Abstract
We conducted a comprehensive humidifier disinfectant exposure characterization for 374 subjects with lung disease who presumed their disease was related to humidifier disinfectant use (patient group) and for 303 of their family members (family group) for an ongoing epidemiological study. We visited the homes of the registered patients to investigate disinfectant use characteristics. Probability of exposure to disinfectants was determined from the questionnaire and supporting evidence from photographs demonstrating the use of humidifier disinfectant, disinfectant purchase receipts, any residual disinfectant and the consistency of their statements. Exposure duration was estimated as cumulative disinfectant use hours from the questionnaire. Airborne disinfectant exposure intensity (μg/m3) was estimated based on the disinfectant volume (mL) and frequency added to the humidifier per day, disinfectant bulk level (μg/mL), the volume of the room (m3) with humidifier disinfectant, and the degree of ventilation. Overall, the distribution patterns of the intensity, duration and cumulative exposure to humidifier disinfectants for the patient group were higher than those of the family group, especially for pregnant women and patients ≤ 6 years old. Further study is underway to evaluate the association between the disinfectant exposure estimated here with clinically diagnosed lung disease.
Keywords: Humidifier disinfectant, PHMG, PGH, Aerosol, nano-particle, exposure assessment
Introduction
In South Korea, several types of disinfectants have been widely used in humidifiers since 1994 to prevent microbial contamination, but their use has been banned since 2011 due to concerns about their health effects (KSEH, 2012). The use of humidifier peaks during the winter and spring season: more than 70% in atopic dermatitis patients and more than 50% in pregnant women(Kim et. al., 2012). 37.2% of general population (Jeon and Park, 2012), 27.8% of pregnant women (Chang et. al., 2012), and 54.3% of children with atopic dermatitis use a humidifier in their rooms. South Korea is believed to be the only country where a disinfectant was added to the water in humidifiers for extended periods of time. The use of humidifier disinfectants is rarer or non-existent in other countries. Several epidemiological studies conducted in South Korea have concluded that humidifier disinfectants can cause fatal lung disease, including interstitial pneumonitis and wide spread lung fibrosis, necessitating lung transplantation (KCDC, 2011b, KCDC, 2011c, Lee et. al. , 2013, Hong et. al. , 2014, Yang et. al. , 2013). Park et. al. (2014) conducted thorough home investigations of 17 families that had at least two cases of lung disease that were presumed associated with the use of humidifier disinfectant and found no other home or occupational exposures that could explain the lung disease. These lung disease patients included a number of pregnant women, infants and preschoolers, who may be particularly vulnerable. As a result, the Korea Center for Disease Control and Prevention (KCDC) officially collected information on individuals with lung disease who presumed that their disease was related to humidifier disinfectant use. The KCDC is conducting a detailed investigation to determine whether these registered cases are indeed associated with the use of disinfectants. The KCDC investigation includes both clinical examination of the registered lung disease patients and a detailed exposure assessment of humidifier disinfectant exposure for the patients and their family members living in the same home.
This current study describes the systematic and transparent exposure assessment approach that was used to estimate the probability, frequency, and intensity of exposure to humidifier disinfectants for the patients and their family members. These estimates will be used in future epidemiological analyses to examine the association between humidifier disinfectant exposure with clinically diagnosed lung disease. In addition, this approach provides a framework for assessing household exposures that could be applied for other household consumer chemical products.
Material and methods
Study Population
The study participants consisted of 374 subjects with self-reported lung disease who presumed their disease was related to humidifier disinfectant use (patient group) and 303 of their family members who lived in the same residence (family group). The participants represented 250 separate families/households, with 87 households representing more than one lung disease case. The classification of patients and non-patients here was determined by self-report. Clinical confirmation of lung disease cases by a committee composed of pediatric pulmonologists, radiologists, pathologists, and epidemiologists is ongoing and not discussed here. The study protocol was approved by the Institutional Review Boards of Seoul National University (42-2013-07-01), and written informed consent to participate in this study was obtained from the parents or guardians at enrollment.
Collection of Disinfectant Information
We visited registered patient's homes and conducted personal interviews with the patients and the family members and conducted home environment investigations. We asked study participants or, for children, their parents or guardians, to complete detailed questionnaires that collected information related to humidifier disinfectant use, including type of disinfectants used, amount of disinfectants added to the humidifiers, frequency of the disinfectant additions, and the duration of time spent in rooms with humidifiers using open-ended questions. To aid recall, the participants were shown photographs of all types of humidifier disinfectants that had been marketed in South Korea. Responses to the following disinfectant-related questions, translated from Korean, were collected:
Q1. Do you have any evidence to demonstrate the use of disinfectant in the humidifier, such as photographs showing the use of disinfectant, receipts and/or any remaining materials?
Q2. For how many years did you use humidifier disinfectants?
Q3. On average, how many months per year, how many weeks per month and how many days per week did you use humidifier disinfectants in the household?
Q4. As a daily average, how long did you spend in a room, including sleeping, where humidifier disinfectants were being used?
Q5. As a daily average, how often did you add disinfectants to your humidifier?
Q6. As a daily average, how much disinfectant (in mL) did you add to your humidifier?
Q7. As a daily average, how long was the room with the humidifier using disinfectant ventilated, such as with an open window?
Q8. What brands of humidifier disinfectants did you normally use?
The questionnaire also collected information on exposure to other chemical agents that could be related to the development of lung disease, including occupational exposures. Because detailed personal interviews and home investigations found no specific employment, lifestyle, or hazardous agents that could be suspected of having caused the lung disease, assessment results for those agents are not reported here.
Assessment of Probability of Exposure to Humidifier Disinfectant
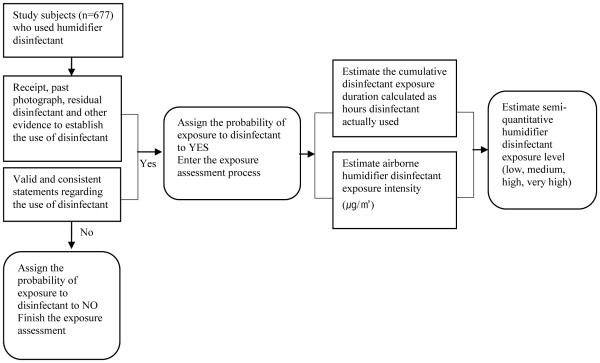
The overall hierarchy framework for estimating the probability, frequency and intensity of exposure to disinfectant based on the collected disinfectant information is shown in Figure 1. The exposure assessment team was blinded to the clinically diagnosed lung disease information of the study subjects.
Fig. 1.
Hierarchical rules for assigning probability, duration, intensity and level of exposure to humidifier disinfectant for study subjects
We developed two steps to determine the probability of exposure to humidifier disinfectant. First, we used photos, receipts for disinfectant purchases and any remaining disinfectants in the home as evidence to demonstrate the household use of disinfectants. If a member of a household provided any of these materials (Q1 in Table 1), we assigned the probability of exposure to disinfectant to “yes” for all members of that household. Second, if no supporting evidence was provided, the investigator assigned the probability of exposure using the responses to several questions related to the use of disinfectants, such as color, method used, the volume of the humidifier disinfectant product used, and the status of the material. If their answers were evaluated as consistent or reliable with disinfectant use, the probability of the use of disinfectants was assigned “yes”. Subjects who indicated no disinfectant use or where there was both lack of supporting evidence and uncertain reliability or consistency in the questionnaire responses were assigned “no” probability of disinfectant exposure.
Table 1.
Level of disinfectant by disinfectant humidifier product from KCDC investigations (KCDC, 2011a)
| Brand name a | Disinfectant contained | Average bulk level, mg/L (no. of samples) |
|---|---|---|
| Oxy | PHMG | 1,276 (n = 3) |
| Lotte yizlak | PHMG | 1,307 (n = 3) |
| Home clinic | CMIT | 127 (n = 3) |
| MIT | 37 (n = 3) | |
| Cefu | PGH | 4,486 (n = 8) |
| Atoaganic | PGH | 300 (n = 3) |
| Cleanup | PHMG | 6,917 (n = 3) |
= four other available disinfectant brands were not analyzed
PHMG = polyhexamethylene guanidine phosphate; PGH = oligo(2-(2-ethoxy)ethoxyethyl guanidinium; CMIT = chloromethylisothiazolinone; MIT = methylisothiazolinone
Assessment of Level of Exposure to Humidifier Disinfectant
For each subject with a probability of “yes”, we estimated the intensity (μg/m3) and duration of exposure to disinfectants as described below.
Exposure Intensity
Because no exposure monitoring data was available, we estimated humidifier disinfectant inhalation exposure based on disinfectant use characteristics. The inhalation disinfectant exposure intensity for each type of disinfectant (Q8) was calculated by multiplying together the bulk level of humidifier disinfectant identified in the specified disinfectant brand during a government mandated inspection conducted by the KCDC (μg/mL)(KCDC, 2011a) (Table 1), the average frequency per day that disinfectant was added to humidifier (Q5), the average volume used for each addition (mL) (Q6), and the room volume (area × height, m3, measured during the home visit) where the humidifier with disinfectant was used. This calculation assumed that the volume of disinfectant added to the humidifier (μg) was completely dispersed into the room (m3), forming an airborne disinfectant concentration (μg/m3). The intensity was then multiplied by a room ventilation factor that was arbitrarily determined according to the level of ventilation in the home (Q7): 1=no or only minor ventilation less than one hour per day; 0.9= ventilation between one and two hours per day; 0.8 = ventilation longer than two hours per day. One of the most challenging aspects of the exposure assessment was to determine ventilation factor or level. Most of people in Korea would use humidifier during winter, when supply of outdoor air is extremely limited. Especially, the door is completely closed during sleeping, which limits the ventilation. We estimated the intensity based on the assumption that the level of ventilation may rarely affect the airborne disinfectant level. We categorized the estimated quantitative exposure intensities based on the quartile of the intensity distribution.
The names of the disinfectants quantified in this report were as follows:
polyhexamethylene guanidine phosphate (PHMG, CAS #: 89697-78-9)
oligo(2-(2-ethoxy)ethoxyethyl guanidinium (PGH, CAS # 374572-91-5)
chloromethylisothiazolinone (CMIT, CAS # 26172-55-5)
methylisothiazolinone (MIT, CAS #: 2682-20-4)
For example, the exposure intensity for a family who reported using 10 mL of a humidifier disinfectant brand that had an estimated level of 1,276 μg/mL PHMG (Table 1) two times per day in a room of 27m3 and who ventilated the room less than one hour per day was calculated as follows:
PHMG amount dispersed into room air (μg)
= 10 mL/addition × 2 additions × 1,276 μg/mL = 25,520 μg
Airborne PHMG level estimated (mg/m3)
= 25,520 μg/27 m3 = 0.945 mg/m3 × 1 (ventilation factor) = 0.945 mg/m3
Exposure Duration
We calculated disinfectant exposure duration as the duration each subject was in a room when the humidifier containing disinfectants was simultaneously being used was assessed using individual-level information reported in the questionnaire. Cumulative disinfectant use hours were calculated by multiplying together the total years (Q2), months per year, weeks per month, days per week (Q3), and hours per day (Q4) during which disinfectant was actually used. Hours per day included hours sleeping in a room with a humidifier that contained disinfectants. Family members who indicated they did not use disinfectants in a humidifier in their bedroom may have had indirect exposure due to their presence in a room or common area where a humidifier containing disinfectants was operating. We accounted for this indirect exposure by considering the actual exposure time spent in any location with a humidifier.
Cumulative hours were classified into four categories according to the quartile distribution. For example, the disinfectant exposure duration for a family who used humidifier disinfectants for two years and six months, every day for eight months per year, with a mean of 11 disinfectant-exposed hours per day was calculated as follows:
Mean cumulative disinfectant hours
= 2.5 years × 8 months/year × 4 weeks/month × 7 days/week × 11 hours/day = 880 hours.
Cumulative exposure Level
The cumulative inhalation exposure levels of each study subject to disinfectants were calculated by multiplying together the quantitative estimates of disinfectant exposure intensity and duration. Cumulative exposure was then semi-quantitatively categorized into four groups based on the quartile distribution; low (< 25th), medium (25th-50th), high (51th-75th) and very high (>75th).
Data Analysis
Descriptive statistics of disinfectant use, intensity, duration, and cumulative exposure were examined separately for the patient group and family group. Each group was also stratified into four groups: six years old or younger, between six and 18 years of age, pregnant women, and 18 years of age or older (excluding pregnant women). These strata were identified for future epidemiological analyses to test whether the level of susceptibility or sensitivity to disinfectants may be substantially different among these groups (Lebowitz, 1995, Park et. al., 2014). In addition, the diverse types of disinfectants used were categorized into guanidine (PGH and PHMG) and non-guanidine group chemicals (CMIT and MIT) because the toxicity between the two types may be different. Because the exposure duration and intensity metrics were highly skewed, a quartile distribution was used to examine differences between the study groups. Analysis of variance (ANOVA) was used to compare the mean of the quartile categorical assignment for exposure intensity and exposure duration for the patient and family groups, and among age groups within each group. All statistical analyses were performed using STATA ver. 12 (StataCorp, College Station, Texas, USA).
Results
Demographic and Disinfectant Use Characteristics
The patient group was slightly more likely to be female (53.5%) than male (46.5%). The age of study subjects averaged 30 years old with an age range of 2 to 99 years. Pre-school children aged less than 8 years old accounted for 37% of lung disease patients group and 13% of the family group (Table 2). The age when the lung disease developed varied from 0 to 93 years old, but the cases were primarily represented by children three years of age or younger (36%) and adults 19 years and older (42%). Of the 250 families included in this study, the numbers of families with two, three and four lung disease patients were 59, 19 and 9, respectively. The most commonly used humidifier disinfectant was PHMG for both the lung disease group (76%) and the family group (83%). The majority of patients (66%) and family (60%) subjects used only one type of disinfectant.
Table 2.
General characteristics of study subjects
| Classification | Lung disease patient group | Non-patients within family | |||
|---|---|---|---|---|---|
|
|
|||||
| n | % | n | % | ||
| Gender | |||||
| Male | 174 | 46.5 | 153 | 50.5 | |
| Female | 200 | 53.5 | 150 | 49.5 | |
| Age at investigation | |||||
| <=3 | 30 | 8.0 | 4 | 1.3 | |
| 4-8 | 108 | 28.9 | 36 | 11.9 | |
| 9-18 | 41 | 11.0 | 16 | 5.3 | |
| 19-65 | 174 | 46.5 | 211 | 69.6 | |
| >65 | 21 | 5.6 | 7 | 2.3 | |
| No information | 29 | 9.6 | |||
| Age when self-reported lung disease developed | |||||
| <=3 | 135 | 36.1 | |||
| 4-8 | 36 | 9.6 | |||
| 9-18 | 6 | 1.6 | |||
| 19-65 | 158 | 42.2 | |||
| >65 | 24 | 6.4 | |||
| No information | 15 | 4.0 | |||
| Type of disinfectant | |||||
| PGH | 33 | 8.8 | 34 | 11.2 | |
| PHMG | 286 | 76.5 | 252 | 83.2 | |
| CMIT & MIT | 27 | 7.2 | |||
| SDT | 3 | 0.8 | 9 | 3.0 | |
| No information | 25 | 6.7 | 8 | 2.6 | |
| No. of different disinfectant brands used | |||||
| 1 | 230 | 65.7 | 179 | 59.5 | |
| 2 | 89 | 25.4 | 90 | 29.9 | |
| 3 | 30 | 8.6 | 25 | 8.3 | |
| No information | 1 | 0.3 | 7 | 2.3 | |
|
| |||||
| Total | 374 | 100 | 303 | 100 | |
PHMG = polyhexamethylene guanidine phosphate; PGH = oligo(2-(2-ethoxy)ethoxyethyl guanidinium; CMIT = chloromethylisothiazohnone; MET = methyhsothiazohnone; SDT= Sodium Dichloro-S-Triazmetrione(Cas No. 2893-78-9)
Exposure Probability
Supporting information on disinfectant use was most commonly provided using a purchase receipt for the disinfectant (overall: 40%) and showing the home visit investigator the residual disinfectant (overall: 40%), while only a small number of participants provided a photograph to verify the use of disinfectant (Table 3). All study subjects (n = 677) were consistent in their statements on the use of disinfectant based on the investigators’ review (Table 3). These patterns were similar in both the patient and family groups.
Table 3.
Evidence for the use of humidifier disinfectant
| Evidence | Lung disease patient |
Non-patient within family |
||
|---|---|---|---|---|
|
|
||||
| yes | no | yes | no | |
| Receipt for the purchase of humidifier disinfectant | 146 | 228 | 128 | 175 |
| Photographs indicating the use of humidifier disinfectant | 5 | 369 | 7 | 296 |
| Residual humidifier disinfectant | 157 | 217 | 117 | 186 |
| Consistent statements about the use of humidifier disinfectant | 374 | 303 | ||
Exposure Intensity
The mean and quartile distribution of estimated exposure intensity is shown in Table 4 for any disinfectant and in Table 5 by disinfectant type. Overall, the mean and quartile cut points of the disinfectant exposure intensities for pregnant women (mean = 1,010 μg/m3) and those six years old and younger (mean = 880 μg/m3) in the patient group were generally higher than those of their corresponding family group and for both the patient and family groups of the two other age groups (Table 4). For the 7-18 year old group and the >18 year old group (excluding pregnant women), the exposure intensity was similar in both the patient and family groups. These trends were also observed in the guanidine disinfectant group (includes PGH and PHMG), but not in the non-guanidine group (Table 5). Overall, exposure intensities for those using guanidine were far higher than those for the non-guanidine disinfectant group for all age groups (Table 5).
Table 4.
Estimated airborne disinfectant concentration
| Group | No | Mean(SD), μg/m3(× 103) |
Quartile distribution, μg/m3(× 103) |
|||
|---|---|---|---|---|---|---|
| 25th | 50th | 75th | ||||
| Pregnant women | ||||||
| Lung disease patients | 37 | 1.0(1.6) | 0.3 | 0.5 | 1.1 | |
| Non-patients | 9 | 0.4(0.3) | 0.1 | 0.3 | 0.5 | |
| <=6 years old | ||||||
| Lung disease patients | 156 | 0.9(1.6) | 0.3 | 0.6 | 1.1 | |
| Non-patients | 53 | 0.7(0.8) | 0.4 | 0.5 | 0.7 | |
| 7 through 18 years old | ||||||
| Lung disease patients | 11 | 0.8(1.4) | 0.1 | 0.5 | 0.7 | |
| Non-patients | 11 | 0.8(0.5) | 0.5 | 0.7 | 0.9 | |
| >18 years old | ||||||
| Lung disease patients | 141 | 0.1(0.8) | 0.3 | 0.5 | 0.9 | |
| Non-patients | 210 | 0.7(0.8) | 0.3 | 0.5 | 0.9 | |
|
| ||||||
| Totala | ||||||
| Lung disease patients | 345(29) | 0.8(1.3) | 0.3 | 0.5 | 1.0 | |
| Non-patients | 283(20) | 0.7(0.7) | 0.3 | 0.5 | 0.8 | |
include the number with no information on the type of disinfectant (21 for patient and 2 for non-patient group)
Table 5.
Estimated airborne disinfectant concentration(μg/m3) by the type of disinfectant
| Group | No | Mean(SD) , μg/m3 (× 103) |
Guanidine quartile distribution, μg /m3(× 103) |
No | Mean(SD), , μg/m1 |
Non-guanidine quartile distribution, μg/m3 |
|||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 25th | 50th | 75th | 25th | 50th | 75th | ||||||
| Pregnant women | |||||||||||
| Lung disease patients | 37 | 1.0(1.6) | 0.3 | 0.5 | 1.1 | ||||||
| Non-patients | 8 | 0.4(0.3) | 0.2 | 0.4 | 0.7 | 1 | 75 | 75 | 75 | 75 | |
| <= 6 years old | |||||||||||
| Lung disease patients | 146 | 0.9(1.7) | 0.4 | 0.6 | 1.1 | 10 | 84(43) | 59 | 79 | 130 | |
| Non-patients | 51 | 0.8(0.8) | 0.4 | 0.5 | 0.7 | 2 | 53(31) | 31 | 53 | 75 | |
| 7 through 18 years old | |||||||||||
| Lung disease patients | 7 | 1.3(1.7) | 0.5 | 0.6 | 1.2 | 4 | 64(74) | 59 | 62 | 70 | |
| Non-patients | 11 | 0.8(0.5) | 0.5 | 0.7 | 0.9 | ||||||
| >18 years old | |||||||||||
| Lung disease patients | 120 | 0.8(0.8) | 0.3 | 0.6 | 1.0 | 21 | 85(77) | 32 | 63 | 100 | |
| Non-patients | 188 | 0.8(0.8) | 0.4 | 0.5 | 1.1 | 22 | 88(67) | 48 | 75 | 95 | |
|
| |||||||||||
| Totala | |||||||||||
| Lung disease patients | 310 | 0.9(1.4) | 0.3 | 0.6 | 1.0 | 35 | 82(64) | 36 | 63 | 100 | |
| Non-patients | 258 | 0.8(0.7) | 0.4 | 0.5 | 0.9 | 25 | 85(64) | 48 | 74 | 88 | |
include the number with no information on the type of disinfectant (29 for patient and 20 for non-patient group)
Exposure Duration
The mean and quartile distribution of cumulative disinfectant exposure hours is reported in Table 6. The patient group reported significantly higher disinfectant exposure duration than those in the family group for all age groups (ANOVA, p=0.047). Cumulative disinfectant use hours among the patients were significantly different by age group (p=0.0092). Average cumulative disinfectant exposure hours for pregnant women (4,400 hours) and the young-age group ≤ 6 years old (4,800 hours) in the patient group were significantly lower than those of the other age groups (p=0.0076).
Table 6.
Cumulative exposure duration (hrsa) of disinfectant
| Group | No | Mean(SD), hrs (× 103) |
Quartile distribution, hrs (× 103) |
|||
|---|---|---|---|---|---|---|
| 25th | 50th | 75th | ||||
| Pregnant women | ||||||
| Lung disease patients | 38 | 4.4(5.2) | 1.5 | 2.7 | 5.0 | |
| Non-patients | 9 | 4.0(4.0) | 1.2 | 2.0 | 4.8 | |
| <= 6 years old | ||||||
| Lung disease patients | 157 | 4.8(6.3) | 1.3 | 2.2 | 5.5 | |
| Non-patients | 56 | 4.3(6.0) | 1.0 | 2.5 | 5.0 | |
| 7 through 18 years old | ||||||
| Lung disease patients | 11 | 10.5(13.4) | 1.4 | 4.4 | 19.4 | |
| Non-patients | 12 | 7.0(7.3) | 1.3 | 4.2 | 10.5 | |
| >18 years old | ||||||
| Lung disease patients | 147 | 7.0(8.8) | 1.5 | 4.2 | 9.1 | |
| Non-patients | 224 | 4.1(5.0) | 1.2 | 2.2 | 4.8 | |
| Totalb | ||||||
| Lung disease patients | 353(21) | 5.9(7.7) | 1.5 | 2.9 | 7.6 | |
| Non-patients | 301(2) | 4.2(5.3) | 1.2 | 2.2 | 4.9 | |
years × months/year × weeks /month × days /weeks × hours / day
include the number with no information on the type of disinfectant (21 for patient and 2 for non-patient group)
Cumulative Exposure Level
The proportions of participants in each disinfectant cumulative exposure quartile is reported by age groups for the patient and family groups in Table 7. The overall distribution of exposure categories by patient and family group were similar, with slightly more lung disease patients classified as “very high” exposure (28%) than the family group (21%). Pregnant women and ≤ 6 years old group in the patient group had higher proportions allocated to the “high” and “very high” exposure category, compared to the family group (Table 7). The proportions by exposure category were similar for the patient and family groups for those 7 to 18 years old. In contrast, adults in the family group were more frequently classified in the “very high” group (16%) than those in the patient group (12%). Similar trends were observed in comparisons by type of humidifier disinfectant (Table 8).
Table 7.
Percent of study subjects according to qualitative exposure levela
| Group | No | Qualitative exposure level |
||||
|---|---|---|---|---|---|---|
| Low | Medium | High | Very high | |||
| Pregnant women | ||||||
| Lung disease patients | 37 | 7(2.0 %) | 12(3.2 %) | 9(2.6 %) | 9(2.6 %) | |
| Non-patients | 9 | 3(1.1%) | 3(1.1%) | 2(0.7 %) | 1(0.4 %) | |
| ≤ 6 years old | ||||||
| Lung disease patients | 154 | 35(10.2 %) | 45(13.1%) | 33(9.6 %) | 41(12.0%) | |
| Non-patients | 53 | 12(4.3 %) | 15(5.3 %) | 18(6.4 %) | 8(2.9 %) | |
| 7 through 18 years old | ||||||
| Lung disease patients | 11 | 3(0.9 %) | 2(0.6 %) | 2(0.6 %) | 4(1.2%) | |
| Non-patients | 11 | 2(0.7 %) | 3(1.1%) | 0 | 6(2.1%) | |
| >18 years old | ||||||
| Lung disease patients | 141 | 35(10.2 %) | 27(7.9 %) | 37(10.8 %) | 42(12.2 %) | |
| Non-patients | 208 | 59(21.0%) | 49(17.4 %) | 55(19.6 %) | 45(16.0 %) | |
|
| ||||||
| Totalb | ||||||
| Lung disease patients | 343(32) | 80(23.3 %) | 86(25.1%) | 81(23.6%) | 96(28.0 %) | |
| Non-patients | 281(22) | 76(27.1%) | 70(24.9 %) | 75(26.7 %) | 60(21.4%) | |
classified by quartile distribution of multiplication of exposure duration and exposure intensity(low<25th, moderate=25-50th, high=5 lth-75th, very high>75th)
include the number with no information on the type of disinfectant (32 for patient and 22 for non-patient group)
Table 8.
Percent of study subjects according to qualitative exposure levela and disinfectant type
| Group | No | Guanidine qualitative exposure level |
Non-guanidine qualitative exposure level |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Low | Medium | High | Very high | Low | Medium | High | Very high | |||
| Pregnant women | ||||||||||
| Lung disease patients | 37 | 7(2.0 %) | 12(3.5 %) | 9(2.6 %) | 9(2.6 %) | |||||
| Non-patients | 9 | 3(1.1%) | 2(0.7 %) | 2(0.7 %) | 1(0.4 %) | 0 | 1(0.4 %) | |||
| ≤ 6 years old | ||||||||||
| Lung disease patients | 154 | 29(8.5 %) | 41(12.0%) | 33(9.6 %) | 41(12.0%) | 6(1.7%) | 4(1.2%) | 0 | 0 | |
| Non-patients | 53 | 10(3.4%) | 15(5.3 %) | 18(6.4 %) | 8(2.8 %) | 2(0.7 %) | 0 | |||
| 7 through 18 years old | ||||||||||
| Lung disease patients | 11 | 1(0.3 %) | 1(0.3 %) | 1(0.3 %) | 4(1.2%) | 2(0.6 %) | 1(0.3 %) | 1(0.3 %) | 0 | |
| Non-patients | 11 | 2(0.7 %) | 3(1.1%) | 0 | 6(2.1%) | |||||
| >18 years old | ||||||||||
| Lung disease patients | 141 | 22(6.4 %) | 25(7.3 %) | 32(9.3 %) | 41(12.0%) | 13(3.8 %) | 2(0.6 %) | 5(1.5 %) | 1(0.3 %) | |
| Non-patients | 208 | 41(14.6 %) | 45(16.0 %) | 55(19.6 %) | 45(16.0 %) | 18(6.4 %) | 4(1.4%) | |||
|
| ||||||||||
| Totalb | ||||||||||
| Lung disease patients | 343(32) | 59(17.2 %) | 79(23.0%) | 75(21.9%) | 95(27.7 %) | 21(6.1 %) | 7(2.0 %) | 6(1.7%) | 1(0.3 %) | |
| Non-patients | 281(22) | 56(19.9 %) | 65(23.1%) | 75(26.7 %) | 60(7.1 %) | 20(7.1 %) | 5(1.8%) | |||
classified by quartile distribution of multiplication of exposure duration and exposure intensity(low<25th, moderate=25-50th, high=51th-75th, very high>75th)
include the number with no information on the type of disinfectant (32 for patient and 22 for non-patient group)
Discussion
We developed a systematic and transparent approach for estimating the potential exposure levels of disinfectants that had been added to household humidifiers. We directly linked responses of study subjects to questions related to disinfectant use characteristics and our field investigation results to estimate exposure probability, intensity and duration to humidifier disinfectants. Overall, our lung disease patients showed significant variability in age, sex, humidifier disinfectant use practices, and duration of exposure to humidifier disinfectants (Table 1). The patient group’s disinfectant use practices, especially for pregnant women and children six years old and younger, generally resulted in higher prevalence, duration, and intensity of exposure compared to participants recruited from family group members. Additionally, those using disinfectants from the guanidine chemical group tended to have much higher exposure estimates than those using disinfectants from the non-guanidine group. These estimates are a necessary first step to elucidating the relationship between humidifier disinfectant exposures and lung disease. In addition, our approach provides a transparent framework that could be adapted to assess exposure for other household agents.
A unique aspect of our study was our use of both material evidence, such as receipts for the purchase of disinfectant, the residual disinfectant, or a photograph from the past showing the use of disinfectant, along with evaluating the consistency in responses to disinfectant-related questions to identify disinfectant-exposed subjects, rather than relying solely on self-reported information. The most common evidence that the participants provided were purchase receipts and containers of the residual disinfectant, both of which was assumed to verify the use of disinfectants (Table 3). Another unique aspect was our development of semi-quantitative exposure estimates of disinfectant exposure. Few other studies have estimated quantitative exposure intensity of household chemicals because of the general lack of information on chemical formulations due to proprietary information (King et. al., 2004, Shin et. al. , 2011).
Estimates of the intensity and duration of exposure incorporated individual-level data on type and frequency of disinfectant use. Although exposure to humidifier disinfectants can occur through multiple pathways and routes, which can be highly variable depending on use patterns (Leung and Paustenbach, 1994), our exposure intensity estimates assumed that the inhalation route predominates because the disinfectant dissolved in humidifier water is dispersed into the air by the humidifier’s aerosolizer. The ultrasonic humidifiers used by most patients readily disperse aerosol water droplets ranging in size from 0.5 to 3 μm, which easily reach the distal airways (Shiue et. al. , 1990, Suda et. al. , 1995). This fine mist is inhaled by individuals near the humidifier. We were currently unable to quantify airborne disinfectant concentrations because its household use in humidifiers has been banned in Korea since 2011 and because no historical measurements were available. Mester et al. (2011) previously used information from company data on chemical formulations to estimate exposure intensity with respect to the agent’s concentration and the intermolecular bond in the formulation. Here, we also used the quantified concentration (μg/mL) in bulk disinfectant products to estimate airborne disinfectant intensity. The exposure levels of PGH and PHMG in the guanidine disinfectant group among bulk humidifier disinfectant brands were estimated to be far higher than those of CMIT and MIT (Table 5), all of which vary substantially in terms of disinfectant level among humidifier disinfectant brands. Our estimates assumed that these bulk levels were constant over time. However, due to the fierce competition among the more than ten humidifier disinfectant manufacturers in South Korea, the amount of disinfectant added to humidifiers may have risen steadily over time to advertise improved microbial contamination prevention. Our estimated disinfectant intensities assumed that the full amount of disinfectant added to the humidifier was dispersed into air, and that the disinfectant concentration in the room volume did not vary over time and was spatially uniform. Kim et. al. (2013) observed granulomatous obliterative bronchiolitis (OB), bronchitis, collagenized fibrosis, alveolar bronchiolarization, and extensive squamous metaplasia in rats exposed to humidifier products with PHMG and PGH at concentrations of 0.4 mg/m3 and 1.75 mg/m3 for ten and seven weeks, respectively, which are in the range of our airborne PHMG and PGH estimates (Table 4). This assumption may represent a worst-case scenario; however, we expect that the true concentrations would be correlated with the exposure estimates and thus appropriate for deriving semi-quantitative cumulative exposure groups.
Our estimates of the frequency of disinfectant exposure had several assumptions. Our aim was to estimate duration based on the duration that humidifier disinfectants were actually used while the subject was in the same room. However, humidifiers were irregularly used and the subjects spent varying times in the rooms containing humidifiers. Based on individual-level typical disinfectant use practices, humidifier disinfectant use duration was found to vary among family members, ranging from < 1month to 12 months per year (mean ± SD = 6.9±2.7 months) and from < 1 hr to 24 hrs per day (mean ± SD= 13.8±5.7hrs). We found that pregnant women and pre-school-age children showed far lower cumulative disinfectant exposure duration than other age groups (Table 6), which may indicate that humidifier disinfectant use may have been used intensively only during a specific period of child development, such as in the pre-gestation, gestational, and post-natal periods. Overall, the lung disease patient group showed longer disinfectant use duration, airborne intensity and level than the family group, although statistical significant differences were not found.
Lastly, because of the assumptions inherent in the exposure intensity and frequency estimates, we semi-quantitatively categorized cumulative humidifier disinfectant exposure levels to identify broad exposure groups rather than relying on the specific point estimates. However, the point estimates are useful to identify relative magnitude differences between groups that are usually unavailable in studies that use ordinal scores that do not have a quantitative characterization of category cut points (Stewart and Stewart, 1994). Although our assessment approach resulted in semi-quantitative estimates, it provided more refined exposure estimates than previous studies that have previously evaluated exposure to household chemicals using dichotomous, categorical, or ordinal exposure variables reflecting “ever/never use” (Zota et. al. , 2010, Rudant et. al. , 2007), “the number of times”, “frequency used” (Alderton et. al. , 2006), “duration of use”, and “presence/absence of contaminant source or contamination” (Cordioli et. al. , 2013) as surrogates for cumulative household chemical exposure.
The next step is to incorporate our exposure assessment into epidemiologic analyses to examine the associations between disinfectant use with clinically diagnosed lung disease cases. The various humidifier disinfectant exposure indices (i.e., the volume of the room with the humidifier, the volume and the frequency of disinfectant added to the humidifier, the type of disinfectant, the duration of humidifier disinfectant use, and the amount or frequency of ventilation) estimated in this study can be used either singly or in combination in future epidemiologic analyses of this population to assess factors related to acute and chronic respiratory symptoms.
The major limitation in our approach is that it relies predominantly on subject recall, since most of the important variables related to disinfectant use characteristics, including ever use, duration and intensity, were predominantly obtained from direct reports from study subjects and are heavily dependent on their memories. For subjects who used several types of disinfectants over different periods, it can be challenging to recall the duration and amount of disinfectant used for each disinfectant. We aimed to improve the accuracy of the participants’ recall by showing photographs of each disinfectant brand and asking additional questions that may be specific to respective disinfectant types. While recall bias may explain some differences between patient and family groups, we minimized the potential bias by recruiting non-patients from family group members, whom we expected to have similar concerns related to disinfectant use as in the patient group (and thus similar recall) than participants selected from the general population. Another limitation is that our intensity estimates relied on a simple model for disinfectant distribution within the room, whereas factors affecting inhalation exposure concentrations includes the proximity of the study subject to the humidifier, the dispersion rate, the type of humidifier, the rate of air exchange, and variations in the amount of disinfectants (and their respective active ingredients) added to the humidifier over time, which were not fully assessed in this study. Our approach does not consider spatial differences in exposure that could occur for individuals who may frequently move throughout the humidified room and other rooms in the house. In particular, we were unable to combine several different disinfectant types that study subjects used over time. Airborne intensity estimated here was based on one major disinfectant type subjects used mostly (patient group; 82 %, non-patient group; 80 %). The fraction of subjects who would use more than two brands over time was 38 % for non-patient group and 32 % patient group, respectively. Further study is underway to examine if number of disinfectant used is associated with the risk of lung disease.
Conclusions
The approach described here is the first attempt to retrospectively assess semi-quantitative levels of household humidifier disinfectant exposure for use in an epidemiological study. The resulting exposure estimates identified important differences in all exposure indices (i.e. intensity, duration and cumulative exposure to humidifier disinfectant) between patient and family groups, between pregnant women and pre-school children groups compared to other age groups, and between participants who used guanidine disinfectants and non-guanidine disinfectants.
Practical implications.
Retrospective exposure to household humidifier disinfectant as estimated here can be used to evaluate associations with clinically diagnosed lung disease due to the use of humidifier disinfectant in Korea. The framework, with modifications to account for dispersion and use patterns, can also be potentially adapted to assessment of other household chemical exposures.
Acknowledgements
This work was supported by the research funded by Korea Center for Disease Control and Prevention (KCDC) (4851-300-210-13). In particular, the authors would like to thank all of the study subjects who were willing to participate in this study for their cooperation. MCF is supported by the Intramural Research Program of the Division of Cancer Epidemiology and Genetics, within the National Cancer Institute of the National Institutes of Health.
REFERENCES
- Alderton LE, Spector LG, Blair CK, Roesler M, Olshan AF, Robison LL, Ross JA. Child and maternal household chemical exposure and the risk of acute leukemia in children with Down's syndrome: a report from the Children's Oncology Group. Am. J. Epidemiol. 2006;164:212–221. doi: 10.1093/aje/kwj203. [DOI] [PubMed] [Google Scholar]
- Chang MH, Park HS, Ha MN, Kim YH, Hong YC, Ha EH. Characteristics of humidifier use in Korean pregnant women: the Mothers and Children's Environmental Health (MOCEH) study. Environ. Health Toxicol. 2012;27 doi: 10.5620/eht.2012.27.e2012003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cordioli M, Ranzi A, De Leo GA, Lauriola P. A review of exposure assessment methods in epidemiological studies on incinerators. J. Environ. Public Health. 2013;2013 doi: 10.1155/2013/129470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong SB, Kim HJ, Huh JW, Do KH, Jang SJ, Song JS, Choi SJ, Heo YJ, Kim YB, Lim CM. A cluster of lung injury associated with home humidifier use: clinical, radiological and pathological description of a new syndrome. Thorax. 2014 doi: 10.1136/thoraxjnl-2013-204135. thoraxjnl-2013-204135. [DOI] [PubMed] [Google Scholar]
- Jeon BH, Park YJ. Frequency of humidifier and humidifier disinfectant usage in Gyeonggi Provine. Environ. Health Toxicol. 2012;27 doi: 10.5620/eht.2012.27.e2012002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KCDC . Analytical results of the chemical components of various humidifier disinfectant brands from KCDC's parliamentary inspection (In Korean) Korea Center for Disease Control and Prevention; 2011a. Vol. Department of Epidemiology Research; Document # 1186. [Google Scholar]
- KCDC . Hospital based case-control study on lung injury with unknown causes. Korea Center for Disease Control and Preventation; 2011b. pp. 825–828. Public health Weekly Report (in Korean) [Google Scholar]
- KCDC . Interim report of epidemiologic investigation of lung injury with unknown causes in Korea (in Korean) Korea Center for Disease Control and Preventation; 2011c. pp. 825–828. [Google Scholar]
- Kim EH, Ahn KM, Cheong HK. Use of humidifiers with children suffering from atopic dermatitis. Environ. Health Toxicol. 2012;27:e2012004. doi: 10.5620/eht.2012.27.e2012004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim YB, Choi SJ, Yang YS, Kim YH, Song CW, Cho JW, Ha CS, Lee KH. Comparative Pulmonary Response to Aerosolized Humidifier Disinfectants by Intratracheal Instillation and Inhalation Exposure. 2013 Annual Meeting; 2013. Poster #207. [Google Scholar]
- King WD, Dodds L, Armson BA, Allen AC, Fell DB, Nimrod C. Exposure assessment in epidemiologic studies of adverse pregnancy outcomes and disinfection byproducts. Journal of Exposure Science and Environmental Epidemiology. 2004;14:466–472. doi: 10.1038/sj.jea.7500345. [DOI] [PubMed] [Google Scholar]
- KSEH . Cases of health problems due to the use of humidifier biocide (in Korean) Korean Society of Environmental Health; 2012. [Google Scholar]
- Lebowitz MD. Exposure assessment needs in studies of acute health effects. Sci. Total Environ. 1995;168:109–117. doi: 10.1016/0048-9697(95)04614-7. [DOI] [PubMed] [Google Scholar]
- Lee E, Seo JH, Kim HY, Yu JH, Jhang WK, Park SJ, Kwon JW, Kim BJ, Do KH, Cho YA. Toxic inhalational injury-associated interstitial lung disease in children. J. Korean Med. Sci. 2013;28:915–923. doi: 10.3346/jkms.2013.28.6.915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung HW, Paustenbach DJ. Techniques for estimating the percutaneous absorption of chemicals due to occupational and environmental exposure. Appl. Occup. Environ. Hyg. 1994;9:187–197. [Google Scholar]
- Park DU, Leem JH, Lee KM, Lim HK, Choi YY, Ahn JJ, Lim SY, Park JI, Choi KH, Lee NR, Jung HJ, Ha JS, Paek DM. Exposure characteristics of familial cases of lung injury associated with the use of humidifier disinfectants. Environmental Health. 2014;13:70. doi: 10.1186/1476-069X-13-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudant J, Menegaux F, Leverger G, Baruchel A, Nelken B, Bertrand Y, Patte C, Pacquement H, Vérité C, Robert A. Household exposure to pesticides and risk of childhood hematopoietic malignancies: The ESCALE study (SFCE) Environ. Health Perspect. 2007:1787–1793. doi: 10.1289/ehp.10596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin HM, Vieira VM, Barry Ryan P, Steenland K, Bartell SM. Retrospective exposure estimation and predicted versus observed serum perfluorooctanoic acid concentrations for participants in the C8 Health Project. Environ. Health Perspect. 2011;119:1760. doi: 10.1289/ehp.1103729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiue S, Scherzer H, Degraff A, Jr, Cole S. Hypersensitivity pneumonitis associated with the use of ultrasonic humidifiers. N. Y. State J. Med. 1990;90:263–265. [PubMed] [Google Scholar]
- Stewart PA, Stewart WF. Occupational case-control studies: II. Recommendations for exposure assessment. Am. J. Ind. Med. 1994;26:313–326. doi: 10.1002/ajim.4700260305. [DOI] [PubMed] [Google Scholar]
- Suda T, Sato A, Ida M, Gemma H, Hayakawa H, Chida K. Hypersensitivity pneumonitis associated with home ultrasonic humidifiers. CHEST Journal. 1995;107:711–717. doi: 10.1378/chest.107.3.711. [DOI] [PubMed] [Google Scholar]
- Yang HJ, Kim HJ, Yu JH, Lee E, Jung YH, Kim HY, Seo JH, Kwon GY, Park JH, Gwack J. Inhalation toxicity of humidifier disinfectants as a risk factor of children’s interstitial lung disease in Korea: a case-control study. PLoS One. 2013;8:e64430. doi: 10.1371/journal.pone.0064430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zota AR, Aschengrau A, Rudel RA, Brody JG. Self-reported chemicals exposure, beliefs about disease causation, and risk of breast cancer in the Cape Cod Breast Cancer and Environment Study: a case-control study. Environmental Health. 2010;9:40. doi: 10.1186/1476-069X-9-40. [DOI] [PMC free article] [PubMed] [Google Scholar]