Abstract
Recent studies raised the alarm that the inhibition of sodium-coupled glucose transporter type 2 in humans increases endogenous glucose production rates by an unclear mechanism. Surprisingly, a potential explanation may be linked directly to the alpha-cell. Is this a mechanistic spoiler or an added benefit?
Keywords: SGLT-2 inhibitors, glucagon, alpha-cell, glucose production, HNF4alpha
There has been a resurging awareness that glucagon is an important contributor to the pathophysiology of Type-2 diabetes mellitus (T2DM). In this scenario, the increased glucagon tone accelerates endogenous glucose production (EGP) raising the glycemic load. Consequently, any therapeutic intervention intended to lower glucose, but that also raises glucagon inappropriately, would have diminished efficacy. The gliflozin class of drugs inhibits the low-affinity (high Km), sodium-coupled glucose transporter type 2 (SGLT-2) in the renal proximal tubule. Consequently, renal reabsorption of filtered glucose is diminished, resulting in significant glycosuria. The glucose loss is intrinsic to the improvements in glycemic control. Two recent studies in humans with T2DM treated with different SGLT-2 inhibitors made the notable observation that the dramatic increases in glycosuria were completely offset by augmented EGP within minutes of administration [1, 2]. Such an increase would theoretically blunt the already significant improvements in glycemic control.
Both studies also identified as a potential explanation for the increased EGP that plasma glucagon was also increased up to 12 days later. The initial difference in EGP was driven by a sudden drop in EGP in the placebo group rather than an increase in the treatment arm, and could not be fully explained by measured insulin, glucagon or glucose [1]. Notably, glucagon also lagged a few hours behind the EGP change. On subsequent days, the placebo EGP rates recovered to baseline and the difference was maintained with treatment, suggesting the non-steady-state conditions might have impacted the calculations. Earlier contributions of glucagon may have been masked if portal and peripheral glucagon levels had not fully equilibrated. After 28 days of treatment, although EGP remained elevated, glucagon had normalized, identifying a potential disconnect [2]. Without non-diabetic controls, it was not possible to rule out additional contributions related to the improved glucose homeostasis. So while glucagon may not be the sole explanation for increased EGP, it clearly remains in the crosshairs, especially following acute treatment with SGLT-2 inhibitors.
This potential association between SGLT-2 inhibition, increased glucagon and increased EGP during euglycemia is a surprise. With some exceptions, SGLT-2 expression has generally been considered to be limited to the proximal tubules and so a direct islet effect was unanticipated. Notably, during studies in dogs, ruminants and humans treated with the non-selective SGLT inhibitor, phloridzin, glucagon suppression was normal or even improved [3–5]. Finally, perifused islets from mice with whole-body knockout of SGLT-2 on normal or high-fat diets or on the diabetic db/db background did not differ from controls in glucagon secretion at high or low glucose [6]. Taken together, SGLT-2 inhibition in the islet would not have been predicted to stimulate alpha-cells.
The recent study by Bonner et al. suggests an alternative and compelling explanation for the glucagon increase [7]. Namely, that functional SGLT-2 transporters are actually present on pancreatic alpha-cells and that blocking transport restricts glucose uptake to increase glucagon even during euglycemia. Indeed, SGLT-2 mRNA and protein determined by both western blots and confocal microscopy were detected in human alpha-cells, but not beta-cells. Moreover, reducing SGLT-2 (by acutely silencing it or treating with dapagliflozin, a clinically used SGLT-2 inhibitor) provoked glucagon release from alphaTC1.9 cells, human islets and in normal mice in vivo. Notably, the glucagon effect in mice was observed at a dose insufficient to lower plasma glucose [7].
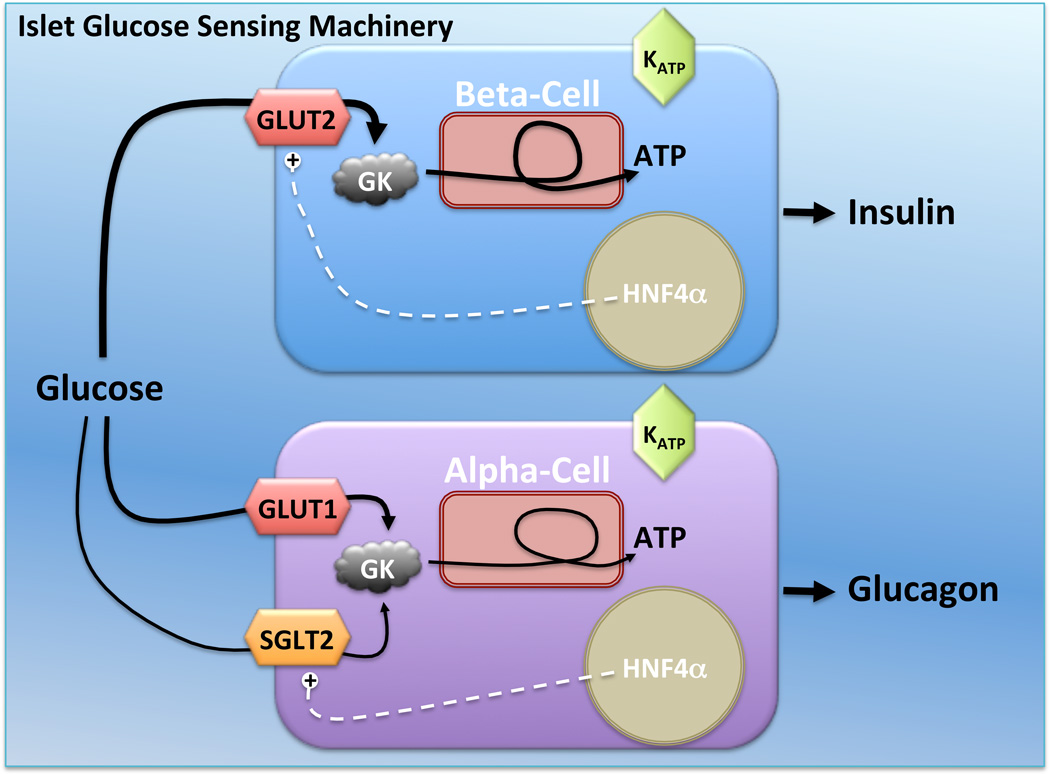
The proposed mechanism for how alpha-cell SGLT-2 inhibition augments glucagon release still requires additional clarification. While there appears to be immunodetectable protein, sodium-glucose currents have not yet been measured to prove quantitatively relevant transport in alpha-cells. Importantly, glucose transport by the high-affinity (low Km) glucose transporter 1 (GLUT1) transporter is well established in alpha-cells (Fig. 1)[8]. Glucose transport does not appear to be rate limiting in alpha-cells where glucose oxidation is controlled by glucokinase at a rate that is nearly an order of magnitude lower than that transported by GLUT1. Importantly, rates of glucose uptake were measured using 3-O-methyl glucose, a substrate transported by GLUT1, but not by SGLT-2 [9]. Thus, until the relative contributions of glucose transport by GLUT1 and SGLT-2 are reconciled, it may be difficult to explain the glucagon stimulation simply as a restriction of glucose transport.
Figure 1. Beta-cells and alpha-cells both use glucose metabolism and KATP channel closure to regulate secretion.
In both cell types glucose oxidation rates are set by glucokinase and cytosolic glucose is not rate-limiting [8]. In beta-cells glucose uptake is via the low-affinity (high Km) GLUT2 transporter. In alpha cells the high-affinity (low Km) GLUT1 and newly reported low-affinity (high Km) SGLT-2 transporter both may transport glucose [7]. The MODY-1 gene, HNFα, in beta-cells regulates GLUT2 expression as well as other proteins in the glucose sensing pathway. A new role for HNFα is identified in the alpha-cell where it is proposed to regulate SGLT-2, though it is unclear if either GLUT1 or GLUT2 are similarly regulated [7, 10].
Another unexpected feature of alpha-cell SGLT-2 was that hepatocyte nuclear factor 4 alpha (HNF4α) promoted its expression. Here, HNF4α was expressed 3–6 fold higher in alpha-cells compared with beta-cells and increased in models of hyperglycemia, obesity and glucose intolerance, but diminished in diabetes [7]. HNF4α is perhaps better known as the maturity onset diabetes of the young (MODY1) gene, where deficiencies cause monogenic diabetes in humans by impairing beta-cell function. In beta-cells, HNF4α promotes expression of many components of the glucose sensing pathway, including GLUT2. Interestingly, recent reports suggest that ectopic expression of HNF4α in alphaTC1.9 cells actually reprograms their differentiation towards a beta-cell phenotype, which is accompanied by suppressed glucagon and induced GLUT2 and insulin expression [10]. Because HNF4α also controls the expression of multiple glucose transporters, the individual contribution of SGLT-2 expression, per se, may be obscured.
It will be important to determine the relationship between SGLT-2 inhibitor therapy and subsequent changes in glucagon and EGP, because these could have significant impact on patient care. In one sense, it is clear that excessive EGP contributes to hyperglycemia in diabetes. It would be easier to maintain euglycemia if EGP were lowered. Towards that goal, therapeutic strategies that reduce glucagon used in combination with an SGLT-2 inhibitor could lower plasma glucose closer to its renal threshold. SGLT-2 inhibitors are clinically effective at lowering not only fasting and prandial glucose, but also favor substantial weight loss. Besides protecting against hypoglycemia, there may be some hidden benefit of the increased EGP in the special case where renal reabsorption is reduced. For example, if the entire EGP excess were excreted, then a higher EGP, in principle, would maximize caloric loss. This would result not only from the grams of sugar lost in the urine, but also from the energetic cost of gluconeogenesis. The latter would be expended largely via enhanced hepatic lipid oxidation, potentially improving insulin sensitivity and reducing steatosis as well. Future studies will be needed to determine whether therapeutic gains can be made by additional suppression of glucagon and/or EGP in combination with SGLT-2 inhibition.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Merovci A, et al. Dapagliflozin improves muscle insulin sensitivity but enhances endogenous glucose production. J Clin Invest. 2014;124(2):509–514. doi: 10.1172/JCI70704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ferrannini E, et al. Metabolic response to sodium-glucose cotransporter 2 inhibition in type 2 diabetic patients. J Clin Invest. 2014;124(2):499–508. doi: 10.1172/JCI72227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McCrimmon RJ, et al. AICAR and phlorizin reverse the hypoglycemia-specific defect in glucagon secretion in the diabetic BB rat. Am J Physiol Endocrinol Metab. 2002;283(5):E1076–E1083. doi: 10.1152/ajpendo.00195.2002. [DOI] [PubMed] [Google Scholar]
- 4.Overton TR, et al. Metabolic adaptation to experimentally increased glucose demand in ruminants. J Anim Sci. 1998;76(11):2938–2946. doi: 10.2527/1998.76112938x. [DOI] [PubMed] [Google Scholar]
- 5.Starke A, et al. Correction of hyperglycemia with phloridzin restores the glucagon response to glucose in insulin-deficient dogs: implications for human diabetes. Proc Natl Acad Sci U S A. 1985;82(5):1544–1546. doi: 10.1073/pnas.82.5.1544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jurczak MJ, et al. SGLT2 deletion improves glucose homeostasis and preserves pancreatic beta-cell function. Diabetes. 2011;60(3):890–898. doi: 10.2337/db10-1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bonner C, et al. Inhibition of the glucose transporter SGLT2 with dapagliflozin in pancreatic alpha cells triggers glucagon secretion. Nat Med. 2015;21(5):512–517. doi: 10.1038/nm.3828. [DOI] [PubMed] [Google Scholar]
- 8.Heimberg H, et al. Differences in glucose transporter gene expression between rat pancreatic alpha- and beta-cells are correlated to differences in glucose transport but not in glucose utilization. J Biol Chem. 1995;270(15):8971–8975. doi: 10.1074/jbc.270.15.8971. [DOI] [PubMed] [Google Scholar]
- 9.Panayotova-Heiermann M, et al. Sugar binding to Na+/glucose cotransporters is determined by the carboxyl-terminal half of the protein. J Biol Chem. 1996;271(17):10029–10034. doi: 10.1074/jbc.271.17.10029. [DOI] [PubMed] [Google Scholar]
- 10.Sangan CB, et al. In vitro reprogramming of pancreatic alpha cells towards a beta cell phenotype following ectopic HNF4alpha expression. Mol Cell Endocrinol. 2015;399:50–59. doi: 10.1016/j.mce.2014.09.009. [DOI] [PubMed] [Google Scholar]