts, particularly patients with paired brain and extra-cerebral samples, is warranted. Moreover, our study is inherently limited by the fact that these metastatectomy samples were obtained at variable timepoints after diagnosis of metastatic disease, and inflammatory content might change with time and with therapy.
Ongoing studies of PD-1 inhibitors in patients with untreated brain metastases (such as NCT02085070) will enable us to determine whether brain lesions are biologically different in terms of T cell content and activity and whether brain metastases can be treated systemically with PD-1 inhibitors. The lower PD-L1 expression and TIL infiltrate in dermal metastases in our study provides some reassurance that the differences might not have therapeutic implications, as clinical experience indicates that dermal metastases are not less sensitive to this class of drugs.
In summary, our studies confirm previous studies by Taube et al showing an association between PD-L1 expression and improved prognosis. These studies were conducted in a larger metastatic melanoma cohort using an automated, quantitative method. We further confirmed the association between PD-L1 expression and T cell infiltrate (by CD3 positivity), and characterized the T cell subtypes. Both overall TIL content and the percent of CD8 positive cells were independent predictors of improved survival, and retained their independence on multivariable analysis. High TIL content in extra-cerebral specimens was associated with increased time to developing brain metastases, suggesting that patients with higher TIL density tumors might be less likely to have tumor dissemination to the brain. Our study did not include multiple specimens from different anatomic sites in individual patients, but the anatomic site of biopsy appears to be associated with variability in PD-L1 expression and TIL content, with dermal and cerebral metastases having a lower TIL content and less PD-L1 expression. Biomarker studies of patients treated with PD-1/PD-L1 inhibitors should include specimens from multiple sites, when possible, to determine whether these differences are clinically meaningful.
Supplementary Material
STATEMENT OF TRANSLATIONAL RELEVANCE.
Given the recent success of PD-1/PD-L1 inhibitors in clinical trials for metastatic melanoma, we used a well annotated cohort of metastatic melanoma samples to characterize PDL1 expression and T cell content and the association with clinical outcome, using an automated, quantitative method. PD-L1 expressing tumors were more likely to have higher TILs. Both overall TIL content and the percent of CD8 positive cells were independent predictors of improved survival, and retained their independence on multivariable analysis. Patients with specimens lacking inflammation were more likely to develop early brain metastases. Moreover, the anatomic site of biopsy appears to be associated with variability in TIL content. Biomarker studies of patients treated with PD-1/PD-L1 inhibitors should include specimens from multiple sites, when possible, to determine whether these differences are clinically meaningful and whether assays combining PD-L1 expression and TIL characterization might be more predictive of response to therapy than PD-L1 alone.
Acknowledgements
Funding: This work was supported by NIH grants R0-1 CA158167 and K24CA172123 (H. Kluger, PI), Yale SPORE in Skin Cancer, P50 CA121974 (R. Halaban, PI), pilot funding from the Yale Cancer Center (H. Kluger, PI), CTSA Grant Number KL2 TR000140 (L. Jilaveanu, PI) from the National Center for Research Resources (NCRR) and the National Center for Advancing Translational Science (NCATS), components of the National Institutes of Health (NIH), and NIH roadmap for Medical Research and a grant from the Lung Cancer research Foundation-LUNGevity and Melanoma Research Alliance, Award#308721 (L. Jilaveanu, PI).
Footnotes
Financial disclosures/conflicts of interest: none
REFERENCES
- 1.Acquavella N, Kluger H, Rhee J, Farber L, Tara H, Ariyan S, et al. Toxicity and activity of a twice daily high-dose bolus interleukin 2 regimen in patients with metastatic melanoma and metastatic renal cell cancer. J Immunother. 2008;31:569–76. doi: 10.1097/CJI.0b013e318177a4ba. [DOI] [PubMed] [Google Scholar]
- 2.Miller RL, Steis RG, Clark JW, Smith JW, 2nd, Crum E, McKnight JE, et al. Randomized trial of recombinant alpha 2b-interferon with or without indomethacin in patients with metastatic malignant melanoma. Cancer Res. 1989;49:1871–6. [PubMed] [Google Scholar]
- 3.Wong MK, Kaufman HL, Daniels GA, McDermott DF, Aung S, Lowder JN, et al. Implementation of an Interleukin-2 National Registry: an opportunity to improve cancer outcomes. J Immunother Cancer. 2014;2:20. doi: 10.1186/2051-1426-2-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen L, Flies DB. Molecular mechanisms of T cell co-stimulation and co-inhibition. Nat Rev Immunol. 2013;13:227–42. doi: 10.1038/nri3405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sznol M. Blockade of the B7-H1/PD-1 pathway as a basis for combination anticancer therapy. Cancer J. 2014;20:290–5. doi: 10.1097/PPO.0000000000000056. [DOI] [PubMed] [Google Scholar]
- 6.Hodi FS, O'Day SJ, McDermott DF, Weber RW, Sosman JA, Haanen JB, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363:711–23. doi: 10.1056/NEJMoa1003466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bagcchi S. Pembrolizumab for treatment of refractory melanoma. Lancet Oncol. 2014;15:e419. doi: 10.1016/s1470-2045(14)70348-1. [DOI] [PubMed] [Google Scholar]
- 8.Hamid O, Robert C, Daud A, Hodi FS, Hwu WJ, Kefford R, et al. Safety and tumor responses with lambrolizumab (anti-PD-1) in melanoma. N Engl J Med. 2013;369:134–44. doi: 10.1056/NEJMoa1305133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Topalian SL, Hodi FS, Brahmer JR, Gettinger SN, Smith DC, McDermott DF, et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med. 2012;366:2443–54. doi: 10.1056/NEJMoa1200690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Topalian SL, Sznol M, McDermott DF, Kluger HM, Carvajal RD, Sharfman WH, et al. Survival, durable tumor remission, and long-term safety in patients with advanced melanoma receiving nivolumab. J Clin Oncol. 2014;32:1020–30. doi: 10.1200/JCO.2013.53.0105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brahmer JR, Drake CG, Wollner I, Powderly JD, Picus J, Sharfman WH, et al. Phase I study of single-agent anti-programmed death-1 (MDX-1106) in refractory solid tumors: safety, clinical activity, pharmacodynamics, and immunologic correlates. J Clin Oncol. 2010;28:3167–75. doi: 10.1200/JCO.2009.26.7609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mahoney KM, Atkins MB. Prognostic and predictive markers for the new immunotherapies. Oncology (Williston Park) 2014:28. [PubMed] [Google Scholar]
- 13.Herbst RS, Soria JC, Kowanetz M, Fine GD, Hamid O, Gordon MS, et al. Predictive correlates of response to the anti-PD-L1 antibody MPDL3280A in cancer patients. Nature. 2014;515:563–7. doi: 10.1038/nature14011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Taube JM, Anders RA, Young GD, Xu H, Sharma R, McMiller TL, et al. Colocalization of inflammatory response with B7-h1 expression in human melanocytic lesions supports an adaptive resistance mechanism of immune escape. Sci Transl Med. 2012;4:127ra37. doi: 10.1126/scitranslmed.3003689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gibson A, Ogese M, Sullivan A, Wang E, Saide K, Whitaker P, et al. Negative regulation by PD-L1 during drug-specific priming of IL-22-secreting T cells and the influence of PD-1 on effector T cell function. J Immunol. 2014;192:2611–21. doi: 10.4049/jimmunol.1302720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hamilton R, Krauze M, Romkes M, Omolo B, Konstantinopoulos P, Reinhart T, et al. Pathologic and gene expression features of metastatic melanomas to the brain. Cancer. 2013;119:2737–46. doi: 10.1002/cncr.28029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jilaveanu LB, Shuch B, Zito CR, Parisi F, Barr M, Kluger Y, et al. PD-L1 Expression in Clear Cell Renal Cell Carcinoma: An Analysis of Nephrectomy and Sites of Metastases. J Cancer. 2014;5:166–72. doi: 10.7150/jca.8167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schalper KA, Velcheti V, Carvajal D, Wimberly H, Brown J, Pusztai L, et al. In situ tumor PD-L1 mRNA expression is associated with increased TILs and better outcome in breast carcinomas. Clinical cancer research : an official journal of the American Association for Cancer Research. 2014;20:2773–82. doi: 10.1158/1078-0432.CCR-13-2702. [DOI] [PubMed] [Google Scholar]
- 19.Velcheti V, Schalper KA, Carvajal DE, Anagnostou VK, Syrigos KN, Sznol M, et al. Programmed death ligand-1 expression in non-small cell lung cancer. Lab Invest. 2014;94:107–16. doi: 10.1038/labinvest.2013.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jilaveanu LB, Zito CR, Aziz SA, Conrad PJ, Schmitz JC, Sznol M, et al. C-Raf is associated with disease progression and cell proliferation in a subset of melanomas. Clin Cancer Res. 2009;15:5704–13. doi: 10.1158/1078-0432.CCR-09-0198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McCarthy MM, DiVito KA, Sznol M, Kovacs D, Halaban R, Berger AJ, et al. Expression of tumor necrosis factor--related apoptosis-inducing ligand receptors 1 and 2 in melanoma. Clin Cancer Res. 2006;12:3856–63. doi: 10.1158/1078-0432.CCR-06-0190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McCarthy MM, Pick E, Kluger Y, Gould-Rothberg B, Lazova R, Camp RL, et al. HSP90 as a marker of progression in melanoma. Ann Oncol. 2008;19:590–4. doi: 10.1093/annonc/mdm545. [DOI] [PubMed] [Google Scholar]
- 23.Jilaveanu LB, Parisi F, Barr ML, Zito CR, Cruz-Munoz W, Kerbel RS, et al. PLEKHA5 as a Biomarker and Potential Mediator of Melanoma Brain Metastasis. Clin Cancer Res. 2014 doi: 10.1158/1078-0432.CCR-14-0861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dong H, Strome SE, Salomao DR, Tamura H, Hirano F, Flies DB, et al. Tumor-associated B7-H1 promotes T-cell apoptosis: a potential mechanism of immune evasion. Nature medicine. 2002;8:793–800. doi: 10.1038/nm730. [DOI] [PubMed] [Google Scholar]
- 25.Camp RL, Chung GG, Rimm DL. Automated subcellular localization and quantification of protein expression in tissue microarrays. Nature medicine. 2002;8:1323–7. doi: 10.1038/nm791. [DOI] [PubMed] [Google Scholar]
- 26.PD-1 Inhibitor Approved for Melanoma. Cancer Discov. 2014;4:1249. doi: 10.1158/2159-8290.CD-NB2014-144. [DOI] [PubMed] [Google Scholar]
- 27.Kim MT, Harty JT. Impact of Inflammatory Cytokines on Effector and Memory CD8+ T Cells. Front Immunol. 2014;5:295. doi: 10.3389/fimmu.2014.00295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fridman WH, Remark R, Goc J, Giraldo NA, Becht E, Hammond SA, et al. The immune microenvironment: a major player in human cancers. Int Arch Allergy Immunol. 2014;164:13–26. doi: 10.1159/000362332. [DOI] [PubMed] [Google Scholar]
- 29.Yu SH, Bordeaux JS, Baron ED. The immune system and skin cancer. Adv Exp Med Biol. 2014;810:182–91. doi: 10.1007/978-1-4939-0437-2_10. [DOI] [PubMed] [Google Scholar]
- 30.Spranger S, Spaapen RM, Zha Y, Williams J, Meng Y, Ha TT, et al. Up-regulation of PD-L1, IDO, and T(regs) in the melanoma tumor microenvironment is driven by CD8(+) T cells. Sci Transl Med. 2013;5:200ra116. doi: 10.1126/scitranslmed.3006504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Taube JM, Klein A, Brahmer JR, Xu H, Pan X, Kim JH, et al. Association of PD-1, PD-1 Ligands, and Other Features of the Tumor Immune Microenvironment with Response to Anti-PD-1 Therapy. Clin Cancer Res. 2014;20:5064–74. doi: 10.1158/1078-0432.CCR-13-3271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Loke P, Allison JP. PD-L1 and PD-L2 are differentially regulated by Th1 and Th2 cells. Proc Natl Acad Sci U S A. 2003;100:5336–41. doi: 10.1073/pnas.0931259100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Darwich L, Coma G, Pena R, Bellido R, Blanco EJ, Este JA, et al. Secretion of interferon-gamma by human macrophages demonstrated at the single-cell level after costimulation with interleukin (IL)-12 plus IL-18. Immunology. 2009;126:386–93. doi: 10.1111/j.1365-2567.2008.02905.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vremec D, O'Keeffe M, Hochrein H, Fuchsberger M, Caminschi I, Lahoud M, et al. Production of interferons by dendritic cells, plasmacytoid cells, natural killer cells, and interferon-producing killer dendritic cells. Blood. 2007;109:1165–73. doi: 10.1182/blood-2006-05-015354. [DOI] [PubMed] [Google Scholar]
- 35.Tumeh PC, Harview CL, Yearley JH, Shintaku IP, Taylor EJ, Robert L, et al. PD-1 blockade induces responses by inhibiting adaptive immune resistance. Nature. 2014;515:568–71. doi: 10.1038/nature13954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Flanigan JC, Jilaveanu LB, Faries M, Sznol M, Ariyan S, Yu JB, et al. Melanoma brain metastases: is it time to reassess the bias? Current problems in cancer. 2011;35:200–10. doi: 10.1016/j.currproblcancer.2011.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.