Abstract
Purpose:
To examine the impact of lower urinary tract symptoms (LUTS) on health-related quality of life (HRQoL) in Korean men aged ≥40 years.
Methods:
A population-based, cross-sectional door-to-door survey was conducted among men aged ≥40 years. Individuals with LUTS were defined as men reporting at least one LUTS using 2002 International Continence Society definitions. Structuredquestionnaires were used to assess several dimensions of HRQoL, including generic health status (EuroQoL-five-dimensions questionnaire), work productivity (work productivity and activity impairment questionnaire), depressive symptoms (center for epidemiologic studies depression scale), and sexual health (sexual satisfaction and erectile dysfunction). The impact of LUTS was assessed by comparing several dimensions of HRQoL among men with and without LUTS.
Results:
Of the 1,842 participants, 1,536 (83.4%) reported having at least one LUTS. The prevalence of LUTS increased with age (78.3% among those aged 40–49 years to 89.6% among those aged 60 years or older). Those with LUTS reported a significantlylower level of generic health status and worse work productivity compared with those without LUTS. Significantly more individuals with LUTS reported having a higher level of major depressive symptoms compared with those without LUTS.Those with LUTS reported worse sexual activity and enjoyment, and were significantly more likely to have erectile dysfunction than those without LUTS.
Conclusions:
LUTS seem to have a substantial impact on several dimensions of HRQoL in Korean men aged ≥40 years.
Keywords: Lower Urinary Tract Symptoms, Quality of Life, Epidemiologic Studies
INTRODUCTION
Lower urinary tract symptoms (LUTS) include a spectrum of storage, voiding, and postmicturition symptoms [1]. These conditions negatively affect many aspects of health-related quality of life (HRQoL), including social and emotional well-being, work productivity, and sexual health [2,3]. LUTS could be a sign of underlying medical pathophysiology, including cardiovascular disease and sleep apnea [4,5]. In fact, the impact of severe LUTS on many dimensions of HRQoL may be similar to that of chronic conditions such as hypertension, diabetes, angina, and gout [6]. LUTS in men might be suggestive of overactive bladder (OAB) and/or bladder outlet obstruction associated with benign prostatic hyperplasia [7] and are believed to be common. Previous reports have estimated the overall prevalence of any LUTS to be 63%–83% in adult men [8,9]. Because LUTS are highly prevalent in men and increase with age, the population burden of these conditions is likely to increase in the near future as demographics shift. Understanding the burden of LUTS is important for improved clinical practice and public health [10].
To date, although epidemiologic studies of LUTS have been performed in many countries [2,3,9,11-13], there is a lack of epidemiologic data in Korean men. To gain more comprehensive and representative information on the prevalence and impact of LUTS in Korea, we conducted a population-based epidemiologic survey. The objective of the present study was to assess the impact of LUTS on HRQoL in men aged ≥40 years in Korea.
MATERIALS AND METHODS
A population-based, cross-sectional door-to-door survey of men aged ≥40 years was carried out in Korea to evaluate the prevalence of LUTS as well as to examine the impact of LUTS on various dimensions of HRQoL, including generic health status, work productivity, depressive symptoms, and sexual health. Only the results of the impact of LUTS are reported in the present study; the results of the prevalence of LUTS have been previously published [8].
More than 1,800 men aged ≥40 years from five Korean provinces (Seoul, Busan, Daegu, Daejeon, and Gwangju) were targeted for recruitment. A random sample was obtained through the Post and Address Registry of Korea using a two-stage sampling method based on geographical variables. Those who reported currently having a urinary tract infection were excluded from this survey. After obtaining informed consent, interviews were conducted by direct interviews, usually in the respondent’s home. To conduct the survey, the interviewer training in general lasted approximately two days before interviewers were authorized to start interviewing study participants. They were regularly tested to maintain consistency and quality control in the use of the questionnaires. This study was approved by our Institutional Review Board of the Samsung Medical Center (IRB No. 2010-02-026).
The questionnaire was divided into two parts: an initial questionnaire about demographics and presence of LUTS that was originally developed for a previous EPIC study [9], and it was translated into an appropriate Korean version [14]. Based on an initial questionnaire, individuals with LUTS were defined as men reporting at least one LUTS using 2002 International Continence Society definitions. An additional questionnaire consisted of questions about detailed demographics and comorbidity, generic QoL (EuroQoL-five-dimensions [EQ-5D] questionnaire), work productivity (work productivity and activity impairment [WPAI] questionnaire), depressive symptoms (center for epidemiologic studies depression scale, CES-D), and sexual satisfaction and erectile dysfunction (ED).
Generic QoL
The EQ-5D questionnaire is a well-validated comprehensive tool designed to measure generic HRQoL [15]. The EQ-5D questionnaire has two components: the EQ-5D index and EQ-visual analogue scale (VAS). The EQ-5D index comprised a questionnaire with five dimensions: mobility, self-care, usual activities, pain or discomfort, and anxiety or depression. For each of the dimensions, the responder can choose from three different options; no problem, some/moderate problem, or extreme problem. A unique EQ-5D health state is defined by combining one level from each of the five dimensions with Korean weight-based scores ranging from 0.229 to 1.000, with higher scores indicating better overall health status [16]. The EQ-VAS produces patients’ self-perceived estimate of their HRQoL on a 100-point scale (0=worst imaginable health state to 100=best imaginable health state).
Work Productivity
Participants were asked about their employment status and work productivity. The WPAI questionnaire was used to assess the impact of health on work productivity loss and impairment in daily activities [17]. The WPAI questionnaire records impairment due to health problems during the past seven days and has six items grouped into four domains. Outcomes for each domain are expressed as impairment percentages, with higher scores indicating a greater proportion of impairment in work (less productivity) or activities. The four WPAI domains are described as follows: absenteeism (the percentage of work time missed due to one’s health problems), presenteeism (the percentage of impairment experienced while at work due to one’s health problems), overall work productivity loss (an overall impairment estimate that is a combination of absenteeism and presenteeism), and activity impairment (the percentage of impairment in daily activities due to one’s health problems). Only respondents who reported being employed full-time or part-time provided data for work productivity, but all respondents provided data for activity impairment. Individuals with LUTS were also asked work productivity questions in relation to their urinary symptoms.
Depressive Symptoms
Depressive symptoms were evaluated with the CES-D [18]. The CES-D is a commonly used screening tool that assesses the presence and severity of symptoms of depression in the general population. It contains 20 items addressing depressive symptoms, and respondents indicate on a 4-point Likert scale how frequently they have experienced each symptom in the last week. Responses to items of the CES-D scale are summed up, and higher scores indicate higher levels of depressive symptoms (0=not at all depressed to 60=very depressed). In the present study, the cutoff for the selection of men with symptoms of depression was determined to be 21 points [19].
Sexuality QoL
Participants were asked if they were currently sexually active. The impact of urinary symptoms on the frequency of sexual activity and on sexual enjoyment was evaluated with general questions about sexual health. Respondents were asked to rate the degree to which their urinary symptoms caused them to decrease or stop sexual activity. Those respondents who reported being sexually active were asked to rate the degree to which their urinary symptoms caused a reduction in enjoyment of sexual activity. Respondents chose from four different options for these questions: not at all, somewhat, quite a bit, and a great deal. Respondents who selected quite a bit and a great deal were considered to be negatively impacted by urinary symptoms. Respondents who reported being sexually active were also asked to rate the degree to which they were satisfied with their overall sexual life on a scale from 1 (very dissatisfied) to 5 (very satisfied). Reponses of 4 or 5 on this scale were considered indicative of satisfaction with sexual activity. The presence of ED was assessed by the validated, single-question, self-report item from the Massachusetts Male Aging Study with the following response choices: none, minimal, moderate, and complete [20].
Statistical Analysis
The impact of LUTS was assessed by comparing generic health status (EQ-5D questionnaire), work productivity (WPAI questionnaire), depressive symptoms (CES-D), and sexual health (sexual satisfaction and ED) among men with LUTS and without LUTS. Results are also reported by age groups (40–49 years, 50–59 years, and ≥60 years). Continuous variables were compared using Student t-test or the Mann-Whitney U-test, while categorical variables were compared using the chi-square test or Fisher exact test. Reliability of the questionnaire was estimated by internal consistency using Cronbach alpha coefficient. A P-value of <0.05 was considered statistically significant. We performed all statistical analyses using the statistical software package R ver. 2.11.1 (R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
Of a total of 6,873 men who were contacted to participate in the study, 1,842 agreed, yielding a response rate of 26.8%, and their responses were analyzed. In our study population, 1,536 men (83.4%) who reported experiencing at least one LUTS were classified as those with LUTS. The mean age was 53.0±9.1 and 49.9±7.9 years in those with LUTS and without LUTS, respectively (P<0.001). The prevalence of LUTS increased with age (Fig. 1). The demographic and clinical characteristics of the participants are presented in Table 1.
Fig. 1.
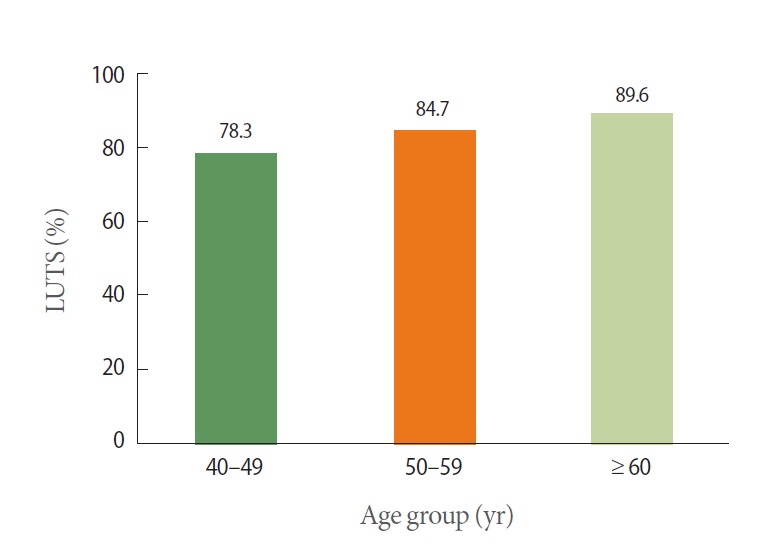
The percentage of respondents with lower urinary tract symptoms (LUTS) by age groups.
Table 1.
Demographic data and medical comorbidities of the participants
| Characteristic | Total participants (n=1,842) | Individuals with LUTS (n=1,536) | Individuals without LUTS (n=306) | P-valuea) |
|---|---|---|---|---|
| Age group (yr) | <0.001 | |||
| 40–49 | 751 (40.8) | 588 (38.3) | 163 (53.3) | |
| 50–59 | 609 (33.1) | 516 (33.6) | 93 (30.4) | |
| ≥60 | 482 (26.2) | 432 (28.1) | 50 (16.3) | |
| Educational level | 0.973 | |||
| High school graduate or less | 408 (22.1) | 340 (22.1) | 68 (22.2) | |
| College or more | 1,434 (77.9) | 1,196 (77.9) | 238 (77.8) | |
| Marital status | 0.602 | |||
| Married or live with partner | 1,670 (90.7) | 1,395 (90.8) | 275 (89.9) | |
| Single or live without partner | 172 (9.3) | 141 (9.2) | 31 (10.1) | |
| Comorbidities | ||||
| Asthma | 88 (4.8) | 84 (5.5) | 4 (1.3) | 0.002 |
| Chronic cough | 146 (7.9) | 136 (8.9) | 10 (3.3) | 0.001 |
| Diabetes | 221 (12.0) | 203 (13.2) | 18 (5.9) | < 0.001 |
| High blood pressure | 542 (29.4) | 475 (30.9) | 67 (21.9) | 0.002 |
| Neurologic disease | 27 (1.5) | 24 (1.6) | 3 (1.0) | 0.605 |
| Depression | 119 (6.5) | 112 (7.3) | 7 (2.3) | 0.001 |
| Chronic constipation | 114 (6.2) | 104 (6.8) | 10 (3.3) | 0.020 |
Values are presented as number (%).
LUTS, lower urinary tract symptoms.
Comparisons among individuals with LUTS and without LUTS
Impact of LUTS
Regarding generic HRQoL assessed by the EQ-5D, those with LUTS had significantly lower mean EQ-5D index and VAS scores compared with those without LUTS (Table 2, both P<0.001). These results were consistent by age groups, except for the EQ-5D VAS score in men aged ≥60 years (Tables 3-5). Cronbach alpha coefficient for the five items in the EQ-5D index was 0.619, which indicated acceptable internal consistency. In all five dimensions of the EQ-5D questionnaire, the percentages of respondents who reported either some/moderate or extreme problems were significantly different among those with LUTS and without LUTS (Fig. 2, all P<0.001). In particular, 25.9% (398/1,536) and 25.8% (396/1,536) of individuals with LUTS reported some/moderate or extreme problems in “pain or discomfort” and “anxiety or depression,” respectively.
Table 2.
Participant-reported outcomes by all age (aged ≥40 years)
| Variable | Individuals with LUTS | Individuals without LUTS | P-value |
|---|---|---|---|
| EQ-5D index score (n=1,842) | 0.89±0.16 | 0.95±0.10 | <0.001 |
| EQ-VAS score (n=1,842) | 74.9±18.8 | 78.0±21.9 | <0.001 |
| Employment status (n=1,842) | |||
| Full time | 924 (60.2) | 224 (73.2) | <0.001 |
| Part time | 196 (12.8) | 29 (9.5) | |
| Not employed | 416 (27.1) | 53 (17.3) | |
| WPAI (%) | |||
| Work time missed due to health (n=995) | 1.4±5.3 | 0.6±4.2 | 0.004 |
| Impairment while working due to health (n=1,231) | 14.5±26.6 | 9.3±23.7 | <0.001 |
| Overall work impairment due to health (n=972) | 14.1±26.0 | 8.3±22.5 | <0.001 |
| Activity impairment due to health (n=1,667) | 15.9±25.4 | 9.5±22.7 | <0.001 |
| Any work impairment (n=1,036) | 326 (39.2) | 50 (24.5) | <0.001 |
| CES-D scale ≥21 (n=1,842) | 177 (11.5) | 9 (2.9) | <0.001 |
| Currently sexually active (n=1,835) | 837 (54.6) | 206 (68.0) | <0.001 |
| Decreased sexual activity (n=1,835) | |||
| ‘Quite a bit’ to ‘a great deal’ | 264 (17.2) | 15 (5.0) | <0.001 |
| Decreased enjoyment of sexual activity (n=1,043) | |||
| ‘Quite a bit’ to ‘a great deal’ | 89 (10.6) | 7 (3.4) | <0.001 |
| Satisfaction for sexual activity (n=1,043) | 724 (86.5) | 190 (92.2) | 0.025 |
| ED (n=1,043) | |||
| ‘Moderately impotent’ to completely impotent’ | 75 (9.0) | 2 (1.0) | <0.001 |
Values are presented as mean±standard deviation or number (%).
LUTS, lower urinary tract symptoms; EQ-5D, EuroQoL-five dimensions; EQ-VAS, EuroQoL-visual analogue scale; WPAI, work productivity and active impairment; CES-D, center for epidemiological studies depression scale; ED, erectile dysfunction.
Table 3.
Participant-reported outcomes by age 40–49 years
| Variable | Individuals with LUTS | Individuals without LUTS | P-value |
|---|---|---|---|
| EQ-5D index score (n=751) | 0.90±0.15 | 0.95±0.09 | <0.001 |
| EQ-VAS score (n=751) | 73.7±18.8 | 77.5±19.4 | 0.001 |
| Employment status (n=751) | |||
| Full time | 454 (77.2) | 129 (79.1) | 0.156 |
| Part time | 66 (11.2) | 9 (5.5) | |
| Not employed | 68 (11.6) | 25 (15.3) | |
| WPAI (%) | |||
| Work time missed due to health (n=474) | 1.8±6.6 | 0.4±3.2 | 0.033 |
| Impairment while working due to health (n=579) | 17.4±29.0 | 11.5±25.3 | 0.068 |
| Overall work impairment due to health (n=460) | 17.3±28.4 | 10.8±24.7 | 0.034 |
| Activity impairment due to health (n=667) | 15.2±25.0 | 10.8±23.3 | 0.005 |
| Any work impairment (n=497) | 176 (45.4) | 32 (29.4) | 0.009 |
| CES-D scale ≥ 21 (n=751) | 99 (16.8) | 6 (3.7) | <0.001 |
| Currently sexually active (n=751) | 346 (58.8) | 111 (68.1) | 0.111 |
| Decreased sexual activity (n=751) | |||
| ‘Quite a bit’ to ‘a great deal’ | 95 (16.2) | 12 (7.4) | 0.010 |
| Decreased enjoyment of sexual activity (n=457) | |||
| ‘Quite a bit’ to ‘a great deal’ | 39 (11.3) | 5 (4.5) | 0.122 |
| Satisfaction for sexual activity (n=457) | 296 (85.6) | 102 (91.9) | 0.309 |
| ED (n=457) | |||
| ‘Moderately impotent’ to completely impotent’ | 18 (5.2) | 1 (0.9) | 0.164 |
Values are presented as mean±standard deviation or number (%).
LUTS, lower urinary tract symptoms; EQ-5D, EuroQoL-five dimensions; EQ-VAS, EuroQoL-visual analogue scale; WPAI, work productivity and active impairment; CES-D, center for epidemiological studies depression scale; ED, erectile dysfunction.
Table 4.
Participant-reported outcomes by age 50–59 years
| Variable | Individuals with LUTS | Individuals without LUTS | P-value |
|---|---|---|---|
| EQ-5D index score (n=609) | 0.89±0.15 | 0.96±0.09 | <0.001 |
| EQ-VAS score (n=609) | 75.6±18.5 | 78.6±26.1 | <0.001 |
| Employment status (n=609) | |||
| Full time | 358 (69.4) | 74 (79.6) | 0.243 |
| Part time | 54 (10.5) | 9 (9.7) | |
| Not employed | 104 (20.2) | 10 (10.8) | |
| WPAI (%) | |||
| Work time missed due to health (n=374) | 1.1±4.1 | 0.9±6.0 | 1.000 |
| Impairment while working due to health (n=457) | 11.8±23.3 | 5.1±18.4 | 0.009 |
| Overall work impairment due to health (n=368) | 11.1±22.3 | 5.6±19.6 | 0.033 |
| Activity impairment due to health (n=561) | 14.8±24.9 | 5.6±20.0 | <0.001 |
| Any work impairment (n=387) | 111 (35.1) | 14 (19.7) | 0.035 |
| CES-D scale ≥ 21 (n=609) | 42 (8.1) | 3 (3.2) | 0.388 |
| Currently sexually active (n=604) | 307 (59.8) | 65 (71.4) | 0.139 |
| Decreased sexual activity (n=604) | |||
| ‘Quite a bit’ to ‘a great deal’ | 75 (14.6) | 2 (2.2) | <0.001 |
| Decreased enjoyment of sexual activity (n=372) | |||
| ‘Quite a bit’ to ‘a great deal’ | 29 (9.5) | 2 (3.1) | 0.405 |
| Satisfaction for sexual activity (n=372) | 270 (88.0) | 59 (90.8) | 1.000 |
| ED (n=372) | |||
| ‘Moderately impotent’ to completely impotent’ | 24 (7.8) | 0 (0) | 0.036 |
Values are presented as mean±standard deviation or number (%).
LUTS, lower urinary tract symptoms; EQ-5D, EuroQoL-five dimensions; EQ-VAS, EuroQoL-visual analogue scale; WPAI, work productivity and active impairment; CES-D, center for epidemiological studies depression scale; ED, erectile dysfunction.
Table 5.
Participant-reported outcomes by age 60 years or older
| Variable | Individuals with LUTS | Individuals without LUTS | P-value |
|---|---|---|---|
| EQ-5D index score (n=482) | 0.88±0.17 | 0.94±0.13 | 0.028 |
| EQ-VAS score (n=482) | 75.7±19.2 | 78.7±21.2 | 0.142 |
| Employment status (n=482) | |||
| Full time | 112 (25.9) | 21 (42.0) | 0.048 |
| Part time | 76 (17.6) | 11 (22.0) | |
| Not employed | 244 (56.5) | 18 (36.0) | |
| WPAI (%) | |||
| Work time missed due to health (n=147) | 1.0±3.3 | 0.2±0.7 | 1.000 |
| Impairment while working due to health (n=195) | 12.7±26.3 | 11.1±28.3 | 1.000 |
| Overall work impairment due to health (n=144) | 12.5±26.0 | 5.5±18.7 | 1.000 |
| Activity impairment due to health (n=439) | 18.0±26.3 | 14.4±24.9 | 0.195 |
| Any work impairment (n=152) | 39 (30.5) | 4 (16.7) | 0.660 |
| CES-D scale ≥ 21 (n=482) | 36 (8.3) | 0 (0) | 0.120 |
| Currently sexually active (n=480) | 184 (42.7) | 30 (61.2) | 0.046 |
| Decreased sexual activity (n=480) | |||
| ‘Quite a bit’ to ‘a great deal’ | 94 (21.8) | 1 (2.0) | <0.001 |
| Decreased enjoyment ofsexual activity (n=214) | |||
| ‘Quite a bit’’ to ‘a great deal’ | 21 (11.4) | 0 (0) | 0.151 |
| Satisfaction for sexual activity (n=214) | 158 (85.9) | 29 (96.7) | 0.413 |
| ED (n=1,043) | |||
| ‘Moderately impotent’ to ‘completely impotent’ | 33 (17.9) | 1 (3.3) | 0.167 |
Values are presented as mean±standard deviation or number (%).
LUTS, lower urinary tract symptoms; EQ-5D, EuroQoL-five dimensions; EQ-VAS, EuroQoL-visual analogue scale; WPAI, work productivity and active impairment; CES-D, center for epidemiological studies depression scale; ED, erectile dysfunction.
Fig. 2.
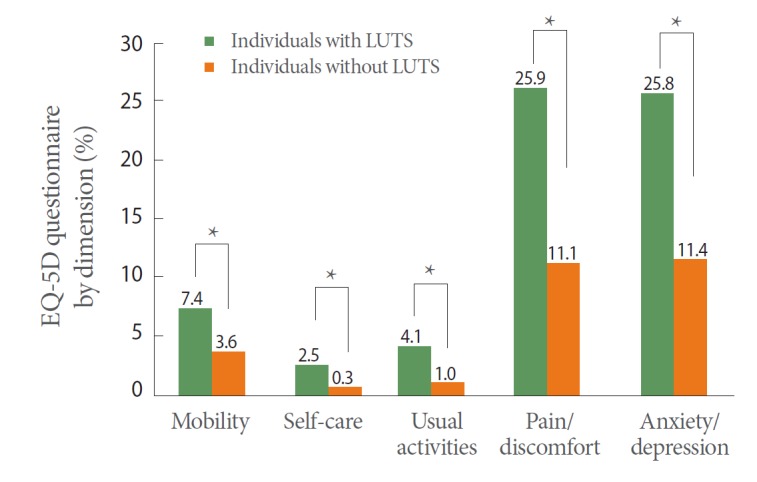
The percentage of the respondents with problems in the quality of life domains of the EQ-5D questionnaire by dimension. LUTS, lower urinary tract symptoms; EQ-5D, EuroQoL-five dimensions. *P<0.001.
Individuals with LUTS were significantly more likely to be unemployed than those without LUTS (27.1% vs. 17.3%, P<0.001). For work productivity, those with LUTS had a greater impairment on all scales of the WPAI questionnaire compared with those without LUTS (Table 2, all P<0.01). Among those with LUTS, 39.2% reported any form of work impairment compared with 24.5% of those without LUTS (P<0.001). However, there were no significant differences across groups with respect to all scales of the WPAI questionnaire among men aged ≥60 years (Table 5). Additionally, among those with LUTS, 13.1% (120/914) reported always worrying about interrupting work with frequent trips to the bathroom; 2.1% (27/1,267) reported having changed jobs, retired early, or been fired because of their urinary symptoms; and 18.7% (171/914) reported that urinary symptoms were a factor in decisions related to time and location of work.
In the evaluation of depression symptoms based on the CES-D, depressive symptoms (CES-D≥21) were significantly more prevalent in those with LUTS than in those without LUTS (Table 2, 11.5% vs. 2.9%, respectively, P<0.001). However, this result was only consistent among men aged 40–49 years among the three age groups (Table 3). Cronbach alpha coefficient for the 20 items in the CES-D was 0.876, which indicated good internal consistency.
With regard to sexual QoL, those with LUTS were less likely to report being currently sexually active compared with those without LUTS (54.6% vs. 68.0%, respectively, P<0.001) (Table 2). Also 17.2% and 10.6% of those with LUTS reported that urinary symptoms caused them to decrease sexual activity and decreased sexual enjoyment compared with 5.0% and 3.4% of those without LUTS, respectively (both P<0.001). Significantly fewer individuals with LUTS indicated satisfaction with their overall sex life compared with those without LUTS (86.5% vs. 92.2%, respectively, P=0.025). The same pattern was found with respect to decreased sexual activity due to urinary symptoms in the three age groups (Tables 3-5). However, there were no significant differences across the age groups with respect to decreased enjoyment and satisfaction of sexual activity due to urinary symptoms (Tables 3-5). Among sexually active respondents, a significantly greater proportion of individuals with LUTS reported having moderate to complete ED relative to those without LUTS (9.0% vs. 1.0%, respectively, P<0.001) (Table 2).
DISCUSSION
LUTS are highly prevalent worldwide, particularly among the elderly [8,9,12]. In 2008, an estimated 1.9 billion individuals (45.2%) worldwide were affected by at least one LUTS [21]. By 2018, it is estimated that around 2.3 billion individuals will be affected by at least one LUTS, and the regional burden of LUTS is expected to be greatest in Asia [21]. We recently reported that the overall prevalence of at least one LUTS was estimated to be 83% in Korean men aged ≥40 years, and storage symptoms (70.1%) were more prevalent than voiding (60.4%) or postmicturition symptoms (38.3%). Nocturia (65.0%) was the most common storage symptom among participants. The most common voiding symptom was terminal dribble (49.4%), and the most common postmicturition symptom was incomplete emptying (27.2%). Combined storage and voiding symptoms were the most frequently reported combination (48.0%), and 30.2% of participants reported experiencing all three symptoms [8].
Although LUTS are not life threatening, they significantly affect many dimensions of HRQoL. In this study, we addressed the individual burden of LUTS on participant-reported outcomes using clinically validated and reliable questionnaires. Our study results illustrate that LUTS are associated with poorer HRQoL. When compared with those without LUTS, those with LUTS reported a significantly lower level of overall health and work productivity, a higher level of depressive symptoms, and less sexual satisfaction. Our generic HRQoL results showed that the EQ-5D index and VAS scores were notably lower in those with LUTS than those without LUTS. In the three age groups (40–49 years, 50–59 years, and ≥60 years), a similar trend was found with respect to the EQ-5D index with significant differences. Based on the WPAI questionnaire, LUTS were associated with work productivity loss and impairment of daily activities. The work productivity loss associated with LUTS was more greatly affected by presenteeism (impairment while working) than by absenteeism (work time missed). LUTS were associated with greater overall work impairment and activity impairment (both 6% greater among those with LUTS than those without LUTS). Individuals with LUTS reported concerns related to participating in social activities and the negative effect on their daily work activities due to their urinary symptoms. These results were consistent among men aged 40–49 years and 50–59 years, but not among men aged ≥60 years. Based on the CES-D, 11.5% of those with LUTS reported having a significant level of depressive symptoms compared with 2.9% of those without LUTS. Although detailed mental health data were not collected in our survey, the results indicate that depression is a highly prevalent issue for men with LUTS. Among the three age groups, only individuals with LUTS aged 40–49 years reported a similar pattern, with significant differences in the CES-D score between those with and without LUTS. The present study also demonstrated that LUTS have been associated with decreased sexual activity and sexual satisfaction and ED. We observed that a significant percentage of those with LUTS reported that their urinary symptoms diminished the frequency of their sexual activity. Among those who were sexually active, a significant percentage of those with LUTS reported that urinary symptoms caused a reduction in their enjoyment of sexual activity and satisfaction with their overall sex lives. Furthermore, 9.0% of those with LUTS reported moderate to complete ED compared with 1.0% of those without LUTS. Although the exact relationship between male LUTS and sexual dysfunction remains unclear, recent studies have demonstrated that male LUTS are associated with decreased sexual activity and enjoyment of sex, ED, ejaculatory dysfunction, and premature ejaculation [3,22-24] Especially, Rosen et al. [22] reported a relationship between LUTS and sexual dysfunction in aging men that is independent of the effects of age, other comorbidities, and lifestyle factors.
The decrease in HRQoL associated with LUTS has been reported in previous studies. A nested case-control analysis of the EPIC study, a large population-based telephone survey in Canada, Germany, Italy, Sweden, and the United Kingdom, reported the substantial impact of OAB alone and OAB with additional LUTS on work productivity, sexuality, and overall health [3]. The Epidemiology of LUTS study, a cross-sectional, population-representative, internet-based survey conducted in the United States, the United Kingdom, and Sweden, also reported that HRQoL is affected by LUTS [25-27]. In these previous studies, a lower level of overall HRQoL, emotional well-being, and work productivity were noted for individuals with LUTS. Our findings are consistent with other epidemiologic studies that have reported that LUTS diminishes overall HRQoL, work productivity, depressive symptoms, and sexuality [2,3,6,22,25-30], and confirm that men with LUTS experience more impairment of HRQoL compared with those without LUTS in our study population.
HRQoL is a multidimensional concept of overall well-being and satisfaction associated with health and is determined by perceptions of physical, mental, emotional, and social health. It is becoming an important factor to consider in the management of a disease or specific condition. Given the impact of LUTS on HRQoL in the current study, a comprehensive and correct understanding of LUTS may facilitate the development of better urologic assessment and management, which could lead to improvements in population health. Strengths of our study include its population-based design and the evaluation of participants through face-to-face interviews.
There were a number of limitations to this study. This cross-sectional study only provided an association between LUTS and several dimensions of HRQoL and did not establish a cause-result relationship. The other major limitation is that a large proportion of individuals who were asked to participate declined, yielding a low response rate (26.8%). Participants were firstly selected at random. However, since participation was voluntary, it is possible that the subjects responding to our survey might be different from those who did not respond, and this may have led to a less representative general population. Additionally, the uneven distribution of those with LUTS and without LUTS needs to be considered. Because the prevalence of LUTS in men tends to increase with age, the number of men without LUTS was relatively small and this uneven distribution could have affected the observed differences.
In conclusion, this survey clearly demonstrated the substantial burden LUTS has on HRQoL, including generic QoL, work productivity, depressive symptoms, and sexual health in Korean men aged ≥40 years. The findings of our study emphasize the need for a timely and appropriate assessment and management of LUTS in order to improve HRQoL.
Acknowledgments
This study was supported by the Research Foundation Grant funded by the Korean Urological Association (KUA-2009-003).
Footnotes
Research Ethics
This study was approved by Institutional Review Board of the Samsung Medical Center (IRB No. 2010-02-026).
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn. 2002;21:167–78. doi: 10.1002/nau.10052. [DOI] [PubMed] [Google Scholar]
- 2.Kupelian V, Wei JT, O’Leary MP, Kusek JW, Litman HJ, Link CL, et al. Prevalence of lower urinary tract symptoms and effect on quality of life in a racially and ethnically diverse random sample: the Boston Area Community Health (BACH) Survey. Arch Intern Med. 2006;166:2381–7. doi: 10.1001/archinte.166.21.2381. [DOI] [PubMed] [Google Scholar]
- 3.Coyne KS, Sexton CC, Irwin DE, Kopp ZS, Kelleher CJ, Milsom I. The impact of overactive bladder, incontinence and other lower urinary tract symptoms on quality of life, work productivity, sexuality and emotional well-being in men and women: results from the EPIC study. BJU Int. 2008;101:1388–95. doi: 10.1111/j.1464-410X.2008.07601.x. [DOI] [PubMed] [Google Scholar]
- 4.Fitzgerald MP, Link CL, Litman HJ, Travison TG, McKinlay JB. Beyond the lower urinary tract: the association of urologic and sexual symptoms with common illnesses. Eur Urol. 2007;52:407–15. doi: 10.1016/j.eururo.2007.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fitzgerald MP, Mulligan M, Parthasarathy S. Nocturic frequency is related to severity of obstructive sleep apnea, improves with continuous positive airways treatment. Am J Obstet Gynecol. 2006;194:1399–403. doi: 10.1016/j.ajog.2006.01.048. [DOI] [PubMed] [Google Scholar]
- 6.Welch G, Weinger K, Barry MJ. Quality-of-life impact of lower urinary tract symptom severity: results from the Health Professionals Follow-up Study. Urology. 2002;59:245–50. doi: 10.1016/s0090-4295(01)01506-0. [DOI] [PubMed] [Google Scholar]
- 7.Chapple CR, Wein AJ, Abrams P, Dmochowski RR, Giuliano F, Kaplan SA, et al. Lower urinary tract symptoms revisited: a broader clinical perspective. Eur Urol. 2008;54:563–9. doi: 10.1016/j.eururo.2008.03.109. [DOI] [PubMed] [Google Scholar]
- 8.Kim TH, Han DH, Lee KS. The prevalence of lower urinary tract symptoms in korean men aged 40 years or older: a population-based survey. Int Neurourol J. 2014;18:126–32. doi: 10.5213/inj.2014.18.3.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Irwin DE, Milsom I, Hunskaar S, Reilly K, Kopp Z, Herschorn S, et al. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol. 2006;50:1306–14. doi: 10.1016/j.eururo.2006.09.019. [DOI] [PubMed] [Google Scholar]
- 10.Lee H, Jeong SJ. Epidemiology of lower urinary tract symptoms: emphasis on the status in Korea. Korean J Urol. 2014;55:300–8. doi: 10.4111/kju.2014.55.5.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Irwin DE, Milsom I, Kopp Z, Abrams P, Artibani W, Herschorn S. Prevalence, severity, and symptom bother of lower urinary tract symptoms among men in the EPIC study: impact of overactive bladder. Eur Urol. 2009;56:14–20. doi: 10.1016/j.eururo.2009.02.026. [DOI] [PubMed] [Google Scholar]
- 12.Coyne KS, Sexton CC, Thompson CL, Milsom I, Irwin D, Kopp ZS, et al. The prevalence of lower urinary tract symptoms (LUTS) in the USA, the UK and Sweden: results from the Epidemiology of LUTS (EpiLUTS) study. BJU Int. 2009;104:352–60. doi: 10.1111/j.1464-410X.2009.08427.x. [DOI] [PubMed] [Google Scholar]
- 13.Robertson C, Link CL, Onel E, Mazzetta C, Keech M, Hobbs R, et al. The impact of lower urinary tract symptoms and comorbidities on quality of life: the BACH and UREPIK studies. BJU Int. 2007;99:347–54. doi: 10.1111/j.1464-410X.2007.06609.x. [DOI] [PubMed] [Google Scholar]
- 14.Lee YS, Lee KS, Jung JH, Han DH, Oh SJ, Seo JT, et al. Prevalence of overactive bladder, urinary incontinence, and lower urinary tract symptoms: results of Korean EPIC study. World J Urol. 2011;29:185–90. doi: 10.1007/s00345-009-0490-1. [DOI] [PubMed] [Google Scholar]
- 15.EuroQol Group EuroQol: a new facility for the measurement of health-related quality of life. Health Policy. 1990;16:199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- 16.Kang EJ, Shin HS, Park HJ, Jo MW, Kim NY. A valuation of health status using EQ-5D. J Korean Health Econo Pol. 2006;12:19–43. [Google Scholar]
- 17.Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics. 1993;4:353–65. doi: 10.2165/00019053-199304050-00006. [DOI] [PubMed] [Google Scholar]
- 18.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 19.Cho MJ, Kim KH. Diagnostic validity of the CES-D (Korean version) in the assessment of DSM-III-R major depression. J Korean Neuropsychiatr Assoc. 1993;32:381–99. [Google Scholar]
- 20.O’Donnell AB, Araujo AB, Goldstein I, McKinlay JB. The validity of a single-question self-report of erectile dysfunction. Results from the Massachusetts Male Aging Study. J Gen Intern Med. 2005;20:515–9. doi: 10.1111/j.1525-1497.2005.0076.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Irwin DE, Kopp ZS, Agatep B, Milsom I, Abrams P. Worldwide prevalence estimates of lower urinary tract symptoms, overactive bladder, urinary incontinence and bladder outlet obstruction. BJU Int. 2011;108:1132–8. doi: 10.1111/j.1464-410X.2010.09993.x. [DOI] [PubMed] [Google Scholar]
- 22.Rosen R, Altwein J, Boyle P, Kirby RS, Lukacs B, Meuleman E, et al. Lower urinary tract symptoms and male sexual dysfunction: the multinational survey of the aging male (MSAM-7) Eur Urol. 2003;44:637–49. doi: 10.1016/j.eururo.2003.08.015. [DOI] [PubMed] [Google Scholar]
- 23.Rosen RC, Giuliano F, Carson CC. Sexual dysfunction and lower urinary tract symptoms (LUTS) associated with benign prostatic hyperplasia (BPH) Eur Urol. 2005;47:824–37. doi: 10.1016/j.eururo.2004.12.013. [DOI] [PubMed] [Google Scholar]
- 24.Wein AJ, Coyne KS, Tubaro A, Sexton CC, Kopp ZS, Aiyer LP. The impact of lower urinary tract symptoms on male sexual health: EpiLUTS. BJU Int. 2009;103 Suppl 3:33–41. doi: 10.1111/j.1464-410X.2009.08447.x. [DOI] [PubMed] [Google Scholar]
- 25.Coyne KS, Wein AJ, Tubaro A, Sexton CC, Thompson CL, Kopp ZS, et al. The burden of lower urinary tract symptoms: evaluating the effect of LUTS on health-related quality of life, anxiety and depression: EpiLUTS. BJU Int. 2009;103 Suppl 3:4–11. doi: 10.1111/j.1464-410X.2009.08371.x. [DOI] [PubMed] [Google Scholar]
- 26.Coyne KS, Sexton CC, Kopp ZS, Ebel-Bitoun C, Milsom I, Chapple C. The impact of overactive bladder on mental health, work productivity and health-related quality of life in the UK and Sweden: results from EpiLUTS. BJU Int. 2011;108:1459–71. doi: 10.1111/j.1464-410X.2010.10013.x. [DOI] [PubMed] [Google Scholar]
- 27.Milsom I, Kaplan SA, Coyne KS, Sexton CC, Kopp ZS. Effect of bothersome overactive bladder symptoms on health-related quality of life, anxiety, depression, and treatment seeking in the United States: results from EpiLUTS. Urology. 2012;80:90–6. doi: 10.1016/j.urology.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 28.Irwin DE, Milsom I, Kopp Z, Abrams P, Cardozo L. Impact of overactive bladder symptoms on employment, social interactions and emotional well-being in six European countries. BJU Int. 2006;97:96–100. doi: 10.1111/j.1464-410X.2005.05889.x. [DOI] [PubMed] [Google Scholar]
- 29.Li MK, Garcia LA, Rosen R. Lower urinary tract symptoms and male sexual dysfunction in Asia: a survey of ageing men from five Asian countries. BJU Int. 2005;96:1339–54. doi: 10.1111/j.1464-410X.2005.05831.x. [DOI] [PubMed] [Google Scholar]
- 30.Irwin DE, Milsom I, Reilly K, Hunskaar S, Kopp Z, Herschorn S, et al. Overactive bladder is associated with erectile dysfunction and reduced sexual quality of life in men. J Sex Med. 2008;5:2904–10. doi: 10.1111/j.1743-6109.2008.01000.x. [DOI] [PubMed] [Google Scholar]


